Abstract
Objective
To evaluate the association between past 30-day use of alcohol, marijuana, and other illicit drugs and past year unmet need for and use of mental health care.
Data Source
A subsample of 18,849 respondents from the 2001 National Household Survey on Drug Abuse and the 2002 National Survey on Drug Use and Health. Subjects were between the ages of 18 and 65 years and had least one past year mental disorder symptom and no past year substance dependency.
Study Design
Logistic regressions of past 30-day substance use on past 12-month unmet need for mental health care and past 12-month use of mental health services controlling for clinical and sociodemographic characteristics. Predicted probabilities and corresponding standard errors are reported.
Principal Findings
Use of illicit drugs other than marijuana increased with unmet need for mental health care (4.4 versus 3.2 percent, p=.046) but was not reduced with mental health-care use. Heavy alcohol use was not associated with increased unmet need for mental health care, but was higher among individuals with no mental health care use (4.4 percent versus 2.7 percent, p<.001). By contrast, marijuana use did not appear associated with either unmet need or mental health care use.
Conclusions
Substance use varies with past year unmet need for mental health care and mental health care use in ways consistent with the self-medication hypothesis. Results suggest that timely screening and treatment of mental health problems may prevent the development of substance-use disorders among those with mental disorders. Further research should identify subgroups of individuals for whom timely and appropriate mental health treatment would prevent the development of substance-use disorders.
Keywords: Co-occurring disorder, unmet need, perceived need, mental health care, substance use, marijuana, illicit drugs, alcohol, self-medication, logistic regression
The high rate at which mental and substance-use disorders occur together has been well documented in epidemiological and clinical studies (Regier and Farmer 1990; Kessler, Nelson et al. 1996). For example, in the National Comorbidity Study, 51 percent of those who met criteria for a substance disorder at some time in their life also met criteria for a mental disorder at some point, and in the large majority of cases individuals reported that the mental disorder preceded the substance disorder (Kessler et al. 1996). Researchers and clinicians have advanced a number of theories to explain the high rates of co-occurrence. One prominent explanation for the high rates of co-occurrence is that individuals use psychoactive substances to “self-medicate” painful or disturbing psychiatric symptoms (Khantzian 1997; Chilcoat and Breslau 1998; Strakowski and DelBello 2000). Other theories suggest that substance-use disorders cause mental health problems or that substance use and mental health problems have common underlying genetic and environmental causes (Chilcoat and Breslau 1998).
Understanding the underlying causes of co-occurrence is important for improving the treatment and prevention of mental health and substance-use problems. If self-medication is common, then timely screening and treatment of mental health problems may prove the key in preventing the onset of substance-use disorders among the population with mental disorders. Although predictions about the substitutability of psychoactive substances and mental health care are implicit in the self-medication hypothesis, they have gone unexplored in the health services literature.
At the same time, empirical tests of the self-medication hypothesis in the clinical and epidemiological literatures have produced largely equivocal results (Khantzian 1997; Chilcoat and Breslau 1998; Raimo and Schuckit 1998; Dixit and Crum 2000; Strakowski and DelBello 2000). Here, mental health symptoms that pre-date the onset of substance use disorders are considered evidence of self-medication. With the exception of several studies based on long-term follow-up of longitudinal cohorts (Chilcoat and Breslau 1998; Vaillant 1998), study designs have been less than ideal, relying on the long-term recall of highly selected samples of patients with advanced substance-use disorders. In clinical interviews, patients may not accurately recall the temporal sequence of the onset of mental health symptoms and substance-use disorders. Further, among patients who did not confuse the temporal sequencing, advanced substance abuse may have exacerbated mental health symptoms.
This study tests for the presence of behavior consistent with self-medication by examining the relationships between drug and alcohol use and perceptions of unmet need for mental health care and use of mental health care. Specifically, we hypothesize that (1) unmet need for mental health care is associated with higher rates of substance use and (2) the mental health care is associated with lower rates of substance use, controlling for clinical and demographic characteristics.
To test these hypotheses, we pool data from the 2001 and 2002 waves of the National Household Survey on Drug Abuse (NHSDA) (renamed the National Survey on Drug Use and Health [NSDUH] in 2002). These data are well structured to identify patterns of substance use that are consistent with self-medication in several important respects. First, we have a reasonable degree of confidence that measured mental health care use and need precede our substance-use measures in time, because mental health care use and need are measured over the past year and substance use is measured in the past month. Second, our data contain a sufficient sample size and clinical symptom measures to eliminate individuals with substance dependence from our analyses. This exclusion makes it possible to isolate a subpopulation where self-medicating behavior, to the extent it occurs, is least likely to be confounded by mental disorders brought about by established substance-use disorders. Third, the large sample size also allows us to examine separately alcohol, marijuana, and other illicit drugs. This is important because these substances vary not only in terms of their psychoactive properties, but also in terms of the risks and costs associated with their use.
