Abstract
Foreign viral proteins expressed by rabies virus (RV) have been shown to induce potent humoral and cellular immune responses in immunized animals. In addition, highly attenuated and, therefore, very safe RV-based vectors have been constructed. Here, an RV-based vaccine vehicle was utilized as a novel vaccine against severe acute respiratory syndrome coronavirus (SARS-CoV). For this approach, the SARS-CoV nucleocapsid protein (N) or envelope spike protein (S) genes were cloned between the RV glycoprotein G and polymerase L genes. Recombinant vectors expressing SARS-CoV N or S protein were recovered and their immunogenicity was studied in mice. A single inoculation with the RV-based vaccine expressing SARS-CoV S protein induced a strong SARS-CoV-neutralizing antibody response. The ability of the RV-SARS-CoV S vector to confer immunity after a single inoculation makes this live vaccine a promising candidate for eradication of SARS-CoV in animal reservoirs, thereby reducing the risk of transmitting the infection to humans.
INTRODUCTION
In November 2002, an atypical pneumonia now known as severe acute respiratory syndrome (SARS) emerged in humans in China and then spread to different countries, including Canada (Drosten et al., 2003; Holmes, 2003; Peiris et al., 2003). The mortality rate of this disease was ~3–6 %, but was as high as 50 % in people over 60 years (Drosten et al., 2003; Holmes, 2003; Peiris et al., 2003). A coronavirus termed SARS-CoV has been identified as the aetiological agent of SARS (Drosten et al., 2003). The genome of SARS-CoV is a 29 727 nt, positive-strand RNA with a genomic organization typical of coronaviruses encoding a replicase (rep), spike (S), envelope (E), membrane (M), nucleocapsid (N) and several other small non-structural proteins (Rota et al., 2003).
Although the SARS epidemic reached its peak at the end of April 2003 and drastically declined thereafter, with few cases reported after June 2003, SARS could return in several ways. The virus may still be carried by some asymptomatic people or, more importantly, the virus may circulate in certain animal species. Regarding the latter situation, coronaviruses almost identical to SARS-CoV have been identified in several wild animal species such as masked palm civets, raccoon dogs and the Chinese ferret badger (Guan et al., 2003). The existence of such animal reservoirs could make control or even eradication of the SARS virus very difficult, if not impossible.
Prophylactic immunization would be the most effective solution to control SARS in humans (Holmes, 2003) and to eradicate SARS virus reservoirs in animals. Protective immunity against the SARS virus could be achieved through vaccination using either killed or live attenuated SARS virus or recombinant virus vaccines expressing particular SARS-CoV proteins. However, it is not yet clear which immune effectors (e.g. antibodies, effector T cells) are capable of either protecting against SARS or enhancing the infection. In this context, several vaccines against feline coronavirus have caused antibody-dependent enhancement of the disease when animals were subsequently infected with the wild-type virus (Holmes, 2003). Thus, several approaches to the development of safe and effective SARS vaccines must be pursued.
For vaccination of free-ranging wildlife, oral vaccination with live attenuated or recombinant virus vaccines is probably the only effective method to control and eventually eradicate a virus infection. The feasibility of this approach has been demonstrated in vaccination campaigns against wildlife rabies, which has resulted in the almost complete eradication of rabies in Western Europe (Aubert et al., 1994). The precise mechanism by which oral immunization with modified live rabies virus (RV) vaccines confers protective immunity is not known. However, it has been shown that the tonsils, a major lymphoid tissue that contains B and T cells as well as antigen-presenting cells, including dendritic cells, is a primary site of infection and replication of the RV vaccine strains (Orciari et al., 2001).
