Abstract
Objective
To better understand medical decision making in the context of “preference sensitive care,” we investigated factors associated with breast cancer patients' satisfaction with the type of surgery received and with the decision process.
Data Sources/Data Collection
For a population-based sample of recently diagnosed breast cancer patients in the Detroit and Los Angeles metropolitan areas (N=1,633), demographic and clinical data were obtained from the Surveillance, Epidemiology, and End Results tumor registry, and self-reported psychosocial and satisfaction data were obtained through a mailed survey (78.4 percent response rate).
Study Design
Cross-sectional design in which multivariable logistic regression was used to identify sociodemographic and clinical factors associated with three satisfaction measures: low satisfaction with surgery type, low satisfaction with the decision process, and decision regret.
Principal Findings
Overall, there were high levels of satisfaction with both surgery and the decision process, and low rates of decision regret. Ethnic minority women and those with low incomes were more likely to have low satisfaction or decision regret. In addition, the match between patient preferences regarding decision involvement and their actual level of involvement was a strong indicator of satisfaction and decision regret/ambivalence. While having less involvement than preferred was a significant indicator of low satisfaction and regret, having more involvement than preferred was also a risk factor. Women who received mastectomy without reconstruction were more likely to report low satisfaction with surgery (odds ratio [OR]=1.54, p<.05), low satisfaction with the process (OR=1.37, p<.05), and decision regret (OR=1.55, p<.05) compared with those receiving breast conserving surgery (BCS). An additional finding was that as patients' level of involvement in the decision process increased, the rate of mastectomy also increased (p<.001).
Conclusions
A significant proportion of breast cancer patients experience a decision process that matches their preferences for participation, and report satisfaction with both the process and the outcome. However, women who report more involvement in the decision process are significantly less likely to receive a lumpectomy. Thus, increasing patient involvement in the decision process will not necessarily increase use of BCS or lead to greater satisfaction. The most salient aspect for satisfaction with the decision making process is the match between patients' preferences and experiences regarding participation.
Keywords: Breast cancer, breast conserving surgery, shared decision making, patient satisfaction
The majority of women diagnosed with breast cancer are clinically eligible for two surgical treatment approaches: mastectomy or lumpectomy (also referred to as breast conserving surgery [BCS]). It is well-established that mastectomy and BCS accompanied by radiation therapy confer an equivalent rate of survival for patients without metastatic disease (National Institutes of Health 1990; Fisher et al. 1999). Thus, the surgical treatment of breast cancer is a good example of what has been described as preference-sensitive care, or care situations in which there are two or more treatment options that are medically justified (Wennberg 2002a). As the label implies, when multiple treatment paths are available and clinically appropriate, the decision process should incorporate and be sensitive to patient preferences regarding the various treatment options (Wennberg 2000b).
Several studies have suggested that shared medical decision making between patients and providers can improve patient satisfaction and even improve some clinical outcomes (Kaplan, Greenfield, and Ware 1989; Laine and Davidoff 1996; Deadman et al. 2001). Many clinicians, researchers, and advocates have argued that breast cancer surgery—as a type of preference-sensitive care—provides an excellent opportunity for shared decision making between patient and provider (Guadagnoli and Ward 1998; Gafni, Charles, and Whelan 1998; Fallowfield et al. 1990). A number of interventions promoting shared-decision models in breast cancer surgical treatment have been designed and evaluated (Whelan et al. 1999; Sepucha et al. 2000). In addition, 20 states have passed laws mandating that patients be informed of both mastectomy and BCS as options (Nayfield et al. 1994; Montini 1997).
An explicit assumption in much of this program and policy development is that mastectomy is “over-used” (National Cancer Policy Board 1999; Morris et al. 2000). The observed geographic and sociodemographic variation in rates of mastectomy versus BCS has not only been labeled as a problem in terms of “over-treatment” but also as an explicit indication of a lack of decision involvement or control among breast cancer patients (Lazovich et al. 1991; Wennberg 2002b). As such, increasing the use of BCS is viewed as a positive goal; and the promotion of patient choice and shared decision making is viewed as the primary means by which this goal can be achieved.
Despite a tacit assumption that increasing patient choice will increase the use of BCS, there is some evidence to suggest that increasing patient involvement is not a simplistic goal, and will not necessarily decrease mastectomy rates. The results of several studies emphasize that not all patients are comfortable with or want to participate in medical decision making, even in the case of preference-sensitive care (Pierce 1993; Schneider 1995; Collins, Kerrigan, and Anglade 1999; Robinson and Thompsom 2001). In addition, Keating et al. (2002) found in a sample of early-stage breast cancer patients that only one-half of the patients participated in the decision making process to the extent that they desired, but that those with more active participation had higher rates of mastectomy. Patients' concerns about cancer recurrence, radiation therapy, the personal costs/benefits of breast reconstruction, and other salient aspects of surgical treatment play important roles in the decision process, even in the face of a strong recommendation for BCS from a surgeon (Nold et al. 2000; Katz, Lantz, and Zemencuk 2001; Keating et al. 2002; Katz et al. 2004).
The primary indicator of progress and quality of breast cancer care should not be the rate of BCS alone (Lantz, Zemencuk, and Katz 2002). Rather, a broader context needs to be considered, including important dimensions of patient satisfaction related to both the outcomes and process of care. The purpose of the research presented here was to investigate patterns in and determinants of satisfaction with surgical treatment and the decision making process in a large, population-based sample of women recently diagnosed with breast cancer. Given that breast cancer surgery is a type of “preference-sensitive care,” there is no ideal or target rate of BCS (Ganz 1992). Therefore, rather than view the prevalence of BCS as the primary indicator of quality of care, we investigated patient satisfaction along three dimensions: (a) satisfaction with the type of surgery received; (b) satisfaction with the process by which the surgery decision was made; and (c) feelings of ambivalence or regret regarding the type of surgery received. The main objectives were to describe the prevalence of low satisfaction and decision ambivalence/regret in a population of breast cancer patients, and to identify patient sociodemographic and clinical characteristics—including the type of surgery received—associated with satisfaction and decision appraisal.
METHODS
Study Population
The study sample was selected from population-based Surveillance, Epidemiology, and End Results (SEER) registries in the greater metropolitan areas of Detroit (4.1 million residents) and Los Angeles (8.8 million residents). Inclusion criteria included: (a) a primary diagnosis of ductal carcinoma in situ (DCIS) or invasive but nonmetastatic breast cancer; (b) no previous breast cancer diagnosis; (c) age 79 years or younger; (d) receipt of a definitive surgical treatment procedure; and (e) ability to complete a self-administered questionnaire in English or Spanish. Exclusion criteria included a diagnosis of lobular carcinoma in situ (because of the different natural history and treatment recommendations for this diagnosis compared with DCIS). In addition, Asian women and U.S.-born women younger than 50 years of age diagnosed with invasive disease in Los Angeles during the study period also were excluded because these women were already enrolled in other studies at this site. We prospectively selected all DCIS cases and an approximate 20 percent random sample of invasive cases meeting the study criteria, accruing a preliminary sample of 2,627 patients over a 14-month study period (December 2001–January 2003). In addition to over-sampling cases of DCIS (34.6 percent of accrued case), we also over-sampled African-American women with invasive disease (19.0 and 32.0 percent of accrued cases in Los Angeles and Detroit, respectively).
