Abstract
Objective
To examine whether racial and ethnic differences in the distribution of individuals across types of health plans explain differences in satisfaction and trust with their physicians.
Data Sources
Data were derived from the 1998–1999 Community Tracking Household and Followback Studies and consisted of a nationwide sample of adults (18 years and older).
Data Collection
The data were collected by telephone survey. Surveys were administered in English and Spanish. The response rate for the Household Survey was 63 percent, and the match rate for the Followback Survey was 59 percent.
Study Design
Multivariate analyses used regression methods to detect independent effects of respondent race and ethnicity on satisfaction and trust with physician, while controlling for enrollment in different types of health plans.
Principal Findings
Racial and ethnic minorities are more likely than whites to have lower levels of trust and satisfaction with their physician. The most prominent differences occurred within the Latino and Native American/Asian American/Pacific Islander/Other (“Other”) populations. Plan type does not mitigate the relationship between race/ethnicity and trust and satisfaction for the overall adult population.
Conclusions
Disparate levels of trust and satisfaction exist within ethnic and minority populations, even when controlling for the distribution of individuals across types of health plans. The results demonstrate a need to better understand the health care-related factors that drive disparate trust and satisfaction.
Keywords: Race, ethnicity, insurance, disparities, physician–patient relationship, health care, patient satisfaction, patient trust
Racial and ethnic disparities in health and health care are well documented (Smedley, Stith, and Nelson 2002). Yet, a full understanding of the causal mechanisms of these disparities remains elusive. Three threads of work stimulated this paper. First, patient preferences may play a pronounced role in explaining disparities—patients' values and beliefs, including their level of trust in clinical advice, influence the level of care they receive (Smedley, Stith, and Nelson 2002). Specifically, a patient's comfort level with an intervention can influence his or her willingness to seek or accept treatment, be it physical or emotional. Second, physicians' advice and behavior may vary depending on perceived patient attributes (Smedley, Stith, and Nelson 2002). Third, racial and ethnic minorities have lower levels of trust and satisfaction with their providers—physicians, hospitals, health plans, and the health care system in general (Meredith and Sui 1995; Auslander et al. 1997; Taira et al. 1997; Morales et al. 1999; Doescher et al. 2000; LaVeist, Nickerson, and Bowie 2000; Murray-García et al. 2000; Morales et al. 2001; Weech-Maldonado et al. 2001; Collins et al. 2002; Corbie-Smith, Thomas, and St. George 2002; Shi et al. 2003).
We wondered whether trust and satisfaction could be explained by the type of plan in which many racial and ethnic minorities find themselves. Prior studies suggest that individuals—regardless of race and ethnicity—enrolled in more heavily managed care plans like capitated or group model health maintenance organizations (HMOs) report less favorable assessments of the care provided by their physicians. Racial and ethnic minorities are more likely to be enrolled in restrictive, tightly managed care plans than whites, thereby explaining their lower levels of trust and satisfaction (Center for Studying Health System Change 2000). Unequal Treatment astutely points out that much of the previous research on racial and ethnic disparities controls for insurance status on a very general level (e.g., insured versus uninsured, privately insured versus publicly insured, etc.), but it does not adequately control for the generosity or restrictiveness of a particular insurance coverage. Findings from this research therefore leave open the possibility that racial disparities in care result to some degree from the disproportionate enrollment of racial and ethnic subgroups in more restrictive health plans (Smedley, Stith, and Nelson 2002). Our study attempts to fill this gap in the literature on trust and satisfaction.
From a public policy standpoint, it is important to understand these differences because trust and satisfaction have been linked to health outcomes (Morales et al. 2001). Patient assessments of health care are associated with service utilization (Zastowny, Roghmann, and Cafferata 1998), the decision to switch health plans (Newcomer, Preston, and Harrington 1996; Allen and Rogers 1997; Schlesinger, Druss, and Thomas 1999), and treatment compliance (Hall and Dornan 1990).
Background
The literature on trust and satisfaction with health care among members of racial and ethnic subgroups ranges across provider types—physicians, hospitals, plans, and the entire health care system. Previous research suggests that members of racial and ethnic minority groups have lower levels of trust in their physician and/or hospital (Saha et al. 1999; Doescher et al. 2000; LaVeist, Nickerson, and Bowie 2000; Corbie-Smith, Thomas, and St. George 2002; Shi et al. 2003). Findings on satisfaction, however, seem to vary based on the subgroup in question and the provider or care setting, which ranges across physician, medical staff, and health plan (Meredith and Sui 1995; Taira et al. 1997; Morales et al. 1999; Doescher et al. 2000; LaVeist, Nickerson, and Bowie 2000; Murray-García et al. 2000; Phillips, Mayer, and Aday 2000; Morales et al. 2001; Weech-Maldonado et al. 2001). Some studies indicate that Latinos/Hispanics are less satisfied with the care provided by physicians and health plans than whites, while others suggest that African Americans are less satisfied. Finally, most findings suggest that Asians and Pacific Islanders have lower levels of satisfaction with their physicians, health care, and/or health plans than whites (Meredith and Sui 1995; Taira et al. 1997; Murray-García et al. 2000; Weech-Maldonado et al. 2001). And, research indicates that dissatisfaction with the health care system may be related to perceived racism (Auslander et al. 1997; LaVeist, Nickerson, and Bowie 2000).
The literature regarding racial and ethnic disparities in trust and satisfaction with provider does not control for the restrictiveness of health plans, despite a strong association between health plan restrictiveness and lower ratings of trust and satisfaction. For example, Reschovsky, Kemper, and Tu (2000), Kemper et al. (2002), and Kao et al. (1998) all find that consumer assessments of satisfaction and trust with physician care are lower in more heavily managed plan settings. Newcomer, Preston, and Harrington (1996) found that individuals who reported higher levels of satisfaction with physician quality and physician–patient relationships were less likely to disenroll from their HMOs. Managed health plans that allow greater provider choice and have fewer gatekeeping restrictions are associated with higher levels of patient satisfaction and trust with physician (Forrest et al. 2002; Haas et al. 2003).
We hypothesized that controlling for the type of health plan in which an individual was enrolled would reduce racial and ethnic disparities in trust and satisfaction. Because of data limitations, we restrict our analysis to respondents' perceptions of trust and satisfaction with physician care, rather than hospital, health plan, or any other provider type. To better understand patient perceptions of the health care system with respect to their physicians, our study asks: does the distribution of individuals across types of health plans explain differences in levels of trust and satisfaction with physician care by racial and ethnic background?
Data and Methods
Data Source
We used data from the Community Tracking Study (CTS) 1998–1999 Household and Followback Surveys for our analysis. The CTS is a longitudinal study of health system change and its effects on individuals nationwide as well as within 60 randomly selected sites across the nation. The study is conducted by the Center for Studying Health System Change. The Household Survey contains information on basic demographics, insurance coverage, service utilization, usual sources of care, trust and satisfaction, chronic health conditions, and risk behaviors. The Followback Survey provides more detailed information about the health plans of individuals who reported private insurance coverage. The Followback information was collected by contacting the employer or health plan associated with a respondent's private coverage and asking about insurance plan characteristics such as product type, in- and out-of-network coverage, and provider payment methods (Center for Studying Health System Change 2002a).