RV has been introduced as a vaccine vector (Foley et al., 2000, 2002; McGettigan et al., 2001a, b, 2003a, McGettigan et al., b; Morimoto et al., 2001b; Schnell et al., 2000; Siler et al., 2002) that could also be used for the expression of relevant SARS virus antigens. There are several advantages of RV that suggest its suitability as an expression vector for SARS virus proteins: (i) the modular genome of RV is organized with short transcription stop/start sequences flanking the genes making it readily amenable to manipulation (Foley et al., 2000); (ii) the RV genome is RNA and the life cycle of RV is exclusively cytoplasmic so no recombination, reversion or integration is observed (McGettigan et al., 2003a; Schnell et al., 1994); (iii) stable incorporation of large and multiple foreign genes of up to 6.5 kb offers advantages over plus-stranded RNA virus vectors (McGettigan et al., 2003a); (iv) RV is non-cytopathic in infected cells and expresses high levels of foreign proteins over extended periods of time (McGettigan et al., 2001b, 2003a, McGettigan et al., b); (v) RV can induce a protective immune response in a variety of animals (e.g. dog and mongoose) following immunization by the oral route (Meslin et al., 1994; Rupprecht et al., 2001) and attenuated RV can target cells in the tonsils and buccal mucosa (Orciari et al., 2001); (vi) multiple mutations introduced into the RV genome that completely abolish the pathogenicity of RV render the RV vector extremely safe (McGettigan et al., 2003b) and replication-defective RVs can be produced that are even safe for completely immunocompromised individuals (reviewed by Dietzschold et al., 2003; Shoji et al., 2004); and (vii) since RV contains a nucleocapsid protein that has the properties of a super-antigen (Lafon et al., 1992), the RV vector is a unique vaccine delivery vehicle.
In this paper, construction of replication-competent recombinant RVs that express the SARS-CoV S or N proteins is described and the immunogenicities of these recombinant viruses were determined in mice.
METHODS
Cells
BSR cells, a BHK-21-derived clone, were grown in DMEM (Mediatech) supplemented with 10 % fetal bovine serum. Mouse neuroblastoma cells (NA) were grown in RPMI medium (Mediatech) supplemented with 10 % fetal bovine serum.
Plasmid construction
The RV vector pSPBNGA, derived from pSPBN (McGettigan et al., 2001b), encodes an RV G protein with an arginine to glutamic acid exchange at position 333 that abolishes the pathogenicity of this RV (reviewed by Dietzschold et al., 2003). cDNAs encoding the SARS-CoV N or S proteins were kindly provided by W. Bellini (Centers for Disease Control, Atlanta, GA, USA). The SARS-CoV N and S genes were amplified using Deep Vent polymerase (New England Biolabs) and the N gene-specific primers NEB(+) (5′-CCGGAATTCCGTACGAAGATGTCTGATA-ATGGACCCCAATCAAACCAAC-3′; BsiWI site underlined, start codon in bold) and NXX(−) (5′-TACCGCTCGAGCGGCGTCTAG-ACGTTTATGCCTGAGTTGAATCAGCAG-3′; XbaI site underlined, stop codon in bold) or S gene-specific primers SEB(+) (5′-CC-GGAATTCCGTACGAAGATGTTTATTTTCTTATTATTTCTTACTC-TCAC-3′; BsiWI site underlined, start codon in bold) and SXN(−) (5′-TACCGCTCGAGCGGCGGCTAGCCGTTTATGTGTAATGTAA-TTTGACACCC-3′; NheI site underlined, stop codon in bold). PCR products were digested with BsiWI and NheI and cloned into pSPBNGA, which had been previously digested with BsiWI and NheI. The presence and sequence of the SARS-CoV S and N genes and the flanking vector sequences were confirmed by sequencing.
Generation of recombinant viruses
Recombinant viruses were rescued as described previously (McGettigan et al., 2003a; McKenna et al., 2003). Briefly, BSR-T7 cells were transfected using a calcium phosphate transfection kit (Stratagene) with 5.0 μg pSPBNGA-SN or pSPBNGA-SS and 5.0 μg pTIT-N, 2.5 μg pTIT-P, 2.5 μg pTIT-L and 2.0 μg pTIT-G. After a 3-day incubation, supernatants were transferred onto BSR cells and incubation continued for 3 days at 37 °C. Cells were examined for the presence of rescued virus by immunostaining with fluorescein isothiocyanate (FITC)-labelled anti-RV N protein antibody (Centocor).
Preparation of virus stocks and virus titration
BSR cells were infected at an m.o.i. of 0.1 and incubated for 72 h at 34 °C. To determine virus yields, monolayers of NA cells in 96-well plates were infected with serial 10-fold virus dilutions as described elsewhere (Wiktor et al., 1984). At 48 h post-infection (p.i.), cells were fixed in 80 % acetone and stained with FITC-labelled RV N protein-specific antibody (Centocor). Foci were counted using a fluorescence microscope and virus titres are given as focus-forming units (f.f.u.). All titrations were determined in triplicate.
Immunofluorescence analysis
NA cells were infected at an m.o.i. of 5. At 48 h p.i., cells were fixed with 4 % paraformaldehyde and then incubated with a human SARS convalescence serum (kindly provided by I. Lipkin, Mailman School of Public Health, Columbia University New York, NY, USA) followed by FITC-labelled goat anti-human IgG (Jackson ImmunoResearch Laboratories).