Staff members from each SEER registry identified the study sample, screened potential participants, and implemented the mailing of a self-administered survey according to a uniform protocol. Potential subjects were identified based on initial pathology reports reported to the registries within 6 weeks of diagnosis. This rapid case ascertainment process captures 90 percent of all breast cancer cases in Detroit and nearly 100 percent of cases in Los Angeles. It was subsequently determined that 2,383 (90.7 percent) of the accrued cases actually met the study criteria. Of these, 78.4 percent (n=1,844) completed the survey questionnaire, with 1,703 completing the written survey and 141 completing an abbreviated telephone survey. For subjects included in this analysis, the median time between diagnosis and survey response was 7.9 months, with 25 percent completing the survey within 6.3 months and 75 percent completing it within 9.4 months of diagnosis.
Data Collection and Management
The data collection protocol had several steps. First, physicians of record were notified via a letter of our intent to solicit patients for this study, with less than 1 percent of patients excluded because of physician concerns (e.g., patient moved or patient too ill to participate in research). Second, an introductory letter was sent to all potential subjects, stating that someone would be calling on the telephone to discuss the study (and also providing a telephone contact number for further information). Third, within 2 weeks of the introductory letter being mailed, telephone contact was initiated to assess eligibility and to collect information on a small set of variables. This included a three-question protocol to determine whether a potential respondent perceived that she was given a choice between mastectomy and lumpectomy for surgical treatment. Fourth, for eligible subjects (and the 14 percent of subjects who could not be reached by telephone), the survey questionnaire and a token gift of a grocery store coupon worth $10 were mailed. Fifth, the Dillman survey method, which involves follow-up reminders and subsequent mailings to nonrespondents, was employed to enhance response (Dillman 1978).
SEER clinical data gathered from medical record audits (including tumor size, node status, regional and distant extension, histologic grade, and treatment information) were subsequently merged with the mail/telephone survey data using patient identification numbers. The fieldwork and SEER data management were performed by investigators and staff at Wayne State University and the University of Southern California. Data entry, management, and analysis were performed by University of Michigan investigators and staff. The protocol was reviewed and approved by three institutional review boards.
Measures
Dependent Variables
There were three dependent variables under study: (1) satisfaction with the type of surgical treatment received; (2) satisfaction with the process by which the surgical treatment decision was made; and (3) ambivalence or regret regarding the type of surgery received. A revised version of the Holmes-Rovner scale was used to measure satisfaction with surgery type (Holmes-Rovner et al. 1996). Confirmatory factor analysis revealed that four of the six items on this scale hung together with a Chronbach's α of 0.90, thus only these four items were included in the revised scale. A 5-point Likert scale (strongly disagree to strongly agree) was used to measure subjects' level of agreement with the following items: (a) I was adequately informed about the issues; (b) the decision about surgery was the best decision for me; (c) the surgery decision was consistent with my personal values; and (d) I am satisfied with my decision about what type of surgery to have. Responses to these items were added together and then divided by four, with the resulting score reflecting a respondent's average response to the four items in the scale.
Satisfaction with the decision process was measured with a scale comprised of four items from the survey that were identified from a larger pool of items through data reduction procedures (i.e., exploratory factor analysis). A 5-point Likert scale (this time ranging from strongly agree to strongly disagree) measured the level of agreement with the four items: (a) I wish I would have given more consideration to other surgery options; (b) I would have liked to have had more information; (c) I would have liked to have been more active in the decision-making process; (d) I did not have as much say as I would have liked. The Cronbach's α for this scale was 0.91, with the scale score also representing the average response to the four items.
Decision regret was measured as a dichotomous variable, based on the response to one item in the survey: “If I had it to do over, I would make a different decision about what type of surgery to have (lumpectomy or mastectomy).” Responses of “strongly disagree” or “disagree” were coded as no decision regret/ambivalence. This question was only asked of women who reported no contraindications to BCS and perceived that they actually had been given a choice between surgical procedures (n=1,183, assessed during telephone screening). Thus, this dependent variable was investigated for the subset of patients (65.1 percent of the weighted sample) who clearly perceived that they had options and were given a choice.
Independent Variables
Independent variables in the multivariable models included sociodemographic characteristics such as age, education, income, marital status, and ethnicity. Age at diagnosis was measured as a categorical variable (<50 years, 50–64 years, and 65+ years) based on information from the survey, using SEER data in the case of missing survey data. Ethnicity, which also was taken from the survey and from SEER if survey data were missing, was coded as White, African American, or other (with 75 percent of those in the latter category being Hispanic). Self-reported education was categorized as less than high school, high school graduate, some college, or college graduate and beyond. Annual gross household income was recoded into four categories: less than $30,000, $30,000–$69,000, $70,000 or more, and missing/refused. Marital status information was recoded as a dichotomous variable identifying those who were currently married/partnered versus those who were not.
Stage at diagnosis (DCIS versus invasive disease) was taken from the SEER registry. Surgery type was measured using three categories: BCS, mastectomy (unilateral or bilateral), and mastectomy followed by breast reconstruction surgery. Similar to published validation studies (Mandelblatt et al. 2000), we found that self-report and SEER data regarding surgery type produced the same answer for 96.3 percent of respondents. Self-report of surgical treatment was used except when it was ambiguous or missing (N=26), in which case SEER data were used.
Perception of involvement in the surgical treatment decision was measured with a survey item through which patients indicated which of five statements (ranging from “my doctor made the surgery decision with little input from me” to “I made the surgery decision with little input from my doctor”) best described how the surgery decision was made (Degner and Sloan 1992). A second related variable measured the extent to which how the decision was made actually matched patient preferences. This variable was created by comparing the answers to the survey item described above with a second item that stated: “Sometimes how you want to make a decision does not match how the decision was really made … Please check the statement that best describes how you would have preferred the decision to have a mastectomy or lumpectomy to have been made.” The same five response categories as described above were provided. After comparing responses to these two parallel questions, a new variable was created indicating one of three levels of congruence: (1) patient preferences regarding participation level matched the actual decision process; (2) the patient participated in the decision at a level that was more than she preferred; and (3) the patient participated in the decision at a level that was less than she preferred.
Analysis
Statistical analyses were performed on data for the 1,633 study subjects (88.6 percent of total sample) for whom there was no missing data on the satisfaction scale items (with a subset of 1,183 cases used for the decision regret analysis). Because DCIS and African-American cases were oversampled, sample weights were created for use in analysis. A total sampling weight was calculated for each subject, based on the probability of selection into the study. These probabilities varied by strata defined by stage at diagnosis (DCIS versus invasive), ethnicity (white, African American, or other), and site (Detroit versus L.A.). The total sampling weights were then normalized for each site in order to maintain the original sample size for statistical testing. (Additional technical details are available from the authors by request.) When weighted, the data are representative of the actual population of breast cancer cases included in this study. Since the weighting scheme does not correct for the exclusion of Asian women and U.S.-born invasive cases under the age of 50 in the Los Angeles sample, the generalizability of the weighted results is somewhat limited. However, because of the relatively small number of cases of invasive breast cancer diagnosed in women under 50, we estimate that this restriction in Los Angeles resulted in only 60 fewer cases in the study sample. Thus, the weighted results generally reflect the surgery decisions and resulting satisfaction of non-Asian women diagnosed with nonmetastatic breast cancer in Detroit and Los Angeles during the study period.
Descriptive statistics (frequencies, contingency tables, and correlation coefficients) were generated to understand and describe the study sample. Continuous versions of the two satisfaction scales were used in bi-variate analysis of means to identify sociodemographic and clinical variables that were associated with the mean score on these scales. Both satisfaction scales had skewed rather than normal distributions, with the majority of respondents reporting fairly high levels of satisfaction. This meant that the distribution of these variables as continuous measures did not meet the assumptions for using ordinary least squares regression and thus some type of transformation of the skewed dependent variable was needed. As such, we dichotomized the outcome variables and conducted multivariable logistic regression analysis to identify sociodemographic and clinical characteristics associated with having low satisfaction on either scale or with having decision regret/ambivalence. The satisfaction scale distributions were used to identify the portion with “low satisfaction,” operationalized as having a scale score indicating the average answer to scale items was neutral, disagree, or strongly disagree. This turned out to be the bottom 11 percent of the distribution for the surgery satisfaction scale and the bottom 19 percent for the process satisfaction scale. The decision regret/ambivalence variable also was a dichotomous measure with a skewed distribution, with approximately 11 percent expressing these feelings.
Full multivariable logistic regression models of the three dependent variables were run, each controlling for age, education, income, marital status, ethnicity, stage of disease, surgery type, decision involvement, and the degree to which patient preferences matched level of involvement. Models also controlled for SEER site (Los Angeles versus Detroit), but these results are not reported since site was not a significant predictor in any of the models. We also conducted analyses using a log transformation and a γ transformation, with findings robust across different modeling approaches that can be used for skewed distributions of the dependent variable.
RESULTS
Study Sample Description
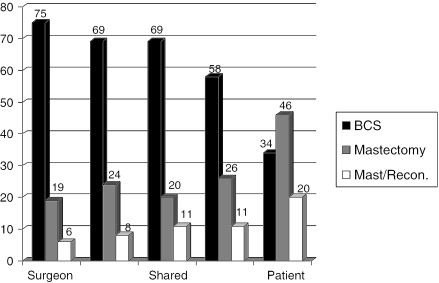
Descriptive information on the weighted sample is shown in Table 1. Of note is that 64.0 percent of the study subjects received BCS for their surgical treatment, 23.6 percent received mastectomy, and 12.2 percent received mastectomy followed by breast reconstruction. The rate of BCS was 67.0 percent among non-Hispanic whites, 62.4 percent for African Americans, and 58.7 percent for other ethnic groups (χ2=63.9, p<.001). In addition, type of surgery received significantly varied (p<.001) by age with BCS rates as follows: 54.6 percent among women under 50, 66.1 percent ages 50–64, and 68.3 percent age 65 and over. BCS rates were similar among women with DCIS (64.7 percent) and those with invasive disease (66.3 percent). Interestingly, the rate of BCS decreased as the level of patient involvement in the decision process increased (χ2=124.2, p<.001). Of women who reported the surgeon made the decision alone, 75.2 percent received BCS, compared with only 34.3 percent of women reporting that they made the decision themselves (Figure 1).
Table 1.
Descriptive Statistics for Population-Based Sample of Breast Cancer Patients (N=1,633)
| Variable | N | Weighted Percent |
|---|---|---|
| Age | ||
| <50 years | 343 | 18.0 |
| 50–64 years | 726 | 45.8 |
| 65+ years | 517 | 33.9 |
| Missing | 47 | 2.4 |
| Education | ||
| College graduate/plus | 441 | 27.1 |
| Some college | 607 | 36.7 |
| High school graduate | 369 | 22.6 |
| <High school | 200 | 13.0 |
| Missing | 16 | 0.7 |
| Household income | ||
| $70,000 or more | 445 | 28.0 |
| $30,000–$69,999 | 499 | 30.5 |
| <$30,000 | 517 | 31.3 |
| Missing | 172 | 10.2 |
| Marital status | ||
| Currently married/partnered | 982 | 61.7 |
| Single/divorced/widowed | 634 | 37.3 |
| Missing | 17 | 1.0 |
| Ethnicity | ||
| White | 1,064 | 67.5 |
| Black | 334 | 15.4 |
| Other | 230 | 16.9 |
| Missing | 5 | 0.2 |
| Stage of disease (SEER) | ||
| Invasive | 829 | 65.0 |
| DCIS | 804 | 35.0 |
| Surgery type | ||
| BCS | 1,051 | 64.0 |
| Mastectomy | 347 | 23.6 |
| Mastectomy/reconstruction | 232 | 12.2 |
| Missing | 3 | 0.2 |
| Who made decision | ||
| Surgeon alone | 147 | 9.6 |
| Surgeon w/patient input | 202 | 12.1 |
| Shared | 594 | 36.9 |
| Patient w/surgeon input | 624 | 37.9 |
| Patient alone | 39 | 2.4 |
| Missing | 27 | 1.2 |
| Participation level | ||
| Matched preferences | 1,134 | 69.0 |
| More than preferred | 320 | 20.0 |
| Less than preferred | 179 | 11.0 |
| Satisfaction—surgery | ||
| Low satisfaction | 191 | 11.7 |
| Not low satisfaction | 1,442 | 88.3 |
| Satisfaction—process | ||
| Low satisfaction | 317 | 19.4 |
| Not low satisfaction | 1,316 | 80.6 |
| Decision regret | ||
| Regret/ambivalence | 183 | 11.4 |
| None | 965 | 59.4 |
| Missing* | 485 | 29.2 |
Decision regret question was only asked of study subjects who perceived they had a choice among surgical treatments.
DCIS, ductal carcinoma in situ; BCS, breast conserving surgery; SEER, Surveillance, Epidemiology, and End Results.
Figure 1.
