Abstract
We examined measures of oral and pharyngeal residues from scintigraphic studies and estimates/observations from videofluorographic (modified barium swallow) studies taken on the same day but not concurrently in 16 dysphagic patients of varying etiologies presenting with oral and/or pharyngeal dysphagia. Oral and pharyngeal residuals following the swallow were quantified scintigraphically and were then compared with measures of residuals obtained from the modified barium swallow. Estimates of oral and pharyngeal residues from the modified barium swallows were generated by a trained observer who was blinded to the scintigraphic data. Positive and significant Spearman correlations between oral and pharyngeal residue measures from scintigraphy and observations of oral and pharyngeal residues from modified barium swallows were found. This supports the validity of observations of oral and pharyngeal residues in clinical studies. Limitations of these observations are discussed.
Keywords: Swallowing, Scintigraphy, Modified barium swallow, Residue, Oropharyngeal swallow efficiency, Deglutition, Deglutition disorders
The oropharyngeal swallow efficiency (OPSE) score was developed as a single global measure to reflect all aspects of oropharyngeal dysphagia during videofluorography: oropharyngeal transit times (speed of movement of the bolus through the oral cavity and pharynx) and the observed or measured percentage of bolus swallowed into the esophagus minus an estimate of the percentage aspirated, thus reflecting the efficiency of swallow [1]. Normal subjects swallow essentially all of the bolus with minimal residue (2%–4%). The percentage swallowed into the esophagus involves subtraction of the approximate percentage of the bolus left as oral residue and pharyngeal residue and the approximate percentage of the bolus judged to be aspirated from 100%. These percentages can be measured from scintigraphy. From videofluorography, residue and aspiration are clinical judgments from observations of the proportion of the bolus remaining in the mouth or pharynx (residue) and the approximate amount of bolus entering the airway (aspiration).
The oropharyngeal swallow efficiency measure has been criticized because of the perceptual judgments involved in its calculation, i.e., approximate percentage of oral and pharyngeal residue and approximate percentage of aspiration. This criticism is based on the fact that these percentages of residues and aspiration are being judged from a two-dimensional view (videofluorography) of three-dimensional structures, the oral cavity and the pharynx [2]. Scintigraphy permits precise quantification of actual percentages of the bolus aspirated or percentages of residue in the mouth or pharynx [2,5-5].
The aim of this study was to compare trained clinician/observer judgments of postswallow oral and pharyngeal bolus residuals derived from videofluorography with comparable measures of oral and pharyngeal residues derived scintigraphically.
Methods
Scintigraphy and the modified barium swallow cannot be done concurrently because of the difference in contrast material required for each test. Therefore, both the scintigraphic studies and the videofluorographic studies were recorded within a 24-hour period at St. George Hospital (Sydney, Australia).
Subjects
Subjects were 16 individuals (8 men, 8 women) between the ages of 64 and 83 (mean age, 74.8) with oral-pharyngeal dysphagia who volunteered for this study. These patients included one with oral dysphagia, six with pharyngeal dysphagia, and nine with both oral and pharyngeal dysphagia. Diagnosis of regional dysfunction was made on the basis of videoradiologic swallowing studies. Subjects included individuals who had sustained stroke, treatment for head and neck cancer, and progressive neurologic disease. Informed consent was obtained from all participants and the study was approved by the Ethics Committees of the Southern Sydney Area Health Service and the University of New South Wales.
Scintigraphic Technique
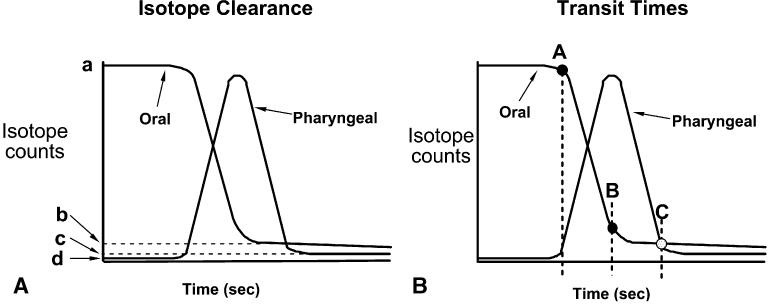
Subjects were studied, sitting in the right lateral position in front of a vertically positioned large-field-of-view Toshiba 402 gamma camera (Toshiba Corp., Tokyo) with a low-energy all-purpose (LEAP) collimator. Three radioactive skin markers were used to delineate oral and pharyngeal regions of interest (ROI). Skin markers were 10-mm lengths of PVC tubing (0.8-mm) filled with a small amount of 99mTc. Two markers were placed by palpation on the neck: one at the superior margin of the hyoid bone in its resting position and the second over the inferior margin of the cricoid cartilage. A third external skin marker was placed in line with the posterior tonsillar pillar which was identified by temporary placement of a radioactive marker (positioned on the tip of a cotton applicator) within the mouth against the posterior tonsillar pillar. The external skin marker was then aligned with the internal marker and taped to the side of the face closest to the camera. The oral ROI was defined as the area anterior to the line joining the posterior tonsillar pillar and the hyoid markers. The pharyngeal region of interest was bounded by the posterior tonsillar pillar and hyoid marks superiorly and the cricoid marker anteroinferiorly (Fig. 1).