Western blot analysis
BSR cells were infected with recombinant virus at an m.o.i. of 5 or mock infected. After 24 h incubation at 37 °C, cells were lysed with lysis buffer [50 mM Tris, pH 7.4, 150 mM NaCl, 1 % NP-40, 0.1 % SDS, 1× protease inhibitor cocktail (Sigma)], subjected to 10 % SDS-PAGE and transferred to a nitrocellulose membrane (Millipore). Blots were blocked overnight in 5 % dry milk powder in PBS (pH 7.4), then washed three times using PBS containing 0.1 % Tween 20 and incubated with a SARS convalescence serum (final dilution 1 : 100) for 4 h at room temperature. Blots were then washed again three times with PBS/0.1 % Tween 20 and secondary goat anti-human IgG (final dilution 1 : 1000) conjugated to Alexa Fluor 555 (Molecular Probes) was added. Blots were incubated for 1 h at room temperature and, after three 10 min washes, scanned using Molecular Imager FX and Quantity One software (Bio-Rad).
Immunoprecipitation analysis
For immunoprecipitation analysis, NA cell cultures were infected with recombinant viruses at an m.o.i. of 5 or mock infected. At 24 h p.i., the medium was replaced with methionine-free RPMI containing 100 μCi (3.7 MBq) [35S]methionine and incubated at 37 °C for 1 h. Cells were lysed with lysis buffer (10 mM Tris/HCl, pH 7.4, 150 mM NaCl, 1 % Triton X-100, 0.5 % sodium deoxycholate). Two microlitres of anti-SARS-CoV S antibody (SARS-Sn antibody; Abgent) was added to 400 μl lysate and the mixture was incubated overnight at 4 °C. The resulting immunocomplexes were adsorbed to protein A–Sepharose beads, solubilized in loading buffer and subjected to 10 % SDS-PAGE. Gels were dried and placed into a storage phosphor screen cassette for 24 h and protein bands were scanned using a Phosphorimager (Molecular Dynamics) and Quantity One software (Bio-Rad).
Immunization of mice
Four- to six-week-old female BALB/c mice were purchased from Taconic. Groups of five mice were immunized intra-muscularly (i.m.) with 100 μl samples containing 107 f.f.u. SPBNGA-SS or SPBNGA-SN and, 2 weeks later, blood was collected under isoflurane anaesthesia by retro-orbital bleeding. Sera from each group were pooled and heat-inactivated at 65 °C for 30 min.
SARS-CoV-neutralizing antibody assay
Two-fold dilutions of heat-inactivated sera were tested in a microneutralization assay for the presence of antibodies that neutralized the infectivity of 100 TCID50 SARS-CoV in Vero cell monolayers, using 4 wells per dilution on a 96-well plate as previously described (Subbarao et al., 2004). The presence of virus cytopathic effect (CPE) was read on days 3 and 4. The dilution of serum that completely prevented CPE in 50 % of the wells was calculated by the Reed–Muench formula (Reed & Muench, 1938).
Determination of RV-neutralizing antibody
Mouse sera were heat-inactivated at 65 °C for 30 min and neutralizing activity was determined using the rapid fluorescent focus inhibition test (RFFIT) assay as described previously (Wiktor et al., 1984).
RESULTS
Construction of attenuated RVs expressing SARS-CoV N and SARS-CoV S
Our new vaccine constructs are based on vector pSPBNGA (also termed pSPBN-333), which carries an RV G gene with an Arg333→Glu333 mutation that renders RV apathogenic even after intra-cranial inoculation. Utilizing the single BsiWI and NheI restriction sites, the SARS-CoV N or S genes were inserted between the G and L genes of pSPBNGA, resulting in pSPBNGA-SN and pSPBNGA-SS, respectively (Fig. 1). Infectious virus was recovered by standard methods from pSPBNGA-SN and pSPBNGA-SS as described previously (McGettigan et al., 2001a, b).
Fig. 1.
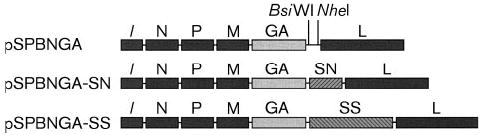
Construction of recombinant RVs containing the SARS-CoV N gene (SN) and SARS-CoV S gene (SS).
Expression of SARS-CoV N and SARS-CoV S by recombinant RVs
To determine whether the recombinant RVs express the SARS-CoV N and S proteins correctly, mouse NA cells were infected with SPBNGA, SPBNGA-SN or SPBNGA-SS at an m.o.i. of 5 and the expression of SARS-CoV N or S proteins was analysed 48 h later using immunofluorescence and a human SARS convalescence serum. Fig. 2 shows the results of the fluorescence staining of NA cells infected with SPBNGA (a), SPBNGA-SN (b) or SPBNGA-SS (c). While no signal was detected for SPBNGA-infected cells, cells infected with SPBNGA-SN and SPBNGA-SS showed brilliantly stained intracellular inclusion body (Fig. 2b) or cell surface (Fig. 2c) staining, respectively.
Fig. 2.
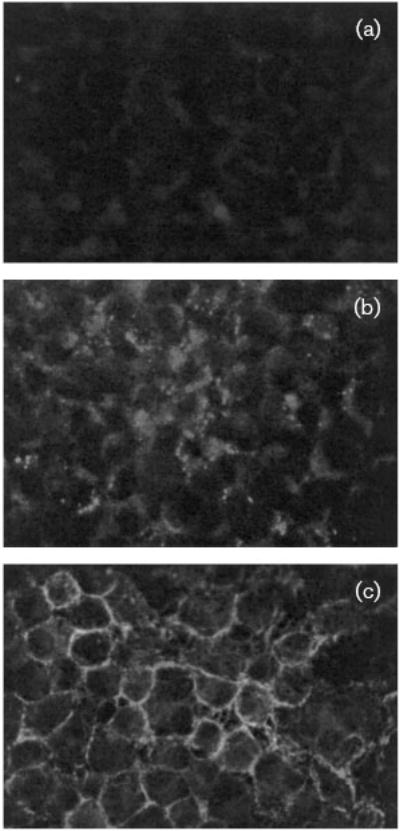
Immunofluorescence analysis of NA cells infected with SPBNGA (a), SPBNGA-SN (b) or SPBNGA-SS (c). Magnification ×20.
After expression of the two SARS-CoV proteins was confirmed by immunofluorescence, Western blot analysis using a human SARS convalescence serum was performed. As shown in Fig. 3(a), the human serum revealed a protein of ~47 kDa in SPBNGA-SN-infected BSR cell lysates, which is the expected size for the SARS-CoV N protein. Of note, this protein was not detected in either uninfected or vector (SPBNGA)-infected cells. However, the same human SARS convalescence serum failed to detect the SARS-CoV S protein in SPBNGA-SS-infected cell lysate using the same Western blot assay. The SARS-CoV S protein was also not detected using a polyclonal rabbit antibody directed against the N terminus of the SARS-CoV S protein (anti-SARS-Sn). It was decided, therefore, to perform immunoprecipitations to detect the native SARS-CoV S protein. SDS-PAGE of an immunoprecipitate obtained with a lysate prepared from [35S]methionine-labelled SPBNGA-SS-infected cells using the anti-SARS-Sn antibody revealed a protein of ~140 kDa that is absent from the lysate of SPBNGA-infected cells (Fig. 3b). These experiments indicate that the RV expression vector is capable of expressing antigenically active SARS-CoV S, as well as SARS-CoV N protein.
Fig. 3.
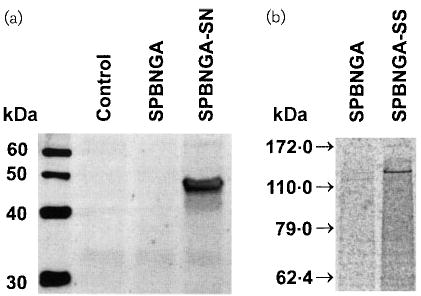
(a) Western blot analysis of lysates from uninfected (control), SPBNGA-infected and SPBNGA-SN-infected BSR cells using a human SARS convalescence serum. (b) SDS-PAGE of immunoprecipitates prepared with a commercial anti-SARS-CoV S antibody and lysates of [35S]methionine-labelled SPBNGA-infected or SPBNGA-SS-infected NA cells.
Immunogenicity of SPBNGA-SN and SPBNGA-SS
The goal of this study was to develop a live anti-SARS-CoV vaccine that can be used to immunize wildlife species that carry SARS-CoV, thereby reducing the risk of transmitting the virus to other animals or humans. Of note, a prerequisite for such a vaccination would be that a single dose of the vaccine is sufficient to induce neutralizing antibodies. To examine whether the recombinant RV-SARS-CoVs are immunogenic, BALB/c mice received a single i.m. inoculation with 107 f.f.u. SPBNGA-SS or SPBNGA-SN. Blood was collected 2 weeks later and sera from SPBNGA-SS-immunized mice were tested for their ability to recognize SARS-CoV S. SDS-PAGE of immunoprecipitates obtained with [35S]methionine-labelled SPBNGA-SS-infected cell lysate and immune serum from SPBNGA-SS-immunized mice revealed a protein of 140 kDa (Fig. 4). The mouse immune sera did not recognize this protein in the lysate of cells infected with the empty vector (SPBNGA). Thus, immunization of mice with SPBNGA-SS can trigger the production of SARS-CoV S-specific antibodies. On the other hand, SARS-CoV N-specific antibodies were not detected in sera of mice immunized with SPBNGA-SN using either Western blot or immunoprecipitation assays.
Fig. 4.
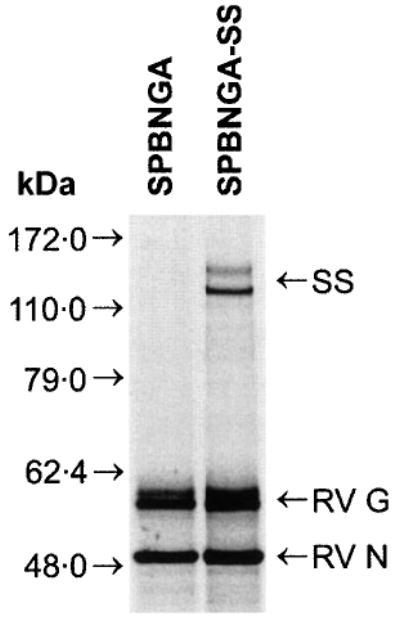
SDS-PAGE of immunoprecipitates prepared with sera obtained from SPBNGA-SS-immunized mice and lysates of [35S]methionine-labelled SPBNGA-infected or SPBNGA-SS-infected NA cells.
Sera from SPBNGA-SS immunized mice induce high levels of SARS-CoV-neutralizing antibodies
In the next step, the virus-neutralizing activity of the sera of mice immunized with SPBNGA, SPBNGA-SN and SPBNGA-SS was analysed. Pooled sera from five BALB/c mice from each group were tested for the presence of both SARS-CoV- and RV-neutralizing antibodies as described above. As expected, SARS-CoV-neutralizing antibodies were detected only in the sera of mice that were immunized with SPBNGA-SS (1 : 161; Table 1), whereas sera from mice immunized with the empty vector or the vaccine vehicle expressing the SARS-CoV N protein had no neutralizing activity (<1 : 8; Table 1). However, all three recombinant RVs induced comparable amounts of RV-neutralizing antibodies (Table 1), i.e. between 12 and 18 IU, suggesting that the three recombinant RVs replicate at similar rates in vivo. These data indicate that a highly attenuated RV-based vector can serve as a potent live virus vaccine against SARS-CoV.
Table 1.
Virus-neutralizing antibody (VNA) response in BALB/c mice immunized with recombinant SARS-CoV-RV vaccines
|
VNA titres |
||
|---|---|---|
| Vaccine | RV (IU ml−1)* | SARS-CoV† |
| SPBNGA | 12 | <1 : 8 |
| SPBNGA-SS | 12 | 1 : 161 |
| SPBNGA-SN | 18 | <1 : 8 |
| Control/uninfected | 0 | na |
RV VNA titres were determined by the RFFIT assay and VNA titres were calibrated to IU using the WHO standard.
SARS-CoV VNA titre is the dilution that neutralizes the infectivity of 100 TCID50 of SARS-CoV in Vero cell monolayers.
na, Not available.
DISCUSSION
SARS-CoV is most likely transmitted via aerosol and there is evidence that certain wildlife species are the reservoir for this virus. Prophylactic immunization would be the most effective solution to protect the human population against infection with SARS virus. Here, an RV-based vector has been used to develop a vaccine against SARS. RV-based vectors show great promise as vaccines against other viruses such as human immunodeficiency virus type 1 (Schnell et al., 2000) and hepatitis C virus (Siler et al., 2002) and induce strong cellular and humoral responses (McGettigan et al., 2001a, b, 2003a). One of the advantages of the RV-based recombinant vaccines, it is presumed, like RV variants such as SAG-2 virus, is their ability to replicate in cells of the mucosal membrane (Orciari et al., 2001), probably making them uniquely suited to induce mucosal immunity in the defence against virus infections like SARS. However, mice are not a good model for oral immunization with RV and a previous study indicates that only 40 % of mice orally immunized with our RV vector were protected against RV challenge. In addition, RV-specific seroconversion against RV N and G was generally low (Morimoto et al., 2001a). Therefore, this initial study in mice was performed using i.m. inoculations. However, in larger animals like dogs, oral immunization is more successful and a recent study showed 100 % protection against RV challenge with our RV vector in this setting (Rupprecht et al., 2005).
With respect to safety, recombinant viruses containing RV G protein with an Arg333→Glu333 mutation have been shown to be non-pathogenic for adult mice after intracranial infection (McGettigan et al., 2003b; Morimoto et al., 2000, 2001a). Therefore, the constructs used for the design of new SARS-CoV recombinant viruses carry the SPBNG with an Arg333→Glu333. Inoculation of these viruses into adult BALB/c mice did not cause any clinical signs or discomfort, strongly suggesting that these vaccines are safe for immunocompetent mammals including humans. However, replication-competent recombinant RVs may cause undesirable side effects in immunocompromised individuals. To overcome this potential problem, replication-deficient recombinant SARS-CoV-S-RV vaccines can be developed by deletion of a different RV gene as shown for example for RV P (Shoji et al., 2004).
Evidence that SARS-CoV-specific neutralizing antibodies alone can prevent replication of the SARS-CoV comes from a recent study that used passive transfer of such antibodies in a mouse model to prevent replication of SARS-CoV (Subbarao et al., 2004). Therefore, this study was directed to the humoral response against SARS-CoV induced by an RV vaccine vector. Our data indicate that a single vaccination with the RV-based vaccine expressing the SARS-CoV S protein induces the production of high levels (1 : 161; Table 1) of SARS-CoV-neutralizing antibodies in mice. Whereas other SARS vaccine approaches induced similar levels of anti-SARS-CoV-directed antibodies, multiple vaccine inoculations were required. For example, vaccination of BALB/c mice using naked DNA encoding the SARS-CoV S protein induced levels of SARS-CoV-neutralizing antibodies in the range of 1 : 50 to 1 : 150, but three inoculations were required (Yang et al., 2004). It has been shown for the attenuated modified vaccinia virus Ankara (MVA) that two inoculations of mice with recombinant MVA expressing SARS-CoV S induce SARS-CoV-neutralizing antibody titres of about 1 : 100, which protect the immunized mice from subsequent challenge with SARS-CoV (Bisht et al., 2004). The failure to detect antibodies against the SARS-CoV N protein was not surprising. In general, a single inoculation with RV induces mainly antibodies against the surface G protein and not against the internal proteins of RV. Therefore, multiple inoculations with the recombinant RV expressing SARS-CoV N are probably required to induce SARS-CoV anti-N antibodies.
Because oral immunization with live replication-competent RV vaccines has been shown to be the only effective method to eradicate RV reservoirs in wildlife, a recombinant RV-SARS vaccine might be very useful in eradicating SARS virus reservoirs. Of note, the immunization of wildlife requires that a single inoculation is able to induce protection against SARS-CoV and our results indicate that this approach might be feasible with an RV-based vaccine. However, further studies in the target species will indicate whether or not our novel SARS-CoV vaccine approach is able to induce similar high levels of neutralizing antibodies via mucosal immunizations. The high level of RV-neutralizing antibodies detected after a single immunization in mongoose indicates that this approach is feasible (Rupprecht et al., 2001).
References
- Aubert, M. F. A., Masson, E., Artois, M. & Barrat, J. (1994). Oral wildlife rabies vaccination field trails in Europe with recent emphasis on France. In Lyssaviruses, pp. 219–243. Edited by C. E. Rupprecht, B. Dietzschold & H. Koprowski. Berlin, Heidelberg, New York: Springer. [DOI] [PubMed]
- Bisht H, Roberts A, Vogel L, Bukreyev A, Collins PL, Murphy BR, Subbarao K, Moss B. Severe acute respiratory syndrome coronavirus spike protein expressed by attenuated vaccinia virus protectively immunizes mice. Proc Natl Acad Sci U S A. 2004;101:6641–6646. doi: 10.1073/pnas.0401939101. (Epub 2004 Apr 19). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dietzschold B, Faber M, Schnell MJ. New approaches to the prevention and eradication of rabies. Expert Rev Vaccines. 2003;2:399–406. doi: 10.1586/14760584.2.3.399. [DOI] [PubMed] [Google Scholar]
- Drosten C, Gunther S, Preiser W 23 other authors. Identification of a novel coronavirus in patients with severe acute respiratory syndrome. N Engl J Med. 2003;348:1967–1976. doi: 10.1056/NEJMoa030747. [DOI] [PubMed] [Google Scholar]
- Foley HD, McGettigan JP, Siler CA, Dietzschold B, Schnell MJ. A recombinant rabies virus expressing vesicular stomatitis virus glycoprotein fails to protect against rabies virus infection. Proc Natl Acad Sci U S A. 2000;97:14680–14685. doi: 10.1073/pnas.011510698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Foley HD, Otero M, Orenstein JM, Pomerantz RJ, Schnell MJ. Rhabdovirus-based vectors with human immunodeficiency virus type 1 (HIV-1) envelopes display HIV-1-like tropism and target human dendritic cells. J Virol. 2002;76:19–31. doi: 10.1128/JVI.76.1.19-31.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guan Y, Zheng BJ, He YQ 15 other authors. Isolation and characterization of viruses related to the SARS coronavirus from animals in southern China. Science. 2003;302:276–278. doi: 10.1126/science.1087139. [DOI] [PubMed] [Google Scholar]
- Holmes KV. SARS coronavirus: a new challenge for prevention and therapy. J Clin Invest. 2003;111:1605–1609. doi: 10.1172/JCI18819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lafon M, Lafage M, Martinez-Arends A, Ramirez R, Vuillier F, Charron D, Lotteau V, Scott-Algara D. Evidence for a viral superantigen in humans. Nature. 1992;358:507–510. doi: 10.1038/358507a0. [DOI] [PubMed] [Google Scholar]
- McGettigan JP, Foley HD, Belyakov IM, Berzofsky JA, Pomerantz RJ, Schnell MJ. Rabies virus-based vectors expressing human immunodeficiency virus type 1 (HIV-1) envelope protein induce a strong, cross-reactive cytotoxic T-lymphocyte response against envelope proteins from different HIV-1 isolates. J Virol. 2001a;75:4430–4434. doi: 10.1128/JVI.75.9.4430-4434.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McGettigan JP, Sarma S, Orenstein JM, Pomerantz RJ, Schnell MJ. Expression and immunogenicity of human immunodeficiency virus type 1 Gag expressed by a replication-competent rhabdovirus-based vaccine vector. J Virol. 2001b;75:8724–8732. doi: 10.1128/JVI.75.18.8724-8732.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McGettigan JP, Naper K, Orenstein J, Koser M, McKenna PM, Schnell MJ. Functional human immunodeficiency virus type 1 (HIV-1) Gag-Pol or HIV-1 Gag-Pol and env expressed from a single rhabdovirus-based vaccine vector genome. J Virol. 2003a;77:10889–10899. doi: 10.1128/JVI.77.20.10889-10899.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McGettigan JP, Pomerantz RJ, Siler CA, McKenna PM, Foley HD, Dietzschold B, Schnell MJ. Second-generation rabies virus-based vaccine vectors expressing human immunodeficiency virus type 1 gag have greatly reduced pathogenicity but are highly immunogenic. J Virol. 2003b;77:237–244. doi: 10.1128/JVI.77.1.237-244.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McKenna PM, Pomerantz RJ, Dietzschold B, McGettigan JP, Schnell MJ. Covalently linked human immunodeficiency virus type 1 gp120/gp41 is stably anchored in rhabdovirus particles and exposes critical neutralizing epitopes. J Virol. 2003;77:12782–12794. doi: 10.1128/JVI.77.23.12782-12794.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meslin, F.-X., Fishbein, D. B. & Matter, H. C. (1994). Rationale and prospects for rabies elimination in developing countries. In Lyssaviruses, pp. 1–26. Edited by B. D. C. E. Rupprecht & H. Koprowski. Berlin, Heidelberg, New York: Springer. [DOI] [PubMed]