Percent of Patients Receiving Different Types of Breast Cancer Surgery by Reported Level of Who Made the Decision
Overall, 11.7 percent of women were classified as having “low satisfaction” with the type of surgery received, and 19.4 percent as having “low satisfaction” with the surgery decision process; in addition, 11.4 percent reported some level of decision regret/ambivalence (Table 1). Although there was some degree of correlation among these outcomes, it was not the same women having poor outcomes across all three dimensions. Approximately one-fourth of the sample (23.4 percent) was in the dissatisfied outcome group for at least 1 of the 2 satisfaction variables (with 7.0 percent scoring low on both dimensions). For the subsample with information on all three dependent variables, 25.1 percent had at least one negative outcome (specifically, 13.4 percent had one, 7.3 percent had two, and 4.4 percent had three negative outcomes). Thus, while overall levels of satisfaction were fairly high and the level of decision regret/ambivalence was fairly low, approximately one out of four women in this sample reported some degree of dissatisfaction regarding their surgery and/or the surgery decision process.
Bivariate Results for Satisfaction Measures
The mean score on the satisfaction with surgery scale was 4.41 and the mean score on the satisfaction with the decision process scale was 3.89 (both out of a possible 5.0 points) suggesting fairly high levels of satisfaction in the population as a whole (with no difference between the Detroit and Los Angeles sites). Satisfaction on both of these dimensions, however, varied by sociodemographic and other patients characteristics (Table 2). In regard to satisfaction with the type of surgery received, a higher level of satisfaction was significantly associated with a higher level of education, a higher level of income, being married, and being non-Hispanic white. In addition, higher levels of satisfaction with the surgery received were observed among women with DCIS, women receiving BCS or mastectomy with reconstruction, and among women whose level of participation in the surgery decision matched their preferences. Women who perceived that their surgeon made the decision alone had the lowest score on this satisfaction scale of all subgroups (Table 2). This finding held for women receiving BCS as well as for those receiving mastectomy (with or without reconstruction).
Table 2.
Bivariate Means for Satisfaction with Decision Process and Satisfaction with Type of Surgery Received
| Variables | Mean Score on Satisfaction with Surgery Scale | F-test (p-value) | Mean Score on Satisfaction with Decision Process Scale | F-test (p-value) |
|---|---|---|---|---|
| Total sample | 4.41 | 3.89 | ||
| Age | ||||
| <50 years | 4.38 | 2.34 | 3.85 | 1.55 |
| 50–64 years | 4.44 | (.10) | 3.93 | (.21) |
| 65+ years | 4.42 | 3.91 | ||
| Education | ||||
| College graduate/plus | 4.51 | 31.24 | 4.07 | 100.60 |
| Some college | 4.46 | (<.001) | 4.01 | (<.001) |
| High school graduate | 4.35 | 3.84 | ||
| <High school | 4.22 | 3.33 | ||
| Household income | ||||
| $70,000 or more | 4.61 | 57.14 | 4.20 | 81.99 |
| $30,000–$69,000 | 4.38 | (<.001) | 3.89 | (<.001) |
| <$30,000 | 4.32 | 3.66 | ||
| Income not reported | 4.29 | 3.78 | ||
| Marital status | ||||
| Currently married/partnered | 4.45 | 11.06 | 3.93 | 3.31 |
| Single/divorced/widowed | 4.36 | (<.001) | 3.83 | (<.05) |
| Ethnicity | ||||
| White | 4.49 | 67.70 | 4.05 | 144.92 |
| Black | 4.25 | (<.001) | 3.69 | (<.001) |
| Other | 4.26 | 3.70 | ||
| Stage of disease | ||||
| Invasive | 4.39 | 10.31 | 3.89 | 0.53 |
| DCIS | 4.46 | (.001) | 3.91 | (.47) |
| Surgery type | ||||
| BCS | 4.45 | 17.91 | 3.95 | 30.29 |
| Mastectomy | 4.31 | (<.001) | 3.69 | (<.001) |
| Mastectomy/reconstruction | 4.46 | 3.97 | ||
| Who made surgery decision | ||||
| Surgeon alone | 3.88 | 94.75 | 3.22 | 72.07 |
| Surgeon w/patient input | 4.40 | (<.001) | 3.82 | (<.001) |
| Shared decision | 4.52 | 4.00 | ||
| Patient w/surgeon input | 4.46 | 4.00 | ||
| Patient alone | 4.36 | 3.83 | ||
| Participation level | ||||
| Matched preferences | 4.52 | 60.04 | 4.01 | 71.46 |
| More than preferred | 4.35 | (p<.001) | 3.74 | (p<.001) |
| Less than preferred | 4.02 | 3.34 | ||
DCIS, ductal carcinoma in situ; BCS, breast conserving surgery.
Patterns in bivariate associations between satisfaction with the decision process and independent variables were similar (Table 2). Significantly higher levels of satisfaction with the decision process were observed for women with higher levels of education and income, married women, white women, those reporting some level of participation in the surgery decision, and those whose level of participation matched their preferences. In the bivariate analysis, those women receiving mastectomy alone had a lower mean level of satisfaction (p<.001) than those receiving BCS or mastectomy with reconstruction. Again, the lowest level of satisfaction on this dimension was observed among women who reported no participation in the decision process.
Multivariable Results for Satisfaction with Surgery
In full multivariable models investigating correlates of low satisfaction with surgery received, younger women and those with lower incomes were significantly more likely to report low satisfaction (Table 3). In addition, nonwhite women had significantly higher odds (p<.05) of having low satisfaction with surgery (odds ratio [OR]=1.57 for African-American women and OR=1.37 for other ethnicities compared with white women).
Table 3.