Fig. 1.
Oral and pharyngeal regions of interest (ROI) were defined by radioactive skin markers placed over the posterior tonsillar pillar, hyoid bone and inferior margin of the cricoid cartilage (see text).
Scintigraphic images were acquired at 20 frames/s for 25 using a 64 × 64 sampling matrix onto a NPS computer (Philips Medical Systems, Hamburg, Germany). Each subject swallowed duplicate 5-ml and 10-ml boluses of water, each labeled with 30 MBq of 99mTc tin-colloid (Amersham International, UK). Subjects were instructed not to move during the recording period and head stability was ensured by interposing a pillow between the subject's head and the camera. Subjects were asked to swallow the entire bolus of water in a single swallow within 2 s of recording commencement. Between recording sequences the subjects were given 200 ml of unlabeled water to drink in order to wash out any isotope remaining in the mouth or pharynx from the previous test bolus. A 1-min frame was recorded before each swallow sequence to quantify regional background counts. Residual counts for each ROI were corrected for background by subtraction. At study completion, 1-min anterior and posterior images of the lungs were acquired to check for aspiration.
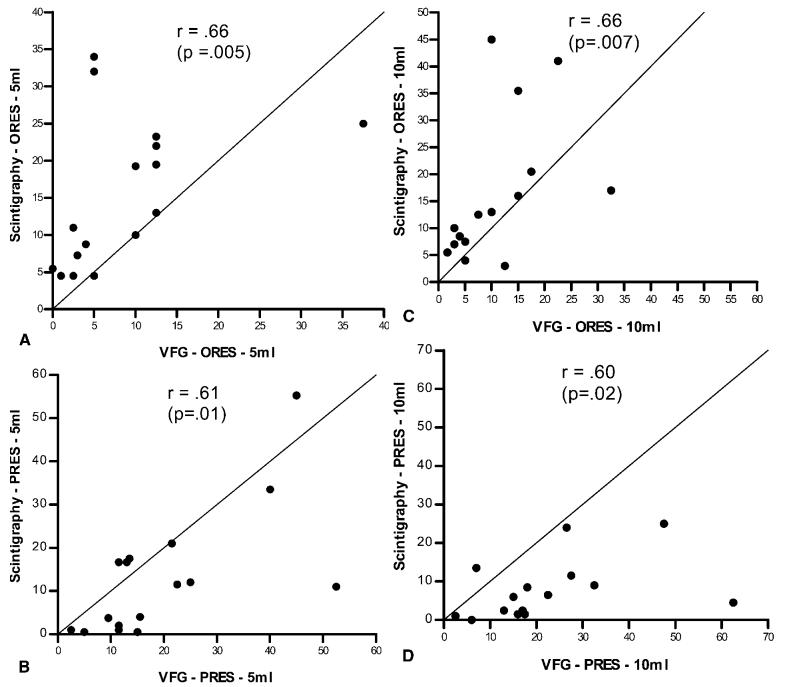
Time–activity curves were generated for the oral and pharyngeal ROI (Fig. 2). Residual counts following the swallow were used as a measure of the completeness of regional emptying and were expressed as a percent of counts delivered to each region. Oral residual (b/a × 100%) was defined as the counts remaining in the oral ROI following the swallow. Pharyngeal residual ([c − d]/[a − b] × 100%) was defined as the counts remaining in the pharyngeal ROI following a completed swallow, (c − d), expressed as a percentage of counts delivered from the oral to the pharyngeal region, (a − b). Because isotope concentration in the 10-ml bolus was half that of the 5-ml bolus, residual counts for the 10-ml swallows were corrected (doubled) for comparison of bolus volume effects. Once the a − d points were identified by a trained observer, the oral and pharyngeal residue data were generated by the scintigraphic computer.
Fig. 2.