Conceptual Framework
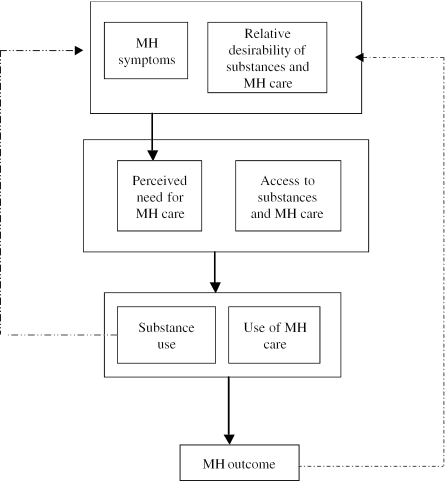
Central to the idea of self-medication is the notion that individuals with mental disorders perceive their symptoms as treatable and act purposefully to mitigate them through the use of substances and/or professionally sanctioned mental health care. Figure 1 illustrates the key relationships among the factors that influence the relative use of mental health care and substances to treatment mental health symptoms. In this context, the relative desirability will be influenced by preferences and beliefs about the relative effectiveness, health, and legal risks associated with substance use, resulting side-effects, and social acceptability of mental heath care and substance use. It is important to emphasize the notion of relative because both substance use and mental health care use are perceived as stigmatizing behaviors—but not necessarily equally so. Notions about relative desirability are formed through one's own experiences (indicated by the dashed arrow from mental health outcomes to desirability in Figure 1), learning through the experiences and opinions of others, and from formal sources of information, such as substance abuse prevention campaigns or programs promoting mental health screening. At the same time, the relative desirability of substance and mental health care use is moderated by access. In the case of mental health care, access is driven by the out-of-pocket cost of care determined by the existence and generosity of health insurance coverage, and the availability of willing providers. While alcohol is widely available to individuals over 21 years of age, safe access to illicit drugs requires a network of social relationships.
Figure 1.
Factors Influencing Perceived Need for Mental Health Care, Use of Mental Health Care, and Substance Use
Applying this framework to our data, we expect substance use to be more common among those with unmet need for mental health care. This group perceives need for care, but have found care either unavailable or rendered care unacceptable. Because of this unmet need, they may be more likely to perceive substance use as relatively more desirable compared with their less needy counterparts. We expect mental health care use to reduce substance use. This can occur in two ways in our model. First, mental health care may alleviate symptoms, mitigating the perceived need to self-medicate. Second, mental health care can change beliefs about the effectiveness of and risks associated with substance use causing patients to re-evaluate their decisions to use substances. For example, mental health care providers may warn patients that use of alcohol would only worsen anxiety or depression problems.
It is widely recognized that frequent and prolonged substance use can produce or exacerbate mental disorders, regardless of whether substance use was initiated for the purpose of self-medication (Popkin and Tucker 1992; Schuckit et al. 1997). (See dashed arrow from substance use to mental health symptoms in Figure 1.) Thus, for the subpopulation with established use disorders, substance use, and mental health care use are likely to be positively correlated, potentially confounding the measured association between substance use and mental health care use. To reduce this potential source of bias, we exclude individuals with past year substance dependencies from our study.
Data Source
Sample
In order to increase the statistical power to detect true differences in substance use across subgroups, we combine waves of the 2001 NHSDA and the renamed 2002 NSDUH (formally called NHSDA). The Substance Abuse and Mental Health Services Administration conducts this survey annually for the primary purpose of estimating the prevalence of illicit drug, alcohol, and tobacco use in the United States (SAMHSA 2003). The pooled sample includes 137,055 respondents aged 12 years and older and has an average response rate of 75 percent (SAMHSA 2002; 2003).
The survey takes roughly 1 hour to complete. To assure confidentiality, questions about substance use, mental health problems, and treatment are completed through audioassisted interview technology (ACASI) where respondents key their responses directly into a laptop computer. Remaining questions are completed through a computer-assisted in-person interview (CAPI). Detailed information on data collection procedures and sampling design is available elsewhere (SAMHSA 2002). The survey can be accessed via the Internet at http://www.icpsr.umich.edu/cgi-bin/SDA12/hsda?samhda+nhsda01.
This study uses a subsample of 18,849 adults between the ages of 18 and 65 who (1) endorsed at least one Diagnostic and Statistical Manual of Mental Disorders, 4th Edition (DSM-IV) symptom in the 12 months prior to the interview based on stem and summary symptom measures drawn from a truncated version of the World Health Organization's Composite International Diagnostic Interview Short Form (CIDI-SF) (Kendler et al. 1996; Kessler et al. 2003) and (2) had no DSM-IV dependency on any substance in the 12 months prior to the interview. The mental health symptoms covered in the surveys represent key constructs from the major disorders (major depressive disorder, mania, generalized anxiety disorder, panic attacks, social phobia, agoraphobia, and posttraumatic stress disorder). A respondent was considered to be substance dependent, if he or she endorsed three or more of criteria listed below for at least one substance: (1) great deal of time spent getting, using, or getting over the substance; (2) inability to set limits on use; (3) tolerance; (4) inability to cut down or stop use; (5) continued use despite emotional, mental, or physical problems; (6) reduced participation in important activities; and (7) withdrawal symptoms (not asked for all substances).
We limit the sample to individuals between the ages of 18 and 65 years for pragmatic and conceptual reasons. Those 18 years and younger were excluded because the surveys asked the mental health symptom questions only for those 18 and older. Those aged 65 years and older were excluded out of concern that our conceptual model is less applicable at older ages. Research suggests that elderly individuals differ from younger age groups in a variety of potentially confounding ways (Korper and Council 2002): (1) the use of heavy alcohol, marijuana, and other illicit drugs is extremely rare among the current cohort of elderly; (2) substance use (both licit and illicit) can have substantially different physiological and psychological effects at older ages; (3) older individuals may have different attitudes about and perceptions of their need for substance abuse and mental health care; and (4) the higher prevalence of physical health problems at older ages may motivate self-medication of painful medical conditions and have independent negative effects on mental health.
