Abstract
The present report meta-analyzes more than 300 empirical articles describing a relationship between psychological stress and parameters of the immune system in human participants. Acute stressors (lasting minutes) were associated with potentially adaptive upregulation of some parameters of natural immunity and downregulation of some functions of specific immunity. Brief naturalistic stressors (such as exams) tended to suppress cellular immunity while preserving humoral immunity. Chronic stressors were associated with suppression of both cellular and humoral measures. Effects of event sequences varied according to the kind of event (trauma vs. loss). Subjective reports of stress generally did not associate with immune change. In some cases, physical vulnerability as a function of age or disease also increased vulnerability to immune change during stressors.
Since the dawn of time, organisms have been subject to evolutionary pressure from the environment. The ability to respond to environmental threats or stressors such as predation or natural disaster enhanced survival and therefore reproductive capacity, and physiological responses that supported such responses could be selected for. In mammals, these responses include changes that increase the delivery of oxygen and glucose to the heart and the large skeletal muscles. The result is physiological support for adaptive behaviors such as “fight or flight.” Immune responses to stressful situations may be part of these adaptive responses because, in addition to the risk inherent in the situation (e.g., a predator), fighting and fleeing carries the risk of injury and subsequent entry of infectious agents into the bloodstream or skin. Any wound in the skin is likely to contain pathogens that could multiply and cause infection (Williams & Leaper, 1998). Stress-induced changes in the immune system that could accelerate wound repair and help prevent infections from taking hold would therefore be adaptive and selected along with other physiological changes that increased evolutionary fitness.
Modern humans rarely encounter many of the stimuli that commonly evoked fight-or-flight responses for their ancestors, such as predation or inclement weather without protection. However, human physiological response continues to reflect the demands of earlier environments. Threats that do not require a physical response (e.g., academic exams) may therefore have physical consequences, including changes in the immune system. Indeed, over the past 30 years, more than 300 studies have been done on stress and immunity in humans, and together they have shown that psychological challenges are capable of modifying various features of the immune response. In this article we attempt to consolidate empirical knowledge about psychological stress and the human immune system through meta-analysis. Both the construct of stress and the human immune system are complex, and both could consume book-length reviews. Our review, therefore, focuses on those aspects that are most often represented in the stress and immunity literature and therefore directly relevant to the meta-analysis.
Conceptualizing Stress
Despite nearly a century of research on various aspects of stress, investigators still find it difficult to achieve consensus on a satisfactory definition of this concept. Most of the studies contributing to this review simply define stress as circumstances that most people would find stressful, that is, stressors. We adopted Elliot and Eisdorfer’s (1982) taxonomy to characterize these stressors. This taxonomy has the advantage of distinguishing among stressors on two important dimensions: duration and course (e.g., discrete vs. continuous). The taxonomy includes five categories of stressors. Acute time-limited stressors involve laboratory challenges such as public speaking or mental arithmetic. Brief naturalistic stressors, such as academic examinations, involve a person confronting a real-life short-term challenge. In stressful event sequences, a focal event, such as the loss of a spouse or a major natural disaster, gives rise to a series of related challenges. Although affected individuals usually do not know exactly when these challenges will subside, they have a clear sense that at some point in the future they will. Chronic stressors, unlike the other demands we have described, usually pervade a person’s life, forcing him or her to restructure his or her identity or social roles. Another feature of chronic stressors is their stability—the person either does not know whether or when the challenge will end or can be certain that it will never end. Examples of chronic stressors include suffering a traumatic injury that leads to physical disability, providing care for a spouse with severe dementia, or being a refugee forced out of one’s native country by war. Distant stressors are traumatic experiences that occurred in the distant past yet have the potential to continue modifying immune system function because of their long-lasting cognitive and emotional sequelae (Baum, Cohen, & Hall, 1993). Examples of distant stressors include having been sexually assaulted as a child, having witnessed the death of a fellow soldier during combat, and having been a prisoner of war.
In addition to the presence of difficult circumstances, investigators also use life-event interviews and life-event checklists to capture the total number of different stressors encountered over a specified time frame. Depending on the instrument, the focus of these assessments can be either major life events (e.g., getting divorced, going bankrupt) or minor daily hassles (e.g., getting a speeding ticket, having to clean up a mess in the house). With the more sophisticated instruments, judges then code stressor severity according to how the average person in similar biographical circumstances would respond (e.g., S. Cohen et al., 1998; Evans et al., 1995).
A smaller number of studies enrolled large populations of adults who were not experiencing any specific difficulty and examined whether their immune responses varied according to their reports of perceived stress, intrusive thoughts, or both. Other studies have examined stressed populations, in which a larger range of subjective responses may be detected. This work grows out of the view that people’s biological responses to stressful circumstances are heavily dependent on their appraisals of the situation and cognitive and emotional responses to it (Baum et al., 1993; Frankenhauser, 1975; Tomaka, Blascovich, Kibler, & Ernst, 1997).
Overview of the Immune System
As many behavioral scientists are unfamiliar with the details of the immune system, we provide a brief overview. For a more complete treatment, the reader is directed to the sources for the information presented here (Benjamini, Coico, & Sunshine, 2000; Janeway & Travers, 1997; Rabin, 1999). Critical characteristics of various immune components and assays are also listed in Table 1.
Table 1.
Immune Parameters Reported and Critical Characteristics
| Parameter | Arm of immune system | Function | Cell surface marker |
|---|---|---|---|
| Cell | |||
| Leukocytes | Natural | All white cells | |
| Granulocytes | Natural | Inflammation | |
| Neutrophils | Natural | Inflammation, phagocytosis | |
| Eosinophils | Natural | Inflammation | |
| Monocytes/macrophages | Natural | Inflammation, phagocytosis | |
| Lymphocytes | Specific | All lymphocytes | CD2 |
| T lymphocytes | Specific | Cellular immunity | CD3, CD45RA (naive) |
| T-helper lymphocytes | Specific | Cellular (Th1) or humoral (Th2) immunity | CD4 |
| T-cytotoxic lymphocytes | Specific | Cellular (Th1) immunity | CD8 |
| B lymphocytes | Specific | Humoral (Th2) immunity | CD19, CD20 |
| Activated B lymphocytes | Specific | Humoral (Th2) immunity | CD23, CD30 |
| Natural killer cells | Natural | Cellular (Th1) immunity | CD16, CD56, CD57 |
| Immunoglobulin | |||
| IgA, IgG, IgM | Specific | Humoral (Th2) immunity | |
| Anti-EBV IgG | Specific | Index of EBV replication/activation | |
| Anti-HSV IgG | Specific | Index of HSV replication/activation | |
| Anti-influenza IgG postimmunization | Specific | Humoral (Th2) immunity | |
| Cytokine | |||
| Interleukin-1β | Natural | Inflammation, T cell activation | |
| Interleukin-2 | Specific | T cell activation (Th1) | |
| Interleukin-4 | Specific | B cell activation, antibody production (Th2) | |
| Interleukin-6 | Natural | Inflammation | |
| Interleukin-10 | Specific | Inhibits T cell activation (Th2) | |
| Interferon-γ | Natural and specific | Macrophage, natural killer cell, and T cell activation (Th1) | |
| Tumor necrosis factor-α | Natural | Inflammation | |
| Complement | Natural | Increases effectiveness of natural immunity | C3 |
| Functional assay | |||
| Neutrophil superoxide release | Natural | Inflammation | |
| Natural killer cell cytotoxicity | Natural | Cellular (Th1) immunity | |
| Proliferation to ConA | Specific | Cellular (Th1) immunity (T cell proliferation) | |
| Proliferation to PHA | Specific | Cellular (Th1) immunity (T cell proliferation) | |
| Proliferation to PWM | Specific | Cellular (Th1) and humoral (Th2) immunity (T and B cell proliferation) | |
Note. Th1 = cells that direct a response to intracellular pathogens; Th2 = cells that direct a response to extracellular pathogens; IgA = immunoglobulin A; IgG = immunoglobulin G; IgM = immunoglobulin M; EBV = Epstein-Barr virus; HSV = herpes simplex virus; ConA = concanavalin A; PHA = phytohemagglutinin; PWM = pokeweed mitogen.
Components of the Immune System
There are several useful ways of dividing elements of the immune response. For the purposes of understanding the relationship of psychosocial stressors to the immune system, it is useful to distinguish between natural and specific immunity. Natural immunity is an immune response that is characteristic not only of mammals but also lower order organisms such as sponges. Cells involved in natural immunity do not provide defense against any particular pathogen; rather, they are all-purpose cells that can attack a number of different pathogens1 and do so in a relatively short time frame (minutes to hours) when challenged. The largest group of cells involved in natural immunity is the granulocytes. These cells include the neutrophil and the macrophage, phagocytic cells that, as their name implies, eat their targets. The generalized response mounted by these cells is inflammation, in which neutrophils and macrophages congregate at the site of injury or infection, release toxic substances such as oxygen radicals that damage invaders, and phagocytose both invaders and damaged tissue. Macrophages in particular also release communication molecules, or cytokines, that have broad effects on the organism, including fever and inflammation, and also promote wound healing. These proinflammatory cytokines include interleukin(IL)-1, IL-6, and tumor necrosis factor alpha (TNFα). Other granulocytes include the mast cell and the eosinophil, which are involved in parasitic defense and allergy.
Another cell involved in natural immunity is the natural killer cell. Natural killer cells recognize the lack of a self-tissue molecule on the surface of cells (characteristic of many kinds of virally infected and some cancerous cells) and lyse those cells by releasing toxic substances on them. Natural killer cells are thought to be important in limiting the early phases of viral infections, before specific immunity becomes effective, and in attacking self-cells that have become malignant.
Finally, complement is a family of proteins involved in natural immunity. Complement protein bound to microorganisms can up-regulate phagocytosis and inflammation. Complement can also aid in antibody-mediated immunity (discussed below as part of the specific immune response).
Specific immunity is characterized by greater specificity and less speed than the natural immune response. Lymphocytes have receptor sites on their cell surfaces. The receptor on each cell fits with one and only one small molecular shape, or antigen, on a given invader and therefore responds to one and only one kind of invader. When activated, these antigen-specific cells divide to create a population of cells with the same antigen specificity in a process called clonal proliferation, or the proliferative response. Although this process is efficient in terms of the number of cells that have to be supported on a day-to-day basis, it creates a delay of up to several days before a full defense is mounted, and the body must rely on natural immunity to contain the infection during this time.
There are three types of lymphocytes that mediate specific immunity: T-helper cells, T-cytotoxic cells, and B cells. The main function of T-helper cells is to produce cytokines that direct and amplify the rest of the immune response. T-cytotoxic cells recognize antigen expressed by cells that are infected with viruses or otherwise compromised (e.g., cancer cells) and lyse those cells. B cells produce soluble proteins called antibody that can perform a number of functions, including neutralizing bacterial toxins, binding to free virus to prevent its entry into cells, and opsonization, in which a coating of antibody increases the effectiveness of natural immunity. There are five kinds of antibody: Immunoglobulin (Ig) A is found in secretions, IgE binds to mast cells and is involved in allergy, IgM is a large molecule that clears antigen from the bloodstream, IgG is a smaller antibody that diffuses into tissue and crosses the placenta, and IgD is of unknown significance but may be produced by immature B cells.
An important immunological development is the recognition that specific immunity in humans is composed of cellular and humoral responses. Cellular immune responses are mounted against intracellular pathogens like viruses and are coordinated by a subset of T-helper lymphocytes called Th1 cells. In the Th1 response, the T-helper cell produces cytokines, including IL-2 and interferon gamma (IFNγ). These cytokines selectively activate T-cytotoxic cells as well as natural killer cells. Humoral immune responses are mounted against extracellular pathogens such as parasites and bacteria; they are coordinated by a subset of T-helper lymphocytes called Th2 cells. In the Th2 response, the T-helper cell produces different cytokines, including IL-4 and IL-10, which selectively activate B cells and mast cells to combat extracellular pathogens.
Immune Assays
Immune assays can quantify cells, proteins, or functions. The most basic parameter is a simple count of the number of cells of different subtypes (e.g., neutrophils, macrophages), typically from peripheral blood. It is important to have an adequate number of different types of immune cells in the correct proportions. However, the normal range for these enumerative parameters is quite large, so that “correct” numbers and proportions can cover a wide range, and small changes are unlikely to have any clinical significance in healthy humans.
Protein production—either of antibody or cytokines—can be measured in vitro by stimulating cells and measuring protein in the supernatant or in vivo by measuring protein in peripheral blood. For both antibody and cytokine, higher protein production may represent a more robust immune response that can confer protection against disease. Two exceptions are levels of proinflammatory cytokines (IL-1, IL-6, and TNFα) and antibody against latent virus. Proinflammatory cytokines are increased with systemic inflammation, a risk factor for poorer health resulting from cardiac disease, diabetes mellitus, or osteoporosis (Ershler & Keller, 2000; Luster, 1998; Papanicoloaou, Wilder, Manolagas, & Chrousos, 1998). Antibody production against latent virus occurs when viral replication triggers the immune system to produce antibodies in an effort to contain the infection. Most people become infected with latent viruses such as Epstein-Barr virus during adolescence and remain asymptomatically infected for the rest of their lives. Various processes can activate these latent viruses, however, so that they begin actively replicating. These processes may include a breakdown in cellular immune response (Jenkins & Baum, 1995). Higher antibody against latent viruses, therefore, may indicate poorer immune control over the virus.
Functional assays, which are performed in vitro, measure the ability of cells to perform specific activities. In each case, higher values may represent more effective immune function. Neutro-phils’ function can be quantified by their ability to migrate in a laboratory assay and their ability to release oxygen radicals. The natural killer cytotoxicity assay measures the ability of natural killer cells to lyse a sensitive target cell line. Lymphocyte proliferation can be stimulated with mitogens that bypass antigen specificity to activate cells or by stimulating the T cell receptor.
Pathways Between Stress and the Immune System
How could stress “get inside the body” to affect the immune response? First, sympathetic fibers descend from the brain into both primary (bone marrow and thymus) and secondary (spleen and lymph nodes) lymphoid tissues (Felten & Felten, 1994). These fibers can release a wide variety of substances that influence immune responses by binding to receptors on white blood cells (Ader, Cohen, & Felten, 1995; Felten & Felten, 1994; Kemeny, Solomon, Morley, & Herbert, 1992; Rabin, 1999). Though all lymphocytes have adrenergic receptors, differential density and sensitivity of adrenergic receptors on lymphocytes may affect responsiveness to stress among cell subsets. For example, natural killer cells have both high-density and high-affinity β2-adrenergic receptors, B cells have high density but lower affinity, and T cells have the lowest density (Anstead, Hunt, Carlson, & Burki, 1998; Landmann, 1992; Maisel, Fowler, Rearden, Motulsky, & Michel, 1989). Second, the hypothalamic–pituitary–adrenal axis, the sympathetic–adrenal–medullary axis, and the hypothalamic–pituitary–ovarian axis secrete the adrenal hormones epinephrine, norepinephrine, and cortisol; the pituitary hormones prolactin and growth hormone; and the brain peptides melatonin, β-endorphin, and enkephalin. These substances bind to specific receptors on white blood cells and have diverse regulatory effects on their distribution and function (Ader, Felten, & Cohen, 2001). Third, people’s efforts to manage the demands of stressful experience sometimes lead them to engage in behaviors—such as alcohol use or changes in sleeping patterns—that also could modify immune system processes (Kiecolt-Glaser & Glaser, 1988). Thus, behavior represents a potentially important pathway linking stress with the immune system.
Maier and Watkins (1998) proposed an even closer relationship between stress and immune function: that the immunological changes associated with stress were adapted from the immunological changes in response to infection. Immunological activation in mammals results in a syndrome called sickness behavior, which consists of behavioral changes such as reduction in activity, social interaction, and sexual activity, as well as increased responsiveness to pain, anorexia, and depressed mood. This syndrome is probably adaptive in that it results in energy conservation at a time when such energy is best directed toward fighting infection. Maier and Watkins drew parallels between the behavioral, neuroendo-crine, and thermoregulatory responses to sickness and stress. The common thread between the two is the energy mobilization and redirection that is necessary to fight attackers both within and without.
Models of Stress, the Immune System, and Health
Conceptualizations of the nature of the relationship between stress and the immune system have changed over time. Selye’s (1975) finding of thymic involution led to an initial model in which stress is broadly immunosuppressive. Early human studies supported this model, reporting that chronic forms of stress were accompanied by reduced natural killer cell cytotoxicity, suppressed lymphocyte proliferative responses, and blunted humoral responses to immunization (see S. Cohen, Miller, & Rabin, 2001; Herbert & Cohen, 1993;Kiecolt-Glaser, Glaser, Gravenstein, Malarkey, & Sheridan, 1996, for reviews). Diminished immune responses of this nature were assumed to be responsible for the heightened incidence of infectious and neoplastic diseases found among chronically stressed individuals (Andersen, Kiecolt-Glaser, & Glaser, 1994; S. Cohen & Williamson, 1991).
Although the global immunosuppression model enjoyed long popularity and continues to be influential, the broad decreases in immune function it predicts would not have been evolutionarily adaptive in life-threatening circumstances. Dhabhar and McEwen (1997, 2001) proposed that acute fight-or-flight stressors should instead cause redistribution of immune cells into the compartments in which they can act the most quickly and efficiently against invaders. In a series of experiments with mice, they found that during acute stress, T cells selectively redistributed into the skin, where they contributed to enhancement of the immune response. In contrast, during chronic stress, T cells were shunted away from the skin, and the immune response to skin test challenge was diminished (Dhabhar & McEwen, 1997). On the basis of these findings they proposed a biphasic model in which acute stress enhances, and chronic stress suppresses, the immune response.
A modification of this model posits that short-term changes in all components of the immune system (natural and specific) are unlikely to occur because they would expend too much energy to be adaptive in life-threatening circumstances. Instead, stress should shift the balance of the immune response toward activating natural processes and diminishing specific processes. The premise underlying this model is that natural immune responses are better suited to managing the potential complications of life-threatening situations than specific immune responses because they can unfold much more rapidly, are subject to fewer inhibitory constraints, and require less energy to be diverted from other bodily systems that support the fight-or-flight response (Dopp, Miller, Myers, & Fahey, 2000; Sapolsky, 1998).
Even with this modification of the biphasic model, neither it nor the global immunosuppression model sufficiently explains findings that link chronic stress with both disease outcomes associated with inadequate immunity (infectious and neoplastic disease) and disease outcomes associated with excessive immune activity (allergic and autoimmune disease). To resolve this paradox, some researchers have chosen to focus on how chronic stress might shift the balance of the immune response. The most well-known of these models hypothesizes that chronic stress elicits simultaneous enhancement and suppression of the immune response by altering patterns of cytokine secretion (Marshall et al., 1998). Th1 cytokines, which activate cellular immunity to provide defense against many kinds of infection and some kinds of neoplastic disease, are suppressed. This suppression has permissive effects on production of Th2 cytokines, which activate humoral immunity and exacerbate allergy and many kinds of autoimmune disease. This shift can occur via the effects of stress hormones such as cortisol (Chiappelli, Manfrini, Franceschi, Cossarizza, & Black, 1994). Th1-to-Th2 shift changes the balance of the immune response without necessarily changing the overall level of activation or function within the system. Because a diminished Th1-mediated cellular immune response could increase vulnerability to infectious and neoplastic disease, and an enhanced Th-2 mediated humoral immune response could increase vulnerability to autoimmune and allergic diseases, this cytokine shift model also is able to reconcile patterns of stress-related immune change with patterns of stress-related disease outcomes (Marshall et al., 1998).
Who Is Vulnerable to Stress-Induced Immune Changes?
If the stress response in the immune system evolved, a healthy organism should not be adversely affected by activation of this response because such an effect would likely have been selected against. Although there is direct evidence that stress-related immunosuppression can increase vulnerability to disease in animals (e.g., Ben Eliyahu, Shakhar, Page, Stefanski, & Shakhar, 2000; Quan et al., 2001; Shavit et al., 1985; Sheridan et al., 1998), there is little or no evidence linking stress-related immune change in healthy humans to disease vulnerability. Even large stress-induced immune changes can have small clinical consequences because of the redundancy of the immune system’s components or because they do not persist for a sufficient duration to enhance disease susceptibility. In short, the immune system is remarkably flexible and capable of substantial change without compromising an otherwise healthy host.
However, the flexibility of the immune system can be compromised by age and disease. As humans age, the immune system becomes senescent (Boucher et al., 1998; Wikby, Johansson, Ferguson, & Olsson, 1994). As a consequence, older adults are less able to respond to vaccines and mount cellular immune responses, which in turn may contribute to early mortality (Ferguson, Wikby, Maxson, Olsson, & Johansson, 1995; Wayne, Rhyne, Garry, & Goodwin, 1990). The decreased ability of the immune system to respond to stimulation is one indicator of its loss of flexibility.
Loss of self-regulation is also characteristic of disease states. In autoimmune disease, for example, the immune system treats self-tissue as an invader, attacking it and causing pathology such as multiple sclerosis, rheumatoid arthritis, Crohn’s disease, and lupus. Immune reactions can also be exaggerated and pathological, as in asthma, and suggest loss of self-regulation. Finally, infection with HIV progressively incapacitates T-helper cells, leading to loss of the regulation usually provided by these cells. Although each of these diseases has distinct clinical consequences, the change in the immune system from flexible and balanced to inflexible and unbalanced suggests increased vulnerability to stress-related immune dysregulation; furthermore, dysregulation in the presence of disease may have clinical consequences (e.g., Bower, Kemeny, Taylor, & Fahey, 1998).
The Present Analysis
We performed a meta-analysis of published results linking stress and the immune system. We feel that this area is in particular need of a quantitative review because of the methodological nature of most studies in this area. For practical and economic reasons, many psychoneuroimmunology studies have a relatively small sample size, creating the possibility of Type II error. Furthermore, many studies examine a broad range of immunological parameters, creating the possibility of Type I error. A quantitative review, of which meta-analysis is the best example, can better distinguish reliable effects from those arising from both Type I and Type II error than can a qualitative review.
We combined studies in such a way as to test the models of stress and immune change reviewed above. First, we examined each stressor type separately, yielding separate effects for stressors of different duration and trajectory. Second, we examined both healthy and medical populations, allowing comparison of the effects of stress on resilient and vulnerable populations; along the same lines, we also examined the effects of age. Finally, we examined all immune parameters separately so that patterns of response (e.g., global immunosuppression vs. cytokine shift) would be clearer.
Method
Article Identification
Articles for the meta-analysis were identified through computerized literature searches and searches of reference lists. MEDLINE and PsycINFO were searched for the years 1960 –2001. Following the example of Herbert and Cohen (1993), we used the terms stress, hassles, and life events in combination with the term immune to search both databases. The reference lists of 11 review articles on stress and the immune system (Benschop, Geenen, et al., 1998; Biondi, 2001; Cacioppo, 1994; S. Cohen & Herbert, 1996; S. Cohen et al., 2001; Herbert & Cohen, 1993; Kiecolt-Glaser, Cacioppo, Malarkey, & Glaser, 1992; Kiecolt-Glaser, McGuire, Robles, & Glaser, 2002; Maier, Watkins, & Fleshner, 1994; O’Leary, 1990; Zorrilla et al., 2001) were then searched to identify additional articles.
We selected only articles that met a number of inclusion criteria. The first criterion was that the work had to include a measure of stress. This criterion could be met if a sample experiencing a stressor was compared with an unstressed control group, if a sample experiencing a stressor was compared with itself at a baseline that could reasonably be considered low stress, or if differing degrees of stress in a sample were assessed with an explicit measure of stress. This criterion was not met if, for example, anxiety—an affective state—was used as a proxy for stress, or it seemed likely that a “baseline” assessment occurred during periods of significant stress. The second criterion was that the stressor had to be psychosocial. Stressors that included a significant physical element such as pain, cold, or physical exhaustion were eliminated (e.g., Antarctic isolation, space flight, military training). The third criterion was that the work had to include a measure of the immune system. This criterion was met by any enumerative or functional in vitro or in vivo immune assay. However, clinical disease outcomes such as HIV progression or rhinovirus infection did not meet this criterion. Finally, we eliminated articles from which a meaningful effect size could not be abstracted. For example, when between- and within-subjects observations were treated as independent, the reported effect was likely to be inflated. In a few cases, effects of stress and clinical status were confounded—that is, a stressed clinical group was compared with an unstressed healthy group—and hence these studies were excluded from the meta-analysis.
Stressor Classification
We coded stressors in the articles into five classes: acute time-limited, brief naturalistic, event sequence, chronic, and distant. The most difficult distinctions among event sequence, chronic, and distant stressors were based on temporal and qualitative considerations. Event sequences included discrete stressors occurring 1 year or less before immune assessment and could be of any severity. These were most often normative stressors such as bereavement. Chronic stressors were ongoing stressors such as caregiving and disability. Distant stressors were severe, traumatic events that could meet the stressor criterion for posttraumatic stress disorder (American Psychiatric Association, 1994), such as combat exposure or abuse, and had happened more than 1 year before immune assessment. Most stressors in this category occurred 5 to 10 years before immune assessment. Disagreements in stressor classification were resolved by consensus. Subgroups for moderator analyses were similarly decided.
The Meta-Analysis
Overview of procedures
Meta-analysis is a tool for synthesizing research findings. It proceeds in two phases. In the first, effect sizes are computed for each study. An effect size represents the magnitude of the relationship between two variables, independent of sample size. In this context it can be viewed as a measure of how much two groups, one experiencing a stressor and the other not, differ on a specific immune outcome. In the second phase, effect sizes from individual studies are combined to arrive at an aggregate effect size for each immune outcome of interest.