Shown schematically are oral and pharyngeal time–activity curves depicting parameters used to calculate regional postswallow residuals (a) and transit times (b). (a) Oral residual, expressed as a percent of preswallow counts. (b/a × 100%). Pharyngeal residual, expressed as a percent of counts delivered to the pharynx and corrected for background counts [(c−d)/(a−b × 100%] a = oral counts from bolus preswallow; b = postswallow oral residual counts; c = post swallow pharyngeal residual counts; d = preswallow background counts from pharyngeal region. (b) Oral transit time = B−A seconds, pharyngeal transit time = C−B seconds, and pharyngeal clearance time = C−A seconds. Pharyngeal clearance time is the interval from the first entry of the bolus head into the pharynx until the exit of the bolus tail from the hypopharynx. A = onset of oral emptying; B = completion of oral emptying; C = completion of pharyngeal emptying.
Videofluoroscopic Technique
Subjects were studied seated upright as previously described [6]. Briefly, images of barium swallows were recorded in the lateral projection using a 9-in. Phillips image intensifier (Phillips, Eindhoven, Holland). Fluoroscopic images of swallows in anteroposterior and lateral projections were recorded on videotape at 25 frames/s by a VHS video recorder (Panasonic, AG6500, Osaka, Japan) for later analysis. Magnification correction was established before the commencement of each study by placing two metallic markers set 3 cm apart in the field of the image intensifier, above the subject's head but in the plane of the upper esophageal sphercter (UES). Duplicate swallows of 5 and 10-ml boluses of high-density liquid barium suspension [250% (wt/vol), E-Z-HD, E-Z EM Inc., Westbury, NY] were measured and delivered to the mouth by syringe. Oral and pharyngeal residues from the modified barium swallow were generated by one trained clinical observer who was blinded to the scintigraphic data. Ten percent of the judgments were repeated within and between observers. Interobserver reliability was r = 0.94 while intraobserver reliability was r = 0.99.
Statistical Analysis
Two swallows were averaged to derive summary data for each measure at each volume. To determine the extent of the relationship between the videofluorographic and the scintigraphic measures, judgments of oral and pharyngeal residues from the videofluorographic study were correlated with measures of oral residue from the scintigraphic study using the Spearman correlation coefficient [7]. To determine the extent to which the two measures were in agreement, Bland–Altman plots were constructed [8]. For oral residue, this is a plot of the difference in the two measures (scintigraphy minus videofluorography oral residue) on the ordinate versus the mean of the two measures on the abscissa. A similar analysis was done for pharyngeal residue. The 5-ml and 10-ml volumes were analyzed separately. Unfortunately, we did not have a sufficient number of subjects to complete a statistical analysis of whether some pathologic conditions had a better or poorer relationship between VFG and scintigraphy.
Results
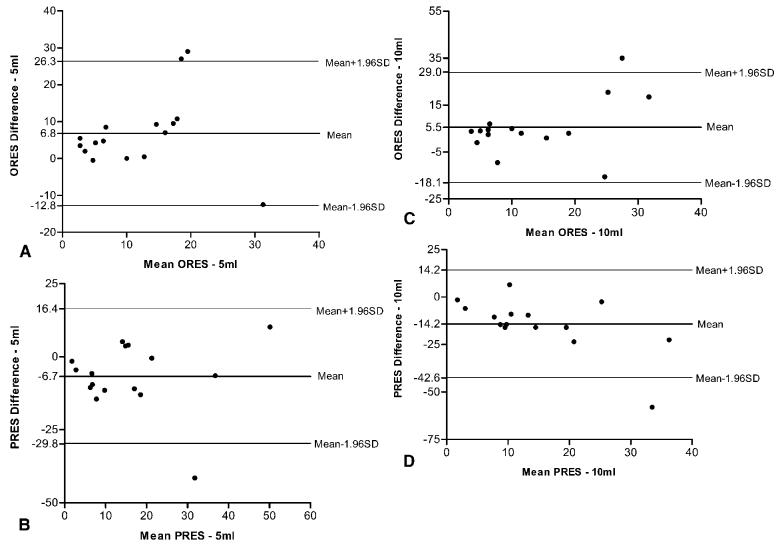
We examined residue data from scintigraphic studies and videofluoroscopic (modified barium swallow) studies taken on the same day but not concurrently in 16 dysphagic patients of varying etiologies. The studies could not be done concurrently because of the difference in contrast materials needed. No patients aspirated so approximate percents of aspiration were not evaluated. The statistical analysis revealed positive and significant (p < 0.02) Spearman correlations were obtained between oral residue measures from scintigraphy and observations of oral residue from modified barium swallow (r = 0.66 for both 5-ml and 10-ml boluses) and pharyngeal residue measures from scintigraphy and observations of pharyngeal residue from the modified barium swallow (r = 0.61 for 5 ml and r = 0.60 for 10-ml boluses). These plots (Fig. 3a-d) show the relationship between the scintigraphic measures and the videofluoroscopic observations which examine the validity of the observations from videofluorography.