- Morimoto K, Foley HD, McGettigan JP, Schnell MJ, Dietzschold B. Reinvestigation of the role of the rabies virus glycoprotein in viral pathogenesis using a reverse genetics approach. J Neurovirol. 2000;6:373–381. doi: 10.3109/13550280009018301. [DOI] [PubMed] [Google Scholar]
- Morimoto K, McGettigan JP, Foley HD, Hooper DC, Dietzschold B, Schnell MJ. Genetic engineering of live rabies vaccines. Vaccine. 2001a;19:3543–3551. doi: 10.1016/s0264-410x(01)00064-0. [DOI] [PubMed] [Google Scholar]
- Morimoto K, Schnell MJ, Pulmanausahakul R, McGettigan JP, Foley HD, Faber M, Hooper DC, Dietzschold B. High level expression of a human rabies virus-neutralizing monoclonal antibody by a rhabdovirus-based vector. J Immunol Methods. 2001b;252:199–206. doi: 10.1016/s0022-1759(01)00353-2. [DOI] [PubMed] [Google Scholar]
- Orciari LA, Niezgoda M, Hanlon CA, Shaddock JH, Sanderlin DW, Yager PA, Rupprecht CE. Rapid clearance of SAG-2 rabies virus from dogs after oral vaccination. Vaccine. 2001;19:4511–4518. doi: 10.1016/s0264-410x(01)00186-4. [DOI] [PubMed] [Google Scholar]
- Peiris JS, Lai ST, Poon LL 14 other authors. Coronavirus as a possible cause of severe acute respiratory syndrome. Lancet. 2003;361:1319–1325. doi: 10.1016/S0140-6736(03)13077-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reed LJ, Muench H. A simple method of estimating fifty percent endpoints. Am J Hyg. 1938;27:493–497. [Google Scholar]
- Rota PA, Oberste MS, Monroe SS 32 other authors. Characterization of a novel coronavirus associated with severe acute respiratory syndrome. Science. 2003;300:1394–1399. doi: 10.1126/science.1085952. [DOI] [PubMed] [Google Scholar]
- Rupprecht, C. E., Hanlon, C. A., Niezgoda, M., Murphy, S., Schnell, M. J. & Dietzschold, B. (2001). Oral rabies vaccination of the mongoose, Herpestes auropunctatus In Rabies in the Americas. XII International Meeting on Advances in Rabies Research and Control in the Americas Peterborough, Ontario, Canada.
- Rupprecht, C. E., Hanlon, C. A., Blanton, J. & 7 other authors (2005). Oral vaccination of dogs with recombinant rabies virus vaccines. Virus Res (in press). [DOI] [PubMed]
- Schnell MJ, Mebatsion T, Conzelmann KK. Infectious rabies viruses from cloned cDNA. EMBO J. 1994;13:4195–4203. doi: 10.1002/j.1460-2075.1994.tb06739.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schnell MJ, Foley HD, Siler CA, McGettigan JP, Dietzschold B, Pomerantz RJ. Recombinant rabies virus as potential live-viral vaccines for HIV-1. Proc Natl Acad Sci U S A. 2000;97:3544–3549. doi: 10.1073/pnas.050589197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shoji Y, Inoue S, Nakamichi K, Kurane I, Sakai T, Morimoto K. Generation and characterization of P gene-deficient rabies virus. Virology. 2004;318:295–305. doi: 10.1016/j.virol.2003.10.001. [DOI] [PubMed] [Google Scholar]
- Siler CA, McGettigan JP, Dietzschold B, Herrine SK, Dubuisson J, Pomerantz RJ, Schnell MJ. Live and killed rhabdovirus-based vectors as potential hepatitis C vaccines. Virology. 2002;292:24–34. doi: 10.1006/viro.2001.1212. [DOI] [PubMed] [Google Scholar]
- Subbarao K, McAuliffe J, Vogel L 7 other authors. Prior infection and passive transfer of neutralizing antibody prevent replication of severe acute respiratory syndrome coronavirus in the respiratory tract of mice. J Virol. 2004;78:3572–3577. doi: 10.1128/JVI.78.7.3572-3577.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wiktor TJ, Macfarlan RI, Foggin CM, Koprowski H. Antigenic analysis of rabies and Mokola virus from Zimbabwe using monoclonal antibodies. Dev Biol Stand. 1984;57:199–211. [PubMed] [Google Scholar]
- Yang ZY, Kong WP, Huang Y, Roberts A, Murphy BR, Subbarao K, Nabel GJ. A DNA vaccine induces SARS coronavirus neutralization and protective immunity in mice. Nature. 2004;428:561–564. doi: 10.1038/nature02463. [DOI] [PMC free article] [PubMed] [Google Scholar]