We used Pearson’s r as the effect size metric in this meta-analysis. Effect sizes for individual studies were computed using descriptive statistics presented in the original published reports. When these statistics were not available, we requested them from authors. This strategy was successful in most circumstances. To compute Pearson’s r from descriptive statistics in between-subjects designs, we subtracted the control group mean from the stressed group mean and divided this value by the pooled sample standard deviation. The value that emerged from this computation, known as Cohen’s d, was then converted into a Pearson’s r by taking the square root of the quantity d2/(d2 + 4). (See Rosenthal, 1994.) To compute Pearson’s r from descriptive statistics in within-subjects designs, we subtracted the group mean at baseline from the group mean during stress and divided this quantity by the sample standard deviation at baseline. This d value was converted into a Pearson’s r by taking the square root of the quantity d2/(d2 + 4). In cases in which descriptive statistics were not available, Pearson’s r was computed from inferential statistics using standard formulae (Rosenthal, 1994). These formulae had to be modified slightly for studies that used within-subjects designs because effect sizes are systematically overestimated when they are calculated from repeated measures test statistics (Dunlap, Cortina, Vaslow, & Burke, 1996). In these situations we derived effect size estimates using the formula d = tc[2 (1 − r)]1/2, where tc corresponds to the value of the t statistic for correlated measures, and r corresponds to the value of the correlation between outcome measures at pretest and posttest (Dunlap et al., 1996). Because very few studies reported the value of r, we used a value of .60 to compute effect sizes in this meta-analysis. This represents the average correlation between pre-stress and poststress measures of immune function in a series of studies performed in our laboratories. To ensure that the meta-analytic findings were robust to variations in r, we conducted follow-up analyses using r values ranging from .45 to .75. Very similar findings emerged from these analyses, suggesting that the values we present below are reliable estimates of effect size. If anything, they are probably conservative estimates, because the pre–post correlation between immune measures often is substantially lower than .60.
The effect size estimates from individual studies were subsequently aggregated using random-effects models with the software program Comprehensive Meta-Analysis (Borenstein & Rothstein, 1999). The random-effects model views each study in a meta-analysis as a random observation drawn from a universe of potential investigations. As such, it assumes that the magnitude of the relationship between stress and the immune system differs across studies as a result of random variance associated with sampling error and differences across individuals in the processes of interest. Because of these assumptions, random-effects models not only permit one to draw inferences about studies that have been done but also to generalize to studies that might be done in the future (Raudenbush, 1994; Shadish & Haddock, 1994). It also bears noting that in the population of studies on stress and immunity there is likely to be a fair amount of nonrandom variance, as researchers who examine ostensibly similar phenomena may still differ in terms of the samples they recruit, the operational definition of stress they use, and the laboratory methods they utilize to assess a specific immune process.
Separate random-effects models were computed for each immune outcome included in the meta-analysis. Prior to computing the random-effects model, r values derived from each study were z-transformed by the software program, as recommended by Shadish and Haddock (1994), to stabilize variance. The z values were later back-transformed into r values to facilitate interpretation of the meta-analytic findings. In the end, each random-effects model yielded an aggregate weighted effect size r, which can be interpreted the same way as a correlation coefficient, ranging in value from −1.00 to 1.00. Each r statistic was weighted before aggregation by multiplying its value by the inverse of its variance; this procedure enabled larger studies to contribute to effect size estimates to a greater extent than smaller ones. Weighting effect sizes is important because larger studies provide more accurate estimates of true population parameters (Shadish & Haddock, 1994). After each aggregate effect size had been derived, we computed 95% confidence intervals around it, assessed whether it was statistically significant, and computed a heterogeneity coefficient to determine whether the studies contributing to it had yielded consistent findings. Following convention, aggregate effect sizes were considered statistically different from zero when (a) their corresponding z value was greater than 1.96 and (b) the 95% confidence intervals around them did not include the value zero (Rosenthal, 1991; Shadish & Haddock, 1994).
To determine whether the studies contributing to each aggregate effect size shared a common population value, we computed the heterogeneity statistic Q (Shadish & Haddock, 1994). This statistic is chi-square distributed with k – 1 degrees of freedom, where k represents the number of independent effect sizes included. When a statistically significant heterogeneity test emerged, we searched for moderators (characteristics of the participants, stressful experience, or measurement strategy) that could explain the variability across studies. The first step in this process involved estimating correlations between participant characteristics (e.g., mean age, percentage female) and immune effects to examine whether the strength of effects varied according to demographics. When it was possible to do so, we then stratified the studies according to characteristics of the stressful experience (e.g., duration, quality) or the measurement strategy (e.g., interview, checklist), and computed separate random-effects analyses for each subgroup.
Handling missing data
Occasionally authors of studies failed to report the descriptive or inferential statistics needed to compute an effect size. In some of these cases, the authors noted that there was a significant difference between a stressed and control group. When this occurred, we computed effect sizes assuming that p values were equivalent to .05. This represents a conservative approach because the actual p values were probably smaller. In other cases, the authors noted that a stressed and control group did not differ with respect to an immune outcome, but failed to provide any further statistical information. When this occurred, we computed effect sizes assuming that there was no difference at all between the groups (r = .00). Because there is seldom no difference at all between two groups, this also represents a conservative strategy. Imputation was used in less than 7% of cases.
Handling dependent data
The validity of a meta-analysis rests on the assumption that each value contributing an aggregate effect size is statistically independent of the others (Rosenthal, 1991). We devised a number of strategies to avoid violating this independence assumption. First, in studies that assessed stimulated-lymphocyte proliferation at multiple mitogen dosages, we computed the average effect size across mitogen dosages, and we used this value to derive aggregate indices. We used an analogous strategy for studies that assessed natural killer cell cytotoxicity at multiple effector:target cell ratios. Second, in studies that utilized designs in which multiple laboratory stressors were compared with a control condition, the average effect size across stressor conditions was computed and later used to derive aggregate indices. Because this averaging procedure in most cases yielded an effect size that was smaller than that of the most potent stressor, we also computed meta-analyses using the larger of the effect sizes from each study rather than the average. Doing so did not alter any of the substantive findings we report. Third, in studies in which immune outcomes were assessed on multiple occasions during a stressful experience, the average effect size across occasions was used to derive aggregate indices. Note that we did not conduct meta-analyses of recovery effects, that is, immune values after a stressor had ended. Although such an analysis would answer interesting questions about the stress-recovery process, there were not enough studies that included similar immune outcomes assessed at similar time points after stress to permit a complete analysis. Fourth, because some data were published in more than one outlet, we contacted authors of multiple publications to determine sample independence or dependence.
Results
Preliminary Findings
The meta-analysis is based on effect sizes derived from 293 independent studies. These studies were reported in 319 separate articles in peer-reviewed scientific journals (see Table 2). A total of 18,941 individuals participated in these studies. Their mean age was 34.8 years (SD = 15.9). Although the studies collectively included a broad range of age groups (range = 5–78 years), most focused heavily on younger adults. More than half of the studies (51.3%) had a mean age under 30.0 years, and more than four fifths (84.8%) had a mean age under 55.0 years. Slightly more than two thirds of the studies (68.5%) included women; in the average study almost half (42.8%) of the participants were female. The vast majority of studies (84.8%) focused on medically healthy adults.2 Of those that included medical populations, most focused on HIV/AIDS (k = 18; 38.3%), arthritis (k = 6; 12.8%), cancer (k = 5; 10.6%), or asthma (k = 4; 8.5%).
Table 2.
Studies Used in the Meta-Analysis by Type of Stressor
With respect to the kinds of stressors examined by studies in the meta-analysis, the most commonly utilized models were acute laboratory challenges (k = 85; 29.0%) and brief naturalistic stressors (k = 63; 21.5%). Stressful event sequences (k = 30; 10.2%), chronic stressors (k = 23; 7.8%), and distant traumatic experiences (k = 9; 3.1%) were explored less frequently. More than a quarter of the studies in the meta-analysis modeled the stress process by administering nonspecific life-event checklists (k = 53; 18.1%) and/or global perceived stress measures (k = 21; 7.1%) to participants. A small minority of studies examined whether reports of perceived stress or intrusive memories were associated with the extent of immune dysregulation within populations who had suffered a specific traumatic experience (k = 9; 3.1%).
The studies in the meta-analysis examined 292 distinct immune system outcomes. A minority of these outcomes were assessed in three or more studies (k = 87; 30.0%), and as such, they are the focus of the meta-analyses we present in the rest of this article (see Table 1). The most commonly assessed enumerative outcomes were counts of T-helper lymphocytes (k = 90; 30.7%), T-cytotoxic lymphocytes (k = 81; 27.6%), natural killer cells (k = 67; 22.9%), and total lymphocytes (k = 52; 17.7%). The most commonly assessed functional outcomes were natural killer cell cytotoxicity (k = 94; 32.1%) and lymphocyte proliferation stimulated by the mitogens phytohemagglutinin (PHA; k = 65; 22.2%), concanavalin A (ConA; k = 39; 13.3%), and pokeweed mitogen (PWM; k = 26; 8.9%).
Interpreting the Meta-Analytic Findings
Table 1 lists the immune parameters analyzed with the arm of the immune system to which they belong (natural or specific) and, briefly, their function. Where relevant, cell surface markers used to identify classes of immunocytes in flow cytometry are given. For example, the cell surface marker CD19 is used to identify B lymphocytes. Recall that different models of stress and the immune system posit differential effects of stress on subsets of the immune system—for example, natural versus specific immunity or cellular (Th1) versus humoral (Th2) immunity. Table 1 acts as a guide for interpreting the pattern of results in light of these models.
In the following sections we describe the meta-analytic results for each stressor category. A useful rule of thumb for judging effect sizes is to consider values of .10, .30, and .50 as corresponding to small, medium, and large effects, respectively (J. Cohen & Cohen, 1983); more generally, the aggregate effect size r can be interpreted in the same fashion as a correlation, with values ranging from −1.00 to 1.00. Positive values indicate that the presence of a stressor increases a particular immune parameter relative to some baseline (or control) condition. We should caution the reader that in some analyses, our statistics are derived from as few as three independent studies. Although meta-analyses of small numbers of studies do not pose any major statistical problems, it is important to remember that they have limited power to detect statistically significant effect sizes. What a meta-analysis can accurately provide in these instances, however, is an estimate of how much and what direction a given stressor’s presence influences a specific immune outcome (i.e., an effect size estimate).
Meta-Analytic Results for the Effects of Stressors
Acute time-limited stressors
Acute time-limited stressors included primarily experimental manipulations of stressful experiences, such as public speaking and mental arithmetic, that lasted between 5 and 100 min. Reliable effects on the immune system included increases in immune parameters, especially natural immunity. The most robust effect of this kind of experience was a marked increase in the number of natural killer cells (r =.43) and large granular lymphocytes (r =.53) in peripheral blood (see Table 3). This effect is consistent with the view that acute stressors cause immune cells to redistribute into the compartments in which they will be most effective (Dhabhar & McEwen, 1997). However, other types of lymphocytes did not show robust redistribution effects: B cells and T-helper cells showed very little change (rs = −.07 and .01, respectively), and this change was not statistically significant across studies. T-cytotoxic lymphocytes did tend to increase reliably in peripheral blood, though to a lesser degree than their natural immunity counterparts (r =.20); this increase drove a reliable decline in the T-helper:T-cytotoxic ratio (r = −.23). However, natural killer cells as well as T-cytotoxic cells can express CD8, the marker most often used to define the latter population. Because some studies did not use the T cell receptor (CD3) to differentiate between CD3–CD8+ natural killer cells and CD3+CD8+ T-cytotoxic cells, it is possible that the effect for “T-cytotoxic cells” is actually being driven by natural killer cells (Benschop, Rodriguez-Feuerhahn, & Schedlowski, 1996).
Table 3.
Meta-Analysis of Immune Responses to Acute Time-Limited Stress in Healthy Participants
| Immune marker | k | N | r | SEr | 95% CI | p | Q |
|---|---|---|---|---|---|---|---|
| Leukocyte subset count | |||||||
| Leukocytes | 25 | 1,129 | .17 | .04 | .10, .25 | .001 | 34.61 |
| Granulocytes | 12 | 397 | .08 | .06 | minus;.04, .19 | .18 | 31.77 |
| Neutrophils | 3 | 86 | .30 | .12 | .08, .50 | .009 | 2.13 |
| Eosinophils | 3 | 81 | −.10 | .16 | −.39, .21 | .53 | 2.99 |
| Monocytes | 15 | 590 | .04 | .05 | −.05, .13 | .43 | 15.43 |
| Lymphocytes | 24 | 828 | .18 | .05 | .09, .26 | .001 | 31.77 |
| T lymphocytes | 33 | 1,452 | .07 | .03 | .01, .12 | .01 | 25.48 |
| T-helper lymphocytes | 42 | 1,678 | .01 | .03 | −.05, .05 | .86 | 23.72 |
| T-cytotoxic lymphocytes | 42 | 1,678 | .20 | .03 | .15, .25 | .001 | 34.05 |
| T-helper:T-cytotoxic ratio | 19 | 920 | −.23 | .10 | −.40, −.04 | .02 | 17.98 |
| Naive T lymphocytes | 3 | 241 | −.09 | .11 | −.29, .12 | .41 | 2.46 |
| B lymphocytes | 18 | 739 | −.07 | .04 | −.14, .01 | .08 | 16.23 |
| Activated B lymphocytes | 4 | 60 | −.15 | .14 | −.40, .14 | .31 | 0.48 |
| Natural killer cells | 41 | 1,635 | .43 | .06 | .33, .51 | .001 | 172.75*** |
| Large granular lymphocytes | 8 | 362 | .53 | .30 | .00, .83 | .05 | 165.64*** |
| Leukocyte subset percentage | |||||||
| Granulocytes | 5 | 295 | −.13 | .10 | −.31, .07 | .20 | 7.24 |
| Neutrophils | 5 | 217 | .04 | .07 | −.10, .18 | .56 | 3.75 |
| Monocytes | 7 | 277 | .06 | .09 | −.12, .23 | .55 | 10.82 |
| Lymphocytes | 7 | 350 | .06 | .06 | −.05, .16 | .30 | 1.34 |
| T lymphocytes | 10 | 497 | −.05 | .09 | −.22, .13 | .62 | 28.05*** |
| T-helper lymphocytes | 14 | 642 | −.24 | .04 | −.31, −.16 | .001 | 13.61 |
| T-cytotoxic lymphocytes | 15 | 692 | .09 | .04 | .01, .16 | .03 | 9.28 |
| B lymphocytes | 5 | 248 | −.11 | .07 | −.24, .02 | .09 | 1.46 |
| Natural killer cells | 15 | 693 | .24 | .11 | .03, .42 | .02 | 90.19*** |
| Total immunoglobulins | |||||||
| Serum IgA | 4 | 91 | .12 | .11 | −.10, .33 | .30 | 0.95 |
| Serum IgM | 3 | 67 | .14 | .13 | −.12, .37 | .30 | 0.61 |
| Secretory IgA secretion rate | 6 | 293 | .22 | .08 | .06, .37 | .008 | 6.92 |
| Secretory IgA concentration | 8 | 337 | .22 | .09 | .05, .38 | .01 | 13.05 |
| Basal cytokine levels | |||||||
| Interleukin-1β | 4 | 89 | −.01 | .11 | −.23, .21 | .91 | 0.25 |
| Natural killer cell function | |||||||
| Natural killer cell cytotoxicity | 37 | 1,398 | .30 | .05 | .20, .39 | .001 | 108.85*** |
| Per-cell cytotoxicity | 8 | 287 | .12 | .11 | −.09, .32 | .26 | 18.12* |
| Lymphocyte proliferation | |||||||
| Proliferation to ConA | 17 | 706 | −.17 | .04 | −.24, −.09 | .001 | 14.12 |
| Proliferation to PHA | 26 | 1,120 | −.17 | .04 | −.23, −.10 | .001 | 35.36 |
| Proliferation to PWM | 10 | 480 | −.10 | −.05 | −.19, −.01 | .03 | 5.84 |
| Cytokine production | |||||||
| Interleukin-1β | 3 | 78 | .01 | .12 | −.23, .23 | .98 | 5.78 |
| Interleukin-4 | 3 | 136 | −.19 | .11 | −.39, .03 | .08 | 2.38 |
| Interleukin-6 | 3 | 143 | .28 | .09 | .13, .44 | .001 | 12.84** |
| Interferon-γ | 3 | 96 | .21 | .11 | .01, .40 | .05 | 0.24 |
Note. CI = confidence interval; IgA = immunoglobulin A; IgM = immunoglobulin M; ConA = concanavalin A; PHA = phytohemagglutinin; PWM = pokeweed mitogen.
p < .05.
p < .01.
p < .001.
The results for cell percentages roughly parallel those for number. However, the percentage data are harder to interpret because any given parameter is linearly dependent on the other parameters: For example, the enumerative data suggest that the decrease in percentage T-helper cells (r = −.24) is probably an artifact of the increases in percentage natural killer cells (r = .24) and percentage T-cytotoxic cells (r = .09).
Another effect that may be considered a redistribution effect is the significant increase in secretory IgA in saliva (r = .22). The time frame of these acute stressors is too short for the synthesis of a significant amount of new antibody; therefore, this increase is probably due to release of already-synthesized antibody from plasma cells and increased translocation of antibody across the epithelium and into saliva (Bosch, Ring, de Geus, Veerman, & Amerongen, 2002). This effect therefore represents relocation, albeit of an immune protein rather than an immune cell.
There were also a number of functional effects. First, natural killer cell cytotoxicity significantly increased with acute stressors (r = .30), but only when the concomitant increase in proportion of natural killer cells in the effector mix was not removed statistically. When examined on a per-cell basis, cytotoxicity did not significantly increase (r = .12). One could, therefore, consider the increase in cytotoxicity a methodological artifact of the definition of effector in effector:target ratios. However, to the degree that one is interested in the general cytotoxic potential of the contents of peripheral blood rather than that of a specific natural killer cell, the uncorrected value is more illustrative. Second, mitogen-stimulated proliferative responses decreased significantly. Again, this could be a methodological artifact of the mix of cells in the assay. However, the proportion of total T and B cells, which are responsible for the proliferative response to PWM and ConA, did not decrease as reliably or as much as did the proliferative response (rs = −.05 to −.11 vs. −.10 to −.17), suggesting that acute stressors do decrease this function of specific immunity. Finally, the production of two cytokines, IL-6 and IFNγ, was increased significantly following acute stress (rs = .28 and .21, respectively).
The data for acute stressors, therefore, support an upregulation of natural immunity, as reflected by increased number of natural killer cells in peripheral blood, and potential downregulation of specific immunity, as reflected by decreased proliferative responses. Other indicators of upregulated natural immunity include increased neutrophil numbers in peripheral blood (r = .30), increased production of a proinflammatory cytokine (IL-6), and increased production of a cytokine that potently stimulates macrophages and natural killer cells as well as T cells (IFNγ). The only exception to this pattern was the increased secretion of IgA antibody, which is a product of the specific immune response. An interesting question for future research is whether this effect is part of a larger nonspecific protein release in the oral cavity in response to acute stress (cf. Bosch et al., 2002).
It bears noting that a number of the findings presented in Table 3 are accompanied by significant heterogeneity statistics. To identify moderating variables that might explain some of this heterogeneity, we examined whether effect sizes varied according to demographic characteristics of the sample (mean age and percentage female) or features of the acute challenge (its duration and nature). Neither of the demographic characteristics showed a consistent relationship with immune outcomes. Although these findings suggest that acute time-limited stressors elicit a similar pattern of immune response for men and women across the life span, this conclusion needs to be viewed somewhat cautiously given the narrow range of ages found in these studies. We also did not find a consistent pattern of relationships between features of the acute challenge and immune outcomes. Acute stressors elicited similar patterns of immune change across a wide spectrum of durations ranging from 5 though 100 min and irrespective of whether they involved social (e.g., public speaking), cognitive (e.g., mental arithmetic), or experiential (e.g., parachute jumping) forms of stressful experience.
Brief naturalistic stressors
Table 4 presents the meta-analysis of brief naturalistic stressors for medically healthy adults. The vast majority of these stressors (k = 60; 95.2%) involved students facing academic examinations. In contrast to the acute time-limited stressors, examination stress did not markedly affect the number or percentage of cells in peripheral blood. Instead, the largest effects were on functional parameters, particularly changes in cytokine production that indicate a shift away from cellular immunity (Th1) and toward humoral immunity (Th2). Brief stressors reliably changed the profile of cytokine production via a decrease in a Th1-type cytokine, IFNγ (r = −.30), which stimulates natural and cellular immune functions, and increases in the Th2-type cytokines IL-6 (r = .26), which stimulates natural and humoral immune functions, and IL-10 (r = .41), which inhibits Th1 cytokine production. Note that IFNγ and IL-6 share the property of stimulating natural immunity but differentially stimulate cytotoxic versus inflammatory effector mechanisms. Their dissociation after brief naturalistic stress indicates differential effects between Th1 and Th2 responses rather than natural and specific responses.
Table 4.
Meta-Analysis of Immune Responses to Brief Naturalistic Stress in Healthy Participants
| Immune marker | k | N | r | SEr | 95% CI | p | Q |
|---|---|---|---|---|---|---|---|
| Leukocyte subset count | |||||||
| Leukocytes | 9 | 249 | .20 | .07 | .07, .32 | .002 | 12.95 |
| Granulocytes | 3 | 56 | .01 | .15 | −.27, .29 | .93 | 0.01 |
| Neutrophils | 5 | 103 | .11 | .11 | −.07, .34 | .18 | 2.33 |
| Monocytes | 6 | 120 | .06 | .10 | −.13, .25 | .52 | 3.90 |
| Lymphocytes | 9 | 236 | .06 | .08 | −.10, .23 | .46 | 10.46 |
| T lymphocytes | 5 | 110 | .03 | .10 | −.18, .22 | .81 | 0.05 |
| T-helper lymphocytes | 7 | 197 | .06 | .08 | −.09, .21 | .43 | 1.08 |
| T-cytotoxic lymphocytes | 6 | 185 | .05 | .08 | −.10, .20 | .50 | 1.74 |
| T-helper:T-cytotoxic ratio | 12 | 351 | .01 | .07 | −.11, .14 | .84 | 13.68 |
| B lymphocytes | 5 | 126 | .48 | .56 | −.51, .92 | .35 | 99.48*** |
| Natural killer cells | 5 | 103 | −.15 | .11 | −.35, .06 | .16 | 2.06 |
| Leukocyte subset percentage | |||||||
| Monocytes | 4 | 98 | .11 | .11 | −.10, .32 | .30 | 2.33 |
| Lymphocytes | 3 | 97 | −.13 | .11 | −.33, .08 | .23 | 2.05 |
| T lymphocytes | 5 | 160 | −.16 | .18 | −.47, .19 | .36 | 13.67** |
| T-helper lymphocytes | 11 | 350 | −.11 | .10 | −.29, .09 | .28 | 26.56** |
| T-cytotoxic lymphocytes | 12 | 362 | −.03 | .06 | −.14, .08 | .60 | 8.84 |
| B lymphocytes | 3 | 121 | .07 | .53 | −.74, .80 | .89 | 42.48*** |
| Natural killer cells | 5 | 163 | −.02 | .19 | −.38, .35 | .93 | 18.20** |
| Total immunoglobulins | |||||||
| Serum IgA | 6 | 243 | .11 | .07 | −.02, .24 | .10 | 1.28 |
| Serum IgG | 7 | 290 | .06 | .06 | −.06, .17 | .37 | 2.54 |
| Serum IgM | 7 | 290 | .02 | .10 | −.17, .21 | .83 | 13.41* |
| Secretory IgA rate | 4 | 139 | .09 | .33 | −.50, .63 | .78 | 31.31*** |
| Secretory IgA concentration | 9 | 350 | .19 | .18 | −.20, .46 | .40 | 66.97*** |
| Specific immunoglobulin | |||||||
| Epstein-Barr virus | 7 | 359 | .20 | .04 | .10, .30 | .001 | 6.56 |
| Herpes simplex virus | 4 | 225 | .18 | .08 | −.02, .34 | .08 | 4.97 |
| Complement molecule | |||||||
| C3 | 3 | 116 | −.16 | .10 | −.34, .03 | .09 | 1.77 |
| Natural killer cell function | |||||||
| Natural killer cell cytotoxicity | 14 | 468 | −.11 | .05 | −.21, −.01 | .04 | 14.55 |
| Lymphocyte proliferation | |||||||
| Proliferation to ConA | 9 | 220 | −.32 | .15 | −.56, −.03 | .03 | 27.08*** |
| Proliferation to PHA | 14 | 443 | −.19 | .09 | −.35, −.02 | .03 | 33.38*** |
| Proliferation to PWM | 3 | 106 | −.17 | .15 | −.43, .12 | .24 | 4.75 |
| Cytokine production | |||||||
| Interleukin-1β | 6 | 149 | .11 | .08 | −.05, .27 | .17 | 15.07*** |
| Interleukin-2 | 4 | 107 | −.17 | .36 | −.71, .49 | .63 | 27.34*** |
| Interleukin-4 | 3 | 81 | −.10 | .12 | −.32, .13 | .39 | 0.69 |
| Interleukin-6 | 3 | 100 | .26 | .11 | .06, .44 | .01 | 0.79 |
| Interleukin-10 | 3 | 95 | .41 | .11 | .21, .57 | .001 | 1.65 |
| Interferon-γ | 8 | 314 | −.30 | .13 | −.51, .05 | .02 | 28.76*** |
| Tumor necrosis factor-α | 3 | 100 | .18 | .19 | −.19, .51 | .34 | 5.10 |
Note. CI = confidence interval; IgA = immunoglobulin A; IgG = immunoglobulin G; IgM = immunoglobulin M; ConA = concanavalin A; PHA = phytohemagglutinin; PWM = pokeweed mitogen.
p < .05.
p <.01.
p <.001.
The functional assay data are consistent with this suggestion of suppression of cellular immunity via decreased Th1 cytokine production: The T cell proliferative response significantly decreased with brief stressors (r = −.19 to −.32), as did natural killer cell cytotoxicity (r = −.11). Increased antibody production to latent virus, particularly Epstein-Barr virus (r = .20), is also consistent with suppression of cellular immunity, enhancement of humoral immunity, or both.
There was also evidence that age contributed to vulnerability to stress-related immune change during brief naturalistic stressors, even within a limited range of relatively young ages. When we examined whether effect sizes varied according to demographic characteristics of the sample, sex ratio did not show a consistent pattern of relations with immune processes. However, the mean age of the sample was strongly related to study effect size. To the extent that a study enrolled participants of older ages, it was likely to observe more pronounced decreases in natural killer cell cytotoxicity (r = −.58, p = .04; k = 14), T lymphocyte proliferation to the mitogens PHA (r = −.58, p = .04; k = 13) and ConA (r = −.31, p = .38; k = 9), and production of the cytokine IFNγ (r = −.63, p = .09; k = 8) in response to brief naturalistic stress. The strength of these findings is particularly surprising given the narrow range of ages found in studies of brief natural stress; the mean participant age in this literature ranged from 15.7 to 35.0 years.
We also calculated effect sizes for three studies examining the effects of examination stress on individuals with asthma (see Table 5). These three studies, all emanating from a team of investigators at the University of Wisconsin—Madison, found that stress reliably increased superoxide release (r = .20 to .37) and decreased natural killer cell cytotoxicity (r = − .33). Because natural killer cells are stimulated by Th1 cytokines, this change is consistent with a Th1-to-Th2 shift. However, stress also reliably increased T cell proliferation to PHA (r = .32), which is not consistent with such a shift. The generally larger effect sizes are consistent with the idea that individuals with immunologically mediated disease are more susceptible to stress-related immune dysregulation, but the reversed sign for T cell proliferation also indicates that that pattern of dysregulation may also be more disorganized. That is, the organized pattern of suppression of Th1 but not Th2 immune responses in healthy individuals undergoing brief stressors may reflect regulation in the healthy immune system. In contrast, the lack of regulation in a diseased immune system may lead to more chaotic changes during stressors.
Table 5.
Meta-Analysis of Immune Responses to Brief Naturalistic Stress in Participants With Asthma
| Immune marker | k | N | r | SEr | 95% CI | p | Q |
|---|---|---|---|---|---|---|---|
| Neutrophil function | |||||||
| Superoxide release with FMLP | 3 | 216 | .20 | .07 | .06, .32 | .004 | 0.39 |
| Superoxide release with PHA | 3 | 216 | .37 | .07 | .24, .49 | .001 | 0.68 |
| Natural killer cell function | |||||||
| Natural killer cell cytotoxicity | 3 | 216 | −.33 | .07 | −.45, −.21 | .001 | 0.50 |
| Lymphocyte proliferation | |||||||
| Proliferation to PHA | 3 | 216 | .32 | .07 | .19, .43 | .001 | 0.35 |
Note. CI = confidence interval; FMLP = N-formyl-met-leu-phe; PHA = phytohemagglutinin.
Stressful event sequences
The meta-analysis of stressful event sequences is presented in Table 6. With the exception of significant increases in the number of circulating natural killer cells and the number of antibodies to the latent Epstein-Barr virus, the findings indicate that stressful event sequences are not associated with reliable immune changes. For many immune outcomes, however, significant heterogeneity statistics are evident. Studies of healthy adults generally fell into two categories that yielded disparate patterns of immune findings. The largest group of studies focused on the death of a spouse as a stressor and, as such, used samples consisting primarily of older women. Collectively, these studies found that losing a spouse was associated with a reliable decline in natural killer cell cytotoxicity (r = − .23, p = .01; k = 6) but not with alterations in stimulated-lymphocyte proliferation by the mitogens ConA (r = − .04, p = .45; k = 4), PHA (r = −.01, p = .93; k = 7), or PWM (r = −.08, p = .76; k = 3) or with changes in the number of T-helper lymphocytes (r = .07, p = .52; k = 6) or T-cytotoxic lymphocytes (r = −.13, p = .45; k = 5) in peripheral blood. The next largest group of studies in this area examined immune responses to disasters, which may have different neuroendocrine consequences than loss; whereas loss is generally associated with increases in cortisol, trauma may be associated with decreases in cortisol (Yehuda, 2001; Yehuda, McFarlane, & Shalev, 1998). Natural disaster samples tended to focus on middle-aged adults of both sexes who were direct victims of the disaster, rescue workers at the scene, or personnel at nearby medical centers. There were medium-size effects suggesting increases in natural killer cell cytotoxicity (r = .25, p = .53; k = 4) and stimulated-lymphocyte proliferation by the mitogen PHA (r = .26, p = .33; k = 2), as well as decreases in the number of T-helper lymphocytes (r = −.20, p = .43; k = 2) and T-cytotoxic lymphocytes (r = −.23, p = .55; k = 2) in the circulation. However, none of them was statistically significant because of the small number of studies involved, and therefore these effects should be considered suggestive but not reliable.
Table 6.
Meta-Analysis of Immune Responses to Stressful Event Sequences in Healthy Participants
| Immune marker | k | N | r | SEr | 95% CI | p | Q |
|---|---|---|---|---|---|---|---|
| Leukocyte subset count | |||||||
| Monocytes | 3 | 113 | −.02 | .10 | −.21, .17 | .87 | 0.39 |
| Lymphocytes | 5 | 223 | .05 | .07 | −.09, .18 | .49 | 2.65 |
| T lymphocytes | 5 | 213 | −.02 | .07 | −.16, .12 | .82 | 0.37 |
| T-helper lymphocytes | 9 | 566 | .03 | .11 | −.19, .25 | .81 | 39.29*** |
| T-cytotoxic lymphocytes | 8 | 544 | −.14 | .15 | −.41, .15 | .35 | 58.22*** |
| T-helper:T-cytotoxic ratio | 6 | 296 | .06 | .08 | −.09, .21 | .44 | 7.54 |
| B lymphocytes | 5 | 185 | .02 | .08 | −.13, .17 | .76 | 0.35 |
| Natural killer cells | 4 | 370 | .17 | .09 | .00, .34 | .05 | 5.06 |
| Leukocyte subset percentage | |||||||
| T lymphocytes | 3 | 129 | .02 | .09 | −.16, .19 | .85 | 0.11 |
| T-helper lymphocytes | 5 | 279 | .00 | .06 | −.12, .12 | .94 | 0.00 |
| T-cytotoxic lymphocytes | 5 | 279 | −.05 | .06 | −.17, .07 | .43 | 3.65 |
| B lymphocytes | 3 | 129 | −.04 | .09 | −.22, .14 | .67 | 0.57 |
| Specific immunoglobulin | |||||||
| Epstein-Barr virus | 3 | 198 | .21 | .07 | .07, .34 | .003 | 1.18 |
| Natural killer cell function | |||||||
| Natural killer cell cytotoxicity | 13 | 698 | −.03 | .17 | −.29, .34 | .87 | 164.40*** |
| Lymphocyte proliferation | |||||||
| Proliferation to ConA | 6 | 297 | −.04 | .06 | −.15, .08 | .53 | 2.53 |
| Proliferation to PHA | 11 | 675 | .10 | .10 | −.09, .28 | .32 | 42.25*** |
| Proliferation to PWM | 7 | 284 | .12 | .16 | −.19, .40 | .45 | 28.72*** |
Note. CI = confidence interval; ConA = concanavalin A; PHA = phytohemagglutinin; PWM = pokeweed mitogen.
p < .001.
An additional group of studies in this area examined immune responses to a positive initial biopsy for breast cancer in primarily middle-aged female participants before and after the procedure. The three studies of this nature did not yield a consistent pattern of relations with any of the immune outcomes.
In summary, stressful event sequences did not elicit a robust pattern of immune changes when considered as a whole. When these sequences are broken down into categories reflecting the stressor’s nature, the meta-analysis yields evidence of declines in natural immune response following the loss of a spouse, nonsignificant increases in natural and specific immune responses following exposure to natural disaster, and no immune alterations with breast biopsy. Unfortunately, we cannot determine whether these disparate patterns of immune response are attributable to features of the stressors, demographic or medical characteristics of the participants, or some interaction between these factors.
Chronic stressors
Chronic stressors included dementia caregiving, living with a handicap, and unemployment. Like other nonacute stressors, they did not have any systematic relationship with enumerative measures of the immune system. They did, however, have negative effects on almost all functional measures of the immune system (see Table 7). Both natural and specific immunity were negatively affected, as were Th1 (e.g., T cell proliferative responses) and Th2 (e.g., antibody to influenza vaccine) parameters. The only nonsignificant change was for antibody to latent virus; this effect size was substantial (r = .44), but there was also substantial heterogeneity. Further analyses showed that demographics did not moderate this effect: Immune responses to chronic stressors were equally strong across the age spectrum as well as across sex.
Table 7.
Meta-Analysis of Immune Responses to Chronic Stress in Healthy Participants
| Immune marker | k | N | r | SEr | 95% CI | p | Q |
|---|---|---|---|---|---|---|---|
| Leukocyte subset count | |||||||
| Leukocytes | 4 | 240 | .07 | .07 | −.06, .19 | .32 | 2.12 |
| Neutrophils | 3 | 124 | .36 | .36 | −.33, .79 | .31 | 20.45*** |
| Eosinophils | 3 | 124 | −.07 | .22 | −.47, .35 | .75 | 8.07* |
| Monocytes | 4 | 240 | −.04 | .17 | −.36, .29 | .83 | 14.33** |
| Lymphocytes | 4 | 240 | −.06 | .10 | −.25, .13 | .54 | 5.24 |
| T lymphocytes | 5 | 470 | −.03 | .05 | −.12, .06 | .55 | 2.75 |
| T-helper lymphocytes | 10 | 786 | −.05 | .04 | −.12, .03 | .22 | 8.54 |
| T-cytotoxic lymphocytes | 10 | 786 | −.08 | .08 | −.23, .08 | .34 | 33.44*** |
| T-helper:T-cytotoxic ratio | 6 | 528 | −.11 | .08 | −.29, .08 | .26 | 17.47** |
| Activated B lymphocytes | 3 | 138 | −.02 | .09 | −.19, .15 | .82 | 0.03 |
| Natural killer cells | 4 | 158 | −.14 | .32 | −.65, .45 | .65 | 33.61*** |
| Leukocyte subset percentage | |||||||
| Monocytes | 3 | 224 | .08 | .10 | −.11, .26 | .42 | 3.18 |
| T lymphocytes | 5 | 522 | −.03 | .05 | −.13, .07 | .59 | 4.93 |
| T-helper lymphocytes | 10 | 860 | −.07 | .06 | −.18, .03 | .19 | 19.45* |
| T-cytotoxic lymphocytes | 10 | 860 | .02 | .05 | −.08, .11 | .75 | 13.72* |
| Natural killer cells | 6 | 246 | .04 | .09 | −.13, .21 | .64 | 7.85 |
| Specific immunoglobulin | |||||||
| Antibody to herpes simplex virus 1 | 3 | 185 | .44 | .34 | −.19, .81 | .17 | 20.78*** |
| Antibody to influenza after vaccination | 3 | 304 | −.22 | .05 | −.33, −.11 | .001 | 0.38 |
| Natural killer cell function | |||||||
| Natural killer cell cytotoxicity | 8 | 563 | −.12 | .05 | −.20, −.01 | .04 | 11.58 |
| Lymphocyte proliferation | |||||||
| Proliferation to ConA | 4 | 486 | −.13 | .06 | −.24, −.02 | .02 | 4.06 |
| Proliferation to PHA | 6 | 636 | −.16 | .06 | −.27, −.05 | .004 | 8.75 |
| Cytokine production | |||||||
| Interleukin-2 | 3 | 355 | −.21 | .05 | −.31, −.11 | .001 | 1.50 |
Note. CI = confidence interval; ConA = concanavalin A; PHA = phytohemagglutinin.
p < .05.
p < .01.
p < .001.
Distant stressors
Distant stressors were traumatic events such as combat exposure or abuse occurring years prior to immune assessment. The meta-analytic results for distant stressors appear in Table 8. The only immune outcome that has been examined regularly in this literature is natural killer cell cytotoxicity, and it is not reliably altered in persons who report a distant traumatic experience.
Table 8.
Meta-Analysis of Immune Responses to Distant Stressors and Posttraumatic Stress Disorder in Healthy Participants
| Immune marker | k | N | r | SEr | 95% CI | p | Q |
|---|---|---|---|---|---|---|---|
| Natural killer cell cytotoxicity | 3 | 94 | −.05 | .25 | −.49, .41 | .84 | 7.67* |
Note. CI = confidence interval.
p < .05.
Meta-Analytic Results for the Effects of Checklists and Ratings
Nonspecific life events
Most of the studies in this area examined whether immune responses varied as a function of the number of life events a person endorsed on a standard checklist, a person’s rating of the impact of those events, or both. As Table 9 illustrates, this methodology yielded little in the way of significant outcomes in healthy participants. To determine whether vulnerability to life events might vary across the life span, we divided studies into two categories on the basis of a natural break in the age distribution. These analyses provided evidence that older adults are especially vulnerable to life-event–induced immune change. In studies that used samples of adults who had a mean age above 55, life events were associated with reliable declines in lymphocyte-proliferative responses to PHA (r = −.40, p = .05; k = 2) and natural killer cell cytotoxicity (r = −.59, p = .001; k = 2). These effects were much weaker in studies with a mean age below 55: Life events were not associated with proliferative responses to PHA (r = −.22, p = .24; k = 2), and showed a reliable but modest relationship with natural killer cell cytotoxicity (r = −.10, p = .03; k = 8). The differences in effect size between older and younger adults were statistically significant for natural killer cell cytotoxicity ( p < .001) but not PHA-induced proliferation ( p <.15). None of the other moderators we examined—sex ratio, kind of life event assessed (daily hassle vs. major event), or the method used to do so (checklist vs. interview)—was related to immune outcomes.
Table 9.
Meta-Analysis of Immune Responses to Major and Minor Life Events of Unknown Duration in Healthy Participants
| Immune marker | k | N | r | SEr | 95% CI | p | Q |
|---|---|---|---|---|---|---|---|
| Leukocyte subset count | |||||||
| Lymphocytes | 5 | 537 | −.18 | .17 | −.47, .14 | .27 | 20.28*** |
| T lymphocytes | 4 | 237 | .00 | .07 | −.13, .13 | .99 | 0.00 |
| T-helper lymphocytes | 5 | 227 | .00 | .07 | −.13, .13 | .99 | 0.00 |
| T-cytotoxic lymphocytes | 5 | 227 | .05 | .07 | −.09, .18 | .48 | 3.02 |
| T-helper:T-cytotoxic ratio | 3 | 70 | .14 | .38 | −.54, .71 | .71 | 12.11** |
| Natural killer cells | 4 | 194 | −.08 | .07 | −.22, .07 | .28 | 2.72 |
| Leukocyte subset percentage | |||||||
| T lymphocytes | 3 | 151 | .20 | .21 | −.21, .55 | .34 | 7.61* |
| T-helper lymphocytes | 7 | 285 | .01 | .06 | −.11, .13 | .83 | 0.54 |
| T-cytotoxic lymphocytes | 6 | 205 | −.01 | .07 | −.15, .14 | .92 | 0.07 |
| Natural killer cells | 5 | 261 | .00 | .06 | −.12, .12 | .99 | 0.00 |
| Total immunoglobulins | |||||||
| Serum IgA | 3 | 124 | −.07 | .10 | −.26, .14 | .52 | 2.19 |
| Serum IgG | 3 | 124 | −.06 | .10 | −.24, .13 | .54 | 2.06 |
| Serum IgM | 3 | 124 | .03 | .09 | −.15, .21 | .72 | 0.72 |
| Secretory IgA rate | 3 | 276 | −.08 | .10 | −.26, .11 | .43 | 3.97 |
| Secretory IgA concentration | 4 | 101 | −.16 | .14 | −.42, .12 | .25 | 4.34 |
| Specific immunoglobulin | |||||||
| Epstein-Barr virus | 3 | 317 | −.02 | .11 | −.23, .19 | .86 | 5.65 |
| Natural killer cell function | |||||||
| Natural killer cell cytotoxicity | 12 | 672 | −.07 | .07 | −.20, .07 | .35 | 29.39*** |
| Lymphocyte proliferation | |||||||
| Proliferation to ConA | 3 | 72 | −.13 | .15 | −.35, .16 | .38 | 2.49 |
| Proliferation to PHA | 4 | 131 | −.26 | .15 | −.50, .03 | .08 | 6.11 |
Note. CI = confidence interval; IgA = immunoglobulin A; IgG = immunoglobulin G; IgM = immunoglob-ulin M; ConA = concanavalin A; PHA = phytohemagglutinin.
p < .05.
p < .01.
p < .001.
Table 10 presents the relationship between life events and immune parameters in participants with HIV/AIDS. The presence of life events was associated with a significant reduction in the number of natural killer cells and a marginal reduction in the number of T-cytotoxic lymphocytes. It is unrelated to the number of T-helper lymphocytes, the percentage of T-cytotoxic lymphocytes, and the T-helper:T-cytotoxic ratio, all of which are recognized indicators of disease progression for patients with HIV/AIDS.
Table 10.
Meta-Analysis of Immune Responses to Major and Minor Life Events of Unknown Duration in Participants With HIV/AIDS
| Immune marker | k | N | r | SEr | 95% CI | p | Q |
|---|---|---|---|---|---|---|---|
| Leukocyte subset count | |||||||
| T-helper lymphocytes | 11 | 998 | −.01 | .03 | −.08, .05 | .70 | 7.70 |
| T-cytotoxic lymphocytes | 6 | 669 | −.14 | .08 | −.29, .01 | .08 | 17.92** |
| T-helper:T-cytotoxic ratio | 3 | 356 | −.02 | .05 | −.13, .09 | .70 | 0.09 |
| Natural killer cells | 3 | 261 | −.27 | .06 | −.38, −.15 | .001 | 0.30 |
| Leukocyte subset percentage | |||||||
| T-helper lymphocytes | 4 | 1,026 | −.02 | .06 | −.15, .10 | .73 | 7.58 |
| T-cytotoxic lymphocytes | 3 | 223 | .00 | .07 | −.13, .13 | .99 | 0.00 |
Note. CI = confidence interval.
p < .01.
We have already proposed that immunological disease diminishes the resilience and self-regulation of the immune system, making it more vulnerable to stress-related disruption, and this may be the case in HIV-infected versus healthy populations. However, studies of HIV-infected populations also utilized more refined measures of life events (interviews that factor in biographical context) than did studies of healthy populations (typically, checklist measures). Unfortunately, we cannot differentiate between these explanations on the basis of the available data.
Global stress appraisals and intrusive thoughts
The meta-analysis of stress appraisals and intrusive thoughts is displayed in Table 11. These studies generally enrolled large populations of adults who were not experiencing any specific form of stress and examined whether their immune responses varied according to stress appraisals and/or intrusive thoughts. This methodology was unsuccessful at documenting immune changes related to stress. Because of the small number of studies in this category, moderator analyses could not be performed.
Table 11.
Meta-Analysis of Immune Responses to Global Stress Appraisals in Healthy Participants
| Immune marker | k | N | r | SEr | 95% CI | p | Q |
|---|---|---|---|---|---|---|---|
| Leukocyte subset count | |||||||
| T lymphocytes | 3 | 241 | −.15 | .09 | −.31, .03 | .10 | 3.15 |
| T-helper lymphocytes | 3 | 241 | −.14 | .10 | −.32, .06 | .18 | 3.80 |
| T-cytotoxic lymphocytes | 4 | 279 | −.02 | .09 | −.19, .15 | .80 | 5.09 |
| Naive T lymphocytes | 3 | 241 | −.09 | .11 | −.29, .12 | .41 | 4.29 |
| Natural killer cells | 3 | 205 | −.20 | .13 | −.42, .04 | .10 | 4.28 |
| Leukocyte subset percentage | |||||||
| T-helper lymphocytes | 3 | 143 | −.02 | .09 | −.19, .15 | .79 | 0.08 |
| T-cytotoxic lymphocytes | 3 | 143 | −.03 | .09 | −.23, .11 | .48 | 0.60 |
| Total immunoglobulin | |||||||
| Serum IgG | 4 | 332 | .02 | .10 | −.18, .20 | .87 | 7.51 |
| Natural killer cell function | |||||||
| Natural killer cell cytotoxicity | 4 | 151 | −.11 | .09 | −.27, .06 | .21 | 1.85 |
Note. CI = confidence interval; IgG = immunoglobulin G.
The meta-analysis results shown in Table 12 address a similar question with regard to persons who are in the midst of a specific event sequence or a chronic stressor. To the extent that they appraise their lives as stressful or report the occurrence of intrusive thoughts, these individuals exhibit a significant reduction in natural killer cell cytotoxicity. Although this effect does not extend to the number of T-helper and T-cytotoxic lymphocytes in the circulation, it suggests that a person’s subjective representation of a stressor may be a determinant of its impact on the immune response.
Table 12.
Meta-Analysis of Immune Responses to Stress Appraisals and Intrusive Thoughts Within Healthy Stressed Populations
| Immune marker | k | N | r | SEr | 95% CI | p | Q |
|---|---|---|---|---|---|---|---|
| Leukocyte subset count | |||||||
| T-helper lymphocytes | 3 | 462 | −.10 | .11 | −.31, .11 | .35 | 7.52* |
| T-cytotoxic lymphocytes | 3 | 462 | −.26 | .32 | −.71, .34 | .40 | 57.99*** |
| Natural killer cell function | |||||||
| Natural killer cell cytotoxicity | 3 | 566 | −.15 | .06 | −.27, −.02 | .02 | 7.97 |
Note. CI = confidence interval.
p < .05.
p < .001.
Evidence Regarding Type I Error and Publication Bias
The large number of effect sizes generated by the meta-analysis raises the possibility of Type I error. One strategy for evaluating this concern involves dividing the number of significant findings in a meta-analysis by the total number of analyses conducted. When we performed this calculation, a value of 25.6% emerged, suggesting that more than one fourth of the analyses yielded reliable findings. This exceeds the 5% value at which investigators typically become concerned about Type I error rates and gives us confidence that the meta-analytic findings presented here are robust.
A second concern arises from the publication bias toward positive findings, which could skew meta-analytic results toward larger effect sizes. Fortunately, recent advances in meta-analysis enable one to evaluate the extent of this publication bias by using graphical techniques. A funnel plot can be drawn in which effect sizes are plotted against sample sizes for any group of studies. Because most studies in any given area have small sample sizes and therefore tend to yield more variable findings, the plot should end up looking like a funnel, with a narrow top and a wide bottom. If there is a bias against negative findings in an area, the plot is shifted toward positive values or a chunk of it will be missing entirely.
We drew funnel plots for all of the immune outcomes in the meta-analysis for which there were a sufficient number of observations. Although not all of them yielded perfect funnels, there was no systematic evidence of publication bias. Space limitations prevent us from including all plots; however, Figure 1 displays three plots that are prototypical of those we drew. As is evident from the data in the figure, psychoneuroimmunology researchers seem to be reporting positive and negative findings—and not hiding unfavorable outcomes when they do emerge. Thus, we do not have any major concerns about publication bias leading this meta-analysis to dramatically overestimate effect sizes.
Figure 1.
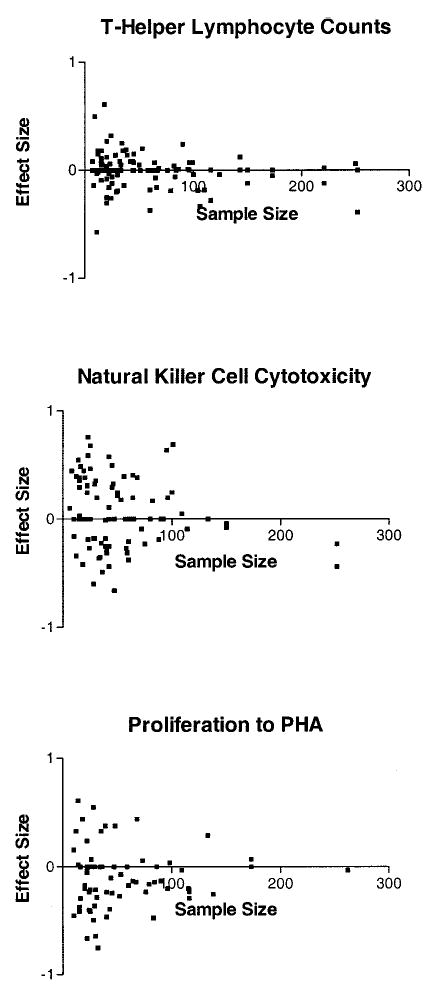
Funnel plots depicting relationship between effect size and sample size. PHA = phytohemagglutinin.
Discussion
The immune system, once thought to be autonomous, is now known to respond to signals from many other systems in the body, particularly the nervous system and the endocrine system. As a consequence, environmental events to which the nervous system and endocrine system respond can also elicit responses from the immune system. The results of meta-analysis of the hundreds of research reports generated by this hypothesis indicate that stressful events reliably associate with changes in the immune system and that characteristics of those events are important in determining the kind of change that occurs.
Models of Stress and the Immune System
Selye’s (1975) seminal findings suggested that stress globally suppressed the immune system and provided the first model for how stress and immunity are related. This model has recently been challenged by views that relations between stress and the immune system should be adaptive, at least within the context of fight-or-flight stressors, and an even newer focus on the balance between cellular and humoral immunity. The present meta-analytic results support three of these models. Depending on the time frame, stressors triggered adaptive upregulation of natural immunity and suppression of specific immunity (acute time-limited), cytokine shift (brief naturalistic), or global immunosuppression (chronic).
When stressors were acute and time-limited—that is, they generally followed the temporal parameters of fight-or-flight stressors—there was evidence for adaptive redistribution of cells and preparation of the natural immune system for possible infection, injury, or both. In evolution, stressor-related changes in the immune system that prepared the organisms for infections resulting from bites, puncture wounds, scrapes, or other challenges to the integrity of the skin and blood could be selected for. This process would be most adaptive when it was also efficient and did not divert excess energy from fight-or-flight behavior. Indeed, changes in the immune system following acute stress conformed to this pattern of efficiency and energy conservation. Acute stress upregu-lated parameters of natural immunity, the branch of the immune system in which most changes occurred, which requires only minimal time and energy investment to act against invaders and is also subject to the fewest inhibitory constraints on acting quickly (Dopp et al., 2000; Sapolsky, 1998). In contrast, energy may actually be directed away from the specific immune response, as indexed by the decrease in the proliferative response. The specific immune response in general and proliferation in particular demand time and energy; therefore, this decrease might indicate a redirection away from this function. Similar redirection occurs during fight-or-flight stressors with regard to other nonessential, future-oriented processes such as digestion and reproduction. As stressors became more chronic, the potential adaptiveness of the immune changes decreased. The effect of brief stressors such as examinations was to change the potency of different arms of specific immunity—specifically, to switch away from cellular (Th1) immunity and toward humoral (Th2) immunity.
The stressful event sequences tended to fall into two substantive groups: bereavement and trauma. Bereavement was associated with decreased natural killer cell cytotoxicity. Trauma was associated with nonsignificantly increased cytotoxicity and increased proliferation but decreased numbers of T cells in peripheral blood. The different results for loss and trauma mirror neuroendocrine effects of these two types of adverse events. Loss—maternal separation in nonhuman animals and bereavement in humans—is commonly associated with increased cortisol production (Irwin, Daniels, Risch, Bloom, & Weiner, 1988; Laudenslager, 1988; McCleery, Bhagwagar, Smith, Goodwin, & Cowen, 2000). In contrast, trauma and posttraumatic stress disorder are commonly associated with decreased cortisol production (see Yehuda, 2001; Yehuda et al., 1998, for reviews). To the degree that cortisol suppresses immune function such as natural killer cell cytotoxicity, these results have the potential to explain the different effects of loss and trauma event sequences.
The most chronic stressors were associated with the most global immunosuppression, as they were associated with reliable decreases in almost all functional immune measures examined. Increasing stressor duration, therefore, resulted in a shift from potentially adaptive changes to potentially detrimental changes, initially in cellular immunity and then in immune function more broadly. It is important to recognize that although the effects of chronic stressors may be due to their duration, the most chronic stressors were associated with changes in identity or social roles (e.g., acquiring the role of caregiver or refugee or losing the role of employee). These chronic stressors may also be more persistent, that is, constantly rather than intermittently present. Finally, chronic stressors may be less controllable and afford less hope for control in the future. These qualities could contribute to the severity of the stressor in terms of both its psychological and physiological impact.
Increasing stressor chronicity also impacted the type of parameter in which changes were seen. Compared with the natural immune system, the specific immune system is time and energy intensive and as such is expected to be invoked only when circumstances (either a stressor or an infection; cf. Maier & Watkins, 1998) persist for a longer period of time. Affected immune domains—natural versus specific—were consistent with the duration of the stressors—acute versus chronic. Furthermore, changing immune responses via redistribution of cells can happen much faster than changes via the function of cells. The time frames of the stressor and the immune domain were also consistent; acute stress affected primarily enumerative measures, whereas stressors of longer duration affected primarily functional measures.
The results of these analyses suggest that the dichotomization of the immune system into natural and specific categories and, within specific immunity, into cellular and humoral measures, is a useful starting point with regard to understanding the effects of stressors. Categorizing an immune response is a difficult process, as each immune response is highly redundant and includes natural, specific, cellular, and humoral immune responses acting together. Given this redundancy, the differential results within these theoretical divisions were remarkably, albeit not totally, consistent. As further immunological research defines these divisions more subtly, the results with regard to stressors may become even clearer. However, the present results suggest that the categories used here are meaningful.
The results of this meta-analysis reflect the theoretical and empirical progress of this literature over the past 4 decades. Increased differentiation in the quality of stressors and the immunological parameters investigated have allowed complex models to be tested. In contrast, previous meta-analyses were bound by a small number of more homogenous studies. Herbert and Cohen (1993) reported on 36 studies published between 1977 and 1991, finding broadly immunosuppressive effects of stress. Zorrilla et al. (2001) reported on 82 studies published between 1980 and 1996, finding potentially adaptive effects of acute stressors in addition to evidence for immunosuppression with longer stressors. It is important to note that meta-analytic findings are bound by the models tested in the literature. As more complex models are tested, more complex relationships emerge in meta-analysis. We next consider some such areas of complexity that should be considered in future psychoneuroimmunology research.
Individual Differences and Immune Change Under Stress
The meta-analytic results indicate that organismic variables such as age and disease status moderate vulnerability to stress-related decreases in functional immune measures. Both aging and HIV are associated with immune senescence and loss of responsiveness (Effros et al., 1994; Effros & Pawelec, 1997), and both are also associated with disruption of neuroendocrine inputs to the immune system (Kumar et al., 2002; Madden, Thyagarajan, & Felten, 1998). The loss of self-regulation in disease and aging likely makes affected people more susceptible to negative immunological effects of stress. Finally, the meta-analysis did not reveal effects of sex on immune responses to stressors. However, these comparisons simply correlated the sex ratio of the studies with effect sizes. Grouping data by sex would afford a more powerful comparison, but few studies organized their data that way. Gender may moderate the effects of stress on immunity by virtue of the effects of sex hormones on immunity; generally, men are considered to be more biologically vulnerable (Maes, 1999), and they may be more psychosocially vulnerable (e.g.,Scanlan, Vitaliano, Ochs, Savage, & Borson, 1998).
It seems likely to us that individual differences in subjective experience also make a substantive contribution to explaining this phenomenon. Studies have convincingly demonstrated that people’s cardiovascular and neuroendocrine responses to stressful experience are dependent on their appraisals of the situation and the presence of intrusive thoughts about it (Baum et al., 1993; Frankenhauser, 1975; Tomaka et al., 1997). Although the same logic should apply to people’s immune responses to stressful experience, few of the studies in this area have included measures of subjective experience, and those reports were limited by methodological issues such as aggregation across heterogeneous stressors. As a consequence, measures of subjective experience were not significantly associated with immune parameters in healthy research participants, with the exception of a modest (r = −.10) relationship between intrusive thoughts and natural killer cell cytotoxicity. Psychological variables such as personality and emotion can give rise to individual differences in psychological and concomitant immunological responses to stress. Optimism and coping, for example, moderated immunological responses to stressors in several studies (e.g., Barger et al., 2000; Bosch et al., 2001; Cruess et al., 2000; Segerstrom, 2001; Stowell, Kiecolt-Glaser, & Glaser, 2001).
Mechanisms of Stress Effects on the Immune System
Virtually nothing is known about the psychological pathways linking stressors with the immune system. Many theorists have argued that affect is a final common pathway for stressors (e.g., S. Cohen, Kessler, & Underwood, 1995; Miller & Cohen, 2001), yet studies have enjoyed limited success in attempting to explain people’s immune responses to life experiences on the basis of their emotional states alone (Bower et al., 1998; Cole, Kemeny, Taylor, Visscher, & Fahey, 1996; Miller, Dopp, Myers, Stevens, & Fahey, 1999; Segerstrom, Taylor, Kemeny, & Fahey, 1998). Furthermore, many studies have focused on the immune effects of emotional valence (e.g., unhappy vs. happy; Futterman, Kemeny, Shapiro, & Fahey, 1994), but the immune system may be even more closely linked to emotional arousal (e.g., stimulated vs. still), especially during acute stressors (S. Cohen et al., 2000). Finally, it is possible that emotion will prove to be relatively unimportant and that other mental processes such as motivational states or cognitive appraisals will prove to be the critical psychological mechanisms linking stress and the immune system (cf. Maier, Waldstein, & Synowski, 2003).
In terms of biological mechanisms, the field is further along, but much remains to be learned. A series of studies in the mid-1990s was able to show via beta-adrenergic blockade that activation of the sympathetic nervous system was responsible for the immune system effects of acute stressors (Bachen et al., 1995; Benschop, Nieuwenhuis, et al., 1994). Apart from these findings, however, little is known about biological mechanisms, especially with regard to more enduring stressors that occur in the real world. Studies that have attempted to identify hormonal pathways linking stressors and the immune system have enjoyed limited success, perhaps because they have utilized snapshot assessments of hormones circulating in blood. Future studies can maximize their chances of identifying relevant mediators by utilizing more integrated measures of hormonal output, such as 24-hr urine collections or diurnal profiles generated through saliva collections spaced throughout the day (Baum & Grunberg, 1995; Stone et al., 2001).
Future studies could also benefit from a greater emphasis on behavior as a potential mechanism. This strategy has proven useful in studies of clinically depressed patients, in which decreased physical activity and psychomotor retardation (Cover & Irwin, 1994; Miller, Cohen, & Herbert, 1999), increased body mass (Miller, Stetler, Carney, Freedland, & Banks, 2002), disturbed sleep (Cover & Irwin, 1994; Irwin, Smith, & Gillin, 1992), and cigarette smoking (Jung & Irwin, 1999) have been shown to explain some of the immune dysregulation evident in this population. There is already preliminary evidence, for instance, that sleep loss might be responsible for some of the immune system changes that accompany stressors (Hall et al., 1998; Ironson et al., 1997).
Stress, the Immune System, and Disease
The most pressing question that future research needs to address is the extent to which stressor-induced changes in the immune system have meaningful implications for disease susceptibility in otherwise healthy humans. In the 30 years since work in the field of psychoneuroimmunology began, studies have convincingly established that stressful experiences alter features of the immune response as well as confer vulnerability to adverse medical outcomes that are either mediated by or resisted by the immune system. However, with the exception of recent work on upper respiratory infection (S. Cohen, Doyle, & Skoner, 1999), studies have not yet tied these disparate strands of work together nor determined whether immune system changes are the mechanism through which stressors increase susceptibility to disease onset. In contrast, studies of vulnerable populations such as people with HIV have shown changes in immunity to predict disease progression (Bower et al., 1998).
To test an effect of this nature, researchers need to build clinical outcome assessments into study designs where appropriate. For example, chronic stressors reliably diminish the immune system’s capacity to produce antibodies following routine influenza vaccinations (see Table 7). Yet as far as we are aware, none of these studies has tracked illness to explore whether stress-related disparities in vaccine response might be sufficient to heighten susceptibility to clinical infection with influenza. Cytokine expression represents a relatively new and promising example of an avenue for research linking stress, immune change, and disease. For example, chronic stress may elicit prolonged secretion of cortisol, to which white blood cells mount a counterregulatory response by downregulating their cortisol receptors. This downregulation, in turn, reduces the cells’ capacity to respond to anti-inflammatory signals and allows cytokine-mediated inflammatory processes to flourish (Miller, Cohen, & Ritchey, 2002). Stress therefore might contribute to the course of diseases involving excessive nonspecific inflammation (e.g., multiple sclerosis, rheumatoid arthritis, coronary heart disease) and thereby increase risk for excess morbidity and mortality (Ershler & Keller, 2000; Papanicoloaou et al., 1998; Rozanski, Blumenthal, & Kaplan, 1999). Another example of the importance of cytokines to clinical pathology is in asthma and allergy, in which emerging evidence implicates excess Th2 cytokine secretion in the exacerbation of these diseases (Busse & Lemanske, 2001; Luster, 1998).
Conclusion
Sapolsky (1998) wrote,
Stress-related disease emerges, predominantly, out of the fact that we so often activate a physiological system that has evolved for responding to acute physical emergencies, but we turn it on for months on end, worrying about mortgages, relationships, and promotions. (p. 7)
The results of this meta-analysis support this assertion in one sense: Stressors with the temporal parameters of the fight-or-flight situations faced by humans’ evolutionary ancestors elicited potentially beneficial changes in the immune system. The more a stres-sor deviated from those parameters by becoming more chronic, however, the more components of the immune system were affected in a potentially detrimental way.
Further research is needed to support two other ideas elicited by this quote: the idea that subjective experience such as worry is more likely to result in stress-related immune change than objective experience and the idea that stress-related immune change results in stress-related disease. Though the results of the meta-analysis were not encouraging on the first point, many of these studies suffered from methodological limitations. We hope that these results will inform investigations that go beyond the relationship between a stressful event and an immune parameter to investigate the psychological phenomena that mediate that relationship. Finally, these results can also inform investigations into stress, immunity, and disease process. Whether the disease is characterized by natural or specific immunity, its cytokine profile, and its regulation by anti-inflammatory agents such as cortisol, may determine the disparate effects of different kinds of stressors.
Acknowledgments
Preparation of this work was supported by American Heart Association Grant 0160367Z, the National Alliance for Research on Schizophrenia and Depression, National Institute of Mental Health Grant 61531, and Michael Smith Foundation for Health Research Grant CI-SCH-58. We thank Edith Chen for her helpful comments on an earlier version of the article and Jennifer Snedeker for assistance with manuscript preparation.
Footnotes
The term pathogen is used here to refer to microorganisms that can cause disease. This term is most appropriate in the evolutionary context we proposed in the article’s introduction because it focuses on susceptibility to infection. However, the reader should be aware that pathogens are only a subset of antigens, that is, all substances that evoke an immune response. Other antigenic substances include, for example, transformed self-cells (i.e., cancer cells), transplanted tissue, and allergens (i.e., antigens that evoke an allergic response).
The proportion of student samples varied across stressor categories. Nearly all of the studies of brief naturalistic stressors used student samples (k = 60; 95.2%) because these stressors were predominantly examinations. Student samples were also used in a large minority of acute time-limited stressor studies (k = 31; 40.5%) but constituted a small minority of samples used in studies of life-event checklists (k = 8; 14.0%) and studies of event sequences (k = 2; 6.6%), and student samples were not used in studies of chronic stressors or stress appraisals and intrusions. These are rough estimates, as some studies did not specify whether young adult samples were drawn from a student population.
Contributor Information
Suzanne C. Segerstrom, University of Kentucky.
Gregory E. Miller, University of British Columbia
References
References marked with an asterisk indicate studies included in the meta-analysis.
- *Abdeljaber MH, Nair MPN, Schork MA, Schwartz SA. Depressed natural killer cell activity in schizophrenic patients. Immunological Investigations. 1994;23:259–268. doi: 10.3109/08820139409066822. [DOI] [PubMed] [Google Scholar]
- *Ackerman KD, Martino M, Heyman R, Moyna NM, Rabin BS. Immunologic response to acute psychological stress in MS patients and controls. Journal of Neuroimmunology. 1996;68:85–94. doi: 10.1016/0165-5728(96)00077-x. [DOI] [PubMed] [Google Scholar]
- *Ackerman KD, Martino M, Heyman R, Moyna NM, Rabin BS. Stressor-induced alteration of cytokine production in multiple sclerosis patients and controls. Psychosomatic Medicine. 1998;60:484– 491. doi: 10.1097/00006842-199807000-00016. [DOI] [PubMed] [Google Scholar]
- Ader R, Cohen N, Felten D. January 14). Psychoneuroimmunology: Interactions between the nervous system and the immune system. Lancet. 1995;345:99–103. doi: 10.1016/s0140-6736(95)90066-7. [DOI] [PubMed] [Google Scholar]
- Ader, R., Felten, D. L., & Cohen, N. (2001). Psychoneuroimmunology (3rd ed.). San Diego, CA: Academic Press.
- *Aloe L, Bracci-Laudiero L, Alleva E, Lambiase A, Micera A, Tirassa P. Emotional stress induced by parachute jumping enhances blood nerve growth factor levels and the distribution of nerve growth factor receptors in lymphocytes. Proceedings of the National Academy of Sciences, USA. 1994;91:10440–10444. doi: 10.1073/pnas.91.22.10440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- American Psychiatric Association. (1994). Diagnostic and statistical manual of mental disorders (4th ed.). Washington, DC: Author.
- *Andersen BL, Farrar WB, Golden-Kreutz D, Kutz LA, MacCallum R, Courtney ME, Glaser R. Stress and immune responses after surgical treatment for regional breast cancer. Journal of the National Cancer Institute. 1998;90:30–36. doi: 10.1093/jnci/90.1.30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Andersen BL, Kiecolt-Glaser JK, Glaser R. A biobehavioral model of cancer stress and disease course. American Psychologist. 1994;49:389– 404. doi: 10.1037//0003-066x.49.5.389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anstead MI, Hunt TA, Carlson SL, Burki NK. Variability of peripheral blood lymphocyte beta-2-adrenergic receptor density in humans. American Journal of Respiratory and Critical Care Medicine. 1998;157:990–992. doi: 10.1164/ajrccm.157.3.9704071. [DOI] [PubMed] [Google Scholar]
- *Antoni MH, August S, LaPerriere A, Baggett HL, Klimas N, Ironson G, et al. Psychological and neuroendocrine measures related to functional immune changes in anticipation of HIV-1 serostatus notification. Psychosomatic Medicine. 1990;52:496–510. doi: 10.1097/00006842-199009000-00002. [DOI] [PubMed] [Google Scholar]
- *Aragona M, Muscatello MRA, Losi E, Panetta S, la Torre F, Pastura G, et al. Lymphocyte number and stress parameter modifications in untreated breast cancer patients with depressive mood and previous life stress. Journal of Experimental Therapeutics and Oncology. 1996;1:354–360. [PubMed] [Google Scholar]
- *Arber N, Berliner S, Arber L, Lipshitz A, Sinai Y, Zajicek G, et al. The state of leukocyte adhesiveness/aggregation in the peripheral blood is more sensitive than the white blood cell count for the detection of acute mental stress. Journal of Psychosomatic Research. 1992;36:37–46. doi: 10.1016/0022-3999(92)90112-f. [DOI] [PubMed] [Google Scholar]
- *Arnetz BB, Brenner SO, Levi L, Petterson IL, Wasserman J, Petrini B, et al. Neuroendocrine and immunologic effects of unemployment and job insecurity. Psychotherapy and Psychosomatics. 1991;55:76– 80. doi: 10.1159/000288412. [DOI] [PubMed] [Google Scholar]
- *Bachen EA, Manuck SB, Cohen S, Muldoon MF, Raible R, Herbert TB, Rabin BS. Adrenergic blockade ameliorates cellular immune responses to mental stress in humans. Psychosomatic Medicine. 1995;57:366–372. doi: 10.1097/00006842-199507000-00008. [DOI] [PubMed] [Google Scholar]
- *Bachen EA, Manuck SB, Marsland AL, Cohen S, Malkoff SB, Muldoon MF, Rabin BS. Lymphocyte subset and cellular immune responses to a brief experimental stressor. Psychosomatic Medicine. 1992;54:673– 679. doi: 10.1097/00006842-199211000-00007. [DOI] [PubMed] [Google Scholar]
- *Baker GHB, Byrom NA, Irani MS, Brewerton DA, Hobbs JR, Wood RJ, Nagvekar NM. March 10). Stress, cortisol, and lymphocyte subpopulations. Lancet. 1984;10:574. doi: 10.1016/s0140-6736(84)90981-4. [DOI] [PubMed] [Google Scholar]
- *Baker GHB, Irani MS, Byrom NA, Nagvekar NM, Wood RJ, Hobbs JR, Brewerton DA. Stress, cortisol concentrations, and lymphocyte subpopulations. British Medical Journal. 1985;290:1393. doi: 10.1136/bmj.290.6479.1393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Barger ST, Marsland AL, Bachen EA, Manuck SB. Repressive coping and blood measures of disease risk: Lipids and endocrine and immunological responses to a laboratory stressor. Journal of Applied Social Psychology. 2000;30:1619–1638. [Google Scholar]
- *Bartrop RW, Luckhurst E, Lazarus L, Kiloh LG, Penny R. April 16). Depressed lymphocyte function after bereavement. Lancet. 1977;1:834– 836. doi: 10.1016/s0140-6736(77)92780-5. [DOI] [PubMed] [Google Scholar]
- *Bauer ME, Vedhara K, Perks P, Wilcock GK, Lightman SL, Shanks N. Chronic stress in caregivers of dementia patients is associated with reduced lymphocyte sensitivity to glucocorticoids. Journal of Neuroimmunology. 2000;103:84–92. doi: 10.1016/s0165-5728(99)00228-3. [DOI] [PubMed] [Google Scholar]
- Baum A, Cohen L, Hall M. Control and intrusive memories as possible determinants of chronic stress. Psychosomatic Medicine. 1993;55:274–286. doi: 10.1097/00006842-199305000-00005. [DOI] [PubMed] [Google Scholar]
- Baum, A., & Grunberg, N. (1995). Measurement of stress hormones. In S. Cohen, R. C. Kessler, & L. G. Underwood (Eds.), Measuring stress: A guide for health and social scientists (pp. 193–212). New York: Oxford University Press.
- *Beck RJ, Cesario TC, Yousefi A, Enamoto H. Choral singing, performance perception, and immune system changes in salivary immunoglobulin A and cortisol. Music Perception. 2000;18:87–106. [Google Scholar]
- *Beem EE, Hooijkaas H, Cleiren MH, Schut HA, Garssen B, Croon MA, et al. The immunological and psychological effects of bereavement: Does grief counseling really make a difference? A pilot study. Psychiatry Research. 1999;85:81–93. doi: 10.1016/s0165-1781(98)00135-8. [DOI] [PubMed] [Google Scholar]
- Ben Eliyahu S, Shakhar G, Page GG, Stefanski V, Shakhar K. Suppression of NK cell activity and of resistance to metastasis by stress: A role for adrenal catecholamines and beta-adrenoceptors. Neuroimmunomodulation. 2000;8:154–164. doi: 10.1159/000054276. [DOI] [PubMed] [Google Scholar]
- Benjamini, E., Coico, R., & Sunshine, G. (2000). Immunology: A short course (4th ed.). New York: Wiley-Liss.
- *Benschop RJ, Brosschot JF, Godaert GLR, de Smet MBM, Geenen R, Olff M, et al. Chronic stress affects immunologic but not cardiovascular responsiveness to acute psychological stress in humans. American Journal of Physiology. 1994;266:R75–R80. doi: 10.1152/ajpregu.1994.266.1.R75. [DOI] [PubMed] [Google Scholar]
- Benschop RJ, Geenen R, Mills PJ, Naliboff BD, Kiecolt-Glaser JK, Herbert TB, et al. Cardiovascular and immune responses to acute psychological stress in young and old women: A meta-analysis. Psychosomatic Medicine. 1998;60:290–296. doi: 10.1097/00006842-199805000-00015. [DOI] [PubMed] [Google Scholar]
- *Benschop RJ, Godaert GLR, Geenen R, Brosschot JF, de Smet MBM, Olff M, et al. Relationships between cardiovascular and immunological changes in an experimental stress model. Psychological Medicine. 1995;25:323–327. doi: 10.1017/s0033291700036229. [DOI] [PubMed] [Google Scholar]
- *Benschop RJ, Jabaaij L, Oostveen FG, Vingerhoets AJJM, Ballieux RE. The influence of psychological stress on immunoregulation of latent Epstein-Barr virus. Stress Medicine. 1998;14:21–29. [Google Scholar]
- *Benschop RJ, Jacobs R, Sommer B, Schürmeyer TH, Raab HR, Schmidt RE, Schedlowski M. Modulation of the immunologic response to acute stress in humans by β-blockade or benzodiazepines. Federation of American Societies for Experimental. Biology Journal. 1996;10:517–524. doi: 10.1096/fasebj.10.4.8647351. [DOI] [PubMed] [Google Scholar]
- *Benschop RJ, Nieuwenhuis EES, Tromp EAM, Godaert GLR, Ballieux RE, van Doornen LJP. Effects of β-adrenergic blockade on immunologic and cardiovascular changes induced by mental stress. Circulation. 1994;89:762–769. doi: 10.1161/01.cir.89.2.762. [DOI] [PubMed] [Google Scholar]
- Benschop RJ, Rodriguez-Feuerhahn M, Schedlowski M. Catecholamine-induced leukocytosis: Early observations, current research, and future directions. Brain, Behavior, and Immunity. 1996;10:77–91. doi: 10.1006/brbi.1996.0009. [DOI] [PubMed] [Google Scholar]
- Biondi, M. (2001). Effects of stress on immune functions: An overview. In R. Ader, D. L. Felten, & N. Cohen (Eds.), Psychoneuroimmunology (3rd ed., pp. 189–226). San Diego, CA: Academic Press.
- *Biondo M, Peronti M, Pacitti F, Pancheri P, Pacifici R, Altieri I, et al. Personality, endocrine and immune changes after eight months in healthy individuals under normal daily stress. Psychotherapy and Psychosomatics. 1994;62:176–184. doi: 10.1159/000288920. [DOI] [PubMed] [Google Scholar]
- *Birmaher B, Rabin BS, Garcia MR, Jain U, Whiteside TL, Wissiamson DE, et al. Cellular immunity in depressed, conduct disorder, and normal adolescents: Role of adverse life events. Journal of the American Academy of Child & Adolescent Psychiatry. 1994;33:671–678. doi: 10.1097/00004583-199406000-00008. [DOI] [PubMed] [Google Scholar]
- *Bisselli R, Farrace S, D’Ameloi R, Fattorossi A. Influence of stress on lymphocyte subset distribution—A flow cytometric study in young student pilots. Aviation, Space, and Environmental Medicine. 1993;64:116–120. [PubMed] [Google Scholar]
- *Bongartz W, Lyncker I, Kossman KT. The influence of hypnosis on white blood cell count and urinary levels of catecholamines and vanillyl mandelic acid. Hypnos. 1987;14:52– 61. [Google Scholar]
- *Borella P, Bargellini A, Rovesti S, Pinelli M, Vivoli R, Solfrini V, Vivoli G. Emotional stability, anxiety, and natural killer activity under examination stress. Psychoneuroendocrinology. 1999;24:613–627. doi: 10.1016/s0306-4530(99)00016-5. [DOI] [PubMed] [Google Scholar]
- Borenstein, M., & Rothstein, H. (1999). Comprehensive meta-analysis: A computer program for research synthesis [Computer software]. Englewood, NJ: Biostat.
- *Boscarino JA, Chang J. Higher abnormal leukocyte and lymphocyte counts 20 years after exposure to severe stress: Research and clinical implications. Psychosomatic Medicine. 1999;61:378–386. doi: 10.1097/00006842-199905000-00019. [DOI] [PubMed] [Google Scholar]
- *Bosch JA, Brand HS, Ligtenberg TJM, Bermond B, Hoogstraten J, Amerongen AVN. Psychological stress as a determinant of protein levels and salivary-induced aggregation of streptococcus gordonii in human whole saliva. Psychosomatic Medicine. 1996;58:374–382. doi: 10.1097/00006842-199607000-00010. [DOI] [PubMed] [Google Scholar]
- *Bosch JA, de Geus EJC, Kelder A, Veerman ECI, Hoogstraten J, Amerongen AVN. Differential effects of active versus passive coping on secretory immunity. Psychophysiology. 2001;38:836– 846. [PubMed] [Google Scholar]
- Bosch JA, Ring C, de Geus EJC, Veerman ECI, Amerongen AVN. Stress and secretory immunity. International Review of Neurobiology. 2002;52:213–253. doi: 10.1016/s0074-7742(02)52011-0. [DOI] [PubMed] [Google Scholar]
- Boucher N, Dufeu-Duchesne T, Vicaut E, Farge D, Effros RB, Schachter F. CD28 expression in T cell aging and human longevity. Experimental Gerontology. 1998;33:267–282. doi: 10.1016/s0531-5565(97)00132-0. [DOI] [PubMed] [Google Scholar]
- Bower JE, Kemeny ME, Taylor SE, Fahey JL. Cognitive processing, discovery of meaning, CD4 decline, and AIDS-related mortality among bereaved HIV-seropositive men. Journal of Consulting and Clinical Psychology. 1998;66:979–986. doi: 10.1037//0022-006x.66.6.979. [DOI] [PubMed] [Google Scholar]
- *Boyce WT, Adams S, Tschann JM, Cohen F, Wara D, Gunnar MR. Adrenocortical and behavioral predictors of immune responses to starting school. Pediatric Research. 1995;38:1009–1017. doi: 10.1203/00006450-199512000-00030. [DOI] [PubMed] [Google Scholar]
- *Boyce WT, Chesterman EA, Martin N, Folkman S, Cohen F, Wara D. Immunologic changes occurring at kindergarten entry predict respiratory illnesses after the Loma Preita earthquake. Developmental and Behavioral Pediatrics. 1993;14:296–303. [PubMed] [Google Scholar]
- *Breznitz S, Ben-Zur H, Berzon Y, Weiss DW, Levitan G, Tarcic N, et al. Experimental induction and termination of acute psychological stress in human volunteers: Effects on immunological, neuroendocrine, cardiovascular, and psychological parameters. Brain, Behavior, and Immunity. 1998;12:34–52. doi: 10.1006/brbi.1997.0511. [DOI] [PubMed] [Google Scholar]
- *Bristow M, Hucklebridge FH, Clow A, Evans PD. Modulation of secretory immunoglobulin A in saliva in relation to an acute episode of stress and arousal. Journal of Psychophysiology. 1997;11:248–255. [Google Scholar]
- *Brosschot JF, Benschop RJ, Godaert GLR, de Smet MB, Olff M, Heijnen CJ, Ballieux RE. Effects of experimental psychological stress on distribution and function of peripheral blood cells. Psychosomatic Medicine. 1992;54:394– 406. doi: 10.1097/00006842-199207000-00002. [DOI] [PubMed] [Google Scholar]
- *Brosschot JF, Benschop RJ, Godaert GLR, Olff M, de Smet M, Heijnen CJ, Ballieux RE. Influence of life stress on immunological reactivity to mild psychological stress. Psychosomatic Medicine. 1994;56:216–224. doi: 10.1097/00006842-199405000-00007. [DOI] [PubMed] [Google Scholar]
- *Brosschot JF, Smelt D, de Smet M, Heijen CJ, Olff M, Ballieux RE, Godaert GLR. Effects of experimental psychological stress on T-lymphocytes and NK cells in man: An exploratory study. Journal of Psychophysiology. 1991;5:59– 67. [Google Scholar]
- *Burleson MH, Malarkey WB, Cacioppo JT, Poehlmann KM, Kiecolt-Glaser JK, Berntson GG, Glaser R. Postmenopausal hormone replacement: Effects on autonomic, neuroendocrine, and immune reactivity to brief psychological stressors. Psychosomatic Medicine. 1998;60:17–25. doi: 10.1097/00006842-199801000-00004. [DOI] [PubMed] [Google Scholar]
- Busse WW, Lemanske RF. Advances in immunology: Asthma. New England Journal of Medicine. 2001;344:350–362. doi: 10.1056/NEJM200102013440507. [DOI] [PubMed] [Google Scholar]
- *Byrnes DM, Antoni MH, Goodkin K, Efantis-Potter J, Asthana D, Simon T, et al. Stressful events, pessimism, natural killer cell cytotoxicity, and cytotoxic/suppressor T cells in HIV positive Black women at risk for cervical cancer. Psychosomatic Medicine. 1998;60:714–722. doi: 10.1097/00006842-199811000-00009. [DOI] [PubMed] [Google Scholar]
- Cacioppo JT. Social neuroscience: Autonomic, neuroendocrine, and immune responses to stress. Psychophysiology. 1994;31:113–128. doi: 10.1111/j.1469-8986.1994.tb01032.x. [DOI] [PubMed] [Google Scholar]
- *Cacioppo JT, Malarkey WB, Kiecolt-Glaser JK, Uchino BN, Sgoutas-Emch SA, Sheridan JF, et al. Heterogeneity in neuroendocrine and immune responses to brief psychological stressors as a function of autonomic cardiac activation. Psychosomatic Medicine. 1995;57:154–164. doi: 10.1097/00006842-199503000-00008. [DOI] [PubMed] [Google Scholar]
- *Cacioppo JT, Poehlmann KM, Kiecolt-Glaser JK, Malarkey WB, Burleson MH, Berntson GG, Glaser R. Cellular immune responses to acute stress in female caregivers of dementia patients and matched controls. Health Psychology. 1998;17:182–189. doi: 10.1037//0278-6133.17.2.182. [DOI] [PubMed] [Google Scholar]
- *Caggiula AR, McAllister CG, Matthews KA, Berga SL, Owens JF, Miller AL. Psychological stress and immunological responsiveness in normally cycling, follicular-stage women. Journal of Neuroimmunology. 1995;59:103–111. doi: 10.1016/0165-5728(95)00031-v. [DOI] [PubMed] [Google Scholar]
- *Caudell KA, Gallucci BB. Neuroendocrine and immunological responses of women to stress. Western Journal of Nursing Research. 1995;17:672– 692. doi: 10.1177/019394599501700607. [DOI] [PubMed] [Google Scholar]
- *Chi DS, Neumann JK, Mota-Marquez M, Dubberley FA. Effects of acute stress on lymphocyte β2-adrenoceptors in White males. Journal of Psychosomatic Research. 1993;37:763–770. doi: 10.1016/0022-3999(93)90105-o. [DOI] [PubMed] [Google Scholar]
- Chiappelli, F., Manfrini, E., Franceschi, C., Cossarizza, A., & Black, K. L. (1994). Steroid regulation of cytokines: Relevance for Th1 to Th2 shift? In E. R. de Kloet, E. C. Azmitia, & P. W. Landfield (Eds.), Annals of the New York Academy of Sciences: Vol. 746. Brain corticosteroid receptors: Studies on the mechanism, function, and neurotoxicity of corticosteroid action (pp. 204–215). New York: New York Academy of Sciences. [DOI] [PubMed]
- *Cohen F, Keaney KA, Zegans LS, Kemeny ME, Neuhaus JM, Stites DP. Differential immune system changes with acute and persistent stress for optimists vs. pessimists. Brain, Behavior, and Immunity. 1999;13:155–174. doi: 10.1006/brbi.1998.0531. [DOI] [PubMed] [Google Scholar]
- Cohen, J., & Cohen, P. (1983). Applied multiple regression/correlation for the behavioral sciences Hillsdale, NJ: Erlbaum.
- Cohen S, Doyle WJ, Skoner DP. Psychological stress, cytokine production, and severity of upper respiratory illness. Psychosomatic Medicine. 1999;61:175–180. doi: 10.1097/00006842-199903000-00009. [DOI] [PubMed] [Google Scholar]
- Cohen S, Frank E, Doyle WJ, Skoner DP, Rabin BS, Gwaltney JM., Jr Types of stressors that increase susceptibility to the common cold in healthy adults. Health Psychology. 1998;17:214–223. doi: 10.1037//0278-6133.17.3.214. [DOI] [PubMed] [Google Scholar]
- *Cohen S, Hamrick N, Rodriguez MS, Feldman PJ, Rabin BS, Manuck SB. The stability of and intercorrelations among cardiovascular, immune, endocrine, and psychological reactivity. Annals of Behavioral Medicine. 2000;22:171–197. doi: 10.1007/BF02895111. [DOI] [PubMed] [Google Scholar]
- Cohen S, Herbert TB. Health psychology: Psychological factors and physical disease from the perspective of human psychoneuroimmunology. Annual Review of Psychology. 1996;47:113–142. doi: 10.1146/annurev.psych.47.1.113. [DOI] [PubMed] [Google Scholar]
- Cohen, S., Kessler, R. C., & Underwood, L. G. (1995). Strategies for measuring stress in studies of psychiatric and physical disorders. In S. Cohen, R. C. Kessler, & L. G. Underwood (Eds.), Measuring stress: A guide for health and social scientists (pp. 3–28). New York: Oxford University Press.
- Cohen S, Miller GE, Rabin BS. Psychological stress and antibody response to immunization: A critical review of the human literature. Psychosomatic Medicine. 2001;63:7–18. doi: 10.1097/00006842-200101000-00002. [DOI] [PubMed] [Google Scholar]
- Cohen S, Williamson GM. Stress and infectious disease in humans. Psychological Bulletin. 1991;109:5–24. doi: 10.1037/0033-2909.109.1.5. [DOI] [PubMed] [Google Scholar]
- Cole SW, Kemeny ME, Taylor SE, Visscher BR, Fahey JL. Accelerated course of human immunodeficiency virus infection in gay men who conceal their homosexual identity. Psychosomatic Medicine. 1996;58:219–231. doi: 10.1097/00006842-199605000-00005. [DOI] [PubMed] [Google Scholar]
- Cover H, Irwin M. Immunity and depression: Insomnia, retardation, and reduction of natural killer cell activity. Journal of Behavioral Medicine. 1994;17:217–223. doi: 10.1007/BF01858106. [DOI] [PubMed] [Google Scholar]
- *Cruess S, Antoni M, Kilbourn K, Ironson G, Klimas N, Fletcher MA, et al. Optimism, distress, and immunologic status in HIV-infected gay men following Hurricane Andrew. International Journal of Behavioral Medicine. 2000;7:160–182. [Google Scholar]
- *Cruse JM, Lewis RE, Jr, Bishop GR, Kliesch WF, Gaitan E, Britt R. Decreased immune reactivity and neuroendocrine alterations related to chronic stress in spinal cord injury and stroke patients. Pathobiology. 1993;61:183–192. doi: 10.1159/000163790. [DOI] [PubMed] [Google Scholar]
- *Davidson RJ, Coe CC, Dolski I, Donzella B. Individual differences in prefrontal activation asymmetry predict natural killer cell activity at rest and in response to challenge. Brain, Behavior, and Immunity. 1999;13:93–108. doi: 10.1006/brbi.1999.0557. [DOI] [PubMed] [Google Scholar]
- *de Gucht V, Fischler B, Demanet C. Immune dysfunction associated with chronic professional stress in nurses. Psychiatry Research. 1999;85:105–111. doi: 10.1016/s0165-1781(98)00131-0. [DOI] [PubMed] [Google Scholar]
- *Deinzer R, Kleineidam C, Stiller-Winkler R, Idel H, Bachg D. Prolonged reduction of salivary immunoglobulin A (sIgA) after a major academic exam. International Journal of Psychophysiology. 2000;37:219–232. doi: 10.1016/s0167-8760(99)00112-9. [DOI] [PubMed] [Google Scholar]
- *Deinzer R, Schüller N. Dynamics of stress-related decrease of salivary immunoglobulin A (sIgA): Relationship to symptoms of the common cold and studying behavior. Behavioral Medicine. 1998;23:161–169. doi: 10.1080/08964289809596372. [DOI] [PubMed] [Google Scholar]
- *Dekaris D, Sabioncello A, Mažuran R, Rabatić S, Svoboda-Beusan I, Računica NL, TomašIć J. Multiple changes of immunologic parameters in prisoners of war. Journal of the American Medical Association. 1993;270:595–599. [PubMed] [Google Scholar]
- *Delahanty DL, Dougall AL, Browning LJ, Hyman KB, Baum A. Duration of stressor and natural killer cell activity. Psychology and Health. 1998;13:1121–1134. [Google Scholar]
- *Delahanty DL, Dougall AL, Craig KJ, Jenkins FJ, Baum A. Chronic stress and natural killer cell activity after exposure to traumatic death. Psychosomatic Medicine. 1997;59:467– 476. doi: 10.1097/00006842-199709000-00002. [DOI] [PubMed] [Google Scholar]
- *Delahanty DL, Dougall AL, Hawken L, Trakowski JH, Schmitz JB, Jenkins FJ, Baum A. Time course of natural killer cell activity and lymphocyte proliferation in response to two acute stressors in healthy men. Health Psychology. 1996;15:48–55. doi: 10.1037//0278-6133.15.1.48. [DOI] [PubMed] [Google Scholar]
- *Delahanty DL, Wang T, Maravich C, Forlenza M, Baum A. Time-of-day effects on response of natural killer cells to acute stress in men and women. Health Psychology. 2000;19:39– 45. doi: 10.1037//0278-6133.19.1.39. [DOI] [PubMed] [Google Scholar]
- Dhabhar FS, McEwen BS. Acute stress enhances while chronic stress suppresses cell-mediated immunity in vivo: A potential role for leukocyte trafficking. Brain, Behavior, and Immunity. 1997;11:286–306. doi: 10.1006/brbi.1997.0508. [DOI] [PubMed] [Google Scholar]
- Dhabhar, F. S., & McEwen, B. S. (2001). Bidirectional effects of stress and glucocorticoid hormones on immune function: Possible explanations for paradoxical observations. In R. Ader, D. L. Felten, & N. Cohen (Eds.), Psychoneuroimmunology (3rd ed., pp. 301–338). San Diego, CA: Academic Press.
- *Dimsdale JE, Mills P, Patterson T, Ziegler M, Dillon E. Effects of chronic stress on beta-adrenergic receptors in the homeless. Psychosomatic Medicine. 1994;56:290–295. doi: 10.1097/00006842-199407000-00003. [DOI] [PubMed] [Google Scholar]
- *Dobbin JP, Harth M, McCain GA, Martin RA, Cousin K. Cytokine production and lymphocyte transformation during stress. Brain, Behavior, and Immunity. 1991;5:339–348. doi: 10.1016/0889-1591(91)90029-a. [DOI] [PubMed] [Google Scholar]
- *Dopp JM, Miller GE, Myers HF, Fahey JL. Increased natural killer-cell mobilization and cytotoxicity during marital conflict. Brain, Behavior, and Immunity. 2000;14:10–26. doi: 10.1006/brbi.1999.0567. [DOI] [PubMed] [Google Scholar]
- *Drummond PD, Hewson-Bower B. Increased psychosocial stress and decreased mucosal immunity in children with recurrent upper respiratory tract infections. Journal of Psychosomatic Research. 1997;43:271–278. doi: 10.1016/s0022-3999(97)00002-0. [DOI] [PubMed] [Google Scholar]
- *Dugué B, Leppänen EA, Teppo AM, Fyhrquiist F, Gräsbeck R. Effects of psychological stress on plasma interleukins-1β and 6, C-reactive protein, tumour necrosis factor alpha, anti-diuretic hormone and serum cortisol. Scandinavian Journal of Clinical Lab Investigation. 1993;53:555–561. [PubMed] [Google Scholar]
- Dunlap WP, Cortina JM, Vaslow JB, Burke MJ. Meta-analysis of experiments with matched groups or repeated measures designs. Psychological Methods. 1996;2:170–177. [Google Scholar]
- *Dworsky R, Paganini-Hill A, Ducey B, Hechinger M, Parker JW. Lymphocyte immunophenotyping in an elderly population: Age, sex, and medication effects—A flow cytometry study. Mechanisms of Ageing and Development. 1989;48:255–266. doi: 10.1016/0047-6374(89)90087-0. [DOI] [PubMed] [Google Scholar]
- Effros RB, Boucher N, Porter V, Zhu X, Spaulding C, Walford RL, et al. Decline in CD28+ T cells in centenarians and in long-term T cell cultures: A possible cause for both in vivo and in vitro immunosenescence. Experimental Gerontology. 1994;29:601– 609. doi: 10.1016/0531-5565(94)90073-6. [DOI] [PubMed] [Google Scholar]
- Effros RB, Pawelec G. Replicative senescence of T cells: Does the Hayflick limit lead to immune exhaustion? Immunology Today. 1997;18:450– 454. doi: 10.1016/s0167-5699(97)01079-7. [DOI] [PubMed] [Google Scholar]
- Elliot, G. R., & Eisdorfer, C. (1982). Stress and human health: An analysis and implications of research. A study by the Institute of Medicine, National Academy of Sciences New York: Springer Publishing.
- *Endresen IM, Relling GB, Tønder O, Myking O, Walther BT, Ursin H. Brief uncontrollable stress and psychological parameters influence human plasma concentrations of IgM and complement component C3. Behavioral Medicine. 1991 Winter;:167–176. doi: 10.1080/08964289.1991.9935168. [DOI] [PubMed] [Google Scholar]
- Ershler WB, Keller ET. Age-associated increased interleukin-6 gene expression, late-life diseases, and frailty. Annual Review of Medicine. 2000;51:245–270. doi: 10.1146/annurev.med.51.1.245. [DOI] [PubMed] [Google Scholar]
- *Esterling BA, Kiecolt-Glaser JK, Bodnar JC, Glaser R. Chronic stress, social support, and persistent alterations in the natural killer cell response to cytokines in older adults. Health Psychology. 1994;13:291–298. doi: 10.1037//0278-6133.13.4.291. [DOI] [PubMed] [Google Scholar]
- *Esterling BA, Kiecolt-Glaser JK, Glaser R. Psychosocial modulation of cytokine-induced natural killer cell activity in older adults. Psychosomatic Medicine. 1996;58:264–272. doi: 10.1097/00006842-199605000-00010. [DOI] [PubMed] [Google Scholar]
- *Evans DL, Leserman J, Perkins DO, Stern RA, Murphy C, Tamul K, et al. Stress-associated reductions of cytotoxic T lymphocytes and natural killer cells in asymptomatic HIV infection. American Journal of Psychiatry. 1995;152:543–550. doi: 10.1176/ajp.152.4.543. [DOI] [PubMed] [Google Scholar]
- Felten SY, Felten D. Neural-immune interaction. Progress in Brain Research. 1994;100:157–162. [PubMed] [Google Scholar]
- Ferguson RG, Wikby A, Maxson P, Olsson J, Johansson B. Immune parameters in a longitudinal study of a very old population of Swedish people: A comparison between survivors and nonsurvivors. Journals of Gerontology: Series A: Biological Sciences and Medical Sciences. 1995;50:B378–B382. doi: 10.1093/gerona/50a.6.b378. [DOI] [PubMed] [Google Scholar]
- *Fittschen B, Schultz KH, Schultz A, Raedler A, von Kerekjarto M. Changes of immunological parameters in healthy subjects under examination stress. International Journal of Neuroscience. 1990;51:241–242. doi: 10.3109/00207459008999708. [DOI] [PubMed] [Google Scholar]
- Frankenhauser, M. (1975). Experimental approaches to the study of catecholamines. In L. Levi (Eds.), Emotions—Their parameters and measurement (pp. 209–234). New York: Raven Press.
- Futterman AD, Kemeny ME, Shapiro D, Fahey JL. Immunological and physiological changes associated with induced positive and negative mood. Psychosomatic Medicine. 1994;56:499–511. doi: 10.1097/00006842-199411000-00005. [DOI] [PubMed] [Google Scholar]
- *Geenen R, Godaert GLR, Heijnen CJ, Vianen ME, Wenting MJG, Nederhoff MGJ, Bijlsma JWJ. Experimentally induced stress in rheumatoid arthritis of recent onset: Effects on peripheral blood lymphocytes. Clinical and Experimental Rheumatology. 1998;16:553–559. [PubMed] [Google Scholar]
- *Gennaro S, Fehder WP, Cnaan A, York R, Campbell DE, Gallagher PR, Douglas SD. Immune responses in mothers of term and preterm very-low-birth-weight infants. Clinical and Diagnostic Laboratory Immunology. 1997;4:565–571. doi: 10.1128/cdli.4.5.565-571.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Gennaro S, Fehder W, Nuamah IF, Campbell DE, Douglas SD. Caregiving to very low birthweight infants: A model of stress and immune response. Brain, Behavior, and Immunity. 1997;11:201–215. doi: 10.1006/brbi.1997.0502. [DOI] [PubMed] [Google Scholar]
- *Gerits P, DeBrabander B. Psychosocial predictors of psychological, neurochemical and immunological symptoms of acute stress among breast cancer patients. Psychiatry Research. 1999;85:95–103. doi: 10.1016/s0165-1781(98)00136-x. [DOI] [PubMed] [Google Scholar]
- *Gerritsen W, Heijnen CJ, Wiegant VM, Bermond B, Frijda NH. Experimental social fear: Immunological, hormonal, and autonomic concomitants. Psychosomatic Medicine. 1996;58:273–286. doi: 10.1097/00006842-199605000-00011. [DOI] [PubMed] [Google Scholar]
- *Gilbert DG, Stuckard ME, Jensen RA, Detwiler FRJ, Martinko JM. Effects of exam stress on mood, cortisol, and immune functioning: Influences of neuroticism and smoker–non-smoker status. Personality and Individual Differences. 1996;21:235–246. [Google Scholar]
- *Glaser R, Friedman SB, Smyth J, Ader R, Bijur P, Brunell P, et al. The differential impact of training stress and final examination stress on herpesvirus latency at the United States Military Academy at West Point. Brain, Behavior, and Immunity. 1999;13:240–251. doi: 10.1006/brbi.1999.0566. [DOI] [PubMed] [Google Scholar]
- *Glaser R, Kennedy S, Lafuse WP, Bonneau RH, Speicher C, Hillhouse J, Kiecolt-Glaser JK. Psychological stress-induced modulation of interleukin 2 receptor gene expression and inter-leukin 2 production in peripheral blood leukocytes. Archives of General Psychiatry. 1990;47:707–712. doi: 10.1001/archpsyc.1990.01810200015002. [DOI] [PubMed] [Google Scholar]
- *Glaser R, Kiecolt-Glaser JK. Chronic stress modulates the virus-specific immune response to latent herpes simplex virus type 1. Annals of Behavioral Medicine. 1997;19:78– 82. doi: 10.1007/BF02883323. [DOI] [PubMed] [Google Scholar]
- *Glaser, R., Kiecolt-Glaser, J. K., Malarkey, W. B., & Sheridan, J. F. (1998). The influence of psychological stress on the immune response to vaccines. In S. M. McCann, J. M. Lipton, E. M. Sternberg, G. P. Chrousos, P. W. Gold, & C. C. Smith (Eds.), Annals of the New York Academy of Sciences: Vol. 840. Neuroimmunomodulation: Molecular aspects, integrative systems, and clinical advances (pp. 649– 655). New York: New York Academy of Sciences. [DOI] [PubMed]
- *Glaser R, Kiecolt-Glaser JK, Speicher CE, Holliday JE. Stress, loneliness, and changes in herpesvirus latency. Journal of Behavioral Medicine. 1985;8:249–260. doi: 10.1007/BF00870312. [DOI] [PubMed] [Google Scholar]
- *Glaser R, Kiecolt-Glaser JK, Stout JC, Tarr KL, Speicher CE, Holliday JE. Stress-related impairments in cellular immunity. Psychiatry Research. 1985;16:233–239. doi: 10.1016/0165-1781(85)90111-8. [DOI] [PubMed] [Google Scholar]
- *Glaser R, MacCallum RC, Laskowski BF, Malarkey WB, Sheridan JF, Kiecolt-Glaser JK. Evidence for a shift in the Th-1 to Th-2 cytokine response associated with chronic stress and aging. Journal of Gerontology: Series A: Biological Sciences and Medical Sciences. 2001;56:M477–M482. doi: 10.1093/gerona/56.8.m477. [DOI] [PubMed] [Google Scholar]
- *Glaser R, Mehl VS, Penn G, Speicher CE, Kiecolt-Glaser JK. Stress-associated changes in plasma immunoglobulin levels. International Journal of Psychosomatics. 1986;33:41– 42. [PubMed] [Google Scholar]
- *Glaser R, Pearl DK, Kiecolt-Glaser JK, Malarkey WB. Plasma cortisol levels and reactivation of latent Epstein-Barr Virus in response to examination stress. Psychoneuroendocrinology. 1994;19:765–772. doi: 10.1016/0306-4530(94)90023-x. [DOI] [PubMed] [Google Scholar]
- *Glaser R, Pearson GR, Bonneau RH, Esterling BA, Atkinson C, Kiecolt-Glaser JK. Stress and the memory T-cell response to the Epstein-Barr virus in healthy medical students. Health Psychology. 1993;12:435– 442. doi: 10.1037//0278-6133.12.6.435. [DOI] [PubMed] [Google Scholar]
- *Glaser R, Pearson GR, Jones JF, Hillhouse J, Kennedy S, Mao H, Kiecolt-Glaser JK. Stress-related activation of Epstein-Barr virus. Brain, Behavior, and Immunity. 1991;5:219–232. doi: 10.1016/0889-1591(91)90018-6. [DOI] [PubMed] [Google Scholar]
- *Glaser R, Rice J, Sheridan J, Fertel R, Stout J, Speicher C, et al. Stress-related immune suppression: Health implications. Brain, Behavior, and Immunity. 1987;1:7–20. doi: 10.1016/0889-1591(87)90002-x. [DOI] [PubMed] [Google Scholar]
- *Glaser R, Rice J, Speicher CE, Stout JC, Kiecolt-Glaser JK. Stress depresses interferon production by leukocytes concomitant with a decrease in natural killer cell activity. Behavioral Neuroscience. 1996;100:675– 678. doi: 10.1037//0735-7044.100.5.675. [DOI] [PubMed] [Google Scholar]
- *Glaser R, Sheridan J, Malarkey WB, MacCallum RC, Kiecolt-Glaser JK. Chronic stress modulates the immune response to a pneumococcal pneumonia vaccine. Psychosomatic Medicine. 2000;62:804–807. doi: 10.1097/00006842-200011000-00010. [DOI] [PubMed] [Google Scholar]
- *Goebel MU, Mills PJ. Acute psychological stress and exercise and changes in peripheral leukocyte adhesion molecule expression and density. Psychosomatic Medicine. 2000;62:664– 670. doi: 10.1097/00006842-200009000-00010. [DOI] [PubMed] [Google Scholar]
- *Goebel MU, Mills PJ, Irwin MR, Ziegler MG. Interleukin-6 and tumor necrosis factor-α production after acute psychological stress, exercise, and infused isoproterenol: Differential effects and pathways. Psychosomatic Medicine. 2000;62:591–598. doi: 10.1097/00006842-200007000-00019. [DOI] [PubMed] [Google Scholar]
- *Gomez V, Zimmerman G, Froehlich WD, Knop J. Stress, control experience, acute hormonal and immune reactions. Psychologische Beiräge. 1994;36:74– 81. [Google Scholar]
- *González-Quijano MI, Martín M, Millán S, López-Calderón A. Lymphocyte response to mitogens: Influence of life events and personality. Neuropsychobiology. 1998;38:90–96. doi: 10.1159/000026523. [DOI] [PubMed] [Google Scholar]
- *Goodkin K, Blaney NT, Feaster D, Fletcher MA, Baum MK, Mantero-Atienza E, et al. Active coping style is associated with natural killer cell cytotoxicity in asymptomatic HIV-1 seropositive homosexual men. Journal of Psychosomatic Research. 1992;36:635– 650. doi: 10.1016/0022-3999(92)90053-5. [DOI] [PubMed] [Google Scholar]
- *Goodkin K, Feaster DJ, Tuttle R, Blaney NT, Kumar M, Baum MK, et al. Bereavement is associated with time-dependent decrements in cellular immune function in asymptomatic human immunodeficiency virus type 1-seropositive homosexual men. Clinical Diagnosis and Lab Immunology. 1996;3:109–118. doi: 10.1128/cdli.3.1.109-118.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Goodkin K, Fuchs I, Feaster D, Leeka J, Rishel DD. Life stressors and coping style are associated with immune measures in HIV-1 infection: A preliminary report. International Journal of Psychiatry in Medicine. 1992;22:155–172. doi: 10.2190/BD46-F4JD-K8TW-RUFH. [DOI] [PubMed] [Google Scholar]
- *Graham NMH, Bartholomeusz CA, Taboonpog N, la Brooy JT. Does anxiety reduce the secretion rate of secretory IgA in saliva? Medical Journal of Australia. 1988;148:131–133. doi: 10.5694/j.1326-5377.1988.tb112773.x. [DOI] [PubMed] [Google Scholar]
- *Gruzelier J, Smith F, Nagy A, Henderson D. Cellular and humoral immunity, mood and exam stress: The influences of self-hypnosis and personality predictors. International Journal of Psychophysiology. 2001;42:55–71. doi: 10.1016/s0167-8760(01)00136-2. [DOI] [PubMed] [Google Scholar]
- *Guidi L, Tricerri A, Vangeli M, Frasca D, Errani AR, Di Giovanni A, et al. Neuropeptide Y plasma levels and immunological changes during academic stress. Neuropsychobiology. 1999;40:188–195. doi: 10.1159/000026618. [DOI] [PubMed] [Google Scholar]
- *Halim S, Kaplan HB, Pollack MS. Moderating effects of gender and vulnerability on the relationships between financial hardship, low education and immune response. Stress Medicine. 2000;16:167–177. [Google Scholar]
- *Hall M, Baum A, Buysse DJ, Prigerson HG, Kupfer DJ, Reynolds CF., III Sleep as a mediator of the stress-immune relationship. Psychosomatic Medicine. 1998;60:48–51. doi: 10.1097/00006842-199801000-00011. [DOI] [PubMed] [Google Scholar]
- *Halvorsen R, Vassend O. Effects of examination stress on some cellular immunity functions. Journal of Psychosomatic Research. 1987;31:693–701. doi: 10.1016/0022-3999(87)90018-3. [DOI] [PubMed] [Google Scholar]
- Herbert TB, Cohen S. Stress and immunity in humans: A meta-analytic review. Psychosomatic Medicine. 1993;55:364–379. doi: 10.1097/00006842-199307000-00004. [DOI] [PubMed] [Google Scholar]
- *Herbert TB, Cohen S, Marsland AL, Bachen EA, Rabin BS, Muldoon MF, Manuck SB. Cardiovascular reactivity and the course of immune response to an acute psychological stressor. Psychosomatic Medicine. 1994;56:337–344. doi: 10.1097/00006842-199407000-00009. [DOI] [PubMed] [Google Scholar]
- *Howland LC, Gotrmaker SL, Mofenson LM, Spinp C, Gardner JD, Gorski H, et al. Effects of negative life events on immune suppression in children and youth infected with human immunodeficiency virus type 1. Pediatrics. 2000;106:540–546. doi: 10.1542/peds.106.3.540. [DOI] [PubMed] [Google Scholar]
- *Inoue-Sakurai C, Maruyama S, Morimoto K. Posttraumatic stress and lifestyles are associated with natural killer cell activity in victims of the Hanshin-Awaji earthquake in Japan. Preventive Medicine. 2000;31:467– 473. doi: 10.1006/pmed.2000.0744. [DOI] [PubMed] [Google Scholar]
- *Ironson G, LaPerriere A, Antoni M, O’Hearn P, Schneiderman N, Klimas N, Fletcher MA. Changes in immune and psychological measures as a function of anticipation and reaction to news of HIV-1 antibody status. Psychosomatic Medicine. 1990;52:247–270. doi: 10.1097/00006842-199005000-00001. [DOI] [PubMed] [Google Scholar]
- *Ironson G, Wynings C, Schneiderman N, Baum A, Rodriguez M, Greenwood D, et al. Posttraumatic stress symptoms, intrusive thoughts, loss, and immune function after Hurricane Andrew. Psychosomatic Medicine. 1997;59:128–141. doi: 10.1097/00006842-199703000-00003. [DOI] [PubMed] [Google Scholar]
- *Irwin M, Brown M, Patterson T, Hauger R, Mascovich A, Grant I. Neuropeptide Y and natural killer cell activity: Findings in depression and Alzheimer caregiver stress. Federation of American Societies for Experimental Biology. 1991;5:3100–3107. doi: 10.1096/fasebj.5.15.1743441. [DOI] [PubMed] [Google Scholar]
- *Irwin M, Daniels M, Bloom ET, Smith TL, Weiner H. Life events, depressive symptoms, and immune function. American Journal of Psychiatry. 1987;144:437– 441. doi: 10.1176/ajp.144.4.437. [DOI] [PubMed] [Google Scholar]
- *Irwin M, Daniels M, Bloom ET, Weiner H. Life events, depression, and natural killer cell activity. Psychopharmacology Bulletin. 1986;22:1093–1096. [PubMed] [Google Scholar]
- *Irwin M, Daniels M, Risch SC, Bloom E, Weiner H. Plasma cortisol and natural killer cell activity during bereavement. Biological Psychiatry. 1988;24:173–178. doi: 10.1016/0006-3223(88)90272-7. [DOI] [PubMed] [Google Scholar]
- *Irwin M, Daniels M, Smith TL, Bloom E, Weiner H. Impaired natural killer cell activity during bereavement. Brain, Behavior, and Immunity. 1987;1:98–104. doi: 10.1016/0889-1591(87)90011-0. [DOI] [PubMed] [Google Scholar]
- *Irwin M, Daniels M, Weiner H. Immune and neuroendocrine changes during bereavement. Psychiatric Clinics of North America. 1987;10:449– 465. [PubMed] [Google Scholar]
- *Irwin M, Hauger R, Patterson TL, Semple S, Ziegler M, Grant I. Alzheimer caregiver stress: Basal natural killer cell activity, pituitary-adrenal cortical function, and sympathetic tone. Annals of Behavioral Medicine. 1997;19:83–90. doi: 10.1007/BF02883324. [DOI] [PubMed] [Google Scholar]
- *Irwin M, Patterson T, Smith TL, Caldwell C, Brown SA, Gillin C, Grant I. Reduction of immune function in life stress and depression. Biological Psychiatry. 1990;27:22–30. doi: 10.1016/0006-3223(90)90016-u. [DOI] [PubMed] [Google Scholar]
- Irwin M, Smith TL, Gillin JC. Electroencephalographic sleep and natural killer cell activity in depressed patients and control subjects. Psychosomatic Medicine. 1992;54:10–21. doi: 10.1097/00006842-199201000-00002. [DOI] [PubMed] [Google Scholar]
- *Jabaaij L, Grosheide PM, Heijtink RA, Duivenvoorden HJ, Ballieux RE, Vingerhoets AJJM. Influence of perceived psychological stress and distress on antibody response to low dose rDNA hepatitis B vaccine. Journal of Psychosomatic Research. 1993;37:361–369. doi: 10.1016/0022-3999(93)90138-6. [DOI] [PubMed] [Google Scholar]
- *Jabaaij L, van Hattum J, Vingerhoets AJJM, Oostveen FG, Duivenvoorden HJ, Ballieux RE. Modulation of immune response to rDNA hepatitis B vaccination by psychological stress. Journal of Psychosomatic Research. 1996;41:129–137. doi: 10.1016/0022-3999(96)00123-7. [DOI] [PubMed] [Google Scholar]
- *Jacobs R, Pawlak CR, Mikeska E, Meyer-Olsen D, Martin M, Heijen CJ, et al. Systemic lupus erythematosus and rheumatoid arthritis patients differ from healthy controls in their cytokine pattern after stress exposure. Rheumatology. 2001;40:868– 875. doi: 10.1093/rheumatology/40.8.868. [DOI] [PubMed] [Google Scholar]
- Janeway, C. A., & Travers, P. (1997). Immunobiology: The immune system in health and disease (3rd ed.). New York: Garland.
- *Jemmott JB, III, Borysenko JZ, Borysenko M, McClelland DC, Chapman R, Meyer D, Benson H. June 25). Academic stress, power motivation, and decrease in secretion rate of salivary secretory immunoglobulin A. Lancet. 1983;1:1400–1402. doi: 10.1016/s0140-6736(83)92354-1. [DOI] [PubMed] [Google Scholar]
- *Jemmott JB, III, Magloire K. Academic stress, social support, and secretory immunoglobulin A. Journal of Personality and Social Psychology. 1988;55:803– 810. doi: 10.1037//0022-3514.55.5.803. [DOI] [PubMed] [Google Scholar]
- Jenkins FJ, Baum A. Stress and reactivation of latent herpes simplex virus: A fusion of behavioral medicine and molecular biology. Annals of Behavioral Medicine. 1995;17:116–123. doi: 10.1007/BF02895060. [DOI] [PubMed] [Google Scholar]
- *Jern C, Wadenvik H, Mark H, Hallgren J, Jern S. Haematological changes during acute mental stress. British Journal of Haematology. 1989;71:153–156. doi: 10.1111/j.1365-2141.1989.tb06290.x. [DOI] [PubMed] [Google Scholar]
- *Johnson VC, Walker LG, Heys SD, Whiting PH, Eremin O. Can relaxation training and hypnotherapy modify the immune response to stress, and is hypnotizability relevant? Contemporary Hypnosis. 1996;13:100–108. [Google Scholar]
- Jung W, Irwin M. Reduction of natural killer cell cytotoxic activity in major depression: Interaction between depression and cigarette smoking. Psychosomatic Medicine. 1999;61:263–270. doi: 10.1097/00006842-199905000-00002. [DOI] [PubMed] [Google Scholar]
- *Kamei T, Kumano H, Iwata K, Yasushi M. Influences of long- and short-distance driving on alpha waves and natural killer cell activity. Perceptual and Motor Skills. 1998;87:1419–1423. doi: 10.2466/pms.1998.87.3f.1419. [DOI] [PubMed] [Google Scholar]
- *Kamei T, Kumano H, Masumura S. Changes of immuno-regulatory cells associated with psychological stress and humor. Perceptual and Motor Skills. 1997;84:1296–1298. doi: 10.2466/pms.1997.84.3c.1296. [DOI] [PubMed] [Google Scholar]
- *Kang DH, Coe CL, Karaszewski J, McCarthy DO. Relationship of social support to stress responses and immune function in healthy and asthmatic adolescents. Research in Nursing and Health. 1998;21:117–128. doi: 10.1002/(sici)1098-240x(199804)21:2<117::aid-nur3>3.0.co;2-m. [DOI] [PubMed] [Google Scholar]
- *Kang DH, Coe CL, McCarthy DO. Academic examinations significantly impact immune responses, but not lung function, in healthy and well-managed asthmatic adolescents. Brain, Behavior, and Immunity. 1996;10:164–181. doi: 10.1006/brbi.1996.0015. [DOI] [PubMed] [Google Scholar]
- *Kang DH, Coe CL, McCarthy DO, Ershler WB. Immune responses to final exams in healthy and asthmatic adolescents. Nursing Research. 1997;46:12–19. doi: 10.1097/00006199-199701000-00003. [DOI] [PubMed] [Google Scholar]
- *Kang DH, Fox C. Neuroendocrine and leukocyte responses and pulmonary function to acute stressors. Annals of Behavioral Medicine. 2000;22:276–285. doi: 10.1007/BF02895663. [DOI] [PubMed] [Google Scholar]
- *Kawakami N, Tanigawa T, Araki S, Nakata A, Sakurai S, Yokoyama K, Morita Y. Effects of job strain on helper-inducer (CD4+CD29+) and suppressor-inducer (CD4+CD45RA+) T cells in Japanese blue-collar workers. Psychotherapy and Psychosomatics. 1997;66:192–198. doi: 10.1159/000289134. [DOI] [PubMed] [Google Scholar]
- *Kawamura N, Yoshiharu K, Asukai N. Suppression of cellular immunity in men with a past history of posttraumatic stress disorder. American Journal of Psychiatry. 2001;158:484– 486. doi: 10.1176/appi.ajp.158.3.484. [DOI] [PubMed] [Google Scholar]
- *Kemeny ME, Cohen F, Zegans LS, Conant MA. Psychological and immunological predictors of genital herpes recurrence. Psychosomatic Medicine. 1989;51:195–208. doi: 10.1097/00006842-198903000-00008. [DOI] [PubMed] [Google Scholar]
- Kemeny, M. E., Solomon, G. F., Morley, J. E., & Herbert, T. B. (1992). Psychoneuroimmunology. In C. B. Nemeroff (Ed.), Neuroendocrinology (pp. 563–591). Boca Raton, FL: CRC Press.
- *Kessler RC, Foster C, Joseph J, Ostrow D, Wortman C, Phair J, Chmiel J. Stressful life events and symptom onset in HIV infection. American Journal of Psychiatry. 1991;148:733–738. doi: 10.1176/ajp.148.6.733. [DOI] [PubMed] [Google Scholar]
- Kiecolt-Glaser JK, Cacioppo JT, Malarkey WB, Glaser R. Acute psychological stressors and short-term immune changes: What, why, for whom, and to what extent? Psychosomatic Medicine. 1992;54:680– 685. doi: 10.1097/00006842-199211000-00008. [DOI] [PubMed] [Google Scholar]
- *Kiecolt-Glaser JK, Dura JR, Speicher CE, Trask J, Glaser R. Spousal caregivers of dementia victims: Longitudinal changes in immunity and health. Psychosomatic Medicine. 1991;53:345–362. doi: 10.1097/00006842-199107000-00001. [DOI] [PubMed] [Google Scholar]
- *Kiecolt-Glaser JK, Fisher LD, Ogrocki P, Stout JC, Speicher CE, Glaser R. Marital quality, marital disruption, and immune function. Psychosomatic Medicine. 1987;49:13–34. doi: 10.1097/00006842-198701000-00002. [DOI] [PubMed] [Google Scholar]
- *Kiecolt-Glaser JK, Garner W, Speicher C, Penn GM, Holliday J, Glaser R. Psychosocial modifiers of immunocompetence in medical students. Psychosomatic Medicine. 1994;46:7–14. doi: 10.1097/00006842-198401000-00003. [DOI] [PubMed] [Google Scholar]
- Kiecolt-Glaser JK, Glaser R. Methodological issues in behavioral immunology research with humans. Brain, Behavior, and Immunity. 1988;2:67–78. doi: 10.1016/0889-1591(88)90007-4. [DOI] [PubMed] [Google Scholar]
- *Kiecolt-Glaser JK, Glaser R, Cacioppo JT, MacCallum RC, Snydersmith M, Kim C, Malarkey WB. Marital conflict in older adults: Endocrinological and immunological correlates. Psychosomatic Medicine. 1997;59:339–349. doi: 10.1097/00006842-199707000-00001. [DOI] [PubMed] [Google Scholar]
- *Kiecolt-Glaser JK, Glaser R, Gravenstein S, Malarkey WB, Sheridan J. Chronic stress alters the immune response to influenza virus vaccine in older adults. Proceedings of the National Academy of Sciences, USA. 1996;93:3043–3047. doi: 10.1073/pnas.93.7.3043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Kiecolt-Glaser JK, Glaser R, Shuttleworth EC, Dyer CS, Ogrocki P, Speicher CE. Chronic stress and immunity in family caregivers of Alzheimer’s disease victims. Psychosomatic Medicine. 1987;49:523–535. doi: 10.1097/00006842-198709000-00008. [DOI] [PubMed] [Google Scholar]
- *Kiecolt-Glaser JK, Glaser R, Strain EC, Stout JC, Tarr KL, Holliday JE, Speicher CE. Modulation of cellular immunity in medical students. Journal of Behavioral Medicine. 1986;9:5–21. doi: 10.1007/BF00844640. [DOI] [PubMed] [Google Scholar]
- *Kiecolt-Glaser JK, Kennedy S, Malkoff S, Fisher L, Speicher CE, Glaser R. Marital discord and immunity in males. Psychosomatic Medicine. 1988;50:213–229. doi: 10.1097/00006842-198805000-00001. [DOI] [PubMed] [Google Scholar]
- *Kiecolt-Glaser JK, Malarkey WB, Chee MA, Newton T, Cacioppo JT, Mao HY, Glaser R. Negative behavior during marital conflict is associated with immunological down-regulation. Psychosomatic Medicine. 1993;55:395– 409. doi: 10.1097/00006842-199309000-00001. [DOI] [PubMed] [Google Scholar]
- *Kiecolt-Glaser JK, Marucha PT, Atkinson C, Glaser R. Hypnosis as a modulator of cellular immune dysregulation during acute stress. Journal of Consulting and Clinical Psychology. 2001;69:674– 682. doi: 10.1037//0022-006x.69.4.674. [DOI] [PubMed] [Google Scholar]
- *Kiecolt-Glaser JK, Marucha PT, Malarkey WB, Mercado AM, Glaser R. November 4). Slowing of wound healing by psychological stress. Lancet. 1995;346:1194–1196. doi: 10.1016/s0140-6736(95)92899-5. [DOI] [PubMed] [Google Scholar]
- Kiecolt-Glaser JK, McGuire L, Robles TF, Glaser R. Psychoneuroimmunology and Psychosomatic Medicine: Back to the future. Psychosomatic Medicine. 2002;64:15–18. doi: 10.1097/00006842-200201000-00004. [DOI] [PubMed] [Google Scholar]
- *Kubitz KA, Peavey BS, Moore BS. The effect of daily hassles of humoral immunity: An interaction moderated by locus of control. Biofeedback and Self-Regulation. 1986;11:115–123. doi: 10.1007/BF00999979. [DOI] [PubMed] [Google Scholar]
- *Kugler J, Reintjes F, Tewes V, Schedlowski M. Competition stress in soccer coaches increases salivary immunoglobulin A and salivary cortisol concentration. Journal of Sports Medicine and Physical Fitness. 1996;36:117–120. [PubMed] [Google Scholar]
- Kumar M, Kumar AM, Waldrop D, Antoni MH, Schneiderman N, Eisdorfer C. The HPA axis in HIV-1 infection. Journal of Acquired Immune Deficiency Syndromes. 2002;31(Suppl 2):S89–S93. doi: 10.1097/00126334-200210012-00010. [DOI] [PubMed] [Google Scholar]
- *Kusaka Y, Kondou H, Morimoto K. Healthy lifestyles are associated with higher natural killer cell activity. Preventive Medicine. 1992;21:602– 615. doi: 10.1016/0091-7435(92)90068-s. [DOI] [PubMed] [Google Scholar]
- *Lacey K, Zaharia MD, Griffiths J, Ravindran AV, Merali Z, Anisman H. A prospective study of neuroendocrine and immune alterations associated with the stress of an oral academic examination among graduate students. Psychoneuroendocrinology. 2000;25:339–356. doi: 10.1016/s0306-4530(99)00059-1. [DOI] [PubMed] [Google Scholar]
- Landmann R. Beta-adrenergic receptors in human leukocyte sub-populations. European Journal of Clinical Investigation. 1992;22:30–36. [PubMed] [Google Scholar]
- *Landmann RMA, Müller FB, Perini C, Wesp M, Erne P, Bühler FR. Changes of immunoregulatory cells induced by psychological and physical stress: Relationship to plasma catecholamines. Clinical and Experimental Immunology. 1984;58:127–135. [PMC free article] [PubMed] [Google Scholar]
- *Lane R, Ungerer J, Bernene J, Askenase P. Skin testing and erythrocyte sedimentation rate in women undergoing breast biopsy. International Journal of Psychiatry in Medicine. 1983;13:37– 46. doi: 10.2190/8d35-c4ue-bwd5-kbx2. [DOI] [PubMed] [Google Scholar]
- *Larson MR, Ader R, Moynihan JA. Heart rate, neuroendocrine, and immunological reactivity in response to an acute laboratory stressor. Psychosomatic Medicine. 2001;63:493–501. doi: 10.1097/00006842-200105000-00020. [DOI] [PubMed] [Google Scholar]
- * Lauc, G., Dabelić, S., Dumić, J., & Flögel, M. (1998). Stress and natural killer cell activity in professional soldiers. In P. Csermely (Ed.), Annals of the New York Academy of Sciences: Vol. 851. Stress of life: From molecules to man (pp. 526–530). New York: New York Academy of Sciences. [DOI] [PubMed]
- Laudenslager ML. The psychobiology of loss: Lessons from humans and nonhuman primates. Journal of Social Issues. 1988;44:19–36. [Google Scholar]
- *Laudenslager ML, Aasal R, Adler L, Berger CL, Montgomery PT, Sandberg E, et al. Elevated cytotoxicity in combat veterans with long-term posttraumatic stress disorder: Preliminary observations. Brain, Behavior, and Immunity. 1998;12:74–79. doi: 10.1006/brbi.1997.0513. [DOI] [PubMed] [Google Scholar]
- *Lerman Y, Melamed S, Shragin Y, Kushnir T, Rotgoltz Y, Shirom A, Aronson M. Association between burnout at work and leukocyte adhesiveness/aggregation. Psychosomatic Medicine. 1999;61:828–833. doi: 10.1097/00006842-199911000-00017. [DOI] [PubMed] [Google Scholar]
- *Leserman J, Petitto JM, Perkins DO, Folds JD, Golden RN, Evans DL. Severe stress, depressive symptoms, and changes in lymphocyte subsets in human immunodeficiency virus-infected men. Archives of General Psychiatry. 1997;54:279–285. doi: 10.1001/archpsyc.1997.01830150105015. [DOI] [PubMed] [Google Scholar]
- *Levy SM, Herberman RB, Simons A, Whiteside T, Lee J, McDonald R, Beadle M. Persistently low natural killer cell activity in normal adults: Immunological, hormonal and mood correlates. Natural Immunity and Cell Growth Regulation. 1989;8:173–186. [PubMed] [Google Scholar]
- *Liang SW, Jemerin JM, Tshann JM, Wara DW, Boyce WT. Life events, frontal electroencephalogram laterality, and functional immune status after acute psychological stressors in adolescents. Psychosomatic Medicine. 1997;59:178–186. doi: 10.1097/00006842-199703000-00010. [DOI] [PubMed] [Google Scholar]
- *Linn BS, Linn MW, Klimas NG. Effects of psychophysical stress on surgical outcome. Psychosomatic Medicine. 1988;50:230–244. doi: 10.1097/00006842-198805000-00002. [DOI] [PubMed] [Google Scholar]
- *Linn MW, Linn BS, Jensen J. Stressful events, dysphoric mood, and immune responsiveness. Psychological Reports. 1984;54:219–222. doi: 10.2466/pr0.1984.54.1.219. [DOI] [PubMed] [Google Scholar]
- *Linn MW, Linn BS, Skyler JS, Jensen J. Stress and immune function in diabetes mellitus. Clinical Immunity and Immunopathology. 1983;27:223–233. doi: 10.1016/0090-1229(83)90072-7. [DOI] [PubMed] [Google Scholar]
- *Lowe G, Urquhart J, Greenman J, Lowe G. Academic stress and secretory immunoglobulin A. Psychological Reports. 2000;87:721–722. doi: 10.2466/pr0.2000.87.3.721. [DOI] [PubMed] [Google Scholar]
- Luster AD. Chemokines—Chemotactic cytokines that mediate inflammation. New England Journal of Medicine. 1998;338:436– 445. doi: 10.1056/NEJM199802123380706. [DOI] [PubMed] [Google Scholar]
- *Lutgendorf SK, Antoni MH, Ironson G, Klimas N, Fletcher MA, Schneiderman N. Cognitive processing style, mood, and immune function following HIV seropositivity notification. Cognitive Therapy and Research. 1997;21:157–184. [Google Scholar]
- *Lutgendorf SK, Reimer TT, Harvey JH, Marks G, Hong S-Y, Hillis SL, Lubaroff DM. Effects of housing relocation on immunocompetence and psychosocial functioning in older adults. Journal of Gerontology: Series A: Biological Sciences and Medical Sciences. 2001;56:M97–M105. doi: 10.1093/gerona/56.2.m97. [DOI] [PubMed] [Google Scholar]
- *Lutgendorf SK, Vitaliano PP, Tripp-Reimer T, Harvey JH, Lubaroff DM. Sense of coherence moderated the relationship between life stress and natural killer cell activity in healthy older adults. Psychology and Aging. 1999;14:552–563. doi: 10.1037//0882-7974.14.4.552. [DOI] [PubMed] [Google Scholar]
- Madden, K. S., Thyagarajan, S., & Felten, D. L. (1998). Alterations in sympathetic noradrenergic innervation in lymphoid organs with age. In S. M. McCann, J. M. Lipton, E. M. Sternberg, G. P. Chrousos, P. W. Gold, & C. C. Smith (Eds.), Annals of the New York Academy of Sciences: Vol. 840. Neuroimmunomodulation: Molecular aspects, integrative systems, and clinical advances (pp. 262–268). New York: New York Academy of Sciences. [DOI] [PubMed]
- Maes, M. (1999). Major depression and activation of the inflammatory response system. In R. Dantzer, E. E. Wollman, & R. Yirmiya (Eds.), Cytokines, stress, and depression (pp. 25– 46). New York: Kluwer. [DOI] [PubMed]
- *Maes M, Hendriks D, van Gastel A, Demedts P, Wauters A, Neels H, et al. Effects of psychological stress on serum immunoglobulin, complement and acute phase protein concentrations in normal volunteers. Psychoneuroendocrinology. 1997;22:397– 409. doi: 10.1016/s0306-4530(97)00042-5. [DOI] [PubMed] [Google Scholar]
- *Maes M, Song C, Lin A, de Jongh R, van Gastel A, Kenis G, et al. The effects of psychological stress on humans: Increased production of pro-inflammatory cytokines and a Th1-like response in stress-induced anxiety. Cytokine. 1998;10:313–318. doi: 10.1006/cyto.1997.0290. [DOI] [PubMed] [Google Scholar]
- *Maes M, van Bockstaele DR, van Gastel A, Song C, Schotte C, Neels H, et al. The effects of psychological stress on leukocyte subset distribution in humans: Evidence of immune activation. Neuropsychobiology. 1999;39:1–9. doi: 10.1159/000026552. [DOI] [PubMed] [Google Scholar]
- Maier KJ, Waldstein SR, Synowski SJ. Relation of cognitive appraisal to cardiovascular reactivity, affect, and task engagement. Annals of Behavioral Medicine. 2003;26:32– 41. doi: 10.1207/S15324796ABM2601_05. [DOI] [PubMed] [Google Scholar]
- Maier SF, Watkins LR. Cytokines for psychologists: Implications of bidirectional immune-to-brain communication for understanding behavior, mood, and cognition. Psychological Review. 1998;105:83–107. doi: 10.1037/0033-295x.105.1.83. [DOI] [PubMed] [Google Scholar]
- Maier SF, Watkins LR, Fleshner M. Psychoneuroimmunology: The interface between behavior, brain, and immunity. American Psychologist. 1994;49:1004–1017. doi: 10.1037//0003-066x.49.12.1004. [DOI] [PubMed] [Google Scholar]
- Maisel AS, Fowler P, Rearden A, Motulsky HJ, Michel M. A new method for isolation of human lymphocyte subsets reveals differential regulation of beta-adrenergic receptors by terbutaline treatment. Clinical Pharmacology and Therapeutics. 1989;46:429– 439. doi: 10.1038/clpt.1989.161. [DOI] [PubMed] [Google Scholar]
- *Manuck SB, Cohen S, Rabin BS, Muldoon MF, Bachen EA. Individual differences in cellular immune response to stress. Psychological Science. 1991;2:111–115. [Google Scholar]
- *Marchesi GF, Cotani P, Santone G, DiGuiseppe S, Bartocci C, Montroni M. Psychological and immunological relationships during acute academic stress. New Trends in Experimental and Clinical Psychiatry. 1989;5:5–22. [Google Scholar]
- *Marshall GD, Jr, Agarwall SK, Lloyd C, Cohen L, Henniger EM, Morris GJ. Cytokine dysregulation associated with exam stress in healthy medical students. Brain, Behavior, and Immunity. 1998;12:297–307. doi: 10.1006/brbi.1998.0537. [DOI] [PubMed] [Google Scholar]
- *Marsland AL, Cohen S, Rabin BS, Manuck SB. Associations between stress, trait negative affect, acute immune reactivity, and antibody response to hepatitis B injection in healthy young adults. Health Psychology. 2001;20:4–11. [PubMed] [Google Scholar]
- *Marsland AL, Manuck SB, Fazzari TV, Stewart CJ, Rabin BS. Stability of individual differences in cellular immune responses to acute psychological stress. Psychosomatic Medicine. 1995;57:295–298. doi: 10.1097/00006842-199505000-00012. [DOI] [PubMed] [Google Scholar]
- *Marsland AL, Muldoon MF, Cohen S, Herbert TB, Bachen EA, Patterson S, et al. Lymphocyte subset redistribution during acute laboratory stress in young adults: Mediating effects on hemoconcentration. Health Psychology. 1997;16:341–348. doi: 10.1037//0278-6133.16.4.341. [DOI] [PubMed] [Google Scholar]
- *Martin RA, Dobbin JP. Sense of humor, hassles, and immunoglobulin A: Evidence for a stress-moderating effect of humor. International Journal of Psychiatry in Medicine. 1988;18:93–105. doi: 10.2190/724b-3v06-qc5n-6587. [DOI] [PubMed] [Google Scholar]
- *Marucha PT, Kiecolt-Glaser JK, Favagehi M. Mucosal wound healing is impaired by examination stress. Psychosomatic Medicine. 1998;60:362–365. doi: 10.1097/00006842-199805000-00025. [DOI] [PubMed] [Google Scholar]
- *Matthews KA, Caggiula AR, McAllister CG, Berga SL, Owens JF, Flory JD, Miller AL. Sympathetic reactivity to acute stress and immune response in women. Psychosomatic Medicine. 1995;57:564–571. doi: 10.1097/00006842-199511000-00009. [DOI] [PubMed] [Google Scholar]
- McCleery JM, Bhagwagar Z, Smith KA, Goodwin GM, Cowen PJ. Modelling a loss event: Effect of imagined bereavement on the hypothalamic-pituitary-adrenal axis. Psychological Medicine. 2000;30:219–223. doi: 10.1017/s0033291799001361. [DOI] [PubMed] [Google Scholar]
- *McClelland DC, Alexander C, Marks E. The need for power, stress, immune function, and illness among male prisoners. Journal of Abnormal Psychology. 1982;91:61–70. doi: 10.1037//0021-843x.91.1.61. [DOI] [PubMed] [Google Scholar]
- *McClelland DC, Floor E, Davidson RJ, Saron C. Stressed power motivation, sympathetic activation, immune function, and illness. Journal of Human Stress. 1980;6:11–19. doi: 10.1080/0097840X.1980.9934531. [DOI] [PubMed] [Google Scholar]
- *McClelland DC, Patel V, Brown D, Kelner SP., Jr Spring). The role of affiliative loss in the recruitment of helper cells among insulin-dependent diabetics. Behavioral Medicine. 1991;17:5–14. doi: 10.1080/08964289.1991.9937547. [DOI] [PubMed] [Google Scholar]
- *McClelland DC, Ross G, Patel V. The effects of an academic examination on salivary norepinephrine and immunoglobulin levels. Journal of Human Stress. 1985;11:52–59. doi: 10.1080/0097840X.1985.9936739. [DOI] [PubMed] [Google Scholar]
- *McDade TW. Lifestyle incongruity, social integration, and immune function in Samoan adolescents. Social Science and Medicine. 2001;53:1351–1362. doi: 10.1016/s0277-9536(00)00414-7. [DOI] [PubMed] [Google Scholar]
- *McDade TW, Stallings JF, Angold A, Costello EJ, Burleson M, Cacioppo JT, et al. Epstein-Barr virus antibodies in whole blood spots: A minimally invasive method for assessing an aspect of cell-mediated immunity. Psychosomatic Medicine. 2000;62:560–567. doi: 10.1097/00006842-200007000-00015. [DOI] [PubMed] [Google Scholar]
- *McDonald RD, Yagi K. A note on eosinopenia as an index of psychological stress. Psychosomatic Medicine. 1960;2:149–150. [Google Scholar]
- *McIntosh WA, Kaplan HB, Kubena KS, Landmann WA. Life events, social support, and immune response in elderly individuals. International Journal of Aging and Human Development. 1993;37:23–36. doi: 10.2190/PW8H-A8UA-W2B5-5B2P. [DOI] [PubMed] [Google Scholar]
- *McKinnon W, Weisse CS, Reynolds CP, Bowles CA, Baum A. Chronic stress, leukocyte subpopulations, and humoral response to latent viruses. Health Psychology. 1989;8:389– 402. doi: 10.1037//0278-6133.8.4.389. [DOI] [PubMed] [Google Scholar]
- *McNaughton ME, Smith LW, Patterson TL, Grant I. Stress, social support, coping resources, and immune status in elderly women. Journal of Nervous and Mental Disease. 1990;178:460– 461. doi: 10.1097/00005053-199007000-00010. [DOI] [PubMed] [Google Scholar]
- *Miletic ID, Schiffman SS, Miletic VD, Sattely-Miller EA. Salivary IgA secretion rate in young and elderly persons. Physiology and Behavior. 1996;60:243–248. doi: 10.1016/0031-9384(95)02161-2. [DOI] [PubMed] [Google Scholar]
- Miller GE, Cohen S. Psychological interventions and the immune system: A meta-analytic review and critique. Health Psychology. 2001;20:47– 63. doi: 10.1037//0278-6133.20.1.47. [DOI] [PubMed] [Google Scholar]
- Miller GE, Cohen S, Herbert TB. Pathways linking major depression and immunity in ambulatory female patients. Psychosomatic Medicine. 1999;61:850– 860. doi: 10.1097/00006842-199911000-00021. [DOI] [PubMed] [Google Scholar]
- Miller GE, Cohen S, Ritchey AK. Chronic psychological stress and the regulation of pro-inflammatory cytokines: A glucocorticoid resistance model. Health Psychology. 2002;21:531–541. doi: 10.1037//0278-6133.21.6.531. [DOI] [PubMed] [Google Scholar]
- *Miller GE, Dopp JM, Myers HF, Stevens SY, Fahey JL. Psychosocial predictors of natural killer cell mobilization during marital conflict. Health Psychology. 1999;18:262–271. doi: 10.1037//0278-6133.18.3.262. [DOI] [PubMed] [Google Scholar]
- Miller GE, Stetler CA, Carney RM, Freedland KE, Banks WA. Clinical depression and inflammatory risk markers for coronary heart disease. American Journal of Cardiology. 2002;90:1279–1283. doi: 10.1016/s0002-9149(02)02863-1. [DOI] [PubMed] [Google Scholar]
- *Mills PJ, Berry CC, Dimsdale JE, Ziegler MG, Nelesen RA, Kennedy BP. Lymphocyte subset redistribution in response to acute experimental stress: Effects of gender, ethnicity, hypertension, and the sympathetic nervous system. Brain, Behavior, and Immunity. 1995;9:61– 69. doi: 10.1006/brbi.1995.1006. [DOI] [PubMed] [Google Scholar]
- *Mills PJ, Dimsdale JE. The effects of acute psychological stress on cellular adhesion molecules. Journal of Psychosomatic Research. 1996;41:49–53. doi: 10.1016/0022-3999(96)00051-7. [DOI] [PubMed] [Google Scholar]
- *Mills PJ, Dimsdale JE, Nelesen RA, Dillon E. Psychologic characteristics associated with acute stressor-induced leukocyte subset redistribution. Journal of Psychosomatic Research. 1996;40:417– 423. doi: 10.1016/0022-3999(95)00614-1. [DOI] [PubMed] [Google Scholar]
- *Mills PJ, Haeri SL, Dimsdale JE. Temporal stability of acute stressor-induced changes in cellular immunity. International Journal of Psychophysiology. 1995;19:287–290. doi: 10.1016/0167-8760(95)00012-h. [DOI] [PubMed] [Google Scholar]
- *Mills PJ, Yu H, Ziegler G, Patterson T, Grant I. Vulnerable caregivers of patients with Alzheimer’s disease have a deficit in circulating CD62L− T lymphocytes. Psychosomatic Medicine. 1999;61:168–174. doi: 10.1097/00006842-199903000-00008. [DOI] [PubMed] [Google Scholar]
- *Mills PJ, Ziegler MG, Dimsdale JE, Parry BL. Enumerative immune changes following acute stress: Effect of the menstrual cycle. Brain, Behavior, and Immunity. 1995;9:190–195. doi: 10.1006/brbi.1995.1018. [DOI] [PubMed] [Google Scholar]
- *Mills PJ, Ziegler MG, Patterson T, Dimsdale JE, Hauger R, Irwin M, Grant I. Plasma catecholamine and lymphocyte β2-adrenergic receptor alterations in elderly Alzheimer caregivers under stress. Psychosomatic Medicine. 1997;59:251–256. doi: 10.1097/00006842-199705000-00008. [DOI] [PubMed] [Google Scholar]
- *Mills PJ, Zeigler MG, Rehman J, Maisel AS. Catecholamines, catecholamine receptors, cell adhesion molecules, and acute stressor-related changes in cellular immunity. Advances in Pharmacology. 1998;42:587–590. doi: 10.1016/s1054-3589(08)60819-4. [DOI] [PubMed] [Google Scholar]
- *Mosnaim AD, Wolf ME, Maturana P, Mosnaim G, Puente J, Kucuk O, Gilman-Sachs A. In vitro studies of natural killer cell activity in posttraumatic stress disorder patients: Response to methionine-enkephalin challenge. Immunopharmacology. 1993;25:107–116. doi: 10.1016/0162-3109(93)90014-h. [DOI] [PubMed] [Google Scholar]
- *Moss H, Bose S, Wolters P, Brouwers P. A preliminary study of factors associated with psychological adjustment and disease course in school-age children infected with the human immunodeficiency virus. Journal of Developmental and Behavioral Pediatrics. 1998;19:18–25. doi: 10.1097/00004703-199802000-00003. [DOI] [PubMed] [Google Scholar]
- *Moss RB, Moss HB, Peterson R. Microstress, mood, and natural killer-cell activity. Psychosomatics. 1989;30:279–283. doi: 10.1016/S0033-3182(89)72272-6. [DOI] [PubMed] [Google Scholar]
- *Moyna NM, Bodnar JD, Goldberg HR, Shurin MS, Robertson RJ, Rabin BS. Relation between aerobic fitness level and stress induced alterations in neuroendocrine and immune function. International Journal of Sports Medicine. 1999;20:136–141. doi: 10.1055/s-2007-971107. [DOI] [PubMed] [Google Scholar]
- *Mulder CL, Antoni MH, Duivenvoorden HJ, Kauffmann RH, Goodkin K. Active confrontational coping predicts decreases clinical progression over a one-year period in HIV-infected homosexual men. Journal of Psychosomatic Research. 1995;39:957–965. doi: 10.1016/0022-3999(95)00062-3. [DOI] [PubMed] [Google Scholar]
- *Nagabhushan M, Mathews HL, Witek-Janusek L. Aberrant nuclear expression of AP-1 and NFkB in lymphocytes of women stresses by the experience of breast biopsy. Brain, Behavior, and Immunity. 2001;15:78– 84. doi: 10.1006/brbi.2000.0589. [DOI] [PubMed] [Google Scholar]
- *Nakamura H, Nagase H, Yoshida M, Ogino K. Natural killer (NK) cell activity and NK cell subsets in workers with a tendency of burnout. Journal of Psychosomatic Research. 1999;46:569–578. doi: 10.1016/s0022-3999(99)00009-4. [DOI] [PubMed] [Google Scholar]
- *Nakano Y, Nakamura S, Hirata M, Harada K, Ando K, Tabuchi T, et al. Immune function and lifestyle of taxi drivers in Japan. Industrial Health. 1998;36:32–39. doi: 10.2486/indhealth.36.32. [DOI] [PubMed] [Google Scholar]
- *Nakata A, Araki S, Tanigawa T, Miki A, Sakuri S, Kawakami N, et al. Decrease of suppressor-inducer (CD4+CD45RA) T lymphocytes and increase of serum immunoglobulin G due to perceived job stress in Japanese nuclear electric power plant workers. Journal of Occupational and Environmental Medicine. 2000;42:143–150. doi: 10.1097/00043764-200002000-00007. [DOI] [PubMed] [Google Scholar]
- *Naliboff BD, Benton D, Solomon GF, Morley JE, Fahey JL, Bloom ET, et al. Immunological changes in young and old adults during brief laboratory stress. Psychosomatic Medicine. 1991;53:121–132. doi: 10.1097/00006842-199103000-00002. [DOI] [PubMed] [Google Scholar]
- *Naliboff BD, Solomon GF, Gilmore SL, Benton D, Morley JE, Fahey JL. The effects of the opiate antagonist naloxone on measures of cellular immunity during rest and brief psychological stress. Journal of Psychosomatic Research. 1995;39:345–359. doi: 10.1016/0022-3999(94)00142-r. [DOI] [PubMed] [Google Scholar]
- *Naliboff BD, Solomon GF, Gilmore SL, Fahey JL, Benton D, Pine J. Rapid changes in cellular immunity following a confrontational role-play stressor. Brain, Behavior, and Immunity. 1995;9:207–219. doi: 10.1006/brbi.1995.1020. [DOI] [PubMed] [Google Scholar]
- *Neumann JK, Chi DS. Relationship of church giving to immunological and TxPA stress response. Journal of Psychology and Theology. 1999;27:43–51. [Google Scholar]
- *Neumann JK, Chi DS, Flemming R., II Hematological and immunological acute mental stress responses of people who are severely and profoundly mentally retarded. Research in Developmental Disabilities. 2000;21:347–353. doi: 10.1016/s0891-4222(00)00047-0. [DOI] [PubMed] [Google Scholar]
- *Neumann JK, Quillen JH, Chi DS, Quillen JH. Physiological stress response and psychological differences as a possible function of perceived paternal religious value similarity and church attendance. Journal of Psychology and Christianity. 1998;17:233–247. [Google Scholar]
- *Ockenfels MC, Stierle G, Stone AA, Hellhammer D. The effect of academic examinations on herpes simplex virus-1 (HSV-1) and adenovirus latency. Psychologische Beiräge. 1994;36:61– 68. [Google Scholar]
- *Ohira H, Watanabe Y, Kobayashi K, Kawai M. The type A behavior pattern and immune reactivity to brief stress: Change of volume of secretory immunoglobulin A in saliva. Perceptual and Motor Skills. 1999;89:423– 430. doi: 10.2466/pms.1999.89.2.423. [DOI] [PubMed] [Google Scholar]
- O’Leary A. Stress, emotion, and human immune function. Psychological Bulletin. 1990;108:363–382. doi: 10.1037/0033-2909.108.3.363. [DOI] [PubMed] [Google Scholar]
- *Olff M, Brosschot JF, Godaert G, Benschop RJ, Ballieux RE, Heijnen CJ, et al. Modulatory effects of defense and coping on stress-induced changes in endocrine and immune parameters. International Journal of Behavioral Medicine. 1995;2:85–103. doi: 10.1207/s15327558ijbm0202_1. [DOI] [PubMed] [Google Scholar]
- *Paik IH, Toh KY, Lee C, Kim JJ, Lee SJ. Psychological stress may induce increased humoral and decreased cellular immunity. Behavioral Medicine. 2000;26:139–141. doi: 10.1080/08964280009595761. [DOI] [PubMed] [Google Scholar]
- Papanicoloaou DA, Wilder RL, Manolagas SC, Chrousos GP. The pathophysiologic roles of interleukin-6 in human disease. Annals of Internal Medicine. 1998;128:127–137. doi: 10.7326/0003-4819-128-2-199801150-00009. [DOI] [PubMed] [Google Scholar]
- *Pariante CM, Carpiniello B, Orrù MG, Sitzia R, Piras A, Farci AMG, et al. Chronic caregiving stress alters peripheral blood immune parameters: The role of age and severity of stress. Psychotherapy and Psychosomatics. 1997;66:199–207. doi: 10.1159/000289135. [DOI] [PubMed] [Google Scholar]
- *Patterson TL, Semple SJ, Temoshok LR, Atkinson JH, Mc-Dutchan JA, Straits-Tröster K, et al. Stress and depressive symptoms prospectively predict immune change among HIV-seropositive men. Psychiatry. 1995;58:299–312. doi: 10.1080/00332747.1995.11024735. [DOI] [PubMed] [Google Scholar]
- *Pawlak CR, Jacobs R, Mikeska E, Ochsmann S, Lombardi MS, Kavelaars A, et al. Patients with systemic lupus erythematosus differ from healthy controls in their immunological response to acute psychological stress. Brain, Behavior, and Immunity. 1999;13:287–302. doi: 10.1006/brbi.1999.0553. [DOI] [PubMed] [Google Scholar]
- *Pawlak CR, Mikeska E, Jacobs R, Ochsmann J, Wollenhaupt J, Kavelaars A, et al. Alterations in immunological and endocrine function after acute psychological stress in patients with systemic lupus erythematosus and healthy controls. Psychologische Beiräge. 2000;42:24–32. [Google Scholar]
- *Pehlivanođlu B, Balkanci ZD, Ridvanađaođlu AY, Durmazlar N, Öztürk G, Erbaş D, Okur H. Impact of stress, gender, and menstrual cycle on immune system: Possible role of nitric oxide. Archives of Physiology and Biochemistry. 2001;109:383–387. doi: 10.1076/apab.109.4.383.4234. [DOI] [PubMed] [Google Scholar]
- *Perry S, Fishman B, Jacobsberg L, Frances A. Relationships over 1 year between lymphocyte subsets and psychosocial variables among adults with infection by human immunodeficiency virus. Archives of General Psychiatry. 1992;49:396– 401. doi: 10.1001/archpsyc.1992.01820050060010. [DOI] [PubMed] [Google Scholar]
- *Peters ML, Godaert GLR, Ballieux RE, Brosschot JF, Sweep FCGJ, Swinkels LMJW, et al. Immune responses to experimental stress: Effects of mental effort and uncontrollability. Psychosomatic Medicine. 1999;61:513–524. doi: 10.1097/00006842-199907000-00016. [DOI] [PubMed] [Google Scholar]
- *Petrey LJ, Weems LB, II, Livingstone JN., II Relationship of stress, distress, and the immunologic response to a recombinant hepatitis B vaccine. Journal of Family Practice. 1991;32:481– 486. [PubMed] [Google Scholar]
- *Pettingale KW, Hussein M, Inayat Q, Tee DEH. Changes in immune status following conjugal bereavement. Stress Medicine. 1994;10:145–150. [Google Scholar]
- *Pike JL, Smith TL, Hauger RL, Nicassio PM, Patterson TL, McClintick J, et al. Chronic life stress alters sympathetic, neuroendocrine, and immune responsivity to an acute psychological stressor in humans. Psychosomatic Medicine. 1997;59:447– 457. doi: 10.1097/00006842-199707000-00015. [DOI] [PubMed] [Google Scholar]
- Quan N, Avitsur R, Stark JL, He L, Shah M, Caligiuri M, et al. Social stress increases the susceptibility to endotoxic shock. Journal of Neuroimmunology. 2001;115:36– 45. doi: 10.1016/s0165-5728(01)00273-9. [DOI] [PubMed] [Google Scholar]
- Rabin, B. S. (1999). Stress, immune function, and health: The connection New York: Wiley.