Fig. 3.
Plots of percent oral residue (ORES) (a and c) and percent pharyngeal residue (PRES) (b and d) as measured from scintigraphy and observed from videofluorography on 5-ml (a and b) and 10-ml (c and d) liquid boluses.
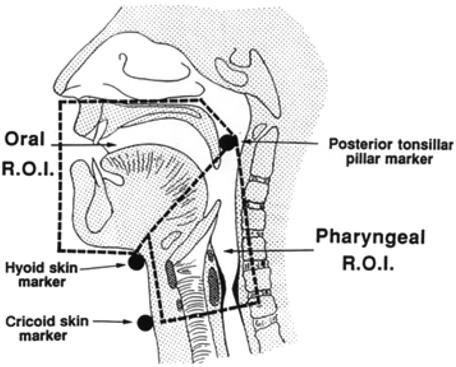
We examined overall agreement between the two modalities using Bland–Altman plots (Fig. 4a-d). Compared with scintigraphy, radiography underestimated oral residual by an average of 6% and overestimated pharyngeal residue by an average of 10% for both bolus sizes. Interestingly, with the exception of a few outliers, most data points are quite close to the mean line. Outlying points are more likely to occur as the amount of residue increases, suggesting that the precision of the comparison decreases under these conditions.
Fig. 4.
Bland–Altman plots of the similarities of the oral (ORES) (a and c) and pharyngeal residue (PRES) (b and d) for 5-ml (a and b) and 10-ml (c and d) boluses. Horizontal lines for the mean difference and for ±1.96 standard deviations of the difference are plotted in the graph.
Discussion
One important characteristic of swallow is its efficiency, i.e., clearance of essentially the entire bolus. Unfortunately, the only instrumental diagnostic procedure currently able to measure residue in the oral cavity or pharynx is oropharyngeal scintigraphy, which is not widely available. The VFG is the most commonly applied technique to assess the disordered pharyngeal swallow. It would be of great clinical use if a valid, semiquantifiable measure of bolus clearance could be obtained from the standard VFG.
This study examined the ability of a trained clinician to observe and judge the percent of the bolus left after the swallow as residue in the mouth and pharynx from observations of videofluoroscopic images in relation to measures taken from scintigraphy on the same bolus volumes. The resulting correlations between oral residue and pharyngeal residue measures from scintigraphy and observations from videofluorography were better than expected. They are particularly impressive in the context that the two tests cannot be done concurrently. By necessity, the radiographic bolus was high-density barium suspension and the scintigraphy bolus was water labeled with Tc from a suspension. This difference could well account for the observation of the systematic error between estimates of residue for the two modalities, as seen in the Bland–Altman plots. The absolute volume of residue cannot be approximated from videofluorography. We would argue that clinical observations of percent residue are particularly accurate when used to compare the patient's performance with himself across time periods or bolus types. Any error from observation would be equally distributed across patients, time periods, or bolus types. If, however, scientific precision of measurement of residue is needed, then scintigraphy is needed. Also, if large volumes of residue are present, scintigraphy is also more accurate.
While scintigraphy has the advantage of enabling measures of percent aspiration and percent residue, as well as oral and pharyngeal transit times, it does not allow determination of swallow disorders and other timing measures of the swallow such as duration of oropharyngeal opening, airway closure, etc. Scintigraphy is also limited by the number of swallows that can be observed (certainly, this is less than that of a fluoroscopic study). In contrast, videofluorography allows visualization of movement disorders and measurements of timing of oropharyngeal swallow events but only approximation of the proportion of aspiration or residue. Thus, the selection of procedures for research or clinical work will depend on what specifically the clinician/investigator wishes to observe or measure.
The data in this article indicate that observations of percent residue from videofluorography can be useful and representative when obtained bya well-trained clinician. The number of hours of training needed to reach a high level of accuracy remains to be defined. Very often we expect clinicians to give us accurate observations with inadequate training. Studies of the relationships between the accuracy of observations and the hours of training received are needed. As in all studies involving perceptual evaluation, training to a criterion level between observers is critical. Since none of these subjects aspirated, a second investigation is needed to compare the accuracy of observation of amount of aspiration from videofluoroscopy with measurement of amount of aspiration from scintigraphy.
Acknowledgment
This work was supported by the Cancer Control Science Project in Head and Neck Cancer Rehabilitation (NIH P01 CA40007).
References
- 1.Rademaker AW, Pauