Abstract
Although recent evidence has confirmed the importance of cytotoxic T-lymphocyte (CTL) responses in controlling human immunodeficiency virus type 1 and simian immunodeficiency virus replication, the relevance of the epitopic breadth of those CTL responses remains unexplored. In the present study, we sought to determine whether vaccination can expand CTL populations which recognize a repertoire of viral epitopes that is greater than is typically generated in the course of a viral infection. We demonstrate that potent secondary CTL responses to subdominant epitopes are rapidly generated following a pathogenic simian-human immunodeficiency virus challenge of rhesus monkeys vaccinated with plasmid DNA or recombinant modified vaccinia virus Ankara vaccines. These data indicate that prior vaccination can increase the breadth of the CTL response that evolves after an AIDS virus infection.
Recent studies have demonstrated the critical role of virus-specific cytotoxic T-lymphocyte (CTL) responses in controlling human immunodeficiency virus type 1 (HIV-1) replication in humans and simian immunodeficiency virus (SIV) replication in rhesus monkeys (12, 16, 21). Candidate AIDS vaccines that elicit potent CTL responses are therefore being developed. In fact, the central importance of CTL in the immune containment of HIV-1 and SIV replication is underscored by the recent demonstration that a simian-human immunodeficiency virus (SHIV) can escape from containment by a vaccine-elicited immune response through the mutation of a single dominant CTL epitope (5). This finding also suggests that a CTL response with significant epitopic breadth may be needed in vaccinated individuals following viral challenge to minimize the likelihood of such eventual vaccine failures.
In preclinical AIDS vaccine studies in nonhuman primates, CTLs in the peripheral blood of vaccinated animals are typically assessed prior to viral challenge. It is likely, however, that the CTL populations relevant for the control of viral replication are not those effector cells circulating at the time of viral exposure, since there is no evidence that effector CTLs can protect against the initial establishment of a viral infection. The important CTLs are probably those that expand in the infected individual from memory CD8+ T lymphocytes during the period of primary infection. These expanding populations of effector cells limit the spread of virus during the early days following infection. In fact, a vaccine may not elicit a particularly potent primary effector CTL response but may generate a substantial memory CTL population that can rapidly expand following exposure to replicating virus. It is therefore important to know the potential of HIV-1 vaccine candidates to elicit memory CTLs specific for a diversity of epitopes that can expand following infection.
CTLs have been implicated in containing AIDS virus replication during two distinct phases of infection. First, they have been shown to contain the early burst of viral replication in infected individuals during the period of primary infection (13). Second, they have been shown to contain ongoing, chronic viral replication (5, 16, 17, 21). A vaccine-elicited memory CTL population might expand rapidly enough following initial infection to limit early viral spread and establish a low set-point level of chronic viral replication. It is also possible that vaccine-elicited memory CTL may expand to a sizeable population too late to contribute to containing early viral spread. Such a late-expanded CTL population may, nevertheless, contribute to the long-term control of chronic viral replication. It will therefore be important to characterize the kinetics of the emergence of effector CTL populations in vaccinated individuals following exposure to replicating virus to determine how a vaccine-elicited immune response may contribute to the control of virus spread.
The natural bias of antiviral immune responses focuses CTL recognition on a limited number of immunodominant epitopes (23). An understanding of this bias has led a number of laboratories to develop AIDS vaccine candidates that elicit CTL responses specific for limited numbers of immunodominant viral epitopes (2, 10, 11, 22). The rationale for pursuing this strategy is that such vaccines will focus the immune response on the biologically relevant viral epitopes. However, virus-specific CTLs that recognize many subdominant epitopes in addition to these limited number of dominant epitopes develop in infected individuals. It has been argued that a CTL response which recognizes a diversity of viral epitopes will decrease the chance that viral mutations that escape from CTL recognition will develop (5).
We have previously shown that plasmid DNA vaccination of rhesus monkeys elicits reproducible high-frequency CTL responses specific for both dominant and subdominant epitopes, with each dominant or subdominant epitope-specific response constituting 0.1 to 0.5% peripheral CD8+ T cells (4). In contrast, recombinant modified vaccinia virus Ankara (rMVA) vaccination elicited high-frequency CTL responses to dominant epitopes (0.1 to 0.4%), but responses to subdominant epitopes were of a substantially lower frequency (0.0 to 0.1%). These findings, however, did not address the issue of whether the subdominant CTL responses could expand in DNA- and rMVA-vaccinated monkeys following exposure to replicating virus or whether they have functional significance. Here we report that robust CTL responses specific for subdominant epitopes develop in both DNA- and rMVA-vaccinated monkeys but not in control animals following a pathogenic viral challenge. The rapid kinetics of the emergence of these secondary CTL responses specific for subdominant epitopes, as well as their persistence following infection, suggests that they may contribute to protection against viral replication both during the period of primary infection and in the setting of chronic infection.
Groups of rhesus monkeys expressing the major histocompatibility complex class I allele Mamu-A*01 were selected for this study. By studying monkeys that expressed this major histocompatibility complex class I allele, we were able to monitor the emergence of CTL responses specific for well-defined dominant and subdominant Mamu-A*01-restricted SIV and HIV epitopes (1, 8, 15). The monkeys were vaccinated with sham plasmid DNA (n = 4) or DNA vaccines expressing SIVmac239 Gag and HIV-1 89.6P Env (n = 3) at weeks 0, 4, 8, and 40 (6, 7). At weeks 0 and 4, certain monkeys also received interleukin-2/immunoglobulin (IL-2/Ig) plasmid (n = 4). At week 46, all monkeys were challenged with 100 50% monkey infective doses (MID50) of SHIV-89.6P by the intravenous route (18, 19). These animals were a subpopulation of a previously described larger group of vaccinated and challenged monkeys (6). Following viral challenge, we monitored CTL responses specific for the Mamu-A*01-restricted immunodominant SIV Gag p11C epitope (CTPYDINQM) (1, 15) as well as the Mamu-A*01-restricted subdominant HIV-1 Env p41A (YAPPISGQI) and SIV Pol p68A (STPPLVRLV) epitopes (8). CTL responses were assessed by staining freshly isolated peripheral blood mononuclear cells (PBMC) with fluorochrome-labeled Mamu-A*01/peptide tetramer complexes followed by flow cytometric analysis (3, 15), staining PBMC following peptide stimulation in culture with these tetramers, and performing standard chromium release cytotoxicity assays. One microgram of phycoerythrin-labeled tetrameric Mamu-A*01/p11C, Mamu-A*01/p41A, or Mamu-A*01/p68A complexes in conjunction with fluorescein isothiocyanate-labeled anti-human CD8α (Leu2a; Becton Dickinson), ECD-labeled anti-human CD8αβ (2ST8-5H7; Beckman Coulter), and allophycocyanin-labeled anti-rhesus CD3 (FN18) monoclonal antibodies (MAbs) were used to stain p11C-, p41A-, or p68A-specific CD8+ T cells as described previously (8, 14). For staining of freshly isolated PBMC, 100 μl of whole blood from both vaccinated and control monkeys was directly stained with these reagents, lysed on an Immunoprep Reagent Q-Prep Workstation (Coulter), washed in 3 ml of phosphate-buffered saline, and fixed in 0.5 ml of phosphate-buffered saline containing 1.5% paraformaldehyde.
Alternatively, peripheral blood lymphocytes (PBL) from rhesus monkeys were isolated and washed in Hanks' balanced salt solution containing 2% fetal calf serum (FCS). PBL (5 × 106) in 2 ml of RPMI 1640 medium containing 12% FCS (R12) were cultured in the presence of 1-μg/ml concentrations of SIV Gag p11C (CTPYDINQM), HIV-1 Env p41A (YAPPISGQI), or SIV Pol p68A (STPPLVRLV) peptides (8, 14). On day 3 of culture, 2 ml of 40 U of human recombinant IL-2 (Hoffman-La Roche) per ml was added. On day 12 of culture, peptide-stimulated PBL were centrifuged over a Ficoll gradient, washed, and stained with tetramer as described elsewhere (14).
Alternatively, on day 3 of culture, 2 ml of 40 U of human recombinant IL-2 (Hoffman-La Roche) per ml was added. On day 12 of culture, peptide-stimulated PBL were centrifuged over Ficoll (Ficoll-Paque) and assessed as effectors in standard 51Cr release assays by using U-bottomed, 96-well plates containing 104 target cells per well. Autologous B-lymphoblastoid cell lines pulsed with 1-μg/ml concentrations of p11C, p68A, or p11B control peptide (ALSEGCTPYDIN) and labeled overnight with 100 μCi of 51Cr per ml were used as targets. After 4 h of incubation at 37°C, supernatants were harvested, mixed with scintillation fluid, and measured by using a Wallac 1450 Microbeta liquid scintillation counter. To measure spontaneous release of 51Cr, target cells were incubated with 100 μl of medium, and for maximum release target cells were incubated with 100 μl of 2% Triton X-100. Percent lysis was calculated as follows: (experimental release − spontaneous release)/(maximum release − spontaneous release) × 100.
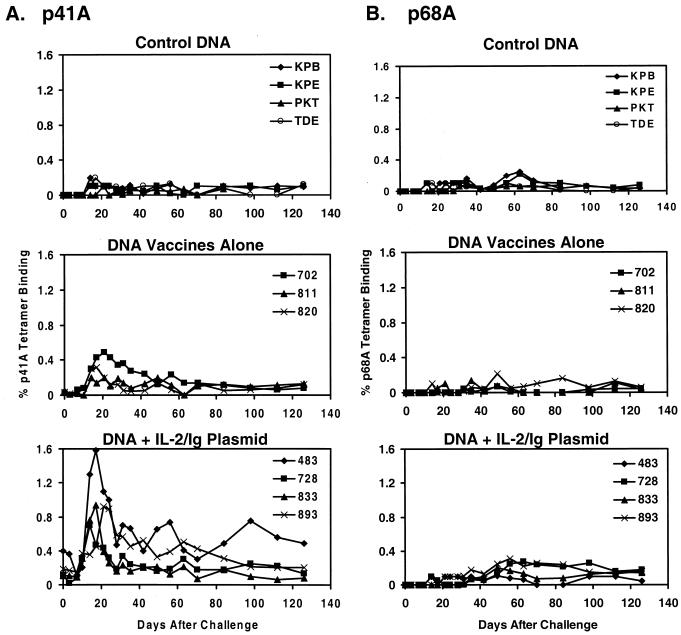
As shown in Fig. 1A, only 0.0 to 0.2% of freshly isolated CD8+ T lymphocytes from the control vaccinated monkeys bound the Env p41A tetramer following SHIV-89.6P challenge, indicating low-frequency p41A-specific CTL responses. These low-frequency primary p41A-specific tetramer responses are consistent with our previous experience with this subdominant epitope in SHIV-infected rhesus monkeys (8). In contrast, 0.2 to 0.5% of freshly isolated CD8+ T lymphocytes from the DNA-vaccinated monkeys bound the p41A tetramer on days 14 to 21 following challenge. In the monkeys that received the DNA vaccines plus IL-2/Ig plasmid, 0.5 to 1.6% of freshly isolated CD8+ T lymphocytes bound the p41A tetramer on days 14 to 21 following challenge. These values are consistent with potent secondary p41A-specific CTL responses. The rapid kinetics of the emergence of these secondary p41A-specific responses were comparable with the kinetics of the secondary CTL responses to the dominant Gag p11C epitope in these monkeys (6).
FIG. 1.
Secondary Env p41A-specific CD8+ T-cell responses in plasmid DNA-vaccinated rhesus monkeys following virus challenge. Control or gag/env DNA-vaccinated rhesus monkeys were assessed by staining freshly isolated PBMC using a Mamu-A*01/p41A tetramer (A) and a Mamu-A*01/p68A tetramer (B). The percentages of CD3+CD8+ T cells that stain positively with each tetramer are shown.
SHIV-89.6P typically causes an abrupt and profound depletion of CD4+ T lymphocytes within 2 to 3 weeks of infection (18, 19). The absence of CD4+-T-lymphocyte-mediated immunologic help in SHIV 89.6P-infected monkeys might have theoretically interfered with the ability of these animals to mount virus-specific CTL responses, and preserved CD4+-T-lymphocyte populations might facilitate the generation of such responses. To determine whether the secondary p41A-specific CTL responses generated in the vaccinated and challenged monkeys were the result of vaccination or the result of preserved CD4+-T-cell help in these animals, we measured CTL responses of these same monkeys to another subdominant epitope, the Pol p68A peptide (8). In another study, animals vaccinated with ALVAC-SIV-gag-pol elicited secondary Pol p68A responses following viral challenge (20). In the present study, vaccinated animals would not be expected to mount secondary CTL responses to this Pol epitope since they did not receive a Pol immunogen. As shown in Fig. 1B, 0.0 to 0.3% of CD8+ T lymphocytes in all groups of monkeys bound the p68A tetramer with no clear peak on days 14 to 21 following challenge. There was no difference in the magnitude of this CTL response between control and experimentally vaccinated monkeys, and the size of the tetramer response did not correlate with CD4+-T-lymphocyte responses following infection. Thus, the absence of substantial p68A-specific CTL responses indicated that the robust p41A-specific CTL responses in the experimentally vaccinated monkeys were the result of vaccine-primed CTL responses rather than simply a reflection of preserved CD4+-T-lymphocyte populations.
