Abstract
Objective
To quantify the effects of informal caregiver availability and public funding on formal long-term care (LTC) expenditures in developed countries.
Data Source/Study Setting
Secondary data were acquired for 15 Organization for Economic Cooperation and Development (OECD) countries from 1970 to 2000.
Study Design
Secondary data analysis, applying fixed- and random-effects models to time-series cross-sectional data. Outcome variables are inpatient or home heath LTC expenditures. Key explanatory variables are measures of the availability of informal caregivers, generosity in public funding for formal LTC, and the proportion of the elderly population in the total population.
Data Collection/Extraction Method
Aggregated macro data were obtained from OECD Health Data, United Nations Demographic Yearbooks, and U.S. Census Bureau International Data Base.
Principal Findings
Most of the 15 OECD countries experienced growth in LTC expenditures over the study period. The availability of a spouse caregiver, measured by male-to-female ratio among the elderly, is associated with a $28,840 (1995 U.S. dollars) annual reduction in formal LTC expenditure per additional elderly male. Availability of an adult child caregiver, measured by female labor force participation and full-time/part-time status shift, is associated with a reduction of $310 to $3,830 in LTC expenditures. These impacts on LTC expenditure vary across countries and across time within a country.
Conclusions
The availability of an informal caregiver, particularly a spouse caregiver, is among the most important factors explaining variation in LTC expenditure growth. Long-term care policies should take into account behavioral responses: decreased public funding in LTC may lead working women to leave the labor force to provide more informal care.
Keywords: Long-term care expenditure, spouse caregiver, adult child caregiver, public funding, international comparison
The age distribution of all developed countries, as well as many developing countries, is shifting toward older ages (Kinsella and Velkoff 2001). Declines in fertility combined with rising longevity are expected to increase the proportion of health expenditures devoted to formal long-term care (LTC) (Spillman and Lubitz 2000). Despite the expected increase in LTC expenditure worldwide, few researchers have examined the determinants of LTC expenditure. Much of the literature on the determinants of total health expenditures in developed nations does not distinguish between acute and long-term care (Gerdtham et al. 1992; Barros 1998).
Our study aims to fill the gap in the literature by exploring the effects of informal caregiver availability and generosity in public LTC funding on LTC expenditure among a subset of Organization for Economic Cooperation and Development (OECD) countries. These relatively wealthy nations collect similar aggregate data on key measures of interest, and there is substantial variation over time and across these nations in policies affecting LTC (Anderson and Hussey 2000; Organization for Economic Cooperation and Development 2003). This group of nations is therefore well-suited for a study of the consequences of alternative policies.
We focus on the availability of informal caregivers, because the absence or limited availability of a spouse, child, or other informal caregiver is associated with an increased demand for formal LTC (Coughlin et al. 1992; Miller and Weissert 2000). Informal care, for the purposes of our study, is care provided without payment. One key distinction is that informal care is a much better substitute for LTC than it is for acute medical care.
Demographic, economic, and social factors have obvious and large effects on informal caregiver availability (Miller and Weissert 2000). For instance, if female longevity increases more rapidly than male longevity, women can expect to spend more years in widowhood, without the support of a spouse, leading to greater risk of needing formal LTC (Lakdawalla and Philipson 1999). Similarly, rising divorce rates increase the likelihood of living alone in industrialized countries (Kinsella and Velkoff 2001). Also, as the female labor force participation rate rises or close relatives live farther away, an elderly patient is less able to rely upon an adult child for informal care in OECD countries (Organization for Economic Cooperation and Development 1994).
Our study also focuses on generosity of public funding for LTC through direct government subsidies or through public insurance coverage for formal LTC. More generous public support reduces the price of formal LTC in both absolute terms and relative to the value, or the shadow price, of informal care (Coughlin et al. 1992). Consequently, a public subsidy for formal LTC increases demand for it, even when an informal caregiver is available (Coughlin et al. 1992). Despite this logic, the literature on the effect of public funding on health expenditure is mixed. Some studies suggest that increased formal home care due to generous public funding does not substitute for informal care, but rather supplements or complements it (Kemper 1988; Picone and Wilson 1999). Other studies find a substitution effect (Ettner 1994). While some authors find that increased use of formal home care reduces inpatient LTC (Ettner 1994; Picone and Wilson 1999), other studies report the opposite (Kemper 1988). In the U.S. National Long Term Care Demonstration, additional community care costs were not offset by reductions in inpatient LTC cost (Kemper 1988). Nevertheless, the benefits of formal LTC may outweigh costs if all benefits, including those that accrue over a long time period and to informal caregivers, are counted (Schulz and Beach 1999). Two explanations for the discrepant findings in the literature are that the studies measure outcomes differently, and that they focus on different study populations.
Cross-national time-series data from this set of OECD countries offer at least three advantages for studying the effects of demographic and policy changes on formal LTC use. Our dataset enables us to examine the long-term associations between LTC expenditure growth rates and their determinants over a period of at least a decade. Available nationally representative individual-level data, in contrast, typically offer a much shorter period of follow-up, so the effects of social and demographic change over time are likely to be too small to detect. Second, in this dataset there is substantial variation in informal caregiver availability and public funding for LTC, both across countries and across time, which would not be typical in time-series data set in any one country. Third, confounding variation in access to other services that affect the demand for LTC, such as acute and subacute medical care, is smaller in the selected sample of OECD countries than in a broader international sample (Organization for Economic Cooperation and Development 2003). For instance, there is only minimal variation in access to Alzheimers' disease medications and stroke rehabilitation services—two important determinants of LTC demand.
The purpose of our study is to answer the following questions: (1) To what extent does the availability of an informal family caregiver reduce the formal LTC expenditure? (2) Does generous public funding for LTC increase LTC expenditure growth rates? (3) Are the determinants of LTC utilization similar across nations and over time?
Data
Our analysis relies on nation-level data extracted from OECD Health Data 2003 (OECD 2003), supplemented by demographic data from United Nations Demographic Yearbooks (United Nations 1970–2001) and the U.S. Census Bureau International Data Base (U.S. Census Bureau 2003). We include 15 countries, with data from 1970 to 2000, based on the availability of LTC expenditure information and of male to female population ratios.1
Outcome variables are inpatient LTC and home heath LTC expenditures measured either by dollars per capita—adjusted by purchasing power parity and the U.S. gross domestic product (GDP) deflator (1995=100)—or by percentage of total health expenditures. Key explanatory variables are measured as follows. Following the literature (Lakdawalla and Philipson 1999), we use male-to-female ratios among the elderly to approximate marital status rates; we examine separate male-to-female ratios for populations aged 65 or older, aged 75 or older, and aged 80 or older. Examining separate male-to-female ratios for different age categories permits us to test the hypothesis that the presence of a spouse is more closely associated with decreased LTC expenditures in older populations (Miller and Weissert 2000; Spillman and Lubitz 2000). Table 1 summarizes some descriptive statistics.
Table 1.
Summary Statistics
| Inpatient Long-term Care | Home Long-term Care | |||
|---|---|---|---|---|
| Obs. | Mean (Std Error) | Obs. | Mean (Std Error) | |
| Long-term care expenditure (dollar per capita)¶ | 242 | 140.88 (109.83) | 63 | 47.22 (49.37) |
| Male/female ratio among aged 75+ (%) | 242 | 55.42 (6.89) | 63 | 51.38 (5.64) |
| Male/female ratio among aged 80+ (%) | 242 | 48.40 (6.70) | 62 | 44.36 (4.62) |
| Male/female ratio among aged 65+ (%) | 242 | 68.81 (7.28) | 62 | 65.98 (6.96) |
| Female labor force participation rate (%) | 242 | 50.77 (8.86) | 61 | 49.45 (5.11) |
| Proportion of female in total labor force participation (%) | 242 | 41.81 (4.36) | 63 | 41.67 (2.53) |
| Proportion of full-time among the all employed women (%) | 190 | 72.93 (12.84) | 63 | 68.09 (16.56) |
| Public funding (% Total health expenditure) | 242 | 7.00 (4.49) | 63 | 2.16 (2.36) |
| Proportion of the population aged 65 or older (%) | 242 | 12.73 (2.13) | 63 | 14.37 (1.35) |
| Income (dollar per capita)¶ | 242 | 18,114 (6,088) | 63 | 21,782 (5,688) |
Adjusted by purchasing power parity and the U.S. GDP deflator (1995=100).
To explore whether informal LTC by adult children substitutes for formal LTC, we examine three measures of female labor force participation: participation rates among women aged between 20 and 64, the female percentage of total labor force participation, and the percentage of full-time workers among all employed women. We expect availability of informal LTC to more clearly substitute for institutional than home care, since home health care could be a complement for informal LTC (Picone and Wilson 1999). Furthermore, we expect the effects of an adult child caregiver on LTC utilization to be smaller than those of a spouse caregiver, since the presence of a spouse appears to predict formal LTC utilization more accurately than the presence of an adult child caregiver (Cohen, Tell, and Wallack 1988; Borsch-Supan 1990).
Generosity in public funding for each type of LTC is measured by the ratio of public expenditure per capita for the type of LTC to the total health expenditure per capita.2 Since public funding typically reduces the marginal costs of LTC to families, we hypothesize that higher levels of public funding will be associated with increases in LTC expenditure. We note, however, that the literature's estimates of the effect of public financing on health expenditure is mixed, reflecting differences in outcome measurements and study populations, as described earlier.
The literature on the association between the percentage of the elderly population and health expenditure in OECD countries reports that aging has either insignificant (Barros 1998) or statistically significant, but small, effects (Hitiris and Posnett 1992). We also include income as an explanatory variable because it is the most powerful single factor explaining variation in total health expenditure among OECD nations (Hitiris and Posnett 1992).
Methods
We use fixed-effects (FE) models and random-effects (RE) models as expressed in the equation below, applying the Hausman test to select between them (Greene 1997). Expenditure of a particular type of LTC in country i during year t is represented by Y. In separate analyses, Y is measured either by dollars per capita, or the proportion of total health expenditures attributable to LTC. The proportion of the population that is elderly (65+) is P. The spouse-effect variable (that is, male-to-female ratio among the elderly population) is S, and PF is a vector of variables indicating generosity in public funding for inpatient and home health LTC. A vector of the female labor force indicators and income per capita are FL and X, respectively. Country and year fixed effects are C and T. Both expenditure and income are in logarithmic form, adjusted for inflation and purchasing power parity.
Results
The discussion of our empirical results addresses each of the hypotheses described earlier in turn:
(1) To what extent does the availability of an informal caregiver reduce formal LTC expenditures?