Dependent Variables
We examine three categories of past month substance use: (1) heavy alcohol, (2) marijuana, and (3) other illicit drugs. The survey defines heavy use of alcohol as drinking five or more drinks on the same occasion 5 or more days in the past 30 days. A drinking “occasion” is defined as at the same time or within a couple of hours of each other. A drink is defined as a can or bottle of beer, a glass of wine or a wine cooler, a shot of liquor, or a mixed drink containing liquor. The marijuana category includes hashish and respondents are asked to consider both smoked and ingested forms. The “other illicit drug” category includes two categories of substances. The first category consists of sedatives, stimulants, tranquilizers, and pain medications (not including over-the-counter medications) that were used in a nonindicated fashion. The survey defines nonindicated use as taking a prescription drug that was not prescribed for the respondent or if prescribed to the individual, taken not for illness and only for the experience or feeling it caused. In some cases, these drugs may or may not have been legally manufactured or imported and were not necessarily obtained with a doctor's prescription at a pharmacy. The second category includes hallucinogens, heroin, cocaine, and inhalants.
Independent Variables
Perceived unmet need for mental health care and use of mental health care in the 12 months prior to the interview constitute the two variables of key interest. To measure unmet need for mental health care, the survey asks all adult respondents whether “During the pasts 12 months, was there any time when you needed mental health treatment or counseling for yourself but didn't get it?” In this study, all sample members responding “yes” are considered to have unmet need for mental health care, regardless of whether they report using services. Respondents were considered mental health care users, if they reported during the past 12 months: (1) an inpatient stay for mental health treatment in a general or psychiatric hospital; (2) care in a mental health clinic; (3) receiving mental health treatment in an office of a doctor, private therapist, psychologist, psychiatrist, social worker, or counselor; (4) receiving mental health treatment in a partial day hospital, day-treatment program, or other locations, such as a church, shelter, or school; or (5) taking any prescription medication prescribed to treat a mental or emotional condition. Throughout the mental health use section of the interview, mental health care was defined as “treatment or counseling for problems with emotions, nerves, or mental health” and respondents were asked explicitly to exclude treatment for alcohol and drug use in answering questions about mental health care use.
A clinically validated six-item summary measure of nonspecific psychological distress is used to control for the severity of mental health problems among those with at least one disorder symptom. Scale values range from 0 to 24 with a score of 13 or above indicating a high likelihood of SMI (Kessler, Barker et al. 2003). We also include a summary measure of the number of CIDI-SF-measured symptoms to further control for the severity of mental health problems.
The NHSDA/NSDUH does not contain information about substance-use problems for the time period prior to the 12 months before the interview. For this reason, measures of lifetime use of substance-abuse treatment (including participation in Alcoholics Anonymous and other self-help groups) and perceived need for substance-abuse treatment in the prior year are used to control for remaining unobserved factors related to the propensity to use both substances and mental health care not eliminated after excluding those with past year substance dependencies.
We use an indicator of self-reported “fair” or “poor” physical health to control for the possibility that painful physical conditions lead to both substance use (nonindicated use of pain medication, in particular) and mental health problems. Other sociodemographic control variables include age, gender, health insurance status, marital status, income, education, and race and ethnicity. An indicator for survey year was included to control for differences across years in the propensity to report substance use, unmet need, and mental health care use.
Estimation Procedures
For each of the three substance-use categories, we estimated a series of binary logistic regression models to measure the effect of past year unmet need and mental health use on past 30 days of substance use. Our goal was to assess the relative contribution of clinical and demographic characteristics in explaining associations between substance use and our two mental health care measures. To this end, the first model contained only the measures of past 12-month unmet need for mental health care and past 12-month mental health care utilization, along with an indicator of the survey year; the second model added the two mental health problem measures, the two measures of substance-abuse treatment, and self-reported health status; and the third model added the full set of sociodemographic controls. All analyses employed sampling weights and were adjusted to account for the clustered sampling design in the NHSDA/NSDUH. Information on stratification was not used, making our standard error estimates conservative (Stata Corporation 2003). Raw regression coefficients are available via http://www.hsr.org.
We then used the logit parameter estimates resulting from each model to generate predicted probabilities of past 30-day substance use by unmet need and mental health care use holding other covariates fixed at their sample means. Corresponding standard error estimates are calculated using a Monte Carlo method described by Tomz et al. (2003).
Results
Descriptive Analyses
Almost a quarter of respondents between the ages of 18 and 65 years reported at least one mental health symptom, with 29.9 percent of symptomatic respondents reporting psychological distress severe enough to be considered seriously mentally ill (see Table 1). Overall, 17.7 percent of the subsample reported unmet need for mental health care and 27.5 percent of the sample reported using mental health care from any professional source (see Table 1). These two rates compare favorably to those obtained from other nationally representative samples of individuals with psychiatric symptoms (Kessler et al. 1994; Wells, Klap et al. 2001; Wells, Sherbourne et al. 2002).
Table 1.