We confirmed these observations by studying PBMC from these monkeys following in vitro stimulation with epitope peptides. As shown in Table 1, stimulation of PBMC obtained from animals 1 month following challenge with the immunodominant Gag p11C peptide expanded the tetramer-positive cells from all groups of monkeys, and these cells exhibited potent functional p11C-specific CTL activity. In contrast, stimulation of these same PBMC with the subdominant Env p41A peptide efficiently expanded the tetramer-positive cells from the vaccinated but not the control monkeys. Moreover, PBMC from the vaccinated but not the control monkeys exhibited potent functional p41A-specific CTL activity, consistent with the previously observed secondary p41A-specific tetramer responses in these animals. Only minimal expansions of p68A-specific CTL were observed in PBMC from all three groups of monkeys. Thus, expanded populations of effector CTL specific for a subdominant viral epitope were detected in PBMC of vaccinated but not unvaccinated monkeys following viral challenge.
TABLE 1.
Secondary Env p41A-specific CTL responses in plasmid DNA-vaccinated rhesus monkeys following virus challengea
| Vaccine and monkey | CTL response specific for:
|
||||||||
|---|---|---|---|---|---|---|---|---|---|
| SIV Gag p11C
|
HIV-1 Env p41A
|
SIV Pol p68A
|
|||||||
| Tetramer
|
Lysis | Tetramer
|
Lysis | Tetramer
|
Lysis | ||||
| Fresh | Stimulated | Fresh | Stimulated | Fresh | Stimulated | ||||
| Control DNA | |||||||||
| KPB | 0.3 | 24 | 35 | 0.1 | 1 | 7 | 0.1 | 0 | 0 |
| KPE | 1.9 | 80 | 57 | 0.1 | 5 | 6 | 0.1 | 2 | 5 |
| PKT | 0.2 | 13 | 19 | 0.0 | 0 | 0 | 0.0 | 0 | 1 |
| TDE | 0.6 | 21 | 43 | 0.0 | 1 | 0 | 0.1 | 0 | 0 |
| DNA vaccines | |||||||||
| 811 | 2.7 | 87 | 48 | 0.2 | 25 | 38 | 0.0 | 0 | 0 |
| 820 | 1.7 | 61 | 57 | 0.1 | 18 | 21 | 0.0 | 1 | 5 |
| 702 | 2.3 | 82 | 50 | 0.4 | 55 | 35 | 0.0 | 0 | 2 |
| DNA vaccines + IL-2/Ig plasmid | |||||||||
| 483 | 17.5 | 93 | 64 | 1.0 | 80 | 66 | 0.1 | 1 | 0 |
| 728 | 5.0 | 81 | 64 | 0.3 | 19 | 48 | 0.0 | 2 | 6 |
| 833 | 4.5 | 72 | 59 | 0.4 | 40 | 53 | 0.0 | 3 | 1 |
| 893 | 9.1 | 89 | 63 | 0.6 | 57 | 51 | 0.1 | 2 | 5 |
PBMC from control or gag-lenv DNA-vaccinated rhesus monkeys were assessed on day 31 following challenge for Gag p11C-, Env p41A-, and Pol p68A-specific CTL responses by tetramer staining of freshly isolated PBMC, tetramer staining of peptide-stimulated PBMC, and functional specific lysis of peptide-pulsed targets at an effector-to-target ratio of 5 to 1.
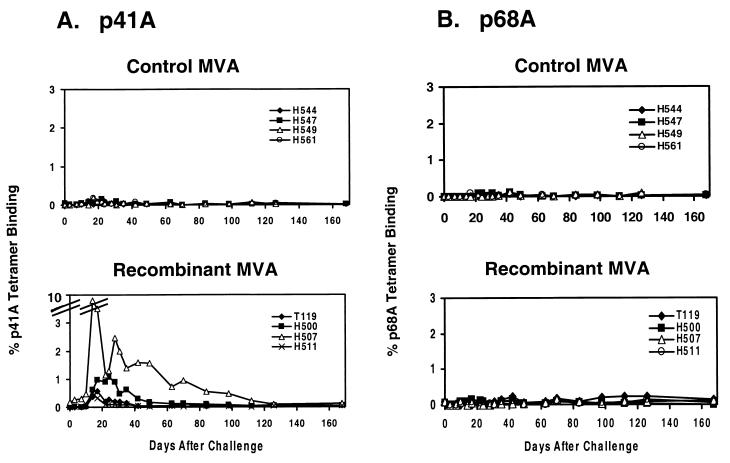
These findings were predicted, since plasmid DNA vaccination was previously shown to elicit potent CTL responses to subdominant viral epitopes in monkeys (4). We next assessed CTL responses to subdominant viral epitopes following viral challenge in monkeys that had received a vaccine which had previously been shown to elicit only marginal subdominant epitope-specific CTL responses in monkeys (4). We assessed CTL responses to the p41A and p68A subdominant epitopes in rMVA-vaccinated monkeys following challenge with SHIV-89.6P. Groups of Mamu-A*01-positive animals were immunized with MVA carrying no gene inserts (n = 4) or rMVA vaccines expressing SIVmac239 Gag-Pol and HIV-1 89.6 Env (n = 4) and challenged as described previously (7). As shown in Fig. 2A, secondary p41A-specific