Multivariable Logistic Regression Full Model Results for Patient Satisfaction Outcomes and Surgical Treatment Decision Regret
| Low Satisfaction with Surgery Received | Low Satisfaction with Decision Process | Decision Regret | ||||
|---|---|---|---|---|---|---|
| Variable | Odds Ratio | p-Value | Odds Ratio | p-Value | Odds Ratio | p-Value |
| Age | ||||||
| <50 years | 1.00 | .002 | 1.00 | 1.00 | ||
| 50–64 years | 0.66 | <.000 | 1.02 | .83 | 0.86 | .26 |
| 65+ years | 0.57 | 1.00 | .98 | 0.75 | .06 | |
| Education | ||||||
| College graduate/plus | 1.00 | 1.00 | 1.00 | |||
| Some college | 0.81 | .12 | 0.82 | .11 | 0.46 | <.001 |
| High school graduate | 0.75 | .09 | 1.31 | .04 | 0.69 | .02 |
| <High school | 0.78 | .20 | 1.77 | <.001 | 1.19 | .35 |
| Household income | ||||||
| $70,000 or more | 1.00 | <.001 | 1.00 | <.001 | 1.00 | |
| $30,000—69,999 | 2.37 | <.00 | 2.12 | <.001 | 2.11 | <.001 |
| <$30,000 | 2.22 | 1 | 3.12 | 2.41 | <.001 | |
| Income not reported | 1.13 | .55 | 1.75 | <.001 | 1.25 | .37 |
| Marital status | ||||||
| Currently married/partnered | 1.00 | <.00 | 1.00 | 1.00 | ||
| Single/divorced/widowed | 1.56 | 1 | 1.71 | .001 | 0.84 | .14 |
| Ethnicity | ||||||
| White | 1.00 | 1.00 | 1.00 | |||
| Black | 1.57 | .002 | 1.57 | <.001 | 1.82 | <.001 |
| Other | 1.37 | .04 | 2.21 | <.001 | 2.58 | <.001 |
| Stage of disease | ||||||
| Invasive | 1.00 | 1.00 | 1.00 | |||
| DCIS | 0.96 | .69 | 0.99 | .88 | 0.81 | .05 |
| Surgery type | ||||||
| BCS | 1.00 | 1.00 | 1.00 | |||
| Mastectomy | 1.54 | .001 | 1.37 | .001 | 1.55 | <.001 |
| Mastectomy and reconstruction | 1.43 | .02 | 1.15 | .33 | .78 | .19 |
| Who made surgery decision | ||||||
| Surgeon alone | 1.00 | 1.00 | 1.00 | |||
| Surgeon w/patient opinion | 0.18 | <.001 | 0.39 | <.001 | 0.38 | <.001 |
| Shared decision | 0.11 | <.001 | 0.39 | <.001 | 0.37 | <.001 |
| Patient w/surgeon opinion | 0.24 | <.001 | 0.24 | <.001 | 0.36 | <.001 |
| Patient alone | 0.28 | <.001 | 0.32 | <.001 | 0.22 | <.001 |
| Participation level | ||||||
| Matched preferences | 1.00 | 1.00 | 1.00 | |||
| More than preferred | 1.52 | .004 | 2.48 | <.001 | 1.71 | <.001 |
| Less than preferred | 2.63 | <.001 | 3.23 | <.001 | 2.42 | <.001 |
DCIS, ductal carcinoma in situ; BCS, breast conserving surgery.
Stage of disease at diagnosis was not associated with surgery satisfaction. Those women receiving a mastectomy or mastectomy with reconstruction had significantly greater odds of having low satisfaction compared with those receiving BCS (Table 3). In addition, the results also suggest that women who reported some level of shared decision making were less likely to have low satisfaction (p<.001), and that participating at a level less than preferred was a significant risk factor for having low satisfaction with the surgery received (OR=2.63, p<.001). However, those women who reported that they participated at a level that was more than preferred also were at greater risk for having low satisfaction (OR=1.52, p=.004).
Multivariable Results for Satisfaction with Decision Process
The results for low satisfaction with the decision process are somewhat similar to those for satisfaction with the surgery received (Table 3). Low education, low and middle income, not currently married/partnered, and nonwhite ethnicity were all significant risk factors for having a low level of satisfaction with the treatment decision process. Also, in the multivariate model, those women receiving mastectomy without reconstruction had significantly greater odds of reporting low satisfaction with the process, compared with women receiving BCS. Women reporting a shared decision making process had the lowest odds of low satisfaction with the process (Table 3). The results further underscore the importance of having a match or congruence between the level of participation in the decision process and patient preferences. The odds of having low satisfaction were significantly higher for those reporting either more (OR=2.48, p<.001) or less participation (OR 3.23, p<.001) than desired (Table 3).
Multivariable Results for Decision Regret/Ambivalence
The final dependent variable under investigation was a measure of surgical treatment decision regret or ambivalence, analyzed only for those respondents who perceived they had a choice between surgical procedures. The odds of having decision regret/ambivalence were significantly higher among women with less than high school education, women with low and middle incomes, and women of color (Table 3). Having a mastectomy without reconstructive surgery was associated with increased odds of decision regret (OR=1.55, p<.001), although not among women who received mastectomy with reconstruction. Decision participation also was important for this third dependent variable. The odds of having decision regret were higher both for those reporting more participation in the surgery decision than desired (OR=1.71, p=.003) and those reporting less (OR=2.42, p<.001).
Taken together, the multivariable results suggest that, controlling for sociodemographic and clinical factors, women receiving mastectomy without reconstruction were more likely to report a low degree of satisfaction with the type of surgery received and with the process by which the surgery decision was made. In addition, women who reported participating at some level in the surgery decision were significantly less likely to report low satisfaction with treatment or process compared with the women whose surgeon made the decision alone, although having either more or less participation than preferred was associated with having low satisfaction and decision regret.
DISCUSSION
Ganz (2002) recently argued that, in an effort to enhance treatment outcomes that are salient for breast cancer patients, key strategies need to be developed in three areas: (1) emphasizing evidence-based treatment; (2) including patient preferences when different treatment alternatives provide equivalent disease-focused outcomes; and (3) providing adequate time for patient–physician communication regarding disease- and patient-focused outcomes, including the provision of training for clinicians so that they can adequately facilitate these discussions. Our work supports this framework, and offers some provocative findings from a large population-based sample that should be useful and informative to researchers and policymakers who are committed to devising key strategies for improving quality of care for cancer patients.
The results presented here support and resonate with a number of findings in the current literature. Our findings suggest that while there is a high level of satisfaction regarding the type of surgery received and the surgery decision process, one out of four patients scored low on at least one of our measures of satisfaction. Women who are socioeconomically disadvantaged or from ethnic minority groups were more likely to report low satisfaction or decision regret. In addition, women who indicated they had some level of involvement in the surgical treatment decision were less likely to have low satisfaction and decision regret, consistent with previous peer-reviewed studies (Moyer and Salovey 1998; Deadman et al. 2001; Liang et al. 2002).
Some of the results reported here, however, are inconsistent with prior research and editorials regarding breast cancer surgery. This includes that there is a significant and positive association between patient decision involvement and receipt of mastectomy, and that the match between patient preferences and their actual level of involvement is a strong indicator of satisfaction and decision regret. While having less participation than preferred is associated with low satisfaction and regret, having more involvement than preferred also is a significant risk factor. Taken together, these results suggest that some of the assertions that permeate the breast cancer research and advocacy literature—including that increasing patient involvement in the decision process will automatically lead to higher rates of BCS—is overly simplistic. These results also suggest caution in using BCS rates as performance measures or quality indicators for health plans or health care systems (Keating et al. 2002; Lantz, Zemencuk, and Katz 2002).
The finding that mastectomy without reconstruction, when controlling for sociodemographic and decision context variables, may be associated with lower levels of satisfaction and decision regret is consistent with some but not all prior research. A key finding across a number of prior studies is that having a choice or options—rather than receiving a specific type of surgery itself—is a fundamental factor for women's satisfaction and psychosocial adjustment to breast cancer surgery (Street and Voigt 1997; Lantz, Zemencuk, and Katz 2002). Our finding that patients with mastectomy without reconstruction were at higher risk for dissatisfaction and decision regret should not be interpreted to mean that mastectomy is an inferior treatment choice or that more women should be receiving BCS. Mastectomy with or without reconstruction is a viable surgical option for breast cancer patients, and there are several reasons that a woman might prefer mastectomy over BCS (including that it confers a reduced risk of recurrence and that for many women means they do not need radiation therapy). Indeed, in this sample, women receiving mastectomy—particularly those under 50—were more likely than women receiving BCS to report that concerns about recurrence of disease and radiation exposure influenced their surgery decision (Katz et al. 2004). Women who received a mastectomy were also less likely to report that concerns about body image influenced their surgical treatment decision.