Probability of Past Month Substance Use by Past Year Mental Health Care Problems, Unmet Need for Mental Health Care, and Use of Mental Health Care for All Adults Aged 18–65 years with No Past Year DSM-IV Dependence on Any Substance and Those with One or More Mental Health Symptoms
| Heavy Use of Alcohol | Marijuana | Other Illegal Drugs | Unweighted | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Characteristic | % | SE | p-value | % | SE | p-value | % | SE | p-value | N | % |
| One or more mental health symptoms | |||||||||||
| No | 6.1 | 0.2 | .097 | 3.7 | 0.1 | <.001 | 2.0 | 0.1 | <.001 | 60,273 | |
| Yes | 5.6 | 0.2 | 4.8 | 0.2 | 4.5 | 0.3 | 18,849 | 23.8 | |||
| One or more mental health symptoms | |||||||||||
| Serious mental illness | |||||||||||
| No | 6.0 | 0.3 | .004 | 4.6 | 0.3 | .148 | 3.7 | 0.3 | <.001 | 13,220 | |
| Yes | 4.6 | 0.4 | 5.3 | 0.4 | 6.5 | 0.6 | 5,629 | 29.9 | |||
| Unmet need for mental health care | |||||||||||
| No | 5.8 | 0.3 | .142 | 4.7 | 0.2 | .303 | 4.0 | 0.3 | <.001 | 15,438 | |
| Yes | 4.8 | 0.6 | 5.3 | 0.5 | 7.4 | 0.8 | 3,328 | 17.7 | |||
| Mental health care use | |||||||||||
| No | 6.6 | 0.3 | <.001 | 5.1 | 0.3 | .063 | 4.2 | 0.3 | .089 | 13,591 | |
| Yes | 3.5 | 0.3 | 4.2 | 0.4 | 5.2 | 0.5 | 5,175 | 27.5 | |||
Note: Unless noted, proportions nationally weighted and standard errors are adjusted to reflect the complex survey design in the 2001–2002 NHSDA/NSDUH.
DSM-IV=Diagnostic and Statistical Manual of Mental Disorders, 4th Edition; NHSDA=National Household Survey on Drug Abuse; NSDUH=National Survey on Drug Use and Health.
Even when excluding the subgroup with substance dependence, those with mental health problems were more likely than the general population to use illicit drugs and rates of use increased with the severity of mental health problems. Table 1 shows that those with at least one mental health symptom were significantly more likely to have used both marijuana and other illicit drugs in the past 30 days (4.8 versus 3.7 percent for marijuana, p<.001; and 4.5 versus 2.0 percent for other illicit drugs, p<.001), compared with those without symptoms. By contrast, those with mental health symptoms did not engage in heavy alcohol use at higher rates. Among the subgroup with one or more mental health symptoms, those with serious mental illness used illicit drugs other than marijuana at higher rates (6.5 versus 3.7 percent, p<.001) and used heavy alcohol at lower rates (4.6 versus 6.0 percent, p=.004).
The simple bivariate relationships between past-month substance use and the mental health unmet need and use variables differ by substance. Table 1 shows that heavy use of alcohol was significantly less among past-year mental health care users compared with nonusers (3.5 versus 6.6 percent, p<.001). At the same time, there was no difference in heavy alcohol use on the basis of unmet need. By contrast, illicit drug use was significantly higher among those with unmet need (7.4 percent versus 4.0, p<.001), while there were no differences between users and nonusers of mental health care. Marijuana use rates were statistically similar for those with unmet need and no unmet need for mental health care and for users and nonusers of mental health care.
Table 2 shows that both perceived unmet need for mental health care and mental health care use were strongly related to clinical and sociodemographic characteristics, highlighting the potential for confounding of the bivariate relationships between substance use and the mental health care measures shown in Table 1. Mean levels of psychological distress were significantly higher among those reporting unmet need for mental health care (13.69 versus 8.12 percent, p<.001) and among mental health users (12.17 versus 7.50 percent, p<.001). Likewise, mental health care users and those with unmet need report a higher number of mental health symptoms. The exclusion of those with substance dependencies resulted in a very small percentage (1.2 percent or less) reporting past year need for substance abuse treatment. Ever receiving substance-abuse treatment was strongly associated with unmet need for mental health care (11.8 versus 7.5 percent, p<.001) and use (12.3 versus 6.3 percent, p<.001). Other sociodemographic characteristics substantially differed across unmet need and mental-health-care-use categories.
Table 2.