tetramer-positive responses were observed in freshly isolated PBMC from the rMVA-vaccinated but not the control-vaccinated monkeys following challenge. At days 14 to 21 following challenge, 0.3 to 1.0% of CD8+ T lymphocytes bound the p41A tetramer in three of the experimentally vaccinated animals, and 9.2% bound the p41A tetramer in the fourth vaccinated animal (H507). Since the rMVA-vaccinated animals did receive an SIV Pol immunogen, we also expected to detect a secondary p68A-specific response in these monkeys. However, as shown in Fig. 2B, there were only minimal CD8+ T-lymphocyte responses specific for the Pol p68A epitope peptide in freshly isolated PBMC in both experimentally vaccinated and control monkeys (0.0 to 0.1%). Nevertheless, as shown in Table 2, both p41A-specific and p68A-specific secondary CTL responses were detected in PBMC from the vaccinated monkeys following in vitro stimulation with peptide. Stimulation with the dominant Gag p11C epitope peptide resulted in the efficient expansion of p11C-specific CD8+ T cells from PBMC of both vaccinated and control animals. Stimulation of PBMC with the subdominant Env p41A epitope peptide expanded tetramer-positive cells from three of the four experimentally vaccinated but not from control-vaccinated monkeys, and these cell populations exhibited p41A-specific lytic activity. In addition, stimulation of PBMC with the subdominant Pol p68A epitope peptide from two of the four vaccinated but none of the control monkeys expanded tetramer-positive cells with p68A-specific lytic activity. These data demonstrate that the rMVA-vaccinated monkeys did indeed generate p68A-specific secondary CTL responses in half of the animals.
FIG. 2.
Secondary Env p41A- and Pol p68A-specific CD8+ T-cell responses in rMVA-vaccinated rhesus monkeys. Control or gag-pol/env rMVA-vaccinated rhesus monkeys were assessed by staining freshly isolated PBMC using a Mamu-A*01/p41A tetramer (A) and a Mamu-A*01/p68A tetramer (B). The percentages of CD3+CD8+ T cells that stain positively with each tetramer are shown.
TABLE 2.
Secondary Env p41A- and Pol p68A-specific CTL responses in rMVA-vaccinated monkeys following virus challengea
| Vaccine and monkey | CTL response specific for:
|
||||||||
|---|---|---|---|---|---|---|---|---|---|
| SIV Gag p11C
|
HIV-1 Env p41A
|
SIV Pol p68A
|
|||||||
| Tetramer
|
Lysis | Tetramer
|
Lysis | Tetramer
|
Lysis | ||||
| Fresh | Stimulated | Fresh | Stimulated | Fresh | Stimulated | ||||
| Control MVA | |||||||||
| H544 | 0.4 | 9 | 3 | 0.0 | 2 | 3 | 0.0 | 0 | 0 |
| H547 | 0.3 | 23 | 18 | 0.1 | 0 | 1 | 0.1 | 0 | 0 |
| H549 | 0.3 | 24 | 46 | 0.0 | 0 | 3 | 0.0 | 0 | 0 |
| H561 | 0.1 | 22 | 32 | 0.0 | 0 | 0 | 0.0 | 0 | 0 |
| rMVA vaccines | |||||||||
| T119 | 5.3 | 76 | 40 | 0.2 | 8 | 13 | 0.1 | 4 | NDb |
| H500 | 1.6 | 68 | 36 | 0.5 | 33 | 22 | 0.0 | 22 | 25 |
| H507 | 16.1 | 86 | 54 | 2.0 | 97 | 51 | 0.0 | 12 | 14 |
| H511 | 1.0 | 11 | 32 | 0.1 | 1 | 2 | 0.0 | 0 | 0 |
PBMC from control or gag-pol-env rMVA-vaccinated rhesus monkeys were assessed on day 31 following challenge for Gag p11C-, Env p41A-, and Pol p68A-specific CTL responses by tetramer staining of freshly isolated PBMC, tetramer staining of peptide-stimulated PBMC, and functional specific lysis of peptide-pulsed targets at an effector-to-target ratio of 5 to 1.
ND, not determined.