Spouse Caregiver
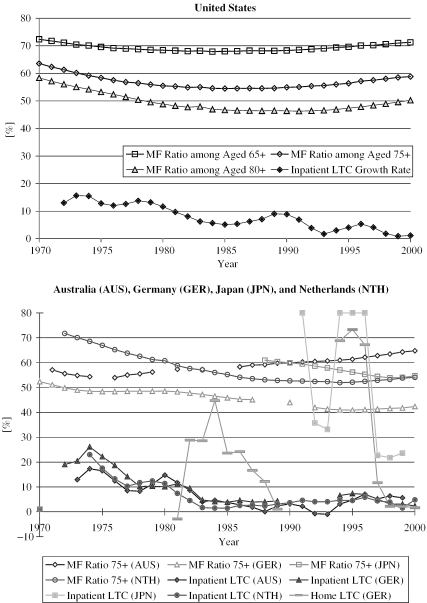
Figure 1 presents trends in elderly male-to-female population ratios alongside LTC expenditure growth rates for the United States and for four typical OECD countries. These countries demonstrate a consistent negative association between inpatient LTC expenditure growth rate and male-to-female (MF) ratio.3 In the United States, for example, the MF ratio declined sharply during the early 1970s, while LTC expenditure increased at a rapid rate: more than 10 percent per year. However, when the MF ratio decreased mildly during the 1980s, the LTC expenditure growth rates decreased as well. But the negative association returned in the 1990s—when the MF ratio increased, inpatient LTC expenditure growth rates declined. LTC expenditure growth rates were most prominently associated with MF among the oldest old (80+) in the U.S., as hypothesized earlier. There was a similar association between MF ratio and LTC growth rates in most of the 15 countries we examined. Figure 1 shows the trends for Australia (◊ for MF Ratio and ♦ for inpatient LTC growth in Figure 1), Japan (□▪), Netherlands (○•) and Germany (▵, ▴ for inpatient LTC growth and — for home LTC growth). The consistently negative association between LTC expenditure growth rate and the MF ratio within countries over time suggests that formal LTC and informal LTC delivered by a spouse are highly substitutable.
Figure 1.
Time Trends of Male-to-Female (MF) Ratio and Long-term Care (LTC) Expenditure Growth Rate (Three-Year Moving Average)
Comparison of Spouse Caregiver and Adult Child Caregiver Availability
Table 2 summarizes our regressions analyzing inpatient (Models 1–4) and home (Models 5–6) LTC expenditures in 15 OECD nations between 1970 and 2000. While Model 1 includes a simple measure of female labor force participation rate, Model 2 distinguishes between full-time and part-time status among employed women, and is our preferred model for inpatient LTC expenditures. Models 3 and 4 test how changing the age cutoff in the measurement of male-to-female ratio affects our results. Models 5 and 6 analyze the determinants of home LTC expenditures. Model 5 includes the limited number of available observations from the 1980s, while Model 6 includes observations from the 1990s only.
Table 2.
Determinants of Long-term Care Expenditure in 15 OECD Countries from 1970 to 2000
| Model 1 | Model 2: Final Model | Model 3 | Model 4 | Model 5 | Model 6: Final Model | |
|---|---|---|---|---|---|---|
| Inpatient Long-term Care Expenditure | Home Long-term Care Expenditure | |||||
| Outcome (Dollars per Capita)¶Period | 1970–2000 | 1976–2000 | 1980–2000 | 1990–2000 | ||
| MF Ratio among Aged 75+ (%) | −0.046 | −0.063 | −0.306 | −0.217 | ||
| (0.009)** | (0.012)** | (0.056)** | (0.054)** | |||
| MF Ratio among Aged 80+ (%) | −0.046 | |||||
| (0.011)** | ||||||
| MF Ratio among Aged 65+ (%) | 0.015 | |||||
| (0.022) | ||||||
| Female Proportion in Total LFP (%) | −0.0969 | 0.0169 | 0.0247 | 0.0443 | −0.0749 | 0.1113 |
| (0.0368)** | (0.0226) | (0.0260) | (0.0330) | (0.0861) | (0.1033) | |
| Female LFP Rate (%) | 0.037 | |||||
| (0.019) | ||||||
| Full-time Employed Women (%)§ | 0.046 | 0.059 | 0.071 | 0.090 | 0.086 | |
| (0.011)** | (0.012)** | (0.015)** | (0.030)** | (0.035)* | ||
| Public Funding: Inpatient LTC (%) | 0.137 | 0.222 | 0.226 | 0.230 | −0.201 | −0.141 |
| (0.025)** | (0.020)** | (0.023)** | (0.025)** | (0.144) | (0.124) | |
| Public Funding: Home LTC (%): | 0.301 | 0.416 | ||||
| (0.066)** | (0.069)** | |||||
| Aged 65+ in Total Population (%) | 0.164 | 0.280 | 0.317 | 0.381 | 0.313 | 0.417 |
| (0.043)** | (0.045)** | (0.048)** | (0.051)** | (0.239) | (0.205) | |
| Income per Capita (dollar per capita)¶ | −0.897 | 1.910 | 1.583 | 2.265 | −3.347 | −1.688 |
| (0.561) | (0.475)** | (0.587)** | (0.614)** | (1.416)* | (1.366) | |
| Country/Obs. | 15/242 | 15/189 | 15/190 | 15/188 | 8/63 | 8/53 |
| Estimation Model | RE | FE | FE | FE | FE | FE |
Adjusted by purchasing power parity and the U.S. GDP deflator (1995=100), in natural log.
Proportion of full-time among all employed women.
MF ratio: Male-to-Female ratio, LFP: Labor Force Participation, LTC: Long-term Care, RE: Random Effects Models, FE: Fixed Effects Models.
Standard errors in parentheses,
Significant at 5%;
Significant at 1%.
Estimated coefficients of country and year fixed variables, included in all models, are available on request.
In Table 2, aging is positively associated with LTC expenditure. For instance, a one-percentage-point increase in the proportion of the population aged 65 or older is associated with a 28 percent and 42 percent increase in inpatient LTC and home LTC expenditure, respectively. The income elasticity of LTC expenditure varies across models, and does not have a consistent sign.
In order to evaluate the effects of the three informal caregiver measures on inpatient LTC presented in Model 2 in Table 2, we explore three scenarios. In each, we change the proxy measure of caregiver availability under consideration by one percentage point (equivalent to one thousand in absolute number of informal caregivers) in a single year and in a hypothetical country where all other variables take a mean value. Under the first scenario, we increase the number of males elderly aged 75 or older by 1,000 (e.g., from 55,000 to 56,000) while the number of females in that age group remains at 100,000. For a country at the mean MF ratio of 55 percent, this amounts to a one-percentage-point increase in the MF ratio. Our model implies that such a change in the population would reduce the inpatient LTC expenditures by 6.3 percent. At the sample mean of the variables in our regression, this amounts to $28,840 per year per elderly male.4
In the second scenario, we envision 1,000 women between 20 and 64 years old entering the labor force, and hence increasing the proportion of women in total labor force participation by one percentage point. Our model predicts that these 1,000 women will raise the inpatient LTC growth rate by 1.7 percent and thus increase the inpatient LTC expenditure by $310 per year per woman entering labor force.5 Similarly, our third scenario envisions 1,000 employed women shifting from part-time to full-time work in one year. The reduced availability of potential adult child caregivers in this scenario would raise inpatient LTC expenditure by $3,830 dollar per woman shifting to full-time work.6 The magnitudes of these factors on home LTC expenditure are summarized in Table 3.
Table 3.
Comparison of Informal Caregiver's Impact on Long-term Care (LTC) Expenditure in 15 OECD Countries
| Inpatient LTC Expenditure | Home LTC Expenditure | |
|---|---|---|
| 1976–2000 | 1990–2000 | |
| 15 Countries | 8 Countries | |
| (N=189) | (N=53) | |
| Model 2 in Table 2 | Model 6 in Table 2 | |
| Expenditure per Capita (General Population) | $163 | $51 |
| Spouse Caregiver Availability | ||
| Scenario 1 in Text: One Male Survives to Age 75 | (−) $28,840 | (−) $27,020 |
| Adult Caregiver Availability | ||
| Scenario 2 in Text: One Woman (Aged between 20 and 64) Entering Labor Force | (+) $310 | (+) $650 |
| Scenario 3 in Text: One Woman (Aged between 20 and 64) Shifting from Part-time to Full-time Employment | (+) $3,830 | (+) $2,290 |
Note: All dollar values adjusted by purchasing power parity and the U.S. GDP deflator (1995=100). All variables in the models are assumed to take the mean value of an estimation model's sample.
As Table 3 shows, the presence of a spouse caregiver is expected to have a large impact on LTC expenditure—more than seven times as large as that of a younger woman shifting between full-time and part-time employment. The impact of the change in female labor force participation is statistically insignificant and much smaller than the effect of a shift in full-time/part-time status. The impacts of informal caregiver availability on home LTC expenditure are comparable in magnitude to those on inpatient LTC expenditure.
(2) Does generous public funding for LTC increase LTC expenditure growth rates?
As hypothesized, generous public funding is positively associated with LTC expenditure. For instance, a one-percentage-point increase in the proportion of public expenditure for inpatient LTC out of total health expenditure is associated with a 22 percent increase in inpatient LTC expenditure (Table 2, Model 2). A comparable increase in the generosity of public funding for home care, say, from 2 percent to 3 percent, would raise this component of LTC expenditure by 42 percent (Table 2, Model 6). The negative but statistically insignificant association between home LTC expenditures and the generosity of public funding for inpatient LTC hints but does not establish that home LTC substitutes for inpatient LTC (Table 2).
(3) Are the determinants of LTC utilization similar across nations and over time?
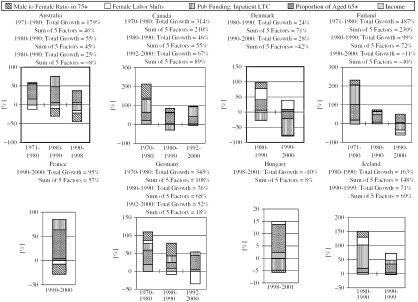
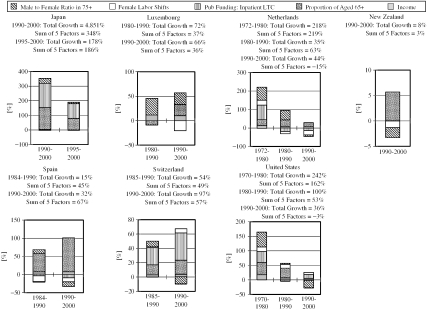
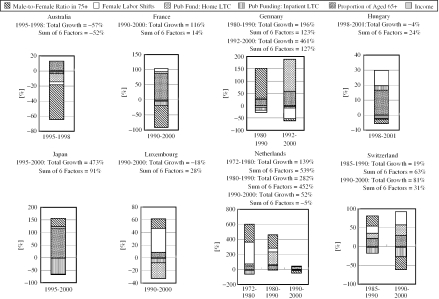
In Figure 2, we decompose growth rates in LTC expenditure during each decade based on the Table 2 (Models 2 and 6) results. For inpatient LTC expenditures, there were data available from 15 OECD countries, while for home LTC expenditures, there were data available from 8 OECD countries. In calculating the decomposed effects, we make imputations of missing values of variables, based on the linear approximation of available values.7 There were no missing values for the LTC variables.