Respondent Characteristics by Unmet Need for Mental Health (MH) Care and MH Care Use in the Past 12 Months for Those Aged 18–65 Years with at Least One Symptom of a Mental Disorder and No DSM-IV Substance Dependence in the Past 12 Months
| Unmet Need for MH Care | Used MH Care | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| No | Yes | No | Yes | |||||||
| Characteristic | ||||||||||
| Mean | SE | Mean | SE | p-value | Mean | SE | Mean | SE | p-value | |
| Continuous measures* | ||||||||||
| Psychological distress score | 8.12 | 0.08 | 13.69 | 0.17 | <.001 | 7.50 | 0.08 | 12.17 | 0.13 | <.001 |
| Number of MH symptoms | 1.92 | 0.02 | 3.02 | 0.09 | <.001 | 1.79 | 0.02 | 2.73 | 0.06 | <.001 |
| Categorical measures† | % | SE | % | SE | p-value | % | SE | % | SE | p-value |
| Race/ethnicity | ||||||||||
| White | 72.5 | 0.7 | 76.9 | 1.4 | <.001 | 69.8 | 0.8 | 80.5 | 1.1 | <.001 |
| African-American | 10.9 | 0.5 | 9.2 | 1.0 | 12.0 | 0.5 | 7.8 | 0.7 | ||
| Hispanic-Latino | 10.9 | 0.5 | 9.3 | 1.0 | 12.3 | 0.5 | 7.3 | 0.7 | ||
| Other non-Hispanic | 5.7 | 0.4 | 4.5 | 0.6 | 6.0 | 0.4 | 4.5 | 6.7 | ||
| Age category | ||||||||||
| 18–22 | 10.8 | 0.3 | 12.1 | 0.6 | <.001 | 13.0 | 0.3 | 6.7 | 0.3 | <.001 |
| 23–24 | 6.7 | 0.2 | 8.4 | 0.4 | 7.9 | 0.2 | 5.0 | 0.2 | ||
| 25–29 | 10.4 | 0.4 | 11.3 | 0.8 | 11.5 | 0.4 | 8.5 | 0.5 | ||
| 30–39 | 22.4 | 0.6 | 26.4 | 1.2 | 22.9 | 0.6 | 23.3 | 0.9 | ||
| 40–49 | 24.3 | 0.6 | 25.6 | 1.3 | 22.6 | 0.6 | 28.3 | 1.0 | ||
| 50–59 | 18.6 | 0.7 | 14.5 | 1.4 | 15.8 | 0.7 | 22.6 | 1.2 | ||
| 60–65 | 6.8 | 0.5 | 1.7 | 0.5 | 6.2 | 0.5 | 5.6 | 0.7 | ||
| Marital status | ||||||||||
| Married | 51.7 | 0.7 | 44.6 | 1.5 | <.001 | 50.6 | 0.8 | 50.4 | 1.2 | <.001 |
| Widowed | 2.8 | 0.2 | 2.7 | 0.4 | 2.7 | 0.3 | 2.6 | 0.4 | ||
| Never married | 29.4 | 0.6 | 32.4 | 1.2 | 32.5 | 0.6 | 24.5 | 0.9 | ||
| Divorced/separated | 16.1 | 0.5 | 20.9 | 1.3 | 14.2 | 0.5 | 22.5 | 1.0 | ||
| Dichotomous measure‡ | % | SE | % | SE | p-value | % | SE | % | SE | p-value |
| SA treatment | ||||||||||
| Prior year need for SA treatment | 0.4 | 0.1 | 1.2 | 0.4 | .069 | 0.5 | 0.1 | 0.5 | 0.1 | .922 |
| Ever treated for SA | 7.5 | 0.4 | 11.8 | 1.0 | <.001 | 6.3 | 0.4 | 12.3 | 0.8 | <.001 |
| Other characteristics | ||||||||||
| Family income <$20,000 | 21.3 | 0.6 | 26.0 | 1.3 | .001 | 21.0 | 0.6 | 24.4 | 1.1 | <.001 |
| Female | 58.3 | 0.7 | 73.4 | 1.3 | <.001 | 56.1 | 0.7 | 70.4 | 1.1 | <.001 |
| No health insurance | 17.1 | 0.5 | 22.1 | 1.2 | <.001 | 20.8 | 0.6 | 11.8 | 0.7 | <.001 |
| College graduate | 20.2 | 0.6 | 22.1 | 1.2 | .133 | 18.3 | 0.6 | 25.0 | 1.0 | <.001 |
| Rural residence | 13.8 | 0.6 | 11.5 | 0.9 | .017 | 13.6 | 0.7 | 13.1 | 0.8 | .625 |
| Health fair or poor | 16.5 | 0.6 | 22.4 | 1.4 | <.001 | 13.5 | 0.6 | 25.9 | 1.1 | .000 |
| 2002 survey year | 53.9 | 0.8 | 55.9 | 1.5 | .193 | 53.0 | 0.8 | 56.7 | 1.2 | .008 |
Note: Entries are nationally weighted and standard errors are adjusted to reflect the complex survey design in the 2001–2002 NHSDA/NSDUH.
Reported p-values correspond to t-tests of differences in means.
Reported p-values correspond to design-corrected F-tests of independence.
Reported p-values correspond to t-tests of differences in proportions.
SA=substance abuse.
Multivariate Analyses
Controlling for a wide range of clinical and sociodemographic characteristics did not alter the patterns of bivariate relationships observed between substance use and the two mental health care variables in Table 1. Across all three specifications, heavy alcohol use remained significantly lower among mental health care users compared with nonusers. In the model with the full set of covariates, mental health care users were only about 0.6 times as likely to report heavy alcohol use (2.7 versus 4.4 percent, p<.001) (Table 3). There continued to be no difference in heavy alcohol or marijuana use by perceived unmet need in the presence of covariates. Likewise, rates of other illicit drug use remained significantly higher for those reporting unmet need for mental health care in all three specifications. In the model with the full set of covariates, rates of other illicit drug use were 1.4 times higher among individuals who reported unmet need for mental health services versus those who did not (4.4 versus 3.2 percent, p=.048). There were no differences in the use of other illicit drugs by mental health care use in any of the three model specifications. By contrast, estimates of the relationship between marijuana use and mental health care use were particularly sensitive to the presence and types of covariates. Controlling for survey year and clinical measures yielded significant differences in predicted substance-use rates by unmet need. However, these differences were not apparent when the full set of covariates was included in the model.
Table 3.