Both plasmid DNA and rMVA vaccination primed for secondary CTL responses to subdominant epitopes that emerged following pathogenic SHIV challenge in rhesus monkeys. The emergence of the secondary CTL responses specific for the subdominant epitopes was rapid, peaking at days 14 to 21 following challenge. These kinetics mirrored the kinetics of the evolution of secondary CTL responses to the immunodominant Gag p11C epitope and were temporally associated with control of primary viremia in the monkeys (6). These secondary CTL responses to subdominant epitopes may therefore have played a functional role in the control of early viral replication.
Moreover, a CTL response specific for multiple epitopes may also contribute to containing viral replication during an ongoing, chronic infection. The present study indicates that vaccination with plasmid DNA or rMVA primed for durable secondary CTL responses to both dominant and subdominant epitopes that persisted in monkeys following SHIV-89.6P challenge. It was previously reported that these two cohorts of experimentally vaccinated monkeys had demonstrated long-term control of viral replication following challenge (6, 7). It is likely that the CTL responses to these multiple epitopes contributed to this long-term containment of viral replication.
It was previously shown that plasmid DNA vaccination elicited CTL responses specific for both dominant and subdominant viral epitopes in rhesus monkeys. In the same study, the rMVA vaccination was shown to elicit lower-frequency CTL responses specific for subdominant epitopes. While those rMVA-induced primary CTL responses specific for subdominant viral epitopes were not readily detected by tetramer staining and functional effector cell assays, the present study shows that rMVA elicited a population of memory CTL specific for these subdominant epitopes that expanded in vivo following exposure to replicating virus.
The present study demonstrates that plasmid DNA and recombinant poxvirus vaccine constructs expressing entire viral genes are able to elicit memory CTL populations specific for subdominant viral epitopes that can expand following exposure to replicating virus. A limitation of this study is that it focuses on only two separate subdominant epitopes. Nevertheless, these data suggest that, in spite of the propensity for the immune system to focus CD8+ T-lymphocyte responses on limited numbers of dominant viral epitopes, these vaccines primed for CTL responses with significant epitopic breadth. These results support previous work that has shown elicitation of both Gag- and Env-specific CTLs by ALVAC vectors in humans (9). There are compelling arguments that vaccine-elicited CTL specific for multiple viral epitopes may prove useful in containing an HIV-1 infection. The greater the diversity of epitope-specific memory CTL populations elicited by vaccination, the greater the likelihood of generating CTL populations that will recognize a diversity of HIV-1 isolates following infection. Moreover, an increased breadth of CTL populations may reduce the frequency at which viral mutations will result in a virus that can escape from CTL control. The findings in the present study suggest that both plasmid and recombinant pox vaccine constructs can induce CTLs reactive with multiple viral epitopes.
Acknowledgments
We thank David Margolin for assistance with computer graphics and John Shiver and Tong-Ming Fu (Merck Research Laboratories), Mark Lewis (Southern Research Laboratories), and Russell Byrum (Bioqual Inc.) for reagents and generous assistance.
This work was supported by NIH grants AI-26507, CA-50139, AI-85343, and AI-20729.
REFERENCES
- 1.Allen, T. M., J. Sidney, M.-F. del Guercio, R. L. Glickman, G. L. Lensmeyer, D. A. Wiebe, R. DeMars, C. D. Pauza, R. P. Johnson, A. Sette, and D. I. Watkins. 1998. Characterization of the peptide binding motif of a rhesus MHC class I molecule (Mamu-A*01) that binds an immunodominant CTL epitope from SIV. J. Immunol. 160:6062-6071. [PubMed] [Google Scholar]
- 2.Allen, T. M., T. U. Vogel, D. H. Fuller, B. R. Mothe, S. Steffen, J. E. Boyson, T. Shipley, J. Fuller, T. Hanke, A. Sette, J. D. Altman, B. Moss, A. J. McMichael, and D. I. Watkins. 2000. Induction of AIDS virus-specific CTL activity in fresh, unstimulated peripheral blood lymphocytes from rhesus macaques vaccinated with a DNA prime/modified vaccinia virus Ankara boost regimen. J. Immunol. 164:4968-4978. [DOI] [PubMed] [Google Scholar]
- 3.Altman, J. D., P. A. H. Moss, P. J. R. Goulder, D. H. Barouch, M. G. McHeyzer-Williams, J. I. Bell, A. J. McMichael, and M. M. Davis. 1996. Phenotypic analysis of antigen-specific T lymphocytes. Science 274:94-96. [DOI] [PubMed] [Google Scholar]
- 4.Barouch, D. H., A. Craiu, S. Santra, M. A. Egan, J. E. Schmitz, M. J. Kuroda, T.-M. Fu, J.-H. Nam, L. S. Wyatt, M. A. Lifton, G. R. Krivulka, C. E. Nickerson, C. I. Lord, B. Moss, M. G. Lewis, V. M. Hirsch, J. W. Shiver, and N. L. Letvin. 2001. Elicitation of high frequency cytotoxic T-lymphocyte responses against both dominant and subdominant simian-human immunodeficiency virus epitopes by DNA vaccination of rhesus monkeys. J. Virol. 75:2462-2467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Barouch, D. H., J. Kunstman, M. J. Kuroda, J. E. Schmitz, S. Santra, F. W. Peyerl, G. R. Krivulka, K. Beaudry, M. A. Lifton, D. A. Gorgone, D. C. Montefiori, M. G. Lewis, S. M. Wolinsky, and N. L. Letvin. 2002. Eventual AIDS vaccine failure in a rhesus monkey by viral escape from CTL. Nature 415:335-339. [DOI] [PubMed] [Google Scholar]
- 6.Barouch, D. H., S. Santra, J. E. Schmitz, M. J. Kuroda, T.-M. Fu, W. Wagner, M. Bilska, A. Craiu, X. X. Zheng, G. R. Krivulka, K. Beaudry, M. A. Lifton, C. E. Nickerson, W. L. Trigona, K. Punt, D. C. Freed, L. Guan, S. Dubey, D. Casimiro, A. Simon, M.-E. Davies, M. Chastain, T. B. Strom, R. S. Gelman, D. C. Montefiori, M. G. Lewis, E. A. Emini, J. W. Shiver, and N. L. Letvin. 2000. Control of viremia and prevention of clinical AIDS in rhesus monkeys by cytokine-augmented DNA vaccination. Science 290:486-492. [DOI] [PubMed] [Google Scholar]
- 7.Barouch, D. H., S. Santra, M. J. Kuroda, J. E. Schmitz, R. Plishka, A. Buckler-White, A. E. Gaitan, R. Zin, J.-H. Nam, L. S. Wyatt, M. A. Lifton, C. E. Nickerson, B. Moss, D. C. Montefiori, V. M. Hirsch, and N. L. Letvin. 2001. Reduction of simian-human immunodeficiency virus 89.6P viremia in rhesus monkeys by recombinant modified vaccinia virus Ankara vaccination. J. Virol. 75:5151-5158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Egan, M. A., M. J. Kuroda, G. Voss, J. E. Schmitz, W. A. Charini, C. I. Lord, M. A. Forman, and N. L. Letvin. 1999. Use of a major histocompatibility complex class I/peptide/β2M tetramers to quantitate CD8+ cytotoxic T lymphocytes specific for dominant and nondominant viral epitopes in simian-human immunodeficiency virus-infected rhesus monkeys. J. Virol. 73:5466-5472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Evans, T. G., M. C. Keefer, K. J. Weinhold, M. Wolff, D. Montefiori, G. J. Gorse, B. S. Graham, M. J. McElrath, M. L. Clements-Mann, M. J. Mulligan, P. Fast, M. C. Walker, J. L. Excler, A. M. Duliege, and J. Tartaglia. 1999. A canarypox vaccine expressing multiple human immunodeficiency virus type 1 genes given alone or with rgp120 elicits broad and durable CD8+ cytotoxic T lymphocyte responses in seronegative volunteers. J. Infect. Dis. 180:290-298. [DOI] [PubMed] [Google Scholar]
- 10.Hanke, T., R. V. Samuel, T. J. Blanchard, V. C. Neumann, T. M. Allen, J. E. Boyson, S. A. Sharpe, N. Cook, G. L. Smith, D. I. Watkins, M. P. Cranage, and A. J. McMichael. 1999. Effective induction of simian immunodeficiency virus-specific cytotoxic T lymphocytes in macaques by using a multiepitope gene and DNA prime-modified vaccinia virus Ankara boost vaccination regimen. J. Virol. 73:7524-7532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ishioka, G. Y., J. Fikes, G. Hermanson, B. Livingston, C. Crimi, M. Qin, M. F. del Guercio, C. Oseroff, C. Dahlberg, J. Alexander, R. W. Chesnut, and A. Sette. 1999. Utilization of MHC class I transgenic mice for development of minigene DNA vaccines encoding multiple HLA-restricted CTL epitopes. J. Immunol. 162:3915-3925. [PubMed] [Google Scholar]
- 12.Jin, X., D. E. Bauer, S. E. Tuttleton, S. Lewin, A. Gettie, J. Blanchard, C. E. Irwin, J. T. Safrit, J. Mittler, L. Weinberger, L. G. Kostrikis, L. Zhang, A. S. Perelson, and D. D. Ho. 1999. Dramatic rise in plasma viremia after CD8+ T cell depletion in simian immunodeficiency virus-infected macaques. J. Exp. Med. 189:991-998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Koup, R. A., J. T. Safrit, Y. Cao, C. A. Andrews, G. McLeod, W. Borkowsky, C. Farthing, and D. D. Ho. 1994. Temporal association of cellular immune responses with the initial control of viremia in primary human immunodeficiency virus type 1 syndrome. J. Virol. 68:4650-4655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kuroda, M. J., J. E. Schmitz, D. H. Barouch, A. Criau, T. M. Allen, A. Sette, D. I. Watkins, M. A. Forman, and N. L. Letvin. 1998. Analysis of Gag-specific cytotoxic T lymphocytes in simian immunodeficiency virus-infected rhesus monkeys by cell staining with a tetrameric major histocompatibility complex class I-peptide complex. J. Exp. Med. 187:1373-1381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Miller, M. D., H. Yamamoto, A. H. Hughes, D. I. Watkins, and N. L. Letvin. 1991. Definition of an epitope and MHC class I molecule recognized by Gag-specific cytotoxic T lymphocytes in SIVmac-infected rhesus monkeys. J. Immunol. 147:320-329. [PubMed] [Google Scholar]
- 16.Musey, L., J. Hughes, T. Schacker, T. Shea, L. Corey, and M. J. McElrath. 1997. Cytotoxic-T-cell responses, viral load, and disease progression in early human immunodeficiency virus type 1 infection. N. Engl. J. Med. 337:1267-1274. [DOI] [PubMed] [Google Scholar]
- 17.Ogg, G. S., X. Jin, S. Bonhoeffer, P. R. Dunbar, M. A. Nowak, S. Monard, J. P. Segal, Y. Cao, S. L. Rowland-Jones, V. Cerundolo, A. Hurley, M. Markowitz, D. D. Ho, D. F. Nixon, and A. J. McMichael. 1998. Quantitation of HIV-1-specific cytotoxic T lymphocytes and plasma load of viral RNA. Science 279:2103-2106. [DOI] [PubMed] [Google Scholar]
- 18.Reimann, K. A., A. Watson, P. J. Dailey, W. Lin, C. I. Lord, T. D. Steenbeke, R. A. Parker, M. K. Axthelm, and G. B. Karlsson. 1999. Viral burden and disease progression in rhesus monkeys infected with chimeric simian-human immunodeficiency viruses. Virology 256:15-21. [DOI] [PubMed] [Google Scholar]
- 19.Reimann, K. A., J. T. Li, R. Veazey, M. Halloran, I.-W. Park, G. B. Karlsson, J. Sodroski, and N. L. Letvin. 1996. A chimeric simian/human immunodeficiency virus expressing a primary patient human immunodeficiency virus type 1 isolate env causes an AIDS-like disease after in vivo passage in rhesus monkeys. J. Virol. 70:6922-6928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Santra, S., J. E. Schmitz, M. J. Kuroda, M. A. Lifton, C. E. Nickerson, C. I. Lord, R. Pal, G. Franchini, and N. L. Letvin. 2002. Recombinant canarypox vaccine-elicited CTL specific for dominant and subdominant simian immunodeficiency virus epitopes in rhesus monkeys. J. Immunol. 168:1847-1853. [DOI] [PubMed] [Google Scholar]
- 21.Schmitz, J. E., M. J. Kuroda, S. Santra, V. G. Sasseville, M. A. Simon, M. A. Lifton, P. Racz, K. Tenner-Racz, M. Dalesandro, B. J. Scallon, G. Ghrayeb, M. A. Forman, D. C. Montefiori, E. P. Rieber, N. L. Letvin, and K. A. Reimann. 1999. Control of viremia in simian immunodeficiency virus infection by CD8+ lymphocytes. Science 283:857-860. [DOI] [PubMed] [Google Scholar]
- 22.Yasutomi, Y., S. Koenig, R. M. Woods, J. Madsen, N. M. Wassef, C. R. Alving, H. J. Klein, T. E. Nolan, L. J. Boots, J. A. Kessler, E. A. Emini, A. J. Conley, and N. L. Letvin. 1995. A vaccine-elicited, single viral epitope-specific cytotoxic T-lymphocyte response does not protect against intravenous, cell-free simian immunodeficiency virus challenge. J. Virol. 69:2279-2284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Yewdell, J. W., and J. R. Bennick. 1999. Immunodominance in major histocompatibility complex class I-restricted T lymphocyte responses. Annu. Rev. Immunol. 17:51-88. [DOI] [PubMed] [Google Scholar]