Figure 2.
Decomposed Growth in Inpatient Long-term Care Expenditure
Inpatient LTC expenditure increased 242 percent from 1970 to 1980 in the United States. The reduction in the availability of a spouse caregiver is responsible for a 51 percent increase in the growth rate, accounting for about one-fifth of the total increase during the 1970s.8 The combined effect of the two female labor force participation (FLFP) measures in Table 2's Model 2 contributed to a 15 percent increase in the growth rate. The effects of public funding and the proportion of elderly were 37 percent and 42 percent respectively during the same period. “Sum of 5 factors” indicates that Model 2 explained approximately two-thirds of the total increase in the United States during the 1970s. Two FLFP variables out of six variables in Model 2 were aggregated into one factor in Figure 2.
These bar charts also indicate that the growth rate in total inpatient LTC expenditure between 1970 and 2000 steadily declined in the United States from around 242 percent to 36 percent. A substantial part of this decline is attributable to changes in spouse availability. That is, the presence of a spouse accounted for a 51 percent increase in the expenditure growth rate during the 1970s, a 3 percent increase during the following decade, and a 25 percent decrease during the last decade. In addition, the reduction in the proportion of aged 65 or older contributed to the decrease in the total growth rates in the United States during the 1990s compared to earlier decades.
The impact of the explanatory factors on LTC expenditures varies across countries and across time within a country (Figures 2 and 3). Most countries experienced growth in LTC expenditures in each decade studied, with an increase in the proportion of the population aged 65 or older a major factor in this growth. The effects of informal caregiver availability and public funding generosity on inpatient and home health LTC expenditures are more variable than population aging.
Figure 3.
Decomposed Growth in Home Long-term Care Expenditure
Discussion
Our analysis demonstrates that in this set of 15 OECD countries, formal and informal LTC serve as close substitutes, similar to findings in other settings (Miller and Weissert 2000).
The availability of a spouse, measured by male-to-female ratio, is negatively associated with formal LTC expenditure growth, as a past study of the U.S. data reported (Lakdawalla and Philipson 1999). The largest effects of MF ratio on inpatient LTC expenditures arise in models where the MF ratio is measured for the 75+ population. Models that measure the MF ratio using the 65+ and the 80+ populations demonstrate smaller effects on inpatient expenditures (Models 3 and 4 in Table 2). These empirical results could be explained by the two opposing influences of aging on the demand and supply of spouse caregivers. When one gets older and more frail, one is less likely to provide informal care for one's spouse, and this diminishes the effect of the MF ratio on expenditures. At the same time, when one gets older, one is more likely to demand informal care, and this raises the MF ratio's effect. Thus, the attenuated effect of this ratio when measured using the 65+ population is likely caused by lower demand, while the attenuated effect when measured using the 80+ population is likely caused by the decreased ability of spouses to care for each other at those advanced ages.
The $28,000 per person-year effect on LTC expenditures of having one potential male elderly caregiver available (Table 3) is comparable to the average annual U.S. Medicaid reimbursement for a resident of an Intermediate Care Facility, which was $21,350, also in 1995 dollars (Swan et al. 1993).9 The availability of a child caregiver has a small effect, perhaps because children are less likely to live with an elderly parent than is a spouse. Previous studies have also shown that child caregivers have a smaller effect (Cohen, Tell, and Wallack 1988; Borsch-Supan 1990).
The unexpected negative association between the proportion of women in the labor force and LTC expenditures (Model 1 in Table 2) may reflect two phenomena. First, the female labor force is heterogeneous. If working women shift from full-time work to part-time work in order to provide care for elderly family members, the rise in the number of part-time working women will be negatively associated with formal LTC. Alternatively, when a woman starts a full-time job and can no longer care for her elderly relatives, the increase in the number of full-time women will be positively associated with formal LTC. Second, behavioral responses may have large effects. If decreased public funding leads some working women to exit the labor force in order to provide care for elderly relatives, decreased tax revenues from these women may further reduce public funding. This behavioral response means that the positive associations we find between generous public funding and LTC expenditures do not necessarily imply additional LTC expenditures by households who provide informal care.
The large positive associations between public funding and LTC expenditures presented in Tables 2 may be upwardly biased because unmeasured features of health policy may increase both public funding and the outcome variable; public LTC expenditure is a component of public funding as well as the outcome variable defined earlier. This endogeneity problem is hard to address with the available data. Our measure of public funding, however, avoids the pitfall that other studies fall into because we do not measure public expenditure as public expenditures divided by the outcome variable (Gerdtham et al. 1992; Barros 1998). The negative association that these studies report between their public funding variable and total health expenditures may be a mechanical consequence of including an explanatory variable that is inversely proportional to the outcome variable.