Estimated Probability of Substance Use in the Past 30 Days by Past Year Unmet Need for Mental Health Care and Use of Mental Health for Those with at Least One Symptom of a Mental Disorder and No Dependence on Any Substance in the Past 12 Months
| Unmet Need for Mental Health Care | Use of Mental Health Care | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| No | Yes | No | Yes | |||||||
| Substance Category | % | SE | % | SE | p-value* | p-value* | ||||
| Heavy alcohol | ||||||||||
| Survey year only | 5.5 | 0.3 | 5.3 | 0.6 | .834 | 6.6 | 0.3 | 3.5 | 0.3 | <.001 |
| Survey year+Clinical measures† | 5.2 | 0.3 | 4.7 | 0.6 | .482 | 6.3 | 0.3 | 3.2 | 0.3 | <.001 |
| Survey year+Clinical measures+ Sociodemographic characteristics‡ | 3.8 | 0.3 | 3.4 | 0.5 | .411 | 4.4 | 0.3 | 2.7 | 0.3 | <.001 |
| Marijuana | ||||||||||
| Survey year only | 4.7 | 0.2 | 5.5 | 0.6 | .150 | 5.1 | 0.3 | 4.1 | 0.4 | .046 |
| Survey year+Clinical measures† | 4.5 | 0.2 | 4.9 | 0.5 | .396 | 4.9 | 0.3 | 3.8 | 0.4 | .017 |
| Survey year+Clinical measures+ Sociodemographic characteristics‡ | 3.3 | 0.3 | 3.4 | 0.5 | .902 | 4.4 | 0.3 | 3.0 | 0.3 | .863 |
| Other illicit drugs | ||||||||||
| Survey year only | 3.9 | 0.3 | 7.2 | 0.8 | <.001 | 4.2 | 0.3 | 4.6 | 5.1 | .463 |
| Survey year+Clinical measures† | 3.7 | 0.3 | 5.5 | 0.7 | .011 | 4.1 | 0.3 | 3.5 | 4.5 | .314 |
| Survey year+Clinical measures+ Sociodemographic characteristics‡ | 3.2 | 0.3 | 4.4 | 0.6 | .048 | 3.3 | 0.3 | 3.4 | 0.4 | .990 |
Note: Adjusted entries are predicted values based on logistic models of substance use on unmet need for mental health care, use of mental health care, and other covariates.
Reported p-value for two-sided t-test of difference in means.
Clinical measures include indicators of mental health disorders, “K6” psychological distress score, prior need for substance abuse treatment, ever received substance abuse treatment, and self-reported health status.
Sociodemographic characteristics include race/ethnicity, categorical age, family income <$20,000, gender, marital status, health insurance status, college graduate, and rural residence.
Discussion
This study finds that substance use in the past 30 days varies with past year unmet need for mental health care and mental health care use in ways predicted by the self-medication hypothesis. However, the nature of the effects varied across the three substance categories. In no category did we observe increased substance use associated with unmet need and decreased substance use associated with mental health care use. Use of illicit drugs other than marijuana increased with unmet need, but was not reduced with mental health care use. Heavy alcohol use was not associated with increased unmet need for mental health care, but was reduced with mental health care use. By contrast, marijuana use did not appear associated with either unmet need or mental health care use.
Notable are differences in our findings across the substance categories. Stronger effects of mental health care use on alcohol may suggest that mental health treatment may be more effective in treating the underlying symptoms that prompt alcohol use. Alternatively, mental health patients may be better screened for alcohol use than for other types of drug use. Likewise, providers may be more forthcoming with advice about the exacerbating effects of alcohol than they are about other forms of substances.
At the same time, the lack of relationship between unmet need for mental health care and heavy alcohol use is somewhat surprising given the frequent observation that alcohol use is common among those with untreated mental health conditions. This lack of relationship suggests that people are not recognizing their mental health symptoms as treatable or, perhaps, attributing symptoms to alcohol use rather than mental health problems.
It is interesting to contrast studies of the relationship between the use of “unconventional” treatments (e.g., homeopathic remedies, herbs) and the use of professionally sanctioned services. Unlike the negative association predicted and observed in this study, previous research has generally found a positive correlation between use of unconventional and conventional medical services (Eisenberg et al. 2001; Druss and Rosenheck 1999; 2001) and a positive (Kessler et al. 2001) or insignificant (Unutzer et al. 2000) correlation in the case of mental health care. Several factors help explain the differences in observed correlations: (1) patients may perceive positive benefits from unconventional treatments, while the negative effects of substance use are well known and (2) unlike the use of unconventional treatments, substance use is more heavily stigmatized than alternative medications and is, in many cases, illegal.
These findings suggest that timely and appropriate mental health treatment may prevent the development of substance-use disorders. However, the implications of our findings for clinical policy depend on an improved understanding of the sources of perceived unmet need. Unfortunately, sample size constraints limited our ability to explore the effect of interactions between unmet need and the use of mental health care use on substance use. In our sample, among individuals with unmet need, 48 percent received no treatment in the past year. Their reasons for not receiving treatment may be similar to those given by National Comorbidity Survey respondents with serious mental illness who perceived a need for treatment, but received no treatment in the past 12 months (Kessler et al. 2001): wanted to solve problem on own (72.1 percent); thought problem would get better by itself (60.6 percent); perceived lack of effectiveness (45.4 percent); had financial barriers (45.6 percent); were unsure about where to go for help (40.8 percent); and thought it would take too much time or be inconvenient (27.7 percent).
Although we know of no published study that examines the determinants of unmet need among those who have received services in the past 12 months (in our sample, 52 percent of those with unmet need), we can speculate. Some might have felt treatment was not effective or not acceptable; others may have been stigmatized by neighbors or coworkers, and therefore exited treatment; some might have experienced partial improvement, but financial barriers precluded further treatment; and others might have found treatment to be inconvenient.