In addition, in this study, the vast majority of women receiving mastectomy were satisfied. For example, although significantly different, the prevalence of low satisfaction with the surgery received was low among both women receiving mastectomy without reconstruction (14.1 percent) and those receiving BCS (9.7 percent). Furthermore, those receiving reconstructive surgery—an increasingly used option for breast cancer patients—were not at risk for low satisfaction with the process or for decision regret, compared with those receiving BCS. A primary area of concern in breast cancer care has been in regard to women who were offered only mastectomy for their surgical treatment (Montini 1997). Perhaps the pendulum has now swung to a place where we also need to be concerned about patients who are only offered BCS as surgical option. In our sample, only one-third of the women who perceived they were not offered a surgical choice reported any contraindication (e.g., multifocal disease) to either type of surgery, and the majority (66 percent) of these women received BCS. Again, the quality of care lens should be on how patients are appraising their treatment and the decision process, not on the relative rates of mastectomy versus BCS.
Wennberg (2000a, b) and others emphasize the importance of involving patients in medical decision making, especially in the context of preference-sensitive care. As Guadagnoli and Ward (1998) argued in regard to breast cancer surgery: “Patient participation in decision making is justified on humane grounds alone.” However, it is important to consider not only patient preferences regarding treatment options, but preferences regarding their own level of involvement in the decision-making process. While it is encouraging that the majority of women reported congruence between their actual and preferred levels of involvement in the surgery decision, a nontrivial number of women reported they were more involved than preferred. Of the women in our sample who had one or more negative satisfaction outcome, 29.9 percent reported having more participation than desired. Attempting to foster greater patient participation in treatment decisions could further decrease satisfaction and increase decision regret among these women. There is a growing literature that underscores our finding that not all patients want to be full or lead participants in an important medical decision during a health crisis, and that pressuring some of these patients to do so could have negative psychosocial consequences (Degner and Sloan 1992; Benbassat, Pilpel, and Tidhar 1998; Aurora and McHorney 2000).
Our study results suggest that most but not all patients perceive that their level of involvement in the surgery decision matched their preferences. Other studies have reported slightly lower levels of concordance (Degner et al. 1997; Keating et al. 2002; Janz et al. in press). If a match between patient preferences and actual involvement is indeed important, then a key goal for clinical practice is to match patient participation with preferences regarding decision control (Keating et al. 2002). This means that clinicians not only need to assess patient preferences regarding the type of surgery preferred, they also need to assess the “type” of decision maker who is before them, ostensibly before any conversations regarding options and choices commence. (Pierce 1993; Street et al. 1995; Pierce 1996; Robinson and Thompsom 2001).
Efforts to improve tailored interactions with patients present a number of challenges, including that this is a labor-intensive endeavor (Charles, Gafni, and Whelan 1997). As such, a strong case needs to be made that patient satisfaction along all of its dimensions matters. At the present time, there is evidence to suggest that satisfaction with the type of breast cancer surgery received and key elements of the decision process (i.e., the perception of choice) have a significant impact on some dimensions of quality of life (Fallowfield et al. 1990; Degner et al. 1997; Street and Voigt 1997; Mandelblatt et al. 2003). Increased understanding of patients' satisfaction regarding treatments received and the decision-making process in relation to quality of life and psychosocial adjustment is critical for the development of effective clinical interventions and sound public policy aimed at cancer patients.
Given the evidence that self-appraisals of satisfaction with surgery and the decision-making process are associated with income and education, additional research should focus on socioeconomically disadvantaged subpopulations. In addition, minority women in our study had higher levels of dissatisfaction and decision regret, although this is not fully explained by the higher use of mastectomy in these groups. The interrelationships between type of surgery received, satisfaction and ethnicity need further exploration (Murray-Garcia et al. 2000).
This study has several limitations worth noting. First, the study sample, although population-based, is representative only of women from two major metropolitan areas in the U.S. The extent to which our findings are generalizable to rural women or to women from other urban areas is unclear. Also, the sample in Los Angeles excluded a subset of cases (Asian women and U.S.-born women under the age of 50 with invasive disease), thus the generalizability of the results is somewhat compromised. Second, given the cross-sectional nature of the study, the results demonstrate associations between factors rather than causal relationships. For example, although there is a strong and significant association between less involvement with the decision process than preferred and low satisfaction on both dimensions, we cannot state unequivocally that increasing the participation of patients who desire more involvement will improve satisfaction.
Third, the satisfaction with process variable required women to recall events that took place on average 8 months earlier. In addition to potential recall bias, subjects' appraisals in regard to all dependent variables under study may have been affected by current health status and quality of life (QoL) (Kane, Maciejewski, and Finch 1997). We did conduct some analyses that included a measure of health-related QoL (Aaronson, Ahmedzai, and Bergman 1993). While we found that women with lower QoL scores were more likely to report low satisfaction and decision regret, the results also showed that including QoL in the model had no impact on any of the other relationships or associations observed. Thus, the findings reported here are robust to the inclusion of current health-related QoL in the analysis.
Despite these limitations, the strengths of this work include that the sample was large with an oversample of women with DCIS and black women, that patient information was collected relatively soon after the treatment decision was made, and that a wide range of sociodemographic, psychosocial, and clinical data were gathered for each patient. Also, unlike most prior studies, there were enough women who received mastectomy with reconstruction that we could look at this group separately from those receiving mastectomy alone. In addition, this is one of the first population-based studies to collect detailed information on breast cancer patient involvement in the decision process and to solicit appraisals of satisfaction with the type of surgery received separately from the decision-making process. This allowed us to investigate different dimensions of satisfaction simultaneously, all in the context of patient preferences regarding decision involvement. Such research should help us to move past the labeling of mastectomy as a problem of “less progressive” or “poor” quality of care with an easy solution of increased patient involvement, to a more nuanced perspective on this complex issue (Collins, Kerrigan, and Anglade 1999; Lantz, Zemencuk, and Katz 2002). The results should also be of interest to those studying other types of preference-sensitive care.
Acknowledgments
This project was funded by the National Cancer Institute, National Institutes of Health, Department of Health and Human Services. The cancer incidence data used in this publication were collected by the California Department of Health Services as part of a statewide cancer reporting program mandated by California Health and Safety Code Section 103885, and by Wayne State University in Detroit, Michigan. The ideas and opinions expressed herein are solely those of the authors. Appreciation is extended to the cancer registry staff who worked diligently to contact patients and solicit their participation in the study, and to the women with breast cancer who agreed to share their experiences and insights.