One study (Hitiris and Posnett 1992) reported that a one-percentage-point increase in the proportion of the population aged 65 or older is associated with 6.5 percent increase in total health expenditure. In our analysis, the same unit of the elderly population increase would increase inpatient LTC expenditure by 28 percent (in Model 2 in Table 2) and home LTC by 42 percent (in Model 6 in Table 2). These estimated effects on home LTC expenditure were at best marginally significant (p=0.052 in Model 6). Expenditures for home care rise more sharply with increases in the size of the elderly population than do other components of health expenditures. These findings are consistent with studies analyzing micro-data for the U.S. population (Spillman and Lubitz 2000).
The income elasticity estimates for LTC expenditure are inconsistent in sign, significance level, and magnitude. This is likely a consequence of measurement error and insufficient variation in this sample of high-income countries. Our estimates range from 1.91 to 2.27 when statistically significant. The point estimate is consistent with the literature—one study estimated an income elasticity of 2.27 for nursing home expenditure using state aggregated data (Scanlon 1980).
Our decomposition of the sources of LTC expenditure growth in the U.S. correspond with Lakdawalla and Philipson's (1999) results on how changes in the size of the elderly population and the availability of a spouse affected inpatient LTC utilization growth during the 1970s and 1980s. Their outcome variable, measured at the county level, is the number of residents in nursing homes in the United States.
Our study has several important limitations. First, we examine a limited number of countries over a limited time period. The small sample size allows us to control only for a small number of variables, and the use of national data precludes examination of within-country heterogeneity, such as provincial and state characteristics. The inclusion of health status measures may have improved the accuracy of our results, although variations in health status are mostly absorbed by year and country fixed effects. Moreover, because few consistently measured health-related variables were available, including them in the analyses would reduce the number of countries and observations in the analyses and hence reduce the external validity of these analyses. Despite these limitations, our results are robust to a number of different empirical design decisions (such as measuring LTC expenditures as a proportion of total expenditure), and largely consistent with the American literature and the literature using aggregate international data. Our results expand on previous analyses by including important explanatory variables, in an international setting, like MF ratio, female labor force attachment, and public expenditures that received less attention than population aging in literature.
Policy Implications
In the past decade, while the male-to-female ratio among the elderly has changed in most countries, there has not been a consistent pattern. In some countries, like Germany and Japan, MF ratio declined, while in others such as the United States, Australia, and Netherlands it increased. The demographic literature predicts, however, that over the next 30 years, the MF ratio among the elderly will rise toward one in the developed world, while it will fall in the developing world (Kinsella and Velkoff 2001). Our results demonstrate that changes in this ratio are important predictors of the demand for long-term care. One is tempted to conclude that these demographic trends will mitigate the increase in long-term care demand caused by population aging in the developed world.
It is important to remember, however, that MF ratio is actually a proxy variable designed to measure the level of support that the elderly have available from their immediate family. Despite the rising MF ratio among the developed nations, the ability of elderly couples to take care of themselves, and thus avoid use of formal long-term care, may be limited. The proportion of the elderly population that is divorced or separated, childless, or that have working daughters and daughter-in-laws, are all rising in industrialized nations (Kinsella and Velkoff 2001; Organization for Economic Cooperation and Development 2003). While disability rates among the elderly have been declining in the past decades (Manton and Gu 2001), the declines are predominantly in the higher-level instrumental activity of daily living (IADLs) rather than in basic functioning activity of daily living (ADLs). Furthermore, it is not clear that such trends will continue (Lakdawalla et al. 2003). Therefore, the fraction of elderly living alone (Kinsella and Velkoff 2001) or with spouses unable to provide needed care may rise in the future. The optimal public policy response will require accounting for the shifting demographic and economic trends in elderly living arrangements.
Our results have important implications for the measurement of moral hazard caused by public funding of formal LTC. The literature examining how public funding affects the demand for long-term care has emphasized the incentives that such funding creates for overuse of long-term care facilities and formal home care. In Japan, some studies (Shimizutani and Noguchi 2003) imply that increases in public generosity for long-term care can lead to increases in the unnecessary use of services. In the United States, several authors argue that increases in Medicaid and Medicare funding for home care have led to increased long-term care utilization (Ettner 1994; Welch, Wennberg and Welch 1996). Our results suggest that the failure to include important demographic controls, such as the MF ratio, can lead to an overestimate of the effect of public funding on formal long-term care expenditures.
Finally, our findings suggest that projections of future long-term care demand should distinguish between female part-time and full-time work. While the literature tends to find that higher female labor force participation increases formal LTC utilization (Doty, Jackson, and Crown 1998), most studies ignore the full-time/part-time distinction. Our results indicate that if increases in female labor force participation are primarily in part-time work, formal sector LTC expenditures would decrease, while if increases are primarily in full-time work, formal sector LTC expenditures would increase, as the literature suggests. This distinction will also be important in future work examining how changes in public funding for LTC affect the female labor supply. Although the conventional wisdom suggests that decreases in public funding will lead to an increase in informal elderly care by women exiting the labor force, it seems plausible that decreases in public funding would induce women to shift from full-time to part-time work.
Acknowledgments
The authors are grateful to Sara Singer for her comments, and to Katherine B. Harrington and Sarah Oh for their excellent research assistance.