The results of this study should be interpreted in light of several limitations. First, while NHSDA/NSDUH offers several advantages over other data sources, it is not possible to unambiguously determine whether the mental health use and need occurred prior to reported substance use and if so, whether need and use of mental health care can meaningfully influence current substance use in the relatively short span of 12 months. Second, the surveys lack a measure of chronic physical pain. While respondents over the age of 65 years were excluded from the analysis and the multivariate analyses contain an indicator of self-reported fair or poor health, these steps are probably insufficient to fully control for the simultaneous effects of pain on mental health and substance use (Rosenblum et al. 2003). However, the inability to fully control for higher use of both substances and mental health care among those in chronic pain would bias the results away from finding evidence of self-medication.
Third, it is reasonable to expect that a subgroup of respondents do not report unmet need for mental health care because their use of substances has satisfactorily reduced symptoms at the time of the interview. However, this type of behavior would reduce observed differences in substance use by unmet need, making inferences about self-medication conservative.
Fourth, although we attempt to exclude the subpopulation for whom established substance-use disorders contribute to mental health problems, it is unlikely that we have been fully successful and the effect on our inferences is different depending on the measure. To the extent that these individuals remain in the sample, psychological and physiological effects of dependency not treated by mental health care providers would serve to reduce negative differences in substance use by mental health care use, resulting in conservative inferences about self-medicating behavior. The effect on unmet need is less clear. To the extent that individuals with substance-induced mental health problems perceive mental health care as less accessible or less effective, then our findings will overstate the positive association between mental health care use and unmet need for mental health care.
Finally, one alternative explanation for the positive relationship between unmet need and illicit drug use is the so-called “Wrath of Grapes” phenomenon observed in clinical interviews (Frances 1997). Here, patients use mental health problems as a post hoc justification for substance use. However, it is not clear whether this occurs among nondependent users like the ones in our sample or in the context of survey administration.
Our study highlights the potentially valuable role of research on perceived mental health care need and service use on the underlying causes of and treatments for co-occurring disorders. While not a causal test, our study represents a first attempt to inform the self-medication hypothesis from a health services perspective. The positive relationship between unmet need and illicit drug use and the negative relationship between mental health care use and heavy alcohol use among those without substance dependency is consistent with the behavior predicted under the self-medication hypothesis and suggests that mental health treatment may prevent the development of substance-use disorders.
Acknowledgments
This work was supported by SAMHSA's Office of Applied Studies and a Research Career Development Award (RCD-03-036) from the VA Health Services Research and Development Services to Dr. Edlund. This paper does not represent the policies or the positions of the Office of Applied Studies, the Substance Abuse and Mental Health Services Administration, the U.S. Department Health and Human Services, or the Department of Veterans Affairs. No official endorsement by any of these organizations is intended nor should be inferred.
References
- Chilcoat HD, Breslau N. “Posttraumatic Stress Disorder and Drug Disorders: Testing Causal Pathways.”. Archives of General Psychiatry. 1998;55(10):913–7. doi: 10.1001/archpsyc.55.10.913. [DOI] [PubMed] [Google Scholar]
- Dixit AR, Crum RM. “Prospective Study of Depression and the Risk of Heavy Alcohol Use in Women.”. American Journal of Psychiatry. 2000;157(5):751–8. doi: 10.1176/appi.ajp.157.5.751. [DOI] [PubMed] [Google Scholar]
- Druss BG, Rosenheck RA. “Association between Use of Unconventional Therapies and Conventional Medical Services.”. Journal of the American Medical Association. 1999;282(7):651–6. doi: 10.1001/jama.282.7.651. [DOI] [PubMed] [Google Scholar]
- Eisenberg DM, Kessler RC, Van Rompay MI, Kaptchuk TJ, Wilkey SA, Appel SA, Davis RB. “Perceptions about Complementary Therapies Relative to Conventional Therapies among Adults Who Use Both: Results from a National Survey.”. Annals of Internal Medicine. 2001;135(5):344–51. doi: 10.7326/0003-4819-135-5-200109040-00011. [DOI] [PubMed] [Google Scholar]
- Frances RJ. “The Wrath of Grapes versus the Self-medication Hypothesis.”. Harvard Review of Psychiatry. 1997;4(5):287–9. doi: 10.3109/10673229709030556. [DOI] [PubMed] [Google Scholar]
- Kendler KS, Gallagher TJ, Abelson JM, Kessler RC. “Lifetime Prevalence, Demographic Risk Factors, and Diagnostic Validity of Nonaffective Psychosis as Assessed in a US Community Sample. The National Comorbidity Survey.”. Archives of General Psychiatry. 1996;53(11):1022–31. doi: 10.1001/archpsyc.1996.01830110060007. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Barker PR, Colpe LJ, Epstein JF, Gfroerer JC, Hiripi E, Howes MJ, Normand SL, Manderscheid RW, Walters EE, Zaslavsky AM. “Screening for Serious Mental Illness in the General Population.”. Archives of General Psychiatry. 2003;60(2):184–9. doi: 10.1001/archpsyc.60.2.184. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Berglund PA, Bruce ML, Koch JR, Laska EM, Leaf PJ, Manderscheid RW, Rosenheck RA, Walters EE, Wang PS. “The Prevalence and Correlates of Untreated Serious Mental Illness.”. Health Services Research. 2001;36(6):987–1007. [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, Davis RB, Foster DF, Van Rompay MI, Walters EE, Wilkey SA, Kaptchuk TJ, Eisenberg DM. “Long-term Trends in the Use of Complementary and Alternative Medical Therapies in the United States.”. Annals of Internal Medicine. 2001;135(4):262–8. doi: 10.7326/0003-4819-135-4-200108210-00011. [DOI] [PubMed] [Google Scholar]
- Kessler RC, McGonagle KA, Zhao S, Nelson CB, Hughes M, Eshleman S, Wittchen HU, Kendler KS. “Lifetime and 12-month Prevalence of DSM-III-R Psychiatric Disorders in the United States.”. Archives of General Psychiatry. 1994;51(1):8–19. doi: 10.1001/archpsyc.1994.03950010008002. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Nelson CB, McGonagle KA, Edlund MJ, Frank RG, Leaf PJ. “The Epidemiology of Co-occurring Addictive and Mental Disorders: Implications for Prevention and Service Utilization.”. American Journal of Orthopsychiatry. 1996;66(1):17–31. doi: 10.1037/h0080151. [DOI] [PubMed] [Google Scholar]
- Khantzian EJ. “The Self-medication Hypothesis of Substance Use Disorders: A Reconsideration and Recent Applications.”. Harvard Review of Psychiatry. 1997;4:231–44. doi: 10.3109/10673229709030550. [DOI] [PubMed] [Google Scholar]
- Korper SP, Council CL, editors. Rockville: MD: Substance Abuse and Mental Health Services Adminstration, Office of Applied Studies.; 2002. “Substance Use by Older Adults: Estimates of Future Impact on the Treatment System.” DHHS Publication No. SMA 03-3763, Analytic Series A-21. [Google Scholar]
- Popkin MK, Tucker GJ. “Secondary and Drug-induced Mood, Anxiety, Psychotic, Catatonic, and Personality Disorders: A Review of the Literature.”. Journal of Neuropsychiatry and Clinical Neurosciences. 1992;4(4):369–85. doi: 10.1176/jnp.4.4.369. [DOI] [PubMed] [Google Scholar]
- Raimo EB, Schuckit MA. “Alcohol Dependence and Mood Disorders.”. Addict Behavior. 1998;23(6):933–46. doi: 10.1016/s0306-4603(98)00068-9. [DOI] [PubMed] [Google Scholar]
- Regier DA, Farmer ME, Rae DS, Locke BZ, Keith SJ, Judd LL, Goodwin FK. “Comorbidity of Mental Disorders with Alcohol and Other Drug Abuse. Results from the Epidemiologic Catchment Area (ECA) Study.”. Journal of the American Medical Association. 1990;264(19):2511–8. [PubMed] [Google Scholar]
- Rosenblum A, Joseph H, Fong C, Kipins S, Cleland C, Portenoy RK. “Prevalence and Characteristics of Chronic Pain Among Chemically Dependent Patients in Methadone Maintenance and Residential Treatment Facilities.”. Journal of the American Medical Association. 2003;289(18):2370–8. doi: 10.1001/jama.289.18.2370. [DOI] [PubMed] [Google Scholar]
- Schuckit MA, Tipp JE, Bergman M, Reich W, Hesslebrock VM, Smith TL. “Comparison of Induced and Independent Major Depressive Disorders in 2,945 Alcoholics.”. American Journal of Psychiatry. 1997;154(7):948–57. doi: 10.1176/ajp.154.7.948. [DOI] [PubMed] [Google Scholar]
- Stata Corporation . Stata Survey Data Reference Manual, Release 8.0. College Station TXStata Corp: 2003. [Google Scholar]
- Strakowski SM, DelBello MP. “The Co-occurrence of Bipolar and Substance Use Disorders.”. Clinical Psychological Review. 2000;20(2):191–206. doi: 10.1016/s0272-7358(99)00025-2. [DOI] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration . Rockville MD: 2002. “Summary of Findings from the 2001 National Household Survey on Drug Abuse: Volume II.” Technical Appendices and Selected Tables. Office of Applied Studies, NHSDA Series H-18, DHHS Publication No. (SMA) 02-3759. [Google Scholar]
- Substance Abuse and Mental Health Services Administration . Rockville: MD; 2003. “Summary of Findings from the 2001 National Household Survey on Drug Abuse.” Office of Applied Studies, NHSDA Series H-22, DHHS Publication No. (SMA) 03-3836. [Google Scholar]
- Tomz M, Wittenburg J, King G. 2003. Clarify: Software for Interpreting and Presenting Statistical Results.
- Unutzer J, Klap R, Sturm R, Young AS, Marmon T, Shatkin J, Wells KB. “Mental Disorders and the Use of Alternative Medicine: Results from a National Survey.”. American Journal of Psychiatry. 2000;157(11):1851–7. doi: 10.1176/appi.ajp.157.11.1851. [DOI] [PubMed] [Google Scholar]
- Vaillant GE. “Natural History of Male Psychological Health, XIV: Relationship of Mood Disorder Vulnerability to Physical Health.”. American Journal of Psychiatry. 1998;155(2):184–91. doi: 10.1176/ajp.155.2.184. [DOI] [PubMed] [Google Scholar]
- Wells K, Klap R, Koike A, Sherbourne C. “Ethnic Disparities in Unmet Need for Alcoholism, Drug Abuse, and Mental Health Care.”. American Journal of Psychiatry. 2001;158(12):2027–32. doi: 10.1176/appi.ajp.158.12.2027. [DOI] [PubMed] [Google Scholar]
- Wells KB, Sherbourne CD, Sturm R, Young AS, Burnam MA. “Alcohol, Drug Abuse, and Mental Health Care for Uninsured and Insured Adults.”. Health Services Research. 2002;37(4):1055–66. doi: 10.1034/j.1600-0560.2002.65.x. [DOI] [PMC free article] [PubMed] [Google Scholar]