Abstract
Objectives
To examine how nursing home characteristics impacted the number of lawsuits filed against the facilities in the United States during 1997–2001.
Data Sources/Study Setting
A stratified random sample of 2,378 nursing home in 45 states from 1997–2001. Data were obtained from Westlaw's Adverse Filings: Lawsuits database, the Centers for Medicare and Medicaid Services' (CMS) Online Survey, Certification, and Reporting (OSCAR) database, state complaint surveys, and through primary data.
Study Design
Negative binomial regression was used to explain total lawsuit variance by year. Explanatory variables included (a) facility characteristics—including staffing, number of beds, multistate system membership, for-profit ownership, (b) quality indicators—including total number and type of quality survey deficiencies, pressure sore development, and (c) market area—state has resident rights statutes, state complaint information. Resident acuity levels and year effects were controlled for.
Data Collection/Extraction Methods
Nursing homes were identified and linked to Westlaw data that was searched for the number of lawsuits filed against the home, and then linked to OSCAR data and a primary data analysis of multistate chain membership.
Principal Findings
Staffing levels for certified nursing assistants (CNAs) and registered nurses (RNs) and multistate chain membership were negatively related with higher numbers of lawsuits. More deficiencies on the licensing survey, larger, for-profit nursing homes, and being located in resident rights states were positively related with higher numbers of lawsuits.
Conclusion
This study suggests that nursing homes that meet long-stay staffing standards and minimum quality indicators, are nonprofit, smaller, and not located in resident rights states will experience fewer lawsuits.
Keywords: Litigation, nursing homes, nurse staffing, long-term care
Policymakers continue to grapple with the escalating growth of the elderly population in the United States. The current and predicted strains on an already resource-strapped sector of the health care system are major concerns for both researchers and the general public. Of particular interest is the quality of care provided to this vulnerable population. Nursing homes trying to meet the requirements of the Omnibus Budget Reconciliation Act of 1987 (P.L. 100-203; 101 Stat. 1330) deal with a resident population that is very vulnerable due to chronic disease and disability. When adverse events occur within the elderly population, a common response is to seek legal remedy through the court system. The nursing home industry believes that many of these lawsuits are driven by monetary greed, while families, trial lawyers, and other advocates see the court system as a legitimate check on a long-term care industry known for high-profile examples of poor quality of care.
There are very few studies that use data aimed at disentangling the relationship between quality of care and litigation activity against nursing homes. Studies are beginning to emerge that examine Florida's experience within its litigious environment. Lobbying groups funded most of the recent national studies for various interests concerned about the ramifications of policy changes to various regulatory statutes around the country (Bourdon and Dubin 2002). The few national studies not funded by these groups show an increase in both the numbers of lawsuits filed against nursing homes and the costs of these suits to the industry (Stevenson and Studdert 2003). Much of this independent empirical work is exploratory in nature and is limited by sample size or geography, but it is providing the first objective evidence about the nursing home litigation climate in the United States.
This study examines these issues through the litigation experience of 2,378 nursing homes operating in 45 states from 1997 to 2001. A stratified random sample of nursing homes was linked to information about lawsuits filed against these facilities stored in Westlaw's Adverse Filings: Lawsuits database. These data were linked to the Centers for Medicare and Medicaid Services' (CMS) Online Survey, Certification, and Reporting (OSCAR) system for structural and quality survey information. Building on previous research in smaller samples, a predictive model was analyzed using negative binomial regression modeling techniques to determine the influence of nursing home quality and structure on the number of lawsuits filed against a facility over time.
We hypothesize that nursing homes will have more lawsuits filed against them if (a) the homes have poor quality of care, (b) have more financial resources available to them, and (c) are more exposed due to their number of residents. Variables used in the analysis were chosen to measure these dimensions while also controlling for the acuity level of the residents.
Nursing Home Litigation in the United States
There is growing evidence that litigation against nursing homes in the United States is placing a strain on industry resources. There is very little question in the empirical literature about the appropriateness of the majority of lawsuits brought against facilities. Most involve legitimate issues surrounding residents, employees, and companies with whom the nursing homes contract. The focus of concern has been on the litigation process. One study examined the costs associated with nursing home litigation, but that study focused only on jury awards (Bennett et al. 2000). The vast majority of nursing home lawsuits are settled out of court and never go to trial. This means that there is little public information available about the total dollars expended by nursing homes and their insurance companies to pay for litigation related costs. The one study that conducted a national sample of lawyers found that 88 percent of all cases were resolved through settlements and that the average recovery of claims was $406,000 (Stevenson and Studdert 2003).
In addition to concern regarding the size of awards paid as a result of these lawsuits, there is concern that liability insurance premiums are skyrocketing. Insurers in Florida began to drastically increase liability insurance premiums to the point that 9 percent of the nursing homes in Florida began to operate with no insurance coverage in 2001. At the same time, most liability insurers in Florida stopped writing new policies for long-term care facilities (Florida Policy Exchange Center on Aging 2001). Those that were still renewing policies were increasing premiums from 100 percent to 1,000 percent from previous year rates (Hedgecock and Salmon 2001).