Footnotes
Data availability for inpatient LTC expenditure: Australia (1971–2000), Canada (1970–2000), Denmark (1980–2000), Finland (1970–2000), France (1990–2000), Germany (1970–1990, 1992–2000), Hungary (1998–2000), Iceland (1980–1999), Japan (1988–2000), Luxembourg (1980, 1985, 1990–1993, 1999–2000), Netherlands (1972–2000), New Zealand (1991–1992), Spain (1984–2000), Switzerland (1985–2000), and United States (1970–2000). Data availability for Home LTC expenditure: Australia (1974, 1989, 1995–1998), France (1990–2000), Germany (1970–1990, 1992–2000), Hungary (1998–2000), Japan (1995–2000), Luxembourg (1980, 1985, 1990–1993, 1999–2000), Netherlands (1972–2000), and Switzerland (1985–2000). Note the break in the German data; data up to 1990 refers to the former Federal Republic of Germany, while data from 1992 onward corresponds to reunified Germany (Organization for Economic Cooperation and Development 2003).
Our dataset defines “public expenditure” as follows: “Expenditure incurred by public funds. Public funds are state, regional, and local government bodies and social security schemes. Public capital formation on health includes publicly financed investment in health facilities plus capital transfers to the private sector for hospital construction and equipment” (Organization for Economic Cooperation and Development 2003).
For all countries except the United States in Figure 1, three-year moving average was used for LTC expenditure growth rate to follow the time trends easily. Japan's expenditure growth rates were capped at 80 when greater than 80, that is, 90 (1991), 178 (1994), 178 (1995), and 175 (1996).
$28,840=$163*155,000*(1/0.0552)*6.3%*(1/1000)=(expenditure per capita general population)*(Total number of aged 75 or older in this scenario)*(inverse of the proportion of the aged 75 or older: to inflate to the general population)*(estimated effect of a male elderly spouse in Model 2 in Table 2)*(inverse of the 1,000 males surviving to age 75).
F and M indicate female and male labor force participation in absolute number respectively. F/(F+M)=0.43 and (F+1000)/(F+1000+M)=0.44 lead to (F+M)=56,000=Total labor force in a hypothetical nation. Since the average labor force participation rate is 49.7 percent in our sample, the total population is 112,680 (=56,000*[1/0.497]). The estimated LTC expenditure reduction per one working woman is $163*112,680*(1.69%)*(1/1000 women entering labor force)=$310.
F and P represent full-time and part-time employed women in absolute number. F/(F+P)=0.65, (F+1000)/(F+1000+P-1000)=0.66, and hence (F+P)=100,000, given total employed women are constant in number. Since the average female employed among the total employed, and the average proportion of the total employed in the entire population are 42.6 percent and 45.9 percent respectively, the total population is 5.1142*(10^5) (=100,000*[1/0.426]*[1/0.459]). The estimated LTC expenditure reduction per one working woman is $163*5.1142*(10^5)*(4.6%)*(1/1000 women shifting from full-time to part-time)=$3,830.
For instance, one variable's value is missing in 1990 and available in 1985 and 2000 for the same country. The value for 1990 was calculated as the weighted average, (2/3)*(value in 1985) + (1/3)*(value in 2000). Further, imputing these weighted average values uses three-year moving average for (value in 1985) and (value in 2000), provided values in 1984–1986 and 1999–2001 are available. When data availability is too limited to impute, we assumed there is no change in the variable during an evaluation period.
Effect of male-to-female ratio (MFR) on inpatient LTC growth rate from 1970 to 1980 in the U.S. in Figure 2 is based on coefficients in Model 2 in Table 2.=50.8%=100%*([MFR in US in 1980]−[MFR in US in 1970])*(Coefficient of MFR)=100%*([55.47%]−[63.54%])*(−0.063).
Swan and colleagues (1993) reported the mean per diem reimbursement rate was $44.17 in 1989 (in 1983–1984 dollar) based on 50 state Medicaid programs in the United States, weighting each state for its bed stock, and that was converted to $58.5 (in 1995 dollar) when adjusted by the U.S. GDP deflator in our dataset. Consequently, the annual reimbursement rate=$21,350=365 (days)*$ 58.5 (per diem).
This research grew from a project funded in part by the Stanford Institute of International Studies (SIIS) Bechtel Initiative Program and by NIA grant AG-05842 in support of the Center on the Demography and Economics of Health and Aging at Stanford University. Additional funding came from NIA Grant AG-17253 and from the “Comparative Health Care Policy Research Support” project of the Asia-Pacific Research Center in SIIS.