REFERENCES
- Aaronson NK, Ahmedzai S, Bergman B. “The European Organization for Research and Treatment of Cancer QLQ-C30: A Quality of Life Instrument for Use in International Clinical Trials in Oncology.”. Journal of the National Cancer Institute. 1993;85:365–76. doi: 10.1093/jnci/85.5.365. [DOI] [PubMed] [Google Scholar]
- Aurora NK, McHorney CA. “Patient Preferences for Medical Decision Making: Who Really Wants to Participate?”. Medical Care. 2000;38:335–412. doi: 10.1097/00005650-200003000-00010. [DOI] [PubMed] [Google Scholar]
- Benbassat J, Pilpel D, Tidhar M. “Patients' Preferences for Participation in Clinical Decision-Making: A Review of Published Surveys.”. Behavioral Medicine. 1998;24(2):81–8. doi: 10.1080/08964289809596384. [DOI] [PubMed] [Google Scholar]
- Charles C, Gafni A, Whelan T. “Shared Decision-Making in the Medical Encounter: What Does It Mean? (Or It Takes Two to Tango).”. Social Science and Medicine. 1997;44:681–92. doi: 10.1016/s0277-9536(96)00221-3. [DOI] [PubMed] [Google Scholar]
- Collins ED, Kerrigan CL, Anglade P. “Surgical Treatment of Early Breast Cancer: What Would Surgeons Choose for Themselves?”. Effective Clinical Practice. 1999;I2(4):149–51. [PubMed] [Google Scholar]
- Deadman JM, Leinster SJ, Owens RG, Dewey ME, Slade PD. “Taking Responsibility for Cancer Treatment.”. Social Science and Medicine. 2001;53(5):669–77. doi: 10.1016/s0277-9536(00)00369-5. [DOI] [PubMed] [Google Scholar]
- Degner LF, Krisjanson LJ, Bowman D, Sloan JA, Carriere KC, O'Neil J, Bilodeau B, Watson P, Mueller B. “Information Needs and Decisional Preferences in Women with Breast Cancer.”. Journal of the American Medical Association. 1997;277:1485–92. [PubMed] [Google Scholar]
- Degner LF, Sloan JA. “Decision Making during Serious Illness: What Role Do Patients Really Want to Play?”. Journal of Clinical Epidemiology. 1992;45:941–50. doi: 10.1016/0895-4356(92)90110-9. [DOI] [PubMed] [Google Scholar]
- Dillman DA. Mail and Telephone Surveys: The Total Design Method. New York: Wiley-Intersciences; 1978. [Google Scholar]
- Fallowfield LJ, Hall A, Maguire P, Baum M. “Psychological Outcomes of Different Treatment Policies in Women with Early Breast Cancer Outside a Clinical Trial.”. British Medical Journal. 1990;301:575–80. doi: 10.1136/bmj.301.6752.575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fisher B, Anderson S, DeCillis A, Dimitrov N, Atkins JN, Fehrenbacher L, Henry PH, Romond EH, Lanier KS, Davila E, Kardinal CG, Laufman L, Pierce HI, Abramson N, Keller AM, Hamm JT, Wickerham DL, Begovic M, Tan-Chiu E, Tian W, Wolmark N. “Pathologic Findings from the National Surgical Adjuvant Breast Project (NSABP) Eight-Year Update of Protocol B-17: Intraductal Carcinoma.”. Cancer. 1999;86(3):429–38. doi: 10.1002/(sici)1097-0142(19990801)86:3<429::aid-cncr11>3.0.co;2-y. [DOI] [PubMed] [Google Scholar]
- Gafni A, Charles C, Whelan T. “The Physician–Patient Encounter: The Physician as a Perfect Agent for the Patient versus the Informed Treatment Decision-Making Model.”. Social Science and Medicine. 1998;47:347–54. doi: 10.1016/s0277-9536(98)00091-4. [DOI] [PubMed] [Google Scholar]
- Ganz PA. “Treatment Options for Breast Cancer—Beyond Survival.”. New England Journal of Medicine. 1992;326(17):1147–9. doi: 10.1056/NEJM199204233261708. [DOI] [PubMed] [Google Scholar]
- Ganz PA. “What Outcomes Matter to Patients: A Physician-Researcher Point of View.”. Medical Care. 2002;40(6, Suppl):III11–19. [PubMed] [Google Scholar]
- Guadagnoli E, Ward P. “Patient Participation in Decision-Making.”. Social Science and Medicine. 1998;47(3):329–39. doi: 10.1016/s0277-9536(98)00059-8. [DOI] [PubMed] [Google Scholar]
- Holmes-Rovner M, Kroll J, Schmitt N, Rovner DR, Breer ML, Rothert ML, Padonu G, Talarczyk G. “Patient Satisfaction with Health Care Decisions: The Satisfaction with Decision Scale.”. Medical Decision Making. 1996;16:58–64. doi: 10.1177/0272989X9601600114. [DOI] [PubMed] [Google Scholar]
- Janz NK, Wren PA, Copeland LA, Lowery JC, Goldfarb SL, Wilkins EG. “Patient–Physician Concordance: Preferences, Perceptions, and Factors Influencing the Breast Cancer Surgical Decision.”. Journal of Clinical Oncology. doi: 10.1200/JCO.2004.09.069. In press. [DOI] [PubMed] [Google Scholar]
- Kane RL, Maciejewski M, Finch M. “The Relationship of Patient Satisfaction with Care and Clinical Outcomes.”. Medical Care. 1997;35(7):714–30. doi: 10.1097/00005650-199707000-00005. [DOI] [PubMed] [Google Scholar]
- Kaplan SH, Greenfield S, Ware JE. “Assessing the Effects of Physician–Patient Interactions on the Outcomes of Chronic Disease.”. Medical Care. 1989;27:S110–27. doi: 10.1097/00005650-198903001-00010. [DOI] [PubMed] [Google Scholar]
- Katz SJ, Lantz PM, Janz NK, Fagerlin A, Schwartz K, Liu L, Salem B, Lakhani I, Morrow M. American Society for Clinical Oncology Annual Meeting. New Orleans, Louisiana: 2004. “Shared Decision-Making and Receipt of Surgical Treatment for Women with Breast Cancer.”. [Google Scholar]
- Katz SJ, Lantz PM, Zemencuk J. “Correlates of Surgical Treatment Choice for Women with Non-Invasive and Invasive Breast Cancer.”. Journal of Women's Health and Gender-Based Medicine. 2001;10:659–70. doi: 10.1089/15246090152563533. [DOI] [PubMed] [Google Scholar]
- Keating NL, Guadagnoli E, Landrum MB, Borbas C, Weeks JC. “Treatment Decision Making in Early Stage Breast Cancer: Should Surgeons Match Patients' Desired Level of Involvement?”. Journal of Clinical Oncology. 2002;20(6):1473–9. doi: 10.1200/JCO.2002.20.6.1473. [DOI] [PubMed] [Google Scholar]
- Lantz PM, Zemencuk J, Katz SJ. “Is Mastectomy Overused? A Call for an Expanded Research Agenda.”. Health Services Research. 2002;37(2):417–31. doi: 10.1111/1475-6773.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Laine C, Davidoff F. “Patient-Centered Medicine.”. Journal of the American Medical Association. 1996;175:152–6. [Google Scholar]