- *Rabkin JG, Williams JBW, Remien RH, Goetz R, Kertzner R, Gorman JM. Depression, distress, lymphocyte subsets, and human immunodeficiency virus symptoms on two occasions in HIV-positive homosexual men. Archives of General Psychiatry. 1991;48:111–119. doi: 10.1001/archpsyc.1991.01810260019002. [DOI] [PubMed] [Google Scholar]
- Raudenbush, S. W. (1994). Random effects models. In H. Cooper & L. V. Hedges (Eds.), The handbook of research synthesis (pp. 301–322). New York: Russell Sage Foundation.
- *Ravindran AV, Griffiths J, Merali Z, Anisman H. Primary dysthymia: A study of several psychosocial, endocrine and immune correlates. Journal of Affective Disorders. 1996;40:73– 84. doi: 10.1016/0165-0327(96)00045-6. [DOI] [PubMed] [Google Scholar]
- *Redwine LS, Altemus M, Leong YM, Carter CS. Lymphocyte responses to stress in postpartum women: Relationship to vagal tone. Psychoneuroendocrinology. 2001;26:241–251. doi: 10.1016/s0306-4530(00)00049-4. [DOI] [PubMed] [Google Scholar]
- *Ring C, Harrison LK, Winzer A, Carroll D, Drayson M, Kendall M. Secretory immunoglobulin A and cardiovascular reactions to mental arithmetic, cold pressor, and exercise: Effects of alpha-adrenergic blockade. Psychophysiology. 2000;37:634– 643. [PubMed] [Google Scholar]
- *Rohleder N, Schommer NC, Hellhammer DH, Engel R, Kirschbaum C. Sex differences in glucocorticoid sensitivity of proinflammatory cytokine production after psychosocial stress. Psychosomatic Medicine. 2001;63:966–972. doi: 10.1097/00006842-200111000-00016. [DOI] [PubMed] [Google Scholar]
- Rosenthal, R. (1991). Meta-analytic procedures for social research. (Rev. ed.) Newbury Park, CA: Sage.
- Rosenthal, R. (1994). Parametric measures of effect size. In H. Cooper & L. V. Hedges (Eds.), The handbook of research synthesis (pp. 231–244). New York: Russell Sage Foundation.
- Rozanski A, Blumenthal JA, Kaplan JR. Impact of psychological factors on the pathogenesis of cardiovascular disease and implications for therapy. Circulation. 1999;99:2192–2217. doi: 10.1161/01.cir.99.16.2192. [DOI] [PubMed] [Google Scholar]
- *Sabioncello A, Kocijan-Hercigonja D, Rabatić S, Tomašić J, Jeren T, Matijević L, et al. Immune, endocrine, and psychological responses in civilians displaced by war. Psychosomatic Medicine. 2000;62:502–508. doi: 10.1097/00006842-200007000-00008. [DOI] [PubMed] [Google Scholar]
- Sapolsky, R. M. (1998). Why zebras don’t get ulcers: An updated guide to stress, stress-related disease, and coping New York: Freeman.
- *Sauer J, Polack E, Wikindki S, Holsboer F, Stalla GK, Arzt E. The glucocorticoid sensitivity of lymphocytes changes according to the activity of the hypothalamus-pituitary-adrenocortical system. Psychoneuroendocrinology. 1995;20:269–280. doi: 10.1016/0306-4530(94)00058-i. [DOI] [PubMed] [Google Scholar]
- *Scanlan JM, Vitaliano PP, Ochs H, Savage MV, Borson S. CD4 and CD8 counts are associated with interactions of gender and psychosocial stress. Psychosomatic Medicine. 1998;60:644– 653. doi: 10.1097/00006842-199809000-00023. [DOI] [PubMed] [Google Scholar]
- *Schaubroeck J, Jones JR, Xie JL. Individual differences in utilizing control to cope with job demands: Effects on susceptibility to infectious disease. Journal of Applied Social Psychology. 2001;86:265–278. doi: 10.1037/0021-9010.86.2.265. [DOI] [PubMed] [Google Scholar]
- *Schedlowski M, Jacobs R, Alker J, Pröhl F, Stratmann G, Richter S, et al. Psychophysiological, neuroendocrine and cellular immune reactions under psychological stress. Neuropsychobiology. 1993;28:87–90. doi: 10.1159/000119006. [DOI] [PubMed] [Google Scholar]
- *Schedlowski M, Jacobs R, Stratmann G, Richter S, Hadicke A, Tewes U, et al. Changes of natural killer cells during acute psychological stress. Journal of Clinical Immunology. 1993;13:119–126. doi: 10.1007/BF00919268. [DOI] [PubMed] [Google Scholar]
- *Schlesinger M, Yodfat Y. Effect of psychosocial stress on natural killer cell activity. Cancer Detection and Prevention. 1988;12:9–14. [PubMed] [Google Scholar]
- *Schlesinger M, Yodfat Y. The impact of stressful life events on natural killer cells. Stress Medicine. 1991;7:53– 60. [Google Scholar]
- *Schmid-Ott G, Jacobs R, Jäger B, Klages S, Wolf J, Werfel T, et al. Stress-induced endocrine and immunological changes in psoriasis patients and healthy controls. Psychotherapy and Psychosomatics. 1998;67:37– 42. doi: 10.1159/000012257. [DOI] [PubMed] [Google Scholar]
- *Schmid-Ott G, Jaeger B, Adamek C, Koch H, Lamprecht F, Kapp A, Werfel T. Levels of circulating CD8+ T lymphocytes, natural killer cells, and eosinophils increase upon acute psychosocial stress in patients with atopic dermatitis. Journal of Allergy and Clinical Immunology. 2001;107:171–177. doi: 10.1067/mai.2001.111850. [DOI] [PubMed] [Google Scholar]
- *Segerstrom SC. Optimism, goal conflict, and stressor-related immune change. Journal of Behavioral Medicine. 2001;24:441– 467. doi: 10.1023/a:1012271410485. [DOI] [PubMed] [Google Scholar]
- *Segerstrom SC, Taylor SE, Kemeny ME, Fahey JL. Optimism is associated with mood, coping, and immune change in response to stress. Journal of Personality and Social Psychology. 1998;74:1646–1655. doi: 10.1037//0022-3514.74.6.1646. [DOI] [PubMed] [Google Scholar]
- Selye, H. (1975). The stress of life New York: McGraw-Hill.
- *Sgoutas-Emch SA, Cacioppo JT, Uchino BN, Malarkey W, Pearl D, Kiecolt-Glaser JK, Glaser R. The effects of an acute psychological stressor on cardiovascular, endocrine, and cellular immune response: A prospective study of individuals high and low in heart rate reactivity. Psychophysiology. 1994;31:264–271. doi: 10.1111/j.1469-8986.1994.tb02215.x. [DOI] [PubMed] [Google Scholar]
- Shadish, W. R., & Haddock, C. K. (1994). Combining estimates of effect size. In H. Cooper & L. V. Hedges (Eds.), The handbook of research synthesis (pp. 261–281). New York: Russell Sage Foundation.
- Shavit Y, Terman GW, Martin FC, Lewis JW, Liebeskind JC, Gale RP. Stress, opioid peptides, the immune system, and cancer. Journal of Immunology. 1985;135(Suppl 2):834s– 837s. [PubMed] [Google Scholar]
- *Shea J, Clover K, Burton R. Relationships between measures of acute and chronic stress and cellular immunity. Medical Science Research. 1991;19:221–222. [Google Scholar]
- Sheridan, J. F., Dobbs, C. M., Jung, J., Chu, X., Konstantinos, A., Padgett, D. A., & Glaser, R. (1998). Stress-induced neuroendocrine modulation of viral pathogenesis and immunity. In S. M. McCann, J. M. Lipton, E. M. Sternberg, G. P. Chrousos, P. W. Gold, & C. C. Smith (Eds.), Annals of the New York Academy of Sciences: Vol. 840. Neuroimmunomodulation: Molecular aspects, integrative systems, and clinical advances (pp. 803– 808). New York: New York Academy of Sciences. [DOI] [PMC free article] [PubMed]
- *Sieber WJ, Rodin J, Larson L, Ortega S, Cummings N, Levy S, et al. Modulation of human natural killer cell activity by exposure to uncontrollable stress. Brain, Behavior, and Immunity. 1992;6:141–156. doi: 10.1016/0889-1591(92)90014-f. [DOI] [PubMed] [Google Scholar]
- *Söderfeldt M, Söderfeldt B, Ohlson CG, Theorell T, Jones I. The impact of sense of coherence and high-demand/low-control job environment on self-reported health, burnout and psychophysiological stress indicators. Work & Stress. 2000;14:1–15. [Google Scholar]
- *Solomon GF, Segerstrom SC, Grohr P, Kemeny M, Fahey J. Shaking up immunity: Psychological and immunologic changes after a natural disaster. Psychosomatic Medicine. 1997;59:114–127. doi: 10.1097/00006842-199703000-00002. [DOI] [PubMed] [Google Scholar]
- *Song C, Kenis G, van Gastel A, Bosmans E, Lin A, de Jong R, et al. Influence of psychological stress on immuneinflammatory variables in normal humans. Part II. Altered serum concentrations of natural anti-inflammatory agents and soluble membrane antigens of monocytes and T lymphocytes. Psychiatry Research. 1999;85:293–303. doi: 10.1016/s0165-1781(99)00012-8. [DOI] [PubMed] [Google Scholar]
- *Spangler G. Psychological and physiological responses during an exam and their relation to personality characteristics. Psychoneuroendocrinology. 1997;22:423– 441. doi: 10.1016/s0306-4530(97)00040-1. [DOI] [PubMed] [Google Scholar]
- *Spivak B, Shohat B, Mester R, Avraham S, Gil-Ad I, Bleich A, et al. Elevated levels of serum interleukin-1β in combat-related posttraumatic stress disorder. Biological Psychiatry. 1997;42:345–348. doi: 10.1016/S0006-3223(96)00375-7. [DOI] [PubMed] [Google Scholar]
- *Spratt ML, Denney DR. Immune variables, depression, and plasma cortisol over time in suddenly bereaved parents. Journal of Neuropsychiatry and Clinical Neurosciences. 1991;3:299–306. doi: 10.1176/jnp.3.3.299. [DOI] [PubMed] [Google Scholar]
- Stone AA, Schwartz J, Smyth J, Kirschbaum C, Cohen S, Hell-hammer D, Grossman S. Individual differences in the diurnal cycle of salivary free cortisol: A replication of flattened cycles for some individuals. Psychoneuroendocrinology. 2001;26:295–306. doi: 10.1016/s0306-4530(00)00057-3. [DOI] [PubMed] [Google Scholar]
- *Stone AA, Valdimarsdottir HB, Katkin ES, Burns J, Cox DS, Lee S, et al. Effects of mental stressors on mitogen-induced lymphocyte responses in the laboratory. Psychology and Health. 1993;8:269–284. [Google Scholar]
- *Stowell JR, Kiecolt-Glaser JK, Glaser R. Perceived stress and cellular immunity: When coping counts. Journal of Behavioral Medicine. 2001;24:323–339. doi: 10.1023/a:1010630801589. [DOI] [PubMed] [Google Scholar]
- *Theorell T, Orth-Gomér K, Eneroth P. Slow-reacting immunoglobulin in relation to social support and changes in job strain: A preliminary note. Psychosomatic Medicine. 1990;52:511–516. doi: 10.1097/00006842-199009000-00003. [DOI] [PubMed] [Google Scholar]
- *Thomason B, Jones G, McClure J, Brantley P. Psychosocial co-factors in HIV illness: An empirically-based model. Psychology and Health. 1996;11:385–393. [Google Scholar]
- *Thornton S, Troop M, Burgess AP, Button J, Goodall R, Flynn R, et al. The relationship of psychological variables and disease progression among long-term HIV-infected men. International Journal of STD & AIDS. 2000;11:734–742. doi: 10.1258/0956462001915165. [DOI] [PubMed] [Google Scholar]
- *Tjemsland L, Søreide JA, Matre R, Malt UF. Preoperative psychological variables predict immunological status in patients with operable breast cancer. Psycho-Oncology. 1997;6:311–320. doi: 10.1002/(SICI)1099-1611(199712)6:4<311::AID-PON285>3.0.CO;2-C. [DOI] [PubMed] [Google Scholar]
- Tomaka J, Blascovich J, Kibler J, Ernst JM. Cognitive and physiological antecedents of threat and challenge appraisal. Journal of Personality and Social Psychology. 1997;73:63–72. doi: 10.1037//0022-3514.73.1.63. [DOI] [PubMed] [Google Scholar]
- *Tsopanakis C, Tsopanakis A. Stress hormonal factors, fatigue, and antioxidant responses to prolonged speed driving. Pharmacology, Biochemistry and Behavior. 1998;60:747–751. doi: 10.1016/s0091-3057(98)00037-9. [DOI] [PubMed] [Google Scholar]
- *Uchakin PN, Tobin B, Cubbage M, Marshall G, Jr, Sams C. Immune responsiveness following academic stress in first-year medical students. Journal of Interferon and Cytokine Research. 2001;21:687– 694. doi: 10.1089/107999001753124426. [DOI] [PubMed] [Google Scholar]
- *Uchino BN, Cacioppo JT, Malarkey W, Glaser R. Individual differences in cardiac sympathetic control predict endocrine and immune responses to acute psychological stress. Journal of Personality and Social Psychology. 1995;69:736–743. doi: 10.1037//0022-3514.69.4.736. [DOI] [PubMed] [Google Scholar]
- *Udelman DL. Stress and immunity. Psychotherapy and Psychosomatics. 1982;37:176–184. doi: 10.1159/000287570. [DOI] [PubMed] [Google Scholar]
- *Værnes RJ, Myhre G, Aas H, Homnes T, Hansen I, Tønder O. Relationships between stress, psychological factors, health, and immune levels among military aviators. Work & Stress. 1991;5:5–16. [Google Scholar]
- *Van der Pompe G, Antoni MH, Duivenvoorden HJ, Heijnen CJ. Relations of plasma ACTH and cortisol levels with the distribution and function of peripheral blood cells in response to a behavioral challenge in breast cancer: An empirical exploration by means of statistical modeling. International Journal of Behavioral Medicine. 1997;4:145–169. doi: 10.1207/s15327558ijbm0402_4. [DOI] [PubMed] [Google Scholar]
- *Van der Pompe G, Antoni MH, Visser A, Heijnen CJ. Effect of mild acute stress on immune cell distribution and natural killer cell activity in breast cancer patients. Biological Psychology. 1998;48:21–35. doi: 10.1016/s0301-0511(98)00002-7. [DOI] [PubMed] [Google Scholar]
- *Van der Voort CR, Heijnen CJ, Wulffraat N, Kuis W, Kavelaars A. Stress induces increases in IL-6 production by leucocytes of patients with the chronic inflammatory disease juvenile rheumatoid arthritis: A putative role for α1-adrenergic receptors. Journal of Neuroimmunology. 2000;110:223–229. doi: 10.1016/s0165-5728(00)00328-3. [DOI] [PubMed] [Google Scholar]
- *Van Rood Y, Goulmy E, Blokland E, Pool J, van Rood J, van Houwelingen H. Stress related changes in immunological and psychological variables induced by the preparation and defense of a PhD-thesis. Psychology and Health. 1995;10:229–244. [Google Scholar]
- *Vassend O, Halvorsen R. Personality, examination stress, and serum concentrations of immunoglobulins. Scandinavian Journal of Psychology. 1987;28:233–241. doi: 10.1111/j.1467-9450.1987.tb00760.x. [DOI] [PubMed] [Google Scholar]
- *Vedhara K, Cox NKM, Wilcock GK, Perks P, Hunt M, Anderson S, et al. February 20). Chronic stress in elderly carers of dementia patients and antibody response to influenza vaccination. Lancet. 1999;353:627– 631. doi: 10.1016/S0140-6736(98)06098-X. [DOI] [PubMed] [Google Scholar]
- *Vedhara K, Nott K. The assessment of the emotional and immunological consequences of examination stress. Journal of Behavioral Medicine. 1996;19:467– 478. doi: 10.1007/BF01857679. [DOI] [PubMed] [Google Scholar]
- *Vialettes B, Ozanon JP, Kaplansky S, Farnarier C, Sauvaget E, Lassmann-Vague V, et al. Stress antecedents and immune status in recently diagnosed type 1 (insulin dependent) diabetes mellitus. Diabete & Metabolisme. 1989;15:45–50. [PubMed] [Google Scholar]
- *Vitaliano PP, Scanlan JM, Ochs HD, Syrjala K, Siegler IC, Snyder EA. Psychosocial stress moderates the relationship of cancer history with natural killer cell activity. Annals of Behavioral Medicine. 1998;20:199–208. doi: 10.1007/BF02884961. [DOI] [PubMed] [Google Scholar]
- *Wadee AA, Kuschke RH, Kometz S, Berk M. Personality factors, stress, and immunity. Stress and Health. 2001;17:25– 40. [Google Scholar]
- *Wang T, Delahanty DL, Dougall AL, Baum A. Responses of natural killer cell activity to acute laboratory stressors in healthy men at different times of day. Health Psychology. 1998;17:428– 435. doi: 10.1037//0278-6133.17.5.428. [DOI] [PubMed] [Google Scholar]
- *Watson PB, Muller HK, Jones IH, Bradley AJ. Cell-mediated immunity in combat veterans with posttraumatic stress disorder. Medical Journal of Australia. 1983;159:513–515. doi: 10.5694/j.1326-5377.1993.tb138003.x. [DOI] [PubMed] [Google Scholar]
- Wayne SJ, Rhyne RL, Garry PJ, Goodwin JS. Cell-mediated immunity as a predictor of morbidity and mortality in subjects over 60. Journals of Gerontology: Series A: Biological Sciences and Medical Sciences. 1990;45:M45–M48. doi: 10.1093/geronj/45.2.m45. [DOI] [PubMed] [Google Scholar]
- *Weiss DW, Hirt R, Tarcic N, Berzon Y, Ben-Zur H, Breznitz S, et al. Studies in psychoneuroimmunology: Psychological, immunological, and neuroendocrinological parameters in Israeli civilians during and after a period of Scud missile attacks. Behavioral Medicine. 1996;22:5–14. doi: 10.1080/08964289.1996.9933760. [DOI] [PubMed] [Google Scholar]
- *Weisse CS, Pato CN, McAllister CG, Littman R, Breier A, Paul SM, Baum A. Differential effects of controllable and uncontrollable acute stress on lymphocyte proliferation and leukocyte percentages in humans. Brain, Behavior, and Immunity. 1990;4:339–351. doi: 10.1016/0889-1591(90)90037-q. [DOI] [PubMed] [Google Scholar]
- *Whitehouse WG, Dinges DF, Orne EC, Keller SE, Bates BL, Bauer NK, et al. Psychosocial and immune effects of self-hypnosis for stress management throughout the first semester of medical school. Psychosomatic Medicine. 1996;58:249–263. doi: 10.1097/00006842-199605000-00009. [DOI] [PubMed] [Google Scholar]
- Wikby A, Johansson B, Ferguson F, Olsson J. Age-related changes in immune parameters in a very old population of Swedish people: A longitudinal study. Experimental Gerontology. 1994;29:531–541. doi: 10.1016/0531-5565(94)90036-1. [DOI] [PubMed] [Google Scholar]
- *Wilcox S, King AC, Vitaliano PP, Brassington GS. Anger expression and natural killer cell activity in family caregivers participating in a physical activity trial. Journal of Health Psychology. 2000;5:431– 440. doi: 10.1177/135910530000500403. [DOI] [PubMed] [Google Scholar]
- *Willemsen G, Ring C, Carroll D, Evans P, Clow A, Hucklebridge F. Secretory immunoglobulin A and cardiovascular reactions to mental arithmetic and cold pressor. Psychophysiology. 1998;35:252–259. [PubMed] [Google Scholar]
- Williams, N. A., & Leaper, D. J. (1998). Infection. In D. J. Leaper & K. G. Harding (Eds.), Wounds: Biology and management (pp. 71– 87). New York: Oxford University Press.
- *Wilson SN, van der Kolk B, Burbridge J, Fisler R, Kradin R. Phenotype of blood lymphocytes in PTSD suggests chronic immune activation. Psychosomatics. 1999;40:222–225. doi: 10.1016/S0033-3182(99)71238-7. [DOI] [PubMed] [Google Scholar]
- *Winzer A, Ring C, Carroll D, Willemsen G, Drayson M, Kendall M. Secretory immunoglobulin A and cardiovascular reactions to mental arithmetic, cold pressor, and exercise: Effects of beta-adrenergic blockade. Psychophysiology. 1999;36:591– 601. [PubMed] [Google Scholar]
- *Wolf TM, Cole B, Fahrion S, Norris P, Coyne L. Age and sex modulate effects of stress on the immune system: A multivariate analysis. International Journal of Neuroscience. 1994;79:121–132. doi: 10.3109/00207459408986073. [DOI] [PubMed] [Google Scholar]
- *Workman EA, La Via MF. T-lymphocyte polyclonal proliferation: Effects of stress and stress response style on medical students taking national board examinations. Clinical Immunology and Immunopathology. 1987;43:308–313. doi: 10.1016/0090-1229(87)90140-1. [DOI] [PubMed] [Google Scholar]
- Yehuda R. Biology of posttraumatic stress disorder. Journal of Clinical Psychiatry. 2001;62:41– 46. [PubMed] [Google Scholar]
- Yehuda R, McFarlane AC, Shalev AY. Predicting the development of posttraumatic stress disorder from the acute response to a traumatic event. Biological Psychiatry. 1998;44:1305–1313. doi: 10.1016/s0006-3223(98)00276-5. [DOI] [PubMed] [Google Scholar]
- *Zakowski SG. The effects of stressor predictability on lymphocyte proliferation in humans. Psychology and Health. 1995;10:409– 425. [Google Scholar]
- *Zakowski SG, Cohen L, Hall MH, Wollman K, Baum A. Differential effects of active and passive laboratory stressors on immune function in healthy men. International Journal of Behavioral Medicine. 1994;1:163–184. doi: 10.1207/s15327558ijbm0102_4. [DOI] [PubMed] [Google Scholar]
- *Zakowski SG, McAllister CG, Deal M, Baum A. Stress, reactivity, and immune function in healthy men. Health Psychology. 1992;11:223–232. doi: 10.1037//0278-6133.11.4.223. [DOI] [PubMed] [Google Scholar]
- *Zautra AJ, Okun MA, Robinson SE, Lee D, Roth SH, Emmanual J. Life stress and lymphocyte alterations among patients with rheumatoid arthritis. Health Psychology. 1989;8:1–14. doi: 10.1037//0278-6133.8.1.1. [DOI] [PubMed] [Google Scholar]
- *Zeier H, Brauchli P, Joller-Jemelka HI. Effects of work demands on immunoglobulin A and cortisol in air traffic controllers. Biological Psychology. 1996;42:413– 423. doi: 10.1016/0301-0511(95)05170-8. [DOI] [PubMed] [Google Scholar]
- *Zisook S, Shuchter SR, Irwin M, Darko DF, Sledge P, Resivsky K. Bereavement, depression, and immune function. Psychiatry Research. 1994;52:1–10. doi: 10.1016/0165-1781(94)90114-7. [DOI] [PubMed] [Google Scholar]
- Zorrilla EP, Luborsky L, McKay JR, Rosenthal R, Houldin A, Tax A, et al. The relationship of depression and stressors to immunological assays: A meta-analytic review. Brain, Behavior, and Immunity. 2001;15:199–226. doi: 10.1006/brbi.2000.0597. [DOI] [PubMed] [Google Scholar]