References
- Anderson G, Hussey P. “Population Aging: A Comparison among Industrialized Countries.”. Health Affairs (Millwood) 2000;19(3):191–203. doi: 10.1377/hlthaff.19.3.191. [DOI] [PubMed] [Google Scholar]
- Barros P. “The Black Box of Health Care Expenditure Growth Determinants.”. Health Economics. 1998;7(6):533–44. doi: 10.1002/(sici)1099-1050(199809)7:6<533::aid-hec374>3.0.co;2-b. [DOI] [PubMed] [Google Scholar]
- Borsch-Supan A. “A Dynamic Analysis of Household Dissolution and Living Arrangement Transitions by Elderly Americans.”. In: Wise D, editor. Issues in the Economics of Aging. Chicago and London: National Bureau of Economic Research Project Report, University of Chicago Press; 1990. pp. 89–119. [Google Scholar]
- Cohen M, Tell E, Wallack S. “The Risk Factors of Nursing Home Entry among Residents of Six Continuing Care Retirement Communities.”. Journal of Gerontology. 1988;43(1):S15–21. doi: 10.1093/geronj/43.1.s15. [DOI] [PubMed] [Google Scholar]
- Coughlin T, McBride T, Perozek M, Liu K. “Home Care for the Disabled Elderly: Predictors and Expected Costs.”. Health Services Research. 1992;27(4):453–79. [PMC free article] [PubMed] [Google Scholar]
- Doty P, Jackson M E, Crown W. “The Impact of Female Caregivers'Employment Status on Patterns of Formal and Informal Eldercare.”. Gerontologist. 1998;38(3):331–41. doi: 10.1093/geront/38.3.331. [DOI] [PubMed] [Google Scholar]
- Ettner S. “The Effect of the Medicaid Home Care Benefit on Long-Term Care Choices of the Elderly.”. Economic Inquiry. 1994;32(1):103–27. [Google Scholar]
- Gerdtham U, Sogaard J, Anderson F, Jonsson B. “An Econometric Analysis of Health Care Expenditure: A Cross-section Study of the OECD Countries.”. Journal of Health Economics. 1992;11(1):63–84. doi: 10.1016/0167-6296(92)90025-v. [DOI] [PubMed] [Google Scholar]
- Greene W. Econometric Analysis. New Jersey: Prentice-Hall, Inc; 1997. pp. 632–33. [Google Scholar]
- Hitiris T, Posnett J. “The Determinants and Effects of Health Expenditure in Developed Countries.”. Journal of Health Economics. 1992;11(2):173–81. doi: 10.1016/0167-6296(92)90033-w. [DOI] [PubMed] [Google Scholar]
- Kemper P. “The Evaluation of the National Long Term Care Demonstration.”. Health Services Research. 1988;23(1):161–74. [PMC free article] [PubMed] [Google Scholar]
- Kinsella K, Velkoff V A. An Aging World: 2001. Washington, DC: U.S. Government Printing Office; 2001. pp. 57–84. U.S. Census Bureau, Series P95/01-1, pp. 7–22. [Google Scholar]
- Lakdawalla D, Goldman D, Bhattacharya J, Hurd M, Joyce G, Panis C. “Forecasting the Nursing Home Population.”. Medical Care. 2003;41(1):8–20. doi: 10.1097/00005650-200301000-00003. [DOI] [PubMed] [Google Scholar]
- Lakdawalla D, Philipson T. Cambridge, MA: National Bureau of Economic Research; 1999. “Aging and the Growth of Long-Term Care.”. Working paper no. 6980. [Google Scholar]
- Manton K G, Gu X. “Changes in the Prevalence of Chronic Disability in the United States Black and Nonblack Population above Age 65 from 1982 to 1999.”. Proceedings of the National Academy of Sciences of the United States of America. 2001;98(11):6354–9. doi: 10.1073/pnas.111152298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller E, Weissert W. “Predicting Elderly People's Risk for Nursing Home Placement, Hospitalization, Functional Impairment, and Mortality: A Synthesis.”. Medical Care Research and Review. 2000;57(3):259–97. doi: 10.1177/107755870005700301. [DOI] [PubMed] [Google Scholar]
- Organization for Economic Cooperation and Development (OECD) OECD Health Data 2003: A Comparative Analysis of Thirty Countries. Washington, DC: OECD Information Center; 2003. [Google Scholar]
- Organization for Economic Cooperation and Development (OECD) New Orientations for Social Policy. Paris: OECD; 1994. “The Care of Frail Elderly People: The Social Policy Issues.”; pp. 37–50. [Google Scholar]
- Picone G, Wilson R. “Medicare Home Health Agency Utilization, 1984–1994.”. Inquiry. 1999;36(3):291–303. [PubMed] [Google Scholar]
- Scanlon W J. “A Theory of the Nursing Home Market.”. Inquiry. 1980;17(1):25–41. [PubMed] [Google Scholar]
- Schulz R, Beach S. “Caregiving as a Risk Factor for Mortality: The Caregiver Health Effects Study.”. Journal of the American Medical Association. 1999;282(23):2215–9. doi: 10.1001/jama.282.23.2215. [DOI] [PubMed] [Google Scholar]
- Shimizutani S, Noguchi H. 2003. “Long-term Projection of Demand for At-home Care Services in Japan.”. Economics and Social Research Institute Discussion Paper Series no. 60. Tokyo: Japan Cabinet Office. [Google Scholar]
- Spillman B, Lubitz J. “The Effect of Longevity on Spending for Acute and Long-term Care.”. New England Journal of Medicine. 2000;342(19):1409–15. doi: 10.1056/NEJM200005113421906. [DOI] [PubMed] [Google Scholar]
- Swan J, Harrington C, Grant L, Luehrs J, Preston S. “Trends in Medicaid Nursing Home Reimbursement: 1978–89.”. Health Care Financing Review. 1993;14(4):111–32. [PMC free article] [PubMed] [Google Scholar]
- U.S. Census Bureau, Dept. of Commerce. 2003. International Data Base [accessed on September 1, 2003 and February 1, 2004]. Available at: http://www.census.gov/ipc/www/ibdsprd.html.
- United Nations, Department of Economic and Social Affairs. Demographic Yearbook. New York: United Nations; 1970–2001. [Google Scholar]
- Welch H G, Wennberg D E, Welch W. “The Use of Medicare Home Health Care Services.”. New England Journal of Medicine. 1996;335(5):324–9. doi: 10.1056/NEJM199608013350506. [DOI] [PubMed] [Google Scholar]