A detailed explanation of the CTS sampling methods is published elsewhere (Kemper et al. 1996; Metcalf et al. 1996). Briefly, the Household Survey is a multistage, clustered sample with stratification based on 60 randomly selected sites and a supplemental national survey. Households are randomly selected for telephone interview using computer-assisted telephone interviewing technology. The majority of respondents are selected through random digit dialing, but households without telephones are also represented in the sample. The survey is conducted in Spanish when necessary. The full 1998–1999 household sample consists of over 58,000 individuals and 32,000 families, and the followback sample consists of more than 22,000 individuals. The response rate for the Household Survey was 63 percent, and the match rate for the Followback Survey was 59 percent.1
For this study, we include individual-level data for adults, age 18 years and over. Individuals who reported insurance coverage through a military plan were excluded from our analysis. The data are weighted to control for clustering, stratification, and nonresponse so that results may be extrapolated to the noninstitutionalized population of the continental United States.
Dependent Variables: Measures of Trust and Satisfaction
We used seven questions from the CTS instrument to construct two trust and satisfaction indices that ranged from one to five. Trust and satisfaction with physician care are highly complex measures to operationalize because they are based on perception. We focused this analysis by looking only at an individual's trust in his or her physician and satisfaction with his or her physician's care at the last office visit. Four of these questions related to trust in physician, and three related to satisfaction with the physician's care during the last visit. The trust questions asked respondents to think about their usual doctor or their last visit to the doctor and indicate whether they agreed with the following statements:
“I think my doctor may not refer me to a specialist when needed;”
“I trust my doctor to put my medical needs above all other considerations when treating my medical problems;”
“I think my doctor is strongly influenced by health insurance company rules when making decisions about my medical care;” and
“I sometimes think that my doctor might perform unnecessary tests or procedures.”
Possible responses for these questions were based on a five-point Likert scale and ranged from strongly disagree to strongly agree. The satisfaction questions asked respondents to rate their last physician visit based on:
“The thoroughness and carefulness of the examination and treatment you received;”
“How well your doctor listened to you;” and
“How well the doctor explained things in a way you could understand.”
The possible responses for these questions were also based on a five-point Likert scale, and they ranged from poor to excellent.
Because the trust and satisfaction variables were highly correlated, we simplified our analysis by constructing trust and satisfaction indices that ranged from one to five. The universe of respondents for the four trust questions included all adults who had a usual physician or at least one visit to a physician in the previous 12 months. We combined these questions into one “trust” index, which is calculated by taking the mean of all four responses for each individual who answered all four questions.2 Therefore, we lost some cases because of question nonresponse—if even one question response was missing for an individual across the four questions, we coded the index missing. Our final sample size for our multivariate analysis on trust was 38,005.3
Similarly, we constructed a satisfaction index based on three highly correlated satisfaction questions from the Household Survey, also mentioned earlier. The universe of respondents for these three satisfaction questions included all adults who completed the self-response module, had a doctor's visit in the past year, and had either a checkup or a visit because of illness. The “satisfaction” index was also calculated by taking the mean response from the relevant questions in the survey. Our final sample size for the multivariate analysis of satisfaction was 32,830.3
To measure the internal reliability of our dependent variables, we calculated Cronbach's α from the questions used to develop our trust and satisfaction indices. The resulting intercorrelation of the variables used to construct both indices was high (trust: α=0.78; satisfaction: α=0.98), which suggests that the number of variables in each index, as well as their average intercorrelation, contributes to our overall confidence in the indices (Knoke and Bohrnstedt 1994).
Independent Variables
One of our key independent variables is race/ethnicity. Race and ethnicity were self-reported in the survey through two separate questions. The first question asked respondents if they considered themselves to be of “Hispanic origin, such as Mexican, Puerto Rican, Cuban, or other Spanish background” and required a yes or no response (Center for Studying Health System Change 2002b). The second question asked respondents: “What race do you consider yourself to be?” The fixed response categories as specified by the survey instrument were: “white,”“African American or Black,”“Native American (American Indian) or Alaska Native,”“Asian or Pacific Islander,” or “other” (Center for Studying Health System Change 2002b). Respondents who self-identified as “mixed race” were coded in the “other” category (Center for Studying Health System Change 2002b). If an individual responded affirmatively to the question of “Hispanic” background, he or she was categorized as “Hispanic,” regardless of the category they selected for race. The remaining categories include only individuals who do not self-identify as “Hispanic.”
Effective communication skills, especially language, are an essential component of the patient–physician relationship (Ferguson and Candib 2002; Collins et al. 2002) . Relationship building between patient and physician via the use of empathy and effective communication skills is critical to forming effective and trusting relationships with patients. We were able to measure language barriers through a crude proxy because our data included information on whether the survey was conducted in Spanish. Using the race/ethnicity questions and the language variable, we constructed a racial/ethnic identifier with the following categories: white, African American, Latino-English speaking, Latino-Spanish speaking, and other (which includes Native American, Asian or Pacific Islander, and other). Ideally, our data would allow for more specific analyses on subgroups including Mexican Americans, Cuban Americans, Native Americans, Asian Americans, and Pacific Islanders. Latino subgroups were not refined down to this level in the survey data. Additionally, we were limited to the “other” category for a number of groups because of small sample sizes. We were concerned that combining such a broad range of racial and ethnic groups into the “other” category would make assumptions about our results difficult because they are so different. Thus, we focus our results and discussion on African Americans, Latinos, and whites and keep the “other” category as a control.
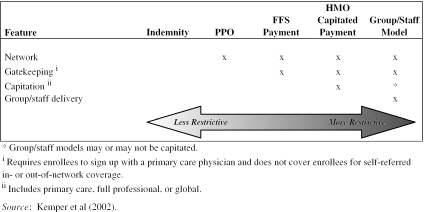
Another key independent variable in explaining differences in trust and satisfaction is health plan payer and type. We were able to measure plan type for about two-thirds of the privately insured. We used the Household and Followback Survey data to construct one insurance type variable that controls for payer (private, Medicare, Medicaid/other public, Military, or uninsured) and plan type (indemnity, preferred provider organization [PPO], or HMO). Figure 1 outlines the factors we used to define the plan type component of this variable, which we derived from Kemper et al.'s (2002) work on insurance product design. We consider HMO plans, particularly capitated payment and group/staff models, to be more restrictive or “tightly managed,” while PPO and indemnity plans are less restrictive or “less managed.” More loosely managed HMOs—those with fee-for-service payment—fall in the middle of our continuum of plan types. Tightly managed plans typically have gatekeeping requirements, physician networks, and capitated payments to providers. Less managed plans generally do not have such restrictions and allow individuals more choice in where they receive their care. We also included a category in our payer/type variable for the remaining one-third of the privately insured for whom followback data were not available. The final variable, therefore, included six categories for the privately insured breaking out plan types (Indemnity, PPO, HMO-FFS payment, HMO-capitated payment, HMO-group/staff model, and type unknown), two categories for publicly insured individuals (Medicare or Medicaid/other public), and one category for the uninsured.
Figure 1.
Description of Plan Types
We also attempted to control for the generosity of a health plan through a proxy—the size of an individual's employer. By plan generosity, we mean the menu of benefits available (preventive, hospital, mental health, etc.) and the associated out-of-pocket payments (copayments, coinsurance, deductibles, etc.). Our proxy for generosity measures the size of a firm that a respondent works for in terms of the number of workers employed by the firm. Larger firms tend to have more generous benefits than smaller firms (GAO 2001; Bundorf 2002; Williams and Lee 2002; Kaiser Family Foundation/HRET 2003). Our firm size variable has the following categories: less than 10 employees, 10–24, 25–99, 100–499, 500–999, 1,000 or more, Government employee, and inapplicable. These categorizations are based on the idea that the two smallest firm size groups have the least generous benefits. We also included a self-reported HMO enrollment variable from the Household Survey to control for self-perceptions of the restrictiveness of the plan. About one-quarter of privately insured people do not correctly report whether they are enrolled in an HMO (Reschovsky, Hargraves, and Smith 2002). And, the type of plan an individual believes himself or herself to be enrolled in affects assessments of health care.