Policymakers have begun to examine the impact of statutes that allow for individual causes of action in resident rights states. These “rights statutes” represent a major remedy offered by the courts for resident care issues. These regulatory changes were put into place because it was believed that malpractice lawsuits brought under negligence standards were too restrictive, although claims could also be brought against nursing homes under various intentional tort and contract claims. The limitations of malpractice law in the nursing home arena are discussed in more detail in previous work (Johnson, Atherly, and Bunderson 2000; Johnson and Bunderson 2002; Williamson 1999). One primary example is that under the Florida Wrongful Death Act of 2004 (Fla. Stat. §§ 768.16–26), only a surviving spouse or child under the age of 25 can bring a wrongful death claim unless the resident was found to be incompetent prior to his or her death. Most nursing home residents do not have a surviving spouse or children under 25. In Florida, 20 percent of long-term care nursing home residents with less than one year in a facility have no identified family (Polivka, Dunlop, and Brooks 1997).
Resident rights statutes establish the individual rights that residents have while under nursing home care and were created to resolve some of the limitations of malpractice law. From a legal standpoint, the statutes create different causes of action that may be brought against nursing homes than those found under malpractice law. Negligence requires the plaintiff to demonstrate that care provided within the nursing home failed its duty to comply with the appropriate standard of care and that the plaintiff was injured as the result of this failure. Lawsuits brought under the resident rights laws require the nursing home to prove that it did not violate the resident's rights as defined by the statutes. This is easier to prove than under a cause of action for negligence (Williamson 1999).
A study commissioned by the American Health Care Association identified Florida, Texas, Arkansas, California, and Georgia as states that had strong resident rights laws that seem to be impacting the number of claims filed against facilities (Bourdon and Dubin 2002). This study provided descriptive data about the claims experiences of 26 percent of the nursing home beds in the United States. The report highlights the high number of claims in Florida and other resident rights states, as well as some states like Louisiana where there are no resident rights laws in place. These data suggest that a more careful empirical examination of these trends be conducted to gather further information about the predictors of litigation activity.
Data Sources
Westlaw's Adverse Filings Lawsuits database was used to gather the number of lawsuits filed against the nursing homes in this study. This is a subscription service and it provides the most comprehensive public records coverage of lawsuit filings available in the United States. This is a database that is part of the public records information maintained by Westlaw that is the “Combined Lawsuit Records” database. It contains the litigation information about lawsuits filed against individuals and organizations in 500 counties and 45 states. The database contains information about the plaintiff and defendant, case number, filing date, and type of action. There are other subscription services available that provide public records of national lawsuit data, but the coverage in those sources is limited to fewer states and counties.
Researchers must overcome a number of issues in order to use Westlaw data for empirical research. Information about the lawsuits is limited and must be searched using each individual nursing home's name, corporate name, or some variation of the two. If the individual case numbers are known for suits brought against facilities, the lawsuit database can be searched using case numbers. In most cases, researchers will not have this information available to them and must do name-based searches. This study counted by year all lawsuits related to the nursing home or its employee's malpractice under negligence or intentional tort or breach of contract that were contained within the public records database.
The sample design used for this study is a stratified sample. A sample is stratified if it is obtained by independently selecting a random sample from each population “stratum” (Lapin 1978). The strata that we are interested in for this study are ownership, member of a chain or system, and by state. We performed this type of sample to ensure that subgroups of a population are represented in the sample in accordance with their prevalence within the population. This means that within our total population of nursing homes, we want to make sure that ownership type and chain membership reflect the numbers found within the population at large. The sample used in this data analysis was stratified using this design. The sample was within±3 percent of the population average for each cell. We used OSCAR to define the population of nursing homes available within each state.
There were fewer than 15,000 nursing homes in the states available in the Westlaw data. With an historical proposition of 0.5, margin of error of 0.02, a 95 percent confidence level, and a z-score 1.96, the sample size necessary is 2,070. Seventy-five percent of the nursing homes in the population available for this study were for-profit, so at least 1,553 of our sample should be for-profit nursing homes, at least 518 should be nonprofit, and we matched the proportion expected for each by the state the nursing home was located in. This proportion was established by continuing to sample the entire population of nursing homes in the states until we achieved the total numbers necessary to satisfy the condition of the strata and reach our required total sample size.
The search methodology used to identify lawsuits and link them to specific cases involves a manual search followed by linking the results of this search to secondary data sources. HealthGrades maintains a crosswalk database that tracks the provider ID of the nursing homes and any name changes that occur for facilities in the United States. This database was used to identify the names that were used to search for lawsuits using both the full name and truncated versions. Once the type of lawsuit was identified, it was added to the total count for the facility for the year the lawsuit occurred.
The Westlaw database has a number of issues associated with it when applied to empirical research. Because we used a conservative inclusion algorithm to count the number of lawsuits, this study may be undercounting the number of lawsuits. There does not appear to be a pattern of systemic exclusion of lawsuits from our data. We base this observation on previous data collected in Hillsborough County's Circuit Court from 1990 to 2001 (Hedgecock et al. Forthcoming) and a comparison with a Florida study that counted the number of lawsuits in Westlaw's data for all nursing homes in Hillsborough County and 29 other Florida counties (Johnson et al. 2003). Where Westlaw data listed individuals and associated nursing homes as defendants on cases, the lawsuit was counted for that nursing home. While the overall numbers of cases included in the Westlaw data were very close when a search was done using known case numbers, a crosscheck of totals using name searches revealed fewer lawsuits from the Westlaw search. The reasons for this discrepancy center around misnamed defendants on lawsuits in the data and listing corporations as defendants without listing the nursing home in question.
Online Survey, Certification, and Reporting (OSCAR) is a database of nursing home licensing survey deficiencies and other structural variables that can be used to analyze the effects of nursing home structure and quality indicators on lawsuit activity. There are concerns related to using OSCAR data (Centers for Medicare and Medicaid Services 2001), but these data have been used to conduct research that examines whether or not nursing homes are meeting minimum quality standards across different health survey variables (Harrington, Zimmerman et al. 2000b). We did not use the “chain” variable in OSCAR because the way that variable is coded included systems that were too small to be considered a chain in this analysis. We hand-corrected all of the OSCAR chain information in our data to reflect nursing homes that were part of nursing home multistate chains or systems.
Specification of the Variables
Explanatory Variables
The OSCAR data and skilled nursing facility complaint data were used to capture information about the staffing structure, care processes that occurred within the nursing home, and deficiency data from 1997 to 2001. These quality-related variables were specified at the nursing-home level and included:
Whether the nursing home met the CMS-recommended, long-stay 2.8 certified nursing assistant (CNA) hour per resident day standard for CNAs, the 1.3 hour per resident day standard for licensed practical nurses (LPN), and the 0.75 hour per resident day standard for registered nurses (RN);
Development of new pressure sores within the facility per resident in the home;
Total number of deficiencies cited on state licensing survey; and
Whether the home was cited for an actual harm severity violation (G or higher) on the state licensing survey.
Many consumer groups and proponents such as the American Association of Retired Persons (AARP) view litigation as the ultimate motivator for higher quality of care within nursing homes (Florida Policy Exchange Center on Aging 2001). This argument rests on the hypothesis that there is a relationship between the quality of care provided by the nursing home and whether or not a nursing home is sued. Nurse staffing levels were shown in a number of studies to impact the quality of care outcomes within long-term care facilities (Bliesmer et al. 1998; Wunderlich, Sloan, and Davis 1996). There are currently no enforced minimum national staffing standards, although many states do mandate that nursing homes staff their facilities at specific levels (Harrington, Kovner et al. 2000a). Abt Associates and CMS made specific recommendations about the resident hours per staff that lead to better outcomes for long-stay residents (Centers for Medicare and Medicaid Services 2001). These long-stay residents are more likely to be involved in litigation activity. We used the weighted threshold staffing ratios that were found related to long-stay quality in nursing homes. Lower staffing levels could mean poorer quality of care for residents and this poorer quality of care may translate into higher numbers of lawsuits. Facility outcomes such as development of preventable pressure sores (U.S. General Accounting Office 1999), the total number of deficiencies cited against a nursing home during state licensing and complaint surveys (Harrington and Carrillo 1999), and the severity of those deficiencies could indicate a poor-quality facility. Nursing home survey deficiencies were found to significantly predict higher numbers of lawsuits in previous work (Johnson et al. 2003).
Structure's impact on nursing home litigation is not limited to staffing considerations. We specified these nursing home financial and size characteristics as:
Member of a system or chain;
Percent Medicaid residents of total residents;
Number of nursing home beds; and
For-profit.
The resources that a nursing home has at its disposal may encourage litigious activity against nursing homes. For example, attorneys may seek lawsuits against people and organizations that have the ability to pay the fines and claims against them. Previous studies found that nursing homes that are part of large systems or chains and are larger facilities were sued at significantly higher levels than smaller systems or independent nursing homes (Johnson et al. 2001). Multifacility organizations generally have access to system-level resources through which judgments can be paid. Less financially strong and smaller nursing homes may not be able to pay the judgment against them and may not have sufficient insurance coverage, causing them to go out of business or declare bankruptcy. Larger homes may also have higher numbers of residents that represent potentially more risk for lawsuits. For-profit multifacility chains have a higher proportion of Medicaid residents (Florida Policy Exchange Center on Aging 2001). For-profit ownership has been shown to be linked to poor quality of care outcomes (Aronson, Zinn, and Rosko 1994; Chou 2002; Grabowski and Hirth 2003; Spector, Selden, and Cohen 1998) and may cause significantly higher numbers of lawsuits.
Market related variables were constructed to examine state environmental influences on litigation activity. These variables included:
Whether or not the state where the nursing home is located in has residents rights statutes in place;
Mean number of complaints filed in the state per 100 beds; and
Mean number of minutes it took the states to investigate complaints.
The specific impacts of statutes on litigation activity is the subject of descriptive and anecdotal analysis, but no national representative empirical study has attempted to disentangle the impacts of these statutes on litigation activity. Our hypothesis that states with private rights to action under resident rights statutes will have higher litigation activity is based on the experiences of Florida and Georgia. The states coded as being resident rights states had these laws in place throughout 1997–2001. The mean number of complaints and the time taken to investigate those complaints may reflect both the dissatisfaction with nursing home care at the state level and the timeliness of complaint investigations within the states. High numbers of complaints and long investigation times could be an indicator of markets that are more likely to attract higher levels of litigation activity.
Dependent Variable
The dependent variable in this analysis was constructed using Westlaw's Adverse Filings: Lawsuits database and is the total number of lawsuits filed against a nursing home each year during 1997–2001. The coverage within the database was limited to 500 nonrural counties in 45 states. The records reflect lawsuits filed against the nursing home, including those filed because of malpractice, negligence, employee problems, or breach of contract. Many of these cases have additional named defendants. A home can be part of a chain and the parent corporation can be listed as a defendant as well as the home's physical plant. In some cases individuals are listed in the case document as defendants. Claims filed against the individual nursing home were included as a lawsuit in this count if the suit named the facility or an individual that worked in the facility as a defendant. Multiple defendants for one claimant were counted as a lawsuit against all listed defendants.
Control Variables
The different acuity levels of residents within facilities were controlled for in this analysis. We controlled for the number of residents that required tube feeding or were bowel incontinent, and new catheter residents per the total resident population in the nursing home. Residents that require tube feeding, are bowel incontinent, or require catheterization can indicate a higher acuity level of residents in the home compared to those homes with fewer residents with these characteristics (Aziz and Campbell-Taylor 1999; Newman and Palmer 1999). Year effects were controlled for in the data using dummy variables for each year, but 1997 was omitted from the analysis because that year had the lowest litigation activity in our data. Table 1 lists the descriptive statistics for all of the variables included in the model. Table 2 lists the variables used in the models and how they were coded for analysis.
Table 1.
Descriptive Statistics for Nursing Homes Sample, 1997–2001 (N=2,378)
| Descriptive Statistics | ||||
|---|---|---|---|---|
| Mean or % | SD | Min. | Max. | |
| Dependent Variables | ||||
| Lawsuits per home per year | 0.22 | 0.69 | 0 | 18 |
| Quality Variables | ||||
| Met CMS recommended long stay CNA staffing levels per any year | 17.1% | |||
| Met CMS recommended long stay LPN+RN staffing levels per any year | 7.1% | |||
| Met CMS recommended long stay RN staffing levels per any year | 14.0% | |||
| Skin pressure sores developed in the nursing home ratio per year | 0.036 | ±0.037 | 0 | 1 |
| Total survey deficiencies per year | 5.50 | ±6.02 | 0 | 62 |
| Actual harm citation | 27.7% | |||
| Resource Variables | ||||
| System membership | 31.8% | |||
| Medicaid resident ratio per year | 0.66 | ±0.22 | 0 | 1 |
| Nursing home size (no. of beds) per year | 118.28 | ±60.29 | 10 | 657 |
| For-profit | 75.0% | |||
| Market Variables | ||||
| Resident rights state | 52.4% | |||
| State complaint mean number | 350.1 | ±411.22 | 0 | 4,129 |
| Mean minutes for state complaint investigation | 986.25 | ±735.91 | 96 | 4,981 |
| Control Variables | ||||
| Residents requiring tube feeding ratio per year | 0.073 | ±0.069 | 0 | 1 |
| Residents bowel incontinent ratio per year | 0.46 | ±0.18 | 0 | 1 |
| New residents requiring catheters in the nursing home ratio per year | 0.019 | ±0.03 | 0 | 0.76 |
| Total residents per year | 100.16 | ±53.35 | 1 | 633 |
Table 2.
Variable Specification
| Dependent Variables | |
|---|---|
| Total Lawsuits Filed | =Total lawsuits brought against the nursing home for that year |
| Quality Variables | |
| Met CMS recommended long stay CNA staffing levels per any year | =1 if nursing home met the 2.8 CNA hour per resident day standard for that year |
| Met CMS recommended long stay LPN+RN staffing levels per any year | =1 if nursing home met the 1.3 LPN+RN hour per resident day standard for that year |
| Met CMS recommended long stay RN staffing levels per any year | =1 if nursing homes met the 0.75 hour per resident day standard for that year |
| Skin pressure sores developed in the nursing home ratio per year | =Total skin sores in home minus total skin sores at admission divided by total residents for that year |
| Total survey deficiencies per year | =Total number of health survey deficiencies for that year |
| Actual harm citation | =1 if nursing home was cited for an actual harm severity (G or higher) on the licensing survey |
| Resource Variables | |
| System membership | =1 if nursing home was a member of a 30 facility or greater nursing home chain |
| Medicaid resident ratio per year | =Total number of Medicaid residents divided by total residents for that year |
| Nursing home size (no. of beds) per year | =Total number of nursing home beds for that year |
| For-profit | =1 if nursing home is a for-profit organization |
| Market Variables | |
| Resident rights state | =1 if state has residents rights laws |
| State complaint mean number | =Mean number of complaints per 100 beds for the state home is located in |
| Mean minutes for state complaint investigation | =Mean hours it takes state to investigate complaint from time filed to investigation initiated |
| Control Variables | |
| Residents requiring tube feeding ratio per year | =Total residents tube feeding dependent divided by total residents for that year |
| Residents bowel incontinent ratio per year | =Total bowel incontinent residents divided by total residents for that year |
| New residents requiring catheters in the nursing home ratio per year | =Total catheter patients in home minus total catheter patients at admission divided by total residents for that year |
| Year* | =1 for year (Year 1997, Year 1998, Year 1999, Year 2000, Year 2001) |
1997 was the omitted comparison year for the analysis.
Data Analysis
The dependent variable in this study is a count of the total number of lawsuits filed against a nursing home during a given year. Poisson models are widely used in the regression analysis of count data such as these. The use of a Poisson model, though, requires the variance of the dependent variable to be equal to the mean. If the variance exceeds the mean, then the counts display extra-Poisson variation, or overdispersion, and another model that takes this into account is necessary. A common model for dealing with overdispersion in count data is a negative binomial regression model. Because overdispersion is present in the count data on the total number of lawsuits filed, the effect of nursing home characteristics on the total number of lawsuits filed is examined using a negative binomial regression. The unconditional likelihood for an observation in a negative binomial regression model is:
where p=1/(1+αμ), α is the shape parameter, which accounts for the level of overdispersion in the data, μ=exp(xiβ), where xi corresponds to the vector of nursing home characteristics, and m=1/α. The coefficients (β) and the shape parameter (α) are estimated using maximum likelihood estimation.
Because individual facilities could appear in the data up to five times (once for each year of data collection), it is possible that observations within facilities are correlated over time. To account for potential correlation among observations from the same facility, the standard errors are adjusted using the Huber/White heteroskedastic consistent estimator of the variance/covariance matrix (White 1980) with a cluster correction, as found in Stata (Stata 2001). The coefficients from the negative binomial regression model are converted to incidence rate ratios by exponentiating the coefficients. These incidence rate ratios enable us to discuss the results in terms of percent differences in the rate at which lawsuits were filed against nursing home facilities.
Findings
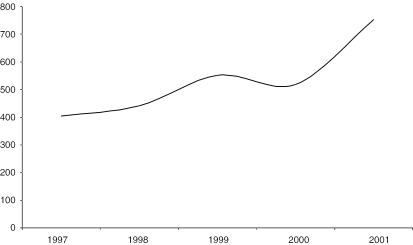
Florida and California contributed only 16 percent of the total nursing homes in our sample yet they accounted for 41 percent of the total lawsuits in our analysis. Ohio contributed 12 percent of the total lawsuits followed by Pennsylvania and Illinois at 7 percent. Texas has been identified in the literature as a high-litigation state. The 145 Texas nursing homes in our data contributed 2 percent of the lawsuits in the sample. Figure 1 shows the number of lawsuits filed against nursing homes in the 45 states from 1997 to 2001. There were 2,668 total lawsuits filed against the nursing homes in our sample during this time period. There was a 6 percent decline in the total number of filed lawsuits from 1999 to 2000. Otherwise, lawsuit activity rose from a low of 404 suits in 1997 to a high of 752 lawsuits in 2001. For-profit homes had a higher overall mean number of suits, were less likely to meet the long-stay staffing ratios, and had poorer quality indicators in comparison to nonprofit homes. For-profit homes were in 68 percent of the systems or chains, had higher Medicaid ratios, and were smaller in size. They were more likely to be in resident rights states that allow for individual causes for action, had more complaints per 100 beds in their state, and faster resolution of complaint investigations. For-profits had more residents that required tube-feeding, catheters, and were bowel incontinent.
Figure 1.
Total Lawsuits for Sample, 1997–2001
The negative binomial regression results in Table 3 indicate that the quality-related explanatory variables that were significant had the hypothesized effect on higher litigation in the sample. Meeting the long-stay recommended standards for CNAs lowered the litigation incidence rate by 15 percent and meeting the RN standard lowered the lawsuit rate 23 percent. Having more total survey deficiencies was significant, but yielded only a 3 percent increase in lawsuit rates. Meeting the LPN plus RN long-stay standard, development of new pressure sores, and having an actual harm citation did not cause the hypothesized impact on lawsuit activity. Meeting the CNA long-stay standard was significant at the .10 level and was the weakest relationship as far as statistical significance is concerned.
Table 3.
Negative Binomial Regression Results
| Total Lawsuits per Year | |||
|---|---|---|---|
| Explanatory and Control Variables | Incidence Rate Ratio | Standard Error | Z-Score |
| Quality Variables | |||
| Met CMS recommended long stay CNA staffing levels per any year | 0.85 | 0.083 | −1.69* |
| Met CMS recommended long stay LPN+RN staffing levels per any year | 1.21 | 0.173 | 1.33 |
| Met CMS recommended long stay RN staffing levels per any year | 0.77 | 0.086 | −2.36** |
| Skin pressure sores developed in the nursing home ratio per year | 0.99 | 0.009 | −0.64 |
| Total survey deficiencies per year | 1.03 | 0.004 | 5.95*** |
| Actual harm citation | 1.03 | 0.064 | 0.48 |
| Resource Variables | |||
| System membership | 0.84 | 0.07 | −2.11** |
| Medicaid resident ratio per year | 0.99 | 0.001 | −1.28 |
| Nursing home size (# of beds) per year | 1.01 | 0.001 | 11.74*** |
| For-profit | 1.28 | 0.14 | 2.24** |
| Market Variables | |||
| Resident rights state | 1.61 | 0.127 | 6.05*** |
| State complaint mean number | 0.99 | 0.0001 | −3.65*** |
| Mean minutes for state complaint investigation | 0.99 | 0.0001 | −4.46*** |
| Control Variables | |||
| Residents requiring tube feeding ratio per year | 1.05 | 0.006 | 9.30*** |
| Residents bowel incontinent ratio per year | 1.00 | 0.002 | 0.51 |
| Residents requiring catheters in the nursing home ratio per year | 0.96 | 0.011 | −3.19*** |
| Year 1998 | 1.17 | 0.094 | 1.89* |
| Year 1999 | 1.25 | 0.093 | 3.04*** |
| Year 2000 | 1.17 | 0.093 | 1.95* |
| Year 2001 | 1.54 | 0.129 | 5.20*** |
Significant at the .10 level;
Significant at the .05 level;
Significant at the .01 level.
The resource related variables that were significant in the analysis were system membership, number of beds within the facility, and for-profit ownership. Facilities that were part of a system experienced a 16 percent decrease in the litigation rate. The size of the facility was highly significant, but only raised the lawsuit incidence rate by 1 percent. For-profit ownership experienced a 28 percent higher lawsuit rate than not-for-profits. Medicaid resident ratios were not significant in the results. These resource-related variables indicate that for-profit, large nursing homes will more likely be sued in the sample, but being a part of a system or chain will have a reducing effect.
The market-related variables were all significant. Nursing homes located in resident rights states experienced a 61 percent higher litigation incidence rate. The mean number of complaints per 100 beds and mean minutes for state complaints were both significant, but not in the hypothesized directions. Facilities in states with fewer mean complaints and shorter investigation times experienced a 1 percent increase in the lawsuit incidence rate.
Residents requiring tube-feeding and catheters had opposite impacts on the number of lawsuits. Facilities with more tube-feeding residents saw a 5 percent increase in their total lawsuits incidence rate. Nursing homes with higher new catheter residents experienced a 4 percent decrease in the rate of lawsuits. The significant results of the year control variables confirm some of the trends shown in Figure 1. Each year in the model was significantly higher in litigation activity compared to 1997. The strength of these relationships almost mirrors the lawsuit activity trend lines.
Discussion
The results from this research are generally consistent with previous work examining litigation activity in Florida at both the state and county level. A 30-county Florida sample found that quality indicators and resource variables were impacting litigation rates in the state. This national sample found similar results with the exception that being a member of a multifacility chain was significant and reduced lawsuits against facilities in this sample. The relationship between size and higher numbers of lawsuits was consistent with our previous work and continues to reflect the greater exposure that larger nursing homes have compared to smaller facilities with fewer residents. However, this effect is small compared to other resource variables in the model. The relationship between for-profit ownership and lawsuit activity is consistent with our Florida work. The empirical question remains unanswered as to whether quality of care explains the filing of a lawsuit or if lawyers target for-profit homes because of their ability to pay settlements or judgments.
This study confirms the quality indicator results from our previous Florida study. High numbers of deficiencies appear to trigger greater litigation activity, although there is only a 3 percent increase in the incidence rate ratio. There are two potential interpretations of this result. The first explanation is that these indicators represent a minimum level of quality that, if not met, will lead to higher litigation activity against the home. Another explanation is that the legal community is aware of the nursing homes that have high numbers of survey deficiencies and target these homes since this information is available to the public. Which explanation is closer to the truth is the subject of further empirical analysis.
The data in this study provide comprehensive insights about litigation activity against nursing homes in the United States. While the Westlaw database is extensive, there is a high probability that we are undercounting the total number of lawsuits filed against nursing homes. The number of homes in our study reflects the experience of facilities in primarily urban counties in 45 states, but these results may not be general enough to be applied to rural parts of the country. The robustness of our quality and resource explanatory variables represents the best that were available to this study, but they are not a perfect set. The reliability and sensitivity of the OSCAR data and the variation in nursing home quality inspections have been questioned in national studies (Centers for Medicare and Medicaid Services 2001). Good financial data about nursing homes at the national level is not released to researchers or the public in any meaningfully way except through SEC reports for those homes and chains required to file those reports. Despite these limitations, what can be said is that (1) staffing- and deficiency-related quality indicators significantly impacted litigation in the United States, (2) multistate membership lowered lawsuit activity while size and for-profit ownership saw higher numbers of lawsuits, and (3) nursing homes located in a resident rights state that allows for individual causes of action experienced higher litigation activity while the mean number of complaints and time associated with complaint investigation lowered lawsuit activity. It does not appear that decisions to sue nursing homes are driven by the specific clinical outcome-related quality indicators used in this analysis, nor does targeting homes with fewer Medicaid residents drive them.
Anecdotal evidence provided in the literature argues that nursing home chains are being unfairly targeted in resident rights states. Many in the nursing home industry argue that they are providing the same quality of care across the country and it is only in states where litigation activity is encouraged by statute that they are experiencing higher numbers of lawsuits. These results partially support this conclusion, but with an alternative explanation. It may be that states with resident rights laws are associated with higher litigation rates against facilities compared to nonresident rights states. It is an empirical question as to whether or not the rate of litigation given the quality of care provided by these facilities reflects the unfairness of statues in resident rights states or if there are too few lawsuits in the states where such laws are not in effect. In any event, it is not surprising that litigation is potentially more common in resident rights states. State legislatures enacted these laws for that very purpose—to make it easier for residents to successfully sue nursing homes that failed to provide treatment in ways that are consistent with the rights of residents as specified in these statutes. In that sense, these statutes may be successful in achieving the goal of providing a cause of action that is easier to prove than traditional malpractice claims based on standards of negligence.
As found in our examination of Florida's litigation experience, the implication for administrators from these results, if taken at face value, is that meeting the CNA and RN long-stay recommended standards and meeting minimum quality standards as measured by the health survey could potentially be defenses a nursing home can use against higher litigation rates. The implications for the nursing home industry is to consider that higher litigation activity may be the cost of doing business in the United States if (1) the facility is for-profit owned, (2) it is a large nursing home, and (3) it is located in a resident rights state that allows individual causes of action. The implications for research are that we need to better understand in larger samples (1) the relationship between staffing and litigation activity in homes, (2) the relationship between “deep” financial pockets and higher lawsuits against facilities, (3) the relationship of lawsuits to the availability and affordability of liability insurance, and (4) the decision-making processes used by lawyers and families to sue nursing homes. This stream of inquiry has begun to uncover the complexities associated with litigation health services research in the nursing home industry. In this current atmosphere of litigation “crisis,” both in the nursing home and physician arenas, untangling these issues will provide information about factors that are better at predicting litigation activity so that administrators and policymakers can make informed decisions about the best way to respond to litigation pressures. Policymakers will have to decide how to balance between the ability of residents to sue nursing homes and the impact of this litigation activity on the industry.
References
- Aronson W E, Zinn J S, Rosko M D. “Do For-Profit Nursing Homes Behave Differently?”. Gerontologist. 1994;34(6):775–86. doi: 10.1093/geront/34.6.775. [DOI] [PubMed] [Google Scholar]
- Aziz S J, Campbell-Taylor I. “Neglect and Abuse Associated with Undernutrition in Long-Term Care in North America: Causes and Solutions.”. Journal of Elder Abuse and Neglect. 1999;10(1–2):91–117. [Google Scholar]
- Bennett R, O'Sullivan J, DeVito E, Remsburg R. “The Increasing Medical Malpractice Risk Related to Pressure Ulcers in the United States.”. Journal of American Geriatric Society. 2000;48(1):73–81. doi: 10.1111/j.1532-5415.2000.tb03033.x. [DOI] [PubMed] [Google Scholar]
- Bliesmer M, Smayling M, L Kane R, Shannon I. “Relationship between Nursing Staffing Levels and Nursing Home Outcomes.”. Journal of Aging and Health. 1998;10(3):351–71. doi: 10.1177/089826439801000305. [DOI] [PubMed] [Google Scholar]
- Bourdon T W, Dubin S C. Long-Term Care General Liability and Professional Liability Actuarial Analysis. Chicago: Aon Risk Consultants; 2002. [Google Scholar]
- Centers for Medicare and Medicaid Services. Appropriateness of Minimum Nurse Staffing Ratios in Nursing Homes. Washington, DC: Centers for Medicare and Medicaid Services; 2001. Report to Congress: Phase II, Final. [Google Scholar]
- Chou S Y. “Asymmetric Information, Ownership and Quality of Care: An Empirical Analysis of Nursing Homes.”. Journal of Health Economics. 2002;21(2):293–311. doi: 10.1016/s0167-6296(01)00123-0. [DOI] [PubMed] [Google Scholar]
- Florida Policy Exchange Center on Aging. Choices, Quality & Limiting Litigation: Three Keys to Improving Long-Term Care in Florida. Tampa, FL: The Center; 2001. Staff Report to the Task Force on Availability and Affordability of Long-Term Care in Response to House Bill 1993. [Google Scholar]
- Grabowski D C, Hirth R A. “Competitive Spillovers across Non-Profit and For-Profit Nursing Homes.”. Journal of Health Economics. 2003;22(1):1–22. doi: 10.1016/s0167-6296(02)00093-0. [DOI] [PubMed] [Google Scholar]
- Harrington C, Carrillo H. “The Regulation and Enforcement of Federal Nursing Home Standards, 1991–1997.”. Medical Care Research & Review. 1999;56(4):471–94. doi: 10.1177/107755879905600405. [DOI] [PubMed] [Google Scholar]
- Harrington C, Kovner C, Mezey M, Kayser-Jones J, Burger S, Mohler M, Burke R, Zimmerman D. “Experts Recommend Minimum Nurse Staffing Standards for Nursing Facilities in the United States.”. Gerontologist. 2000;40(1):5–16. doi: 10.1093/geront/40.1.5. [DOI] [PubMed] [Google Scholar]
- Harrington C, Zimmerman D, Karon S L, Robinson J, Beutel P. “Nursing Home Staffing and Its Relationship to Deficiencies.”. Journal of Gerontology. 2000;55B(5):S278–87. doi: 10.1093/geronb/55.5.s278. [DOI] [PubMed] [Google Scholar]
- Hedgecock D K, Oakley M L, Johnson C E, Salmon J R, Polivka L, Hyer K. “Nursing Home Litigation: A Ten-Year Analysis of One Metropolitan Florida County.”. Long-Term Care Interface. 2004;4(11):17–21. [Google Scholar]
- Hedgecock D K, Salmon J R. 2001. “Lawsuits and Liability Insurance Experience of Florida Nursing Homes January–October 5, 2001: Initial Impact of Senate Bill 1202.” Tampa, FL: Florida Policy Exchange Center on Aging.
- Johnson C E, Atherly A, Bunderson J S. “The Many Dimensions of Florida Nursing Home Litigation.”. Long-Term Care Interface. 2000;1(5):42–8. [Google Scholar]
- Johnson C E, Bunderson J S. “Enacting Litigious Environments: Litigation and Florida's Nursing Homes.”. Health Care Management Review. 2002;27(3):7–20. doi: 10.1097/00004010-200207000-00002. [DOI] [PubMed] [Google Scholar]
- Johnson C E, Dobalian A, Burkhard J, Hedgecock D K, Harman J. “Factors Predicting Lawsuits against Nursing Homes in Florida 1997–2001.”. Gerontologist. 2004;44(3):339–47. doi: 10.1093/geront/44.3.339. [DOI] [PubMed] [Google Scholar]
- Johnson C E, Hedgecock D K, Oakley M L, Dobalian A, Salmon J R, Hyer K, Polivka L. 2001. “Predictors of Lawsuit Activity against Nursing Homes in Hillsborough County Florida.”Annual Meeting Proceedings, the Gerontological Society of America, Chicago. [Google Scholar]
- Lapin L. Statistics for Modern Business Decisions. 2d ed. New York: Harcourt Brace Jovanich; 1978. [Google Scholar]
- Newman D K, Palmer M H. “Incontinence and PPS: A New Era.”. Ostomy Wound Management. 1999;45(12):32–8. 40–4, 46 passim. [PubMed] [Google Scholar]
- Polivka L, Dunlop B, Brooks M. Project Two: The Florida Long-Term Care Elder Population Profile Survey. Tampa, FL: Florida Policy Exchange on Aging; 1997. [Google Scholar]
- Spector W D, Selden T M, Cohen J W. “Impact of Ownership Type on Nursing Home Outcomes.”. Health Economics. 1998;7(7):639–53. doi: 10.1002/(sici)1099-1050(1998110)7:7<639::aid-hec373>3.0.co;2-0. [DOI] [PubMed] [Google Scholar]
- Stata. Stata Reference Manual. College Station, TX: Stata Press; 2001. (Release 7). [Google Scholar]
- Stevenson D G, Studdert D M. “The Rise of Nursing Home Litigation: Findings from a National Survey of Attorneys.”. Health Affairs. 2003;22(2):219–29. doi: 10.1377/hlthaff.22.2.219. [DOI] [PubMed] [Google Scholar]
- U.S. General Accounting Office. Nursing Homes: Additional Steps Needed to Strengthen Enforcement of Federal Quality Standards: Report to Congressional Requesters. Washington, DC: U.S. General Accounting Office; 1999. [Google Scholar]
- White H. “A Heteroskedasticity-Consistent Covariance Matrix Estimator and a Direct Test for Heteroskedasticity.”. Econometrica. 1980;48(4):817–30. [Google Scholar]
- Williamson J L. “The Siren Song of the Elderly: Florida's Nursing Homes and the Dark Side of Chapter 400.”. American Journal of Law and Medicine. 1999;25(2):423–43. [PubMed] [Google Scholar]
- Wunderlich G S, Sloan F, Davis C K, editors. Nursing Staff in Hospitals and Nursing Homes: Is It Adequate? Washington, DC: National Academy Press; 1996. [PubMed] [Google Scholar]