- Lazovich D, White E, Thomas DB, Moe RE. “Underutilization of Breast-Conserving Surgery and Radiation Therapy among Women with Stage I and II Breast Cancer.”. Journal of the American Medical Association. 1991;266:3433–8. [PubMed] [Google Scholar]
- Liang W, Burnett CB, Rowland JH, Meropol NJ, Eggert L, Hwang YT, Silliman RA, Weeks JC, Mandelblatt JS. “Communication between Physicians and Older Women with Localized Breast Cancer: Implications for Treatment and Patient Satisfaction.”. Journal of Clinical Oncology. 2002;20(4):1008–16. doi: 10.1200/JCO.2002.20.4.1008. [DOI] [PubMed] [Google Scholar]
- Mandelblatt JS, Edge SB, Meropol NJ, Seine R, Tsangaris T, Grey L, Peterson BM, Jr., Hwang YT, Kerner J, Weeks J. “Predictors of Long-Term Outcomes in Older Breast Cancer Survivors: Perceptions versus Patterns of Care.”. Journal of Clinical Oncology. 2003;21(5):855–63. doi: 10.1200/JCO.2003.05.007. [DOI] [PubMed] [Google Scholar]
- Mandelblatt JS, Hadley J, Kerner JF, Schulman KA, Gold K, Dunmore-Griffith J, Edge S, Guadagnoli E, Lynch JJ, Meropol NJ, Weeks JC, Winn R. “Patterns of Breast Carcinoma Treatment in Older Women: Patient Preference and Clinical and Physical Influences.”. Cancer. 2000;89(3):561–73. [PubMed] [Google Scholar]
- Montini T. “Resist and Redirect: Physicians Respond to Breast Cancer Informed Consent Legislation.”. Women and Health. 1997;26:85–104. doi: 10.1300/J013v26n01_06. [DOI] [PubMed] [Google Scholar]
- Morris CR, Cohen R, Schlag R, Wright WE. “Increasing Trends in the Use of Breast-Conserving Surgery in California.”. American Journal of Public Health. 2000;90:281–4. doi: 10.2105/ajph.90.2.281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moyer A, Salovey P. “Patient Participation in Treatment Decision Making and the Psychological Consequences of Breast Cancer Surgery.”. Women's Health. 1998;4(2):103–16. [PubMed] [Google Scholar]
- Murray-Garcia JL, Selvy JV, Schmittdiel J, Grumbach K, Quesenberry CP. “Racial and Ethnic Differences in Patient Surveys: Patients' Values, Ratings, and Reports Regarding Physician Primary Care Performance in a Large Health Maintenance Organization.”. Medical Care. 2000;38(3):300–10. doi: 10.1097/00005650-200003000-00007. [DOI] [PubMed] [Google Scholar]
- National Cancer Policy Board, Institute of Medicine and National Research Council. In: Ensuring Quality Cancer Care. Hewitt M, Simone JV, editors. Washington, DC: National Academy Press; 1999. [Google Scholar]
- National Institutes of Health. National Institutes of Health Consensus Development Conference Statement. The Treatment of Early Stage Breast Cancer. Bethesda, MD: NIH; 1990. June 18–21. [PubMed] [Google Scholar]
- Nayfield SG, Bongiovanni GC, Alciati MH, Fischer RA, Bergner L. “Statutory Requirements for Disclosure of Breast Cancer Treatment Alternatives.”. Journal of the National Cancer Institute. 1994;86:1202–8. doi: 10.1093/jnci/86.16.1202. [DOI] [PubMed] [Google Scholar]
- Nold RJ, Beamer RL, Helmer SD, McBoyle MF. “Factors Influencing a Woman's Choice to Undergo Breast-Conserving Surgery versus Modified Radical Mastectomy.”. American Journal of Surgery. 2000;180(6):413–8. doi: 10.1016/s0002-9610(00)00501-8. [DOI] [PubMed] [Google Scholar]
- Pierce PF. “Deciding on Breast Cancer Treatment: A Description of Decision Behavior.”. Nursing Research. 1993;42:22–8. [PubMed] [Google Scholar]
- Pierce PF. “When the Patient Chooses: Describing Unaided Decisions in Health Care.”. Human Factors. 1996;38:278–87. doi: 10.1177/001872089606380208. [DOI] [PubMed] [Google Scholar]
- Robinson A, Thompsom R. “Variability in Patient Preferences for Participating in Medical Decision-Making: Implication for the Use of Decision Support Tools.”. Quality in Health Care. 2001;102:520–8. doi: 10.1136/qhc.0100034... [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schneider CE. “From Consumer Choice to Consumer Welfare.”. 1995:S25–8. Hastings Center Report. [PubMed] [Google Scholar]
- Sepucha KR, Belkora JK, Tripahty D, Esserman LJ. “Building Bridges between Physicians and Patients: Results of a Pilot Study Examining New Tools for Collaborative Decision Making in Breast Cancer.”. Journal of Clinical Oncology. 2000;18(6):1230–8. doi: 10.1200/JCO.2000.18.6.1230. [DOI] [PubMed] [Google Scholar]
- Street RL, Voigt B. “Patient Participation in Deciding Breast Cancer Treatment and Subsequent Quality of Life.”. Medical Decision Making. 1997;17:298–306. doi: 10.1177/0272989X9701700306. [DOI] [PubMed] [Google Scholar]
- Street RL, Voigt B, Geyer C, Jr., Manning T, Swanson GP. “Increasing Patient Involvement in Choosing Treatment for Early Breast Cancer.”. Cancer. 1995;76:2275–83. doi: 10.1002/1097-0142(19951201)76:11<2275::aid-cncr2820761115>3.0.co;2-s. [DOI] [PubMed] [Google Scholar]
- Wennberg JE. “Unwarranted Variations in Healthcare Delivery: Implications for Academic Medical Centres.”. British Medical Journal. 2002a;325:961–4. doi: 10.1136/bmj.325.7370.961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wennberg JE. “Testimony before the Subcommittee on Health of the House Committee on Ways and Means, Hearing on Promoting Disease Management in Medicare”. 2002b. [accessed on March 8, 2004]. Available at http://waysandmeans.house.gov/legacy/health/107cong/4-16-02/4-16wenn.htm.
- Whelan T, Levine M, Gafni A, Sanders K, Willan A, Mirsky D, Schnider D, McCread D, Reid S, Kobylecky A, Reed K. “Mastectomy or Lumpectomy? Helping Women Make Informed Choices.”. Journal of Clinical Oncology. 1999;17(6):1727–35. doi: 10.1200/JCO.1999.17.6.1727. [DOI] [PubMed] [Google Scholar]