Our model also includes a number of covariates to address predisposing, enabling, need, and medical care factors (Andersen 1995).
Predisposing Factors
We included age and gender as basic demographic variables. Age was broken down into four categories: 18–34, 35–64, 65–79, and 80 years and over. Education was also included, and it was measured as less than high school versus high school or more.
Enabling Factors
Poverty status and county demographics were included as enabling factors. Poverty status is based on family income as a percentage of the federal poverty level (FPL). We included a categorical measure that broke poverty status down into less than 100 percent of FPL, 100–199 percent of FPL, 200–399 percent of FPL, and 400 percent or more of FPL.
We included metropolitan statistical area (MSA) category, county unemployment rate, the percentage of African Americans in a county, and the percentage of Latinos in a county to try to control for local area details that might impact disparities. MSA was measured as over 200,000 residents, under 200,000 residents, or nonmetro area. We also included the CTS site variable in our final model to control for the 60 sites randomly selected for the survey. We included the CTS site variable as an attempt to control for small area variation in services. Previous research indicates that for some racial and ethnic groups, disparities in care are more pronounced in some regions than in others (Chandra and Skinner 2003; Skinner et al. 2003, forthcoming).
Need Factors
Health status was included as a “need” factor. We included two continuous variables to measure physical and mental health status. These continuous variables were based on SF-12 summary scores, a validated measure of health status that ranges from zero to 100 (Ware, Kosinski, and Keller 1996).
Medical Care Factors
Unmet need measures whether an individual reports that he or she did not get or had to put off care when it was necessary. We also looked at whether an individual reported a usual source of care and whether he or she saw the same provider of care at this place. Previous research indicates that continuity of care is associated with better outcomes. Finally, we included utilization, which is measured as whether an individual is a high user of health services or not. We defined high users of health as having four or more doctor visits in the past 12 months and either one overnight hospital stay, one visit to the emergency department, or one surgery during the same time period.
Two of our medical care covariates are potentially endogenous with satisfaction: unmet need and utilization. The direction of causality between these factors and satisfaction is unclear. On the one hand, having an unmet need or being a high user of health care services is related to an individual's satisfaction. On the other, if someone is less satisfied they might not access services, and it would ultimately impact their utilization. Therefore, we do not include these variables in the satisfaction model. In addition, prior research from LaVeist, Nickerson, and Bowie (2000) indicates the importance of trust in a model of satisfaction. Therefore, we included our trust index in the satisfaction model.
Estimation Methodology
The unit of analysis for our models is the individual. We estimated ordinary least squares models to test the effects of race and plan type on trust and satisfaction with physician. We added baseline characteristics, health plan characteristics, and geography characteristics as independent variables. Baseline characteristics include predisposing, enabling, need, and medical care characteristics. Health plan characteristics included plan type, firm size, and self-reported HMO enrollment. And geography characteristics included the CTS site variable.
To maximize our sample size and account for persons who did not respond to certain questions, we included a “missing” category on some variables. Results were considered to be statistically significant at the 5 percent error level. We used SUDAAN to calculate standard errors since our data used complex sampling procedures (Brogan 1998). The data are weighted to extrapolate the results to the characteristics of the national civilian, noninstitutionalized U.S. population, and to account for nonresponse.4
Results
Using more recent CTS Household data (1998–1999), supplemented with the CTS Followback data, our results confirm the earlier findings of Doescher et al. (2000) that perceptions of and satisfaction with physicians vary with race and ethnicity. More importantly, we find that differences in perceptions of trust and satisfaction by race and ethnicity cannot be explained by the restrictiveness of the health plan for the general population. Among the privately insured only, however, differences in satisfaction are explained by the restrictiveness of health plans for African Americans and the Latino-English-speaking subgroup, although it is unclear whether this finding results from lower statistical power.
Descriptive Results
Table 1 provides the sample composition for both of our multivariate analyses.5 The frequency distributions of variables included in the trust and satisfaction analyses were similar. About 66 percent of our sample reported private coverage, and we have plan-specific data from the Followback Survey on two-thirds of respondents who reported private coverage. About three-quarters of our sample respondents were white, 12 percent were African Americans, 9 percent were Latino, and 4 percent fell into the “other” category. Most privately insured individuals were enrolled in a PPO, an HMO with FFS payment, or an HMO with capitated payment.
Table 1.
Sample Composition Adults 18 Years and Older, 1998–1999
| Trust in Physician Sample | Satisfaction with Physician Style Sample | |||
|---|---|---|---|---|
| Independent Variable | Weighted | Unweighted Sample Size | Weighted | Unweighted Sample size |
| Total | 100.0% | 38,005 | 100.0% | 32,830 |
| Race/ethnicity | ||||
| White | 75.2% | 29,498 | 75.9% | 25,654 |
| African American | 11.7% | 4,123 | 11.5% | 3,544 |
| Latino-English speaking | 6.0% | 2,016 | 5.9% | 1,701 |
| Latino-Spanish speaking | 3.4% | 988 | 3.1% | 787 |
| Other | 3.7% | 1,380 | 3.6% | 1,144 |
| Age (years) | ||||
| 18–34 | 31.3% | 11,172 | 30.2% | 9,352 |
| 35–64 | 52.3% | 21,224 | 52.1% | 18,274 |
| 65–79 | 13.4% | 4,665 | 14.5% | 4,327 |
| 80 and older | 3.0% | 944 | 3.2% | 877 |
| Gender | ||||
| Female | 54.8% | 21,633 | 57.9% | 19,589 |
| Male | 45.2% | 16,372 | 42.1% | 13,241 |
| Federal poverty index (FPL) | ||||
| <100% FPL | 11.4% | 3,483 | 11.0% | 2,894 |
| 100–199% FPL | 16.4% | 5,538 | 16.1% | 4,664 |
| 200–399% FPL | 34.4% | 12,598 | 34.4% | 10,864 |
| 400% or more FPL | 37.8% | 16,386 | 38.5% | 14,408 |
| Education | ||||
| Less than high school | 14.2% | 4,261 | 13.6% | 3,549 |
| High school or more | 85.8% | 33,744 | 86.4% | 29,281 |
| MSA category | ||||
| Large metro over 200,000 | 71.5% | 32,160 | 71.9% | 27,903 |
| Small metro under 200,000 | 6.8% | 1,294 | 6.9% | 1,100 |
| Nonmetro area | 21.7% | 4,551 | 21.3% | 3,827 |
| Physical health status (SF-12 summary score) | 45.5% | 38,005 | 47.9% | 32,830 |
| Mental health status (SF-12 summary score) | 52.2% | 38,005 | 52.0% | 32,830 |
| Unmet health care needs | ||||
| Have unmet or putoff health care needs | 25.5% | 9,534 | NA | NA |
| Do not have unmet/putoff health care needs | 74.3% | 28,409 | NA | NA |
| Missing values | 0.2% | 62 | NA | NA |
| Usual source of care | ||||
| Have a usual source of care and same provider | 78.8% | 30,404 | 79.4% | 26,437 |
| 13.4% | 4,852 | 11.8% | 3,737 | |
| Have a usual source of care and same provider | ||||
| No usual source of care | 7.0% | 2,462 | 8.2% | 2,433 |
| Missing values | 0.8% | 287 | 0.7% | 223 |
| Utilization | ||||
| Not a high user of health care services | 80.2% | 30,498 | NA | NA |
| High user of health care services | 19.8% | 7,507 | NA | NA |
| Mean county unemployment rate (1998) | 4.5% | 38,005 | 4.5% | 32,830 |
| Mean percentage of African Americans residing in county (1998) | 12.7% | 38,005 | 12.7% | 32,830 |
| Mean percentage of Latinos residing in county (1998) | 9.4% | 38,005 | 9.3% | 32,830 |
| Trust in physician (mean score) | NA | 4.1% | 32,830 | |
| Index of health plan type | ||||
| Private, indemnity | 1.9% | 795 | 2.0% | 712 |
| Private, PPO | 12.7% | 5,093 | 12.7% | 4,424 |
| Private, HMO—FFS payment | 10.8% | 4,951 | 11.1% | 4,383 |
| Private, HMO—capitated payment | 7.5% | 3,258 | 7.8% | 2,881 |
| Private, HMO—group/staff model | 1.7% | 762 | 1.7% | 660 |
| Private, type unknown | 31.0% | 11,667 | 30.6% | 9,945 |
| Medicare | 18.9% | 6,418 | 20.3% | 5,951 |
| Medicaid/other public | 4.8% | 1,620 | 4.8% | 1,418 |
| Uninsured | 10.8% | 3,441 | 9.0% | 2,456 |
| Size of firm respondent works for | ||||
| <10 employees | 11.2% | 4,234 | 10.6% | 3,469 |
| 10–24 employees | 5.5% | 2,098 | 5.2% | 1,731 |
| 25–99 employees | 7.3% | 2,760 | 6.9% | 2,265 |
| 100–499 employees | 7.9% | 3,076 | 7.7% | 2,564 |
| 500–999 employees | 2.6% | 1,025 | 2.6% | 898 |
| 1,000 or more employees | 17.9% | 7,072 | 17.8% | 6,102 |
| Government employee | 10.5% | 4,386 | 10.8% | 3,891 |
| Not applicable | 37.1% | 13,354 | 38.4% | 11,910 |
| Respondent reported enrollment in an HMO | ||||
| No | 30.4% | 11,992 | 30.5% | 10,376 |
| Yes | 33.8% | 13,977 | 34.1% | 12,168 |
| Missing | 35.8% | 12,036 | 35.4% | 10,286 |
Source: Center for Studying Health System Change (1998); Community Tracking Study 1998–1999 Household and Followback Surveys, excluding children and those in the military.
NA, not applicable.
Table 2 presents some descriptive results for our indices. In order to show the variation of responses by race and ethnicity, we also included the frequencies for the variables used to construct our indices. The variables used to construct our trust and satisfaction indices suggest that the general population is highly trusting of its physicians and, for the most part, satisfied with the care they are receiving. On average, people tend to respond to these questions with a high rating—they tend to somewhat or strongly agree with the trust questions, and they tend to rate elements of their last visit to the doctor as very good or excellent. Responding any lower is not the “norm.”Table 2 shows, however, that African Americans, Latinos, and others are less trusting and less satisfied with their physicians than whites—almost all of these differences are statistically significant (see table footnote for exception). For example, three-quarters of whites responded that the thoroughness of their last exam was very good or excellent while only about half of Latino-Spanish-speaking respondents responded in the same way. Thus, the satisfaction index difference between white and Latino-Spanish-speaking respondents indicates that whites are more likely to provide responses on the higher end of the scale.
Table 2.
Trust and Satisfaction Measures and Indices by Race (Unadjusted) Adults 18 Years and Older, 1998–1999
| Percent Who Somewhat/Strongly Agree with the Statement … | Percent Who Rate the Following as Very Good or Excellent… | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Independent Variable | Doctor Refers to a Specialist When Needed* | Trust Doctor to Put Medical Needs Above All Other Considerations When Treating Medical Problems | The Doctor Is Not Strongly Influenced by Health Insurance Company Rules When Making Decisions about Medical Care* | The Doctor Does Not Perform Unecessary Tests or Proceduresa | Trust in Provider Index | Thoroughness/Carefulness of Last Exam Received | How Well the Doctor Listened | How Well the Doctor Explained Things | Satisfaction with Physician Style Index |
| Total population | 83 | 92 | 54 | 86 | 4.09 | 72 | 75 | 76 | 4.05 |
| Race/ethnicity | |||||||||
| White | 86 | 93 | 58 | 88 | 4.17 | 76 | 78 | 79 | 4.12 |
| African American | 79 | 92 | 42 | 81 | 3.89 | 64 | 69 | 70 | 3.90 |
| Latino-English speaking | 76 | 88 | 45 | 81 | 3.85 | 62 | 64 | 67 | 3.80 |
| Latino-Spanish speaking | 67 | 88 | 38 | 75 | 3.67 | 48 | 55 | 56 | 3.61 |
| Other | 76 | 89 | 47 | 79 | 3.84 | 57 | 62 | 65 | 3.74 |
Source: Center for Studying Health System Change (1998); Community Tracking Survey 1998–1999 Household Survey, excluding children and those in the military.
These variables were recoded from their original format.
Note: All race/ethnicity categories are statistically different from whites at least at the 95% level, with one exception. For “the doctor is not strongly influenced by health insurance company rules when making decisions,” African-American responses are not statistically different from those of whites.
Multivariate Results
Levels of trust in and satisfaction with physician vary significantly by race even after controlling for predisposing, enabling, and need factors as well as medical care factors. Key results from our multivariate analyses are presented in Tables 3 and 4. In the satisfaction model, the baseline characteristics appear to have a larger effect on race estimates, but race is still significant. The estimates for race are much higher when trust is excluded from the model. This finding suggests that trust is an important intervening factor in the relationship between race and satisfaction.
Table 3.
Effects of Race and Plan Type on Provider Trust—Key Multivariate Results Adults and 18 Years and Older, 1998–1999
| Unadjusted | Adjusted for Baseline Characteristics | Adjusted for Baseline and Health Plan Characteristics | ||||
|---|---|---|---|---|---|---|
| β | p | β | p | β | p | |
| Total number of observations in analysis | 38,005 | 38,005 | 38,005 | |||
| Intercept | 4.1749 | 0 | 3.2822 | 0 | 3.3688 | 0 |
| Race/ethnicity | ||||||
| White | Reference | Reference | Reference | |||
| African American | −0.2830 | 0 | −0.2064 | 0 | −0.1905 | 0 |
| Latino-English speaking | −0.3205 | 0 | −0.1959 | 0 | −0.1838 | 0 |
| Latino-Spanish speaking | −0.5070 | 0 | −0.2742 | .0003 | −0.2547 | .0005 |
| Other | −0.3319 | 0 | −0.2514 | 0 | −0.2458 | 0 |
| Age (years) | ||||||
| 18–34 | Reference | Reference | ||||
| 35–64 | 0.0537 | .0003 | 0.0407 | .0057 | ||
| 65–79 | 0.1695 | 0 | 0.0397 | .2117 | ||
| 80 and older | 0.0975 | .0079 | −0.0304 | .4123 | ||
| Gender | ||||||
| Female | Reference | Reference | ||||
| Male | −0.1701 | 0 | −0.1684 | 0 | ||
| Federal poverty index (FPL) | ||||||
| <100% FPL | −0.1223 | 0 | −0.1232 | 0 | ||
| 100–199% FPL | −0.0569 | .0014 | −0.0496 | .0053 | ||
| 200–399% FPL | −0.0296 | .0134 | −0.0247 | .0292 | ||
| 400% or more FPL | Reference | Reference | ||||
| Education | ||||||
| Less than high school | Reference | Reference | ||||
| High school or more | 0.1299 | 0 | 0.1260 | 0 | ||
| MSA category | ||||||
| Large metro over 200,000 | Reference | Reference | ||||
| Small metro under 200,000 | 0.0170 | .2486 | −0.0033 | .8278 | ||
| Nonmetro area | 0.0015 | .9650 | −0.0134 | .6841 | ||
| Physical health status | 0.0028 | 0 | 0.0035 | 0 | ||
| Mental health status | 0.0096 | 0 | 0.0097 | 0 | ||
| Unmet health care needs | ||||||
| Have unmet/put off health care needs | Reference | Reference | ||||
| No unmet/put off health care needs | 0.2886 | 0 | 0.2764 | 0 | ||
| Missing values | 0.0084 | .9631 | 0.0057 | .9739 | ||
| Usual source of care | ||||||
| Have a usual source of care and same provider | Reference | Reference | ||||
| −0.3180 | 0 | −0.3085 | 0 | |||
| Have usual source of care but different provider | ||||||
| No usual source of care | −0.3264 | 0 | −0.3227 | 0 | ||
| Missing values | −0.4453 | 0 | −0.4342 | 0 | ||
| Utilization | ||||||
| Not a high user of health care services | Reference | Reference | ||||
| High user of health care services | 0.1385 | 0 | 0.1331 | 0 | ||
| County unemployment rate (1998) | 0.0015 | .7774 | 0.0009 | .8496 | ||
| Percent African Americans residing in county (1998) | 0.0007 | .1587 | 0.0005 | .3716 | ||
| Percent Latinos residing in county (1998) | −0.0019 | .1305 | −0.0014 | .2186 | ||
| Index of health plan type | ||||||
| Private, indemnity | 0.0366 | .2457 | ||||
| Private, PPO | Reference | |||||
| Private, HMO—FFS payment | −0.0125 | .5401 | ||||
| Private, HMO—capitated payment | −0.1116 | .0000 | ||||
| Private, HMO—group/staff model | −0.1752 | .0000 | ||||
| Private, type unknown | −0.0340 | .0192 | ||||
| Medicare | 0.1109 | .0017 | ||||
| Medicaid/other public | −0.0014 | .9716 | ||||
| Uninsured | −0.0731 | .0468 | ||||
| Size of firm respondent works for | ||||||
| <10 employees | 0.0003 | .9861 | ||||
| 10–24 employees | 0.0168 | .4712 | ||||
| 25–99 employees | −0.0007 | .9744 | ||||
| 100–499 employees | −0.0177 | .3407 | ||||
| 500–999 employees | 0.0155 | .6265 | ||||
| 1,000 or more employees | Reference | |||||
| Government employee | 0.0269 | .0909 | ||||
| Inapplicable | 0.0282 | .0560 | ||||
| Respondent reported enrollment in an HMO | ||||||
| No | Reference | |||||
| Yes | −0.1493 | 0 | ||||
| Missing | −0.1137 | .0001 | ||||
| R2 | 2.87% | 12.59% | 13.49% | |||
Source: Center for Studying Health System Change (1998); Community Tracking Study 1998–1999 Household and Followback Surveys, excluding children and those in the military.
p<.05;
p<.01;
p<.001.
Table 4.
Effects of Race and Plan Type on Satisfaction with Provider Care—Key Multivariate Results Adults 18 Years and Older, 1998–1999
| Unadjusted | Adjusted for Baseline Characteristics | Adjusted for Baseline and Health Plan Characteristics | ||||
|---|---|---|---|---|---|---|
| β | p | β | p | β | p | |
| Total number of observations in analysis | 32,830 | 32,830 | 32,830 | |||
| Intercept | 4.1194 | 0 | 1.8267 | 0 | 1.7432 | 0 |
| Race/ethnicity | ||||||
| White | Reference | Reference | ||||
| African American | −0.2196 | 0 | −0.0750 | .0001 | −0.0739 | .0002 |
| Latino-English speaking | −0.3157 | 0 | −0.1343 | .0001 | −0.1303 | .0001 |
| Latino-Spanish speaking | −0.5049 | 0 | −0.2286 | .0001 | −0.2198 | .0001 |
| Other | −0.3801 | 0 | −0.2161 | 0 | −0.2168 | 0 |
| Age (years) | ||||||
| 18–34 | Reference | Reference | ||||
| 35–64 | 0.1045 | 0 | 0.0979 | 0 | ||
| 65–79 | 0.1465 | 0 | 0.0108 | .7625 | ||
| 80 and older | 0.0960 | .0082 | −0.0401 | .4323 | ||
| Gender | ||||||
| Female | Reference | Reference | ||||
| Male | −0.0897 | 0 | −0.0857 | 0 | ||
| Federal poverty index (FPL) | ||||||
| <100% FPL | −0.0433 | .0940 | −0.0649 | .0139 | ||
| 100–199% FPL | −0.0498 | .0081 | −0.0549 | .0078 | ||
| 200–399% FPL | −0.0398 | .0006 | −0.0416 | .0002 | ||
| 400% or more FPL | Reference | Reference | ||||
| Education | ||||||
| Less than high school | Reference | Reference | ||||
| High school or more | −0.0179 | .4243 | −0.0126 | .5714 | ||
| MSA category | ||||||
| Large metro over 200,000 | Reference | Reference | ||||
| Small metro under 200,000 | 0.0184 | .3676 | 0.0163 | .3980 | ||
| Nonmetro area | −0.0051 | .8002 | −0.0059 | .7675 | ||
| Physical health status | 0.0040 | 0 | 0.0049 | 0 | ||
| Mental health status | 0.0088 | 0 | 0.0092 | 0 | ||
| Usual source of care | ||||||
| Have a usual source of care and same provider | Reference | Reference | ||||
| Have usual source of care but different provider | −0.1671 | 0 | −0.1605 | 0 | ||
| No usual source of care | −0.1561 | 0 | −0.1478 | 0 | ||
| Missing values | −0.2518 | .0001 | −0.2471 | .0001 | ||
| County unemployment rate (1998) | 0.0009 | .8630 | 0.0000 | 1.0000 | ||
| Percent African Americans residing in county (1998) | 0.0006 | .3077 | 0.0006 | .2996 | ||
| Percent Latinos residing in county (1998) | −0.0006 | .4226 | −0.0004 | .5473 | ||
| Trust in physician | 0.3952 | 0 | 0.3913 | 0 | ||
| Index of health plan type | ||||||
| Private, Indemnity | 0.0245 | .4967 | ||||
| Private, PPO | Reference | |||||
| Private, HMO—FFS payment | 0.0025 | .9217 | ||||
| Private, HMO—capitated payment | −0.0664 | .0147 | ||||
| Private, HMO—group/staff model | −0.0774 | .0739 | ||||
| Private, Type unknown | −0.0033 | .8761 | ||||
| Medicare | 0.1050 | .0394 | ||||
| Medicaid/other public | 0.0417 | .3572 | ||||
| Uninsured | −0.0728 | .1381 | ||||
| Size of firm respondent works for | ||||||
| <10 employees | 0.0512 | .0295 | ||||
| 10–24 employees | 0.0333 | .3134 | ||||
| 25–99 employees | 0.0510 | .1239 | ||||
| 100–499 employees | 0.0244 | .3078 | ||||
| 500–999 employees | −0.0273 | 4946 | ||||
| 1,000 or more employees | Reference | |||||
| Government employee | 0.0541 | .0659 | ||||
| Inapplicable | 0.0794 | .0001 | ||||
| Respondent reported enrollment in an HMO | ||||||
| No | Reference | |||||
| Yes | 0.0086 | .5016 | ||||
| Missing | 0.0021 | .9442 | ||||
| R2 | 2.19% | 20.09% | 20.33% | |||
Source: Center for Studying Health System Change (1998); Community Tracking Study 1998–1999 Household and Followback Surveys, excluding children and those in the military.
p<.05;
p<.01;
p<.001.
More importantly, when we add health plan characteristics to our trust and satisfaction models, we see no substantial difference in our coefficients for race.6 We fail to reject our null hypothesis that controlling for the type of health plan in which an individual is enrolled would reduce disparities in trust and satisfaction. We did confirm, however, that enrollment in a tightly managed HMO plan (capitated or group model) is significantly associated with lower levels of trust in physician compared with enrollment in a PPO plan. Enrollment in a capitated model HMO plan is significantly associated with lower levels of satisfaction compared with a PPO plan. We also found that among individuals for whom Followback data were not collected (private, type unknown), levels of trust were lower compared with individuals enrolled in a PPO plan. Finally, estimates for the uninsured were significant and indicated lower levels of trust. Medicare enrollees tended to have higher levels of trust and satisfaction compared with individuals enrolled in a PPO plan even though we controlled for age. Finally, we added the CTS site variable to our multivariate analyses. The addition of the site variable had little to no impact on our race estimates.
To check the robustness of our results, we also ran our analyses for different subsamples based on length of time since the respondent's last visit to the doctor. We wanted to be sure that there was no negative relationship between time and satisfaction. We constructed a variable that indicated the number of months that had passed between a respondent's survey interview date and his or her last visit to the doctor. About half the sample had seen a doctor within 7 months of their interview. Our results showed that that there is not necessarily a negative relationship between time and satisfaction. In fact, the magnitude of our estimates for the Latino-Spanish-speaking and Native American/Asian/Pacific Islander/other subgroups suggested that satisfaction with physician care was better for respondents who had not been to the doctor for 8 or more months. Importantly, analyzing the data based on this time construct did not dramatically change our results.
The CTS Household file includes some self-reported information regarding health plan restrictiveness from individuals insured by private or Medicare plans. Because we lost a number of observations on the privately insured because of Followback study nonresponse (the private, type unknown group), we re-constructed our insurance variable to include self-reported data on whether the plan requires an individual to sign up with a specific doctor from the Household survey. This test also allowed us to see whether individuals' perceptions had any impact on our results. The self-reported measure was not significant, and this change had little to no impact on our original β estimates for race and ethnicity.
Since individuals who are less satisfied with their care tend to switch providers and plans, we re-ran our models to include a control for whether a respondent was covered by a different plan or uninsured in the previous year. Individuals who switched plans in the past year might be more satisfied with their new plans. When we included this variable in our models it was not significant, and it had no impact on our race and ethnicity estimates.
Finally, we re-ran our models for the privately insured population only, including observations from the Followback sample only. The trust estimates for the Latino-Spanish-speaking population was slightly smaller in magnitude while the Native American/Asian/Pacific Islander/other estimate grew in magnitude—both remained statistically significant. Our satisfaction estimates, however, changed in more meaningful ways. The β estimates for the African-American and Latino-English-speaking populations were no longer significant. At the same time, the estimate for the Latino-Spanish-speaking population nearly doubled in size. These findings must be interpreted with caution because the sample size for these analyses is much smaller than in our general model (<15,000 versus >38,000), and we lose the 9,000+ privately insured individuals who did not participate in the Followback survey. We may not have enough statistical power to detect differences within this subsample.
It is possible that some of the covariates, particularly our medical care variables, could be endogenously determined by the health plan variable in our satisfaction model and we therefore did not include unmet need and utilization as part of this model. However, we did include usual source of care in our satisfaction model. If endogeneity was an issue in either of our models, the coefficients on the race variables could be estimated with some bias. To explore this possibility, we eliminated every covariate from the base trust and satisfaction models that conceivably could be jointly determined with health plan choices, but did not observe a change in the results.
Discussion
Our work suggests that plan type does not explain why some minority groups receive worse care or are less satisfied with their care. We find that for all populations health plan type is not a confounding factor in the relationship between race/ethnicity and trust and satisfaction with physician—the disparate distribution of individuals across health plan types does not help to explain differences in perceptions of trust and satisfaction by race and ethnicity. When we restrict our analysis to the privately insured respondents for whom we have Followback study data, however, the satisfaction model estimates for African-American and Latino-English-speaking respondents are no longer different than those for whites. This finding bears further investigation, but it should be interpreted with caution because of the model's limited statistical power.
More importantly, our analyses suggest that the differential distribution of individuals across health plan types is not a mitigating factor in the relationship between race/ethnicity and trust and satisfaction with physician. The results of our work both confirm and add to earlier findings by Doescher et al. (2000) on racial and ethnic disparities in trust and satisfaction. Doescher et al. similarly found that minorities have lower levels of trust and satisfaction when controlling for demographics, access, health status, and health system utilization. We add to their study by including more specific health plan details for the privately insured population.
Lastly, we found that baseline characteristics had a larger effect on the estimates in the satisfaction model than in the trust model. This may in large part be because of the fact that trust is included as a control variable in the satisfaction model. Previous research has actually found the addition of “mistrust,” along with a variable that measures perceptions of racism, to a satisfaction model completely removed the effects of race (LaVeist, Nickerson, and Bowie 2000).
Limitations
Our model has several limitations. First, we were constrained to several crude proxies—communication barriers are one example. We used a variable indicating whether or not the survey was conducted in Spanish to control for communication barriers in our models, which is not a perfect measure for communication barriers. Since our estimates for Latino-Spanish speaking are significant and strong in magnitude, we know this is an important construct that needs further investigation in future research. Our coefficients are likely somewhat conservative.
In addition, measurement of trust is an emerging science, and the questions we use from the CTS instrument were based on questions that were under development to measure public opinion on physician trust (Center for Studying Health System Change 1998). The questions that eventually emerged from that larger trust scale were later modified and validated through psychometric analysis (Kao et al. 1998). It is important to note, however, that patients' trust in physicians could potentially be influenced by other perceptions for which we are unable to control, such as trust in an individual's health plan (Kao et al. 1998).
We did not have data on physician–patient racial concordance, which is an important intervening factor in patient trust and satisfaction (Saha et al. 1999; LaVeist and Nuru-Jeter 2002). Since minority individuals are less likely to have racially concordant physicians than whites, this would suggest that our satisfaction, and probably our trust estimates, may be conservative (LaVeist and Nuru-Jeter 2002).
We were unable to control for the restrictiveness of Medicaid plans. The CTS does not include any detailed information on this issue. However, we ran our models separately for the Medicaid population versus the non-Medicaid population and found that trust and satisfaction levels are actually higher among Medicaid beneficiaries.
Finally, nonresponse for both our dependent variables and for the Followback Survey could skew the findings. We checked the distribution of race and ethnicity in both eligible sample and final sample and found that it was nearly identical for both the trust and satisfaction questions—meaning that bias because of question nonresponse is controlled. As for the Followback Survey, data are missing for about 40 percent of the privately insured, who were more likely to be racial minorities. They also had lower levels of trust, but no differences with respect to satisfaction. To control for nonresponse, we included the category, “Private, Type Unknown,” in our insurance type variable. In additional sensitivity analyses, we were able to use some self-reported data on plan restrictiveness for respondents identified as “Private, Type Unknown,” which did not influence our race/ethnicity estimates.
Conclusion
After controlling for the type of health plan in which an individual was enrolled, we found that racial and ethnic differences in trust and satisfaction with physicians remain. The only exception to this finding emerges in the satisfaction analysis restricted to the Followback study sample, which should be interpreted with caution because of its limited sample size. These results merit further study in order to understand whether they are an issue of statistical power or a real finding.
The results of our study of the overall population demonstrate a need to better understand the health care-related factors that drive disparate trust and satisfaction. Our findings suggest that trust and satisfaction should be carefully considered as interventions are designed to address racial and ethnic disparities in health care. In evaluating programs designed to reduce disparities in trust and satisfaction, we need the ability to measure patient assessments of care as well as other health outcomes. Such data would allow us to address trust and satisfaction on all levels because these issues have been linked to patient assessments of health care (Morales et al. 2001), service utilization (Zastowny, Roghmann, and Cafferata 1998), the decision to switch health plans (Newcomer, Preston, and Harrington 1996; Allen and Rogers 1997; Schlesinger, Druss, and Thomas 1999), and treatment compliance (Hall and Dornan 1990). By implementing programs to reduce disparities in trust and satisfaction, we may be able to impact these other related outcomes.
Acknowledgments
The authors would like to thank Joseph Betancourt, J. Lee Hargraves, James Knickman, James Reschovsky, and Brian Smedley for their comments on an earlier version of this work. The interpretations and opinions are those of the authors and may not necessarily reflect those of The Robert Wood Johnson Foundation.
Notes
Since the Followback Survey was based on the group of individuals who reported private insurance coverage, it does not have a response rate. The “match rate” is simply the percentage of individuals from the privately insured group for whom CTS researchers were able to collect Followback data. The number of respondents who reported private coverage in the household sample was 37,486, and the survey firm contacted 22,235 organizations associated with these individuals' plans.
The response scale for the question: “I trust my doctor to put my medical needs above all other considerations when treating my medical problems” was in the opposite direction of the other three trust questions. We recoded this question prior to creating the index.
In all, we lose about 10% of the sample eligible to answer a trust or satisfaction question, which was cause for some concern. Therefore, we looked at the distribution of race/ethnicity for both the sample eligible to respond to one of these questions and our final sample, and it looked nearly identical for both groupings.
As mentioned, the Followback Survey did not reach the entire privately insured group. Therefore, the sample weights for the entire study population do not control for nonresponse in the Followback Survey. We ran our analyses on the full adult sample using the national sample weights. To test the extent to which this may have biased our estimates, we re-ran our analysis using a weight constructed of the national sample weight for nonprivately insured individuals and the followback weight for privately insured individuals. We excluded privately insured cases that were not matched to the Followback Survey. We found that the results were reasonably similar to our original analysis.
Descriptive data for the CTS site variable are not presented in Table 1 because of space considerations.
We also re-ran our model to include individual variables for the specific rules of private health plans as reported by employers and plans in the CTS followback study data, rather than the large groupings of these rules. For our trust model, we found that our new β estimates for race and ethnicity were still statistically significant and in the right direction. The magnitude of the estimates was comparable to our original estimates. For our satisfaction model, we found the same. The estimate for “Latino-Spanish Speaking” showed a marked increased in magnitude (−0.3515), suggesting that our original estimates for this group were conservative.
References
- Allen HM, Rogers WH. “The Consumer Health Plan Value Survey: Round Two.”. Health Affairs. 1997;16(4):156–66. doi: 10.1377/hlthaff.16.4.156. [DOI] [PubMed] [Google Scholar]
- Andersen RM. “Revisiting the Behavioral Model and Access to Medical Care; Does It Matter?”. Journal of Health and Social Behavior. 1995;36:1–10. [PubMed] [Google Scholar]
- Auslander WF, Thompson SJ, Dreitzer D, Santiago JV. “Mothers' Satisfaction with Medical Care: Perceptions of Racism, Family Stress, and Medical Outcomes in Children with Diabetes.”. Health and Social Work. 1997;22(3):190–9. doi: 10.1093/hsw/22.3.190. [DOI] [PubMed] [Google Scholar]
- Brogan D. “Software for Survey Data, Misuse of Standard Packages.”. In: Armitage P, Colton T, editors. Encyclopedia of Biostatistics. Boston: John Wiley and Sons; 1998. [Google Scholar]
- Bundorf MK. “Employee Demand for Health Insurance and Employer Health Plan Choices.”. Health Economics. 2002;21:65. doi: 10.1016/s0167-6296(01)00127-8. [DOI] [PubMed] [Google Scholar]
- Center for Studying Health System Change . Community Tracking Study. Household Survey. Survey Methodology Report (Round One), Technical Publication No. 15. Washington, DC: Center for Studying Health System Change; 1998. [Google Scholar]
- Center for Studying Health System Change . Community Tracking Study. Followback Survey Data Files. Washington, DC: Center for Studying Health System Change; 2000. [Google Scholar]
- Center for Studying Health System Change . Community Tracking Study. Followback Survey Methodology Report (Round 2), Technical Publication No. 35. Washington, DC: Center for Studying Health System Change; 2002a. [Google Scholar]
- Center for Studying Health System Change . Community Tracking Study. Household Survey Restricted Use File: Users' Guide (Round 2, Release 2). Technical Publication No. 23. Washington, DC: Center for Studying Health System Change; 2002b. [Google Scholar]
- Chandra A, Skinner J. “Geography and Racial Health Disparities.”. 2003. NBER Working Paper No. w9513.
- Collins KS, Hughes DL, Doty MM, Ives BL, Edwards JN, Tenney K. Diverse Communities, Common Concerns: Assessing Health Care Quality for Minority Americans. New York: The Commonwealth Fund; 2002. [Google Scholar]
- Corbie-Smith G, Thomas SB, St. George DMM. “Distrust, Race, and Research.”. Archives of Internal Medicine. 2002;162:2458–63. doi: 10.1001/archinte.162.21.2458. [DOI] [PubMed] [Google Scholar]
- Doescher MP, Saver BG, Franks P, Fiscella K. “Racial and Ethnic Disparities in Perceptions of Physician Style and Trust.”. Archives of Family Medicine. 2000;9:1156–63. doi: 10.1001/archfami.9.10.1156. [DOI] [PubMed] [Google Scholar]
- Ferguson WJ, Candib LM. “Culture, Language, and the Doctor–Patient Relationship.”. Family Medicine. 2002;34(5):353–61. [PubMed] [Google Scholar]
- Forrest CB, Shi L, von Schrader S, Ng J. “Managed Care, Primary Care, and the Patient–Practitioner Relationship.”. Journal of General Internal Medicine. 2002;17:270–7. doi: 10.1046/j.1525-1497.2002.10309.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- General Accounting Office 2001 Private Health Insurance: Small Employers Continue to Face Challenges in Providing Coverage. GAO-02-8. Washington, DC. [Google Scholar]
- Haas JS, Phillips KA, Baker LC, Sonneborn D, McCulloch CE. “Is the Prevalence of Gatekeeping in a Community Associated with Individual Trust in Managed Care?”. Medical Care. 2003;41(5):660–8. doi: 10.1097/01.MLR.0000062703.14190.61. [DOI] [PubMed] [Google Scholar]
- Hall JA, Dornan MC. “Patient Sociodemographic Characteristics as Predictors of Satisfaction with Medical Care: A Meta-Analysis.”. Social Science and Medicine. 1990;30(7):811–8. doi: 10.1016/0277-9536(90)90205-7. [DOI] [PubMed] [Google Scholar]
- The Kaiser Family Foundation and Health Research and Educational Trust 2003. Employer Health Benefits Survey 2003.
- Kao AC, Green DC, Zaslavsky AM, Koplan JP, Cleary PD. “Journal of the American Medical Association.”. 1998;280(19):1708–14. doi: 10.1001/jama.280.19.1708. [DOI] [PubMed] [Google Scholar]
- Kemper P, Blumenthal D, Corrigan JM, Cunningham PJ, Felt SM, Grossman JM, Kohn LT, Metcalf CE, St. Peter RF, Strouse RC, Ginsburg PB. “The Design of the Community Tracking Study: A Longitudinal Study of Health System Change and Its Effects on People.”. Inquiry. 1996;33:195–206. [PubMed] [Google Scholar]
- Kemper P, Tu HT, Reschovsky JD, Schaefer E. “Insurance Product Design and Its Effects: Trade-Offs Along the Managed Care Continuum.”. Inquiry. 2002;39:101–17. doi: 10.5034/inquiryjrnl_39.2.101. [DOI] [PubMed] [Google Scholar]
- Knoke D, Bohrnstedt GW. Statistics for Social Data Analysis. Illinois: F.E. Peacock Publishers, Inc; 1994. [Google Scholar]
- LaVeist TA, Nickerson KJ, Bowie JV. “Attitudes about Racism, Medical Mistrust, and Satisfaction with Care among African American and White Cardiac Patients.”. Medical Care Research and Review. 2000;57(suppl 1):146–61. doi: 10.1177/1077558700057001S07. [DOI] [PubMed] [Google Scholar]
- LaVeist TA, Nuru-Jeter A. “Is Doctor–Patient Race Concordance Associated with Greater Satisfaction with Care?”. Journal of Health and Social Behavior. 2002;43(September):296–306. [PubMed] [Google Scholar]
- Meredith LS, Sui AL. “Variation and Quality of Self-Report Health Data.”. Medical Care. 1995;33(11):1120–31. doi: 10.1097/00005650-199511000-00005. [DOI] [PubMed] [Google Scholar]
- Metcalf CE, Kemper P, Kohn LT, Pickreign JD. “Site Definition and Sample Design for the Community Tracking Study.”. 1996. Technical Publication No. 1 Washington, DC: Center for Studying Health System Change.
- Morales LS, Cunningham WE, Brown JA, Liu H, Hays RD. “Are Latinos Less Satisfied with Communications by Health Care Providers?”. Journal of General Internal Medicine. 1999;14:409–17. doi: 10.1046/j.1525-1497.1999.06198.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morales LS, Elliott MN, Weech-Maldonado R, Spritzer KL, Hays RD. “Differences in CAHPS© Adult Survey Reports and Ratings by Race and Ethnicity: An Analysis of the National CAHPS© Benchmarking Data 1.”. Health Services Research. 2001;36(3):595–617. [PMC free article] [PubMed] [Google Scholar]
- Murray-García JL, Selby JV, Schmittdiel J, Grumbach K, Quesenberry CP. “Racial and Ethnic Differences in a Patient Survey: Patients' Values, Ratings, and Reports Regarding Physician Primary Care Performance in a Large Health Maintenance Organization.”. Medical Care. 2000;38(3):300–10. doi: 10.1097/00005650-200003000-00007. [DOI] [PubMed] [Google Scholar]
- Newcomer R, Preston S, Harrington C. “Health Plan Satisfaction and Risk of Disenrollment among Social/HMO and Fee-for-service Recipients.”. Inquiry. 1996;33:144–54. [PubMed] [Google Scholar]
- Phillips KA, Mayer ML, Aday LA. “Barriers to Care among Racial/Ethnic Groups under Managed Care.”. Health Affairs. 2000;19(4):65–75. doi: 10.1377/hlthaff.19.4.65. [DOI] [PubMed] [Google Scholar]
- Reschovsky JD, Hargraves JL, Smith AF. “Consumer Beliefs and Health Plan Performance: It's Not Whether You Are in an HMO but Whether You Think You Are.”. Journal of Health Politics, Policy and Law. 2002;27(3):353–77. doi: 10.1215/03616878-27-3-353. [DOI] [PubMed] [Google Scholar]
- Reschovsky JD, Kemper P, Tu H. “Does Type of Health Insurance Affect Health Care Use and Assessments of Care among the Privately Insured?”. Health Services Research. 2000;35(1):219–37. [PMC free article] [PubMed] [Google Scholar]
- Saha S, Komaromy M, Koepsell TD, Bindman AB. “Patient–Physician Racial Concordance and the Perceived Quality and Use of Health Care.”. Archives of Internal Medicine. 1999;159:997–1004. doi: 10.1001/archinte.159.9.997. [DOI] [PubMed] [Google Scholar]
- Schlesinger M, Druss B, Thomas T. “No Exit?”. Health Services Research. 1999;34:547–76. [PMC free article] [PubMed] [Google Scholar]
- Shi L, Forrest CB, von Schrader S, Ng J. “Vulnerability and the Patient–Practitioner Relationship: The Roles of Gatekeeping and Primary Care Performance.”. American Journal of Public Health. 2003;93(1):138–45. doi: 10.2105/ajph.93.1.138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Skinner J, Weinstein JN, Sporer SM, Wennberg JE. “Racial, Ethnic, and Geographic Disparities in Rates of Knee Arthroplasty among Medicare Patients.”. New England Journal of Medicine. 2003;349(14):1350–59. doi: 10.1056/NEJMsa021569. [DOI] [PubMed] [Google Scholar]
- Skinner JS, Weinstein JN, Sporer SM, Wennberg JE. “Racial Ethnic, and Geographic Disparity in Knee Arthroplasty in Medicare Patients.”. New England Journal of Medicine. 349:1350–9. doi: 10.1056/NEJMsa021569. forthcoming. [DOI] [PubMed] [Google Scholar]
- Smedley BD, Stith AY, Nelson AR. Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care. Washington, DC: National Academy Press; 2002. Editors. [PubMed] [Google Scholar]
- Taira DA, Safran DG, Seto TB, Rogers WH, Kosinski M, Ware JE, Lieberman N, Tarlov AR. “Asian-American Patient Ratings of Physician Primary Care Performance.”. Journal of General Internal Medicine. 1997;12(April):237–42. doi: 10.1046/j.1525-1497.1997.012004237.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ware JE, Kosinksi M, Keller SD. “A 12-Item Short-Form Health Survey.”. Medical Care. 1996;34:220–33. doi: 10.1097/00005650-199603000-00003. [DOI] [PubMed] [Google Scholar]
- Weech-Maldonado R, Morales LS, Spritzer K, Elliott M, Hays RD. “Racial and Ethnic Differences in Parents' Assessments of Pediatric Care in Medicaid Managed Care.”. Health Services Research. 2001;36(3):575–94. [PMC free article] [PubMed] [Google Scholar]
- Williams C, Lee J. “Are Health Insurance Premiums Higher for Small Firms?”. 2002. http://www.rwjf.org/publications/synthesis/reports_and_briefs/pdf/no2_researchreport.pdf Research Synthesis Report No. 2. Available at [accessed May 16, 2003]. [PubMed]
- Zastowny TR, Roghmann KJ, Cafferata GL. “Patient Satisfaction and the Use of Health Services.”. Medical Care. 1998;27(7):705–23. doi: 10.1097/00005650-198907000-00005. [DOI] [PubMed] [Google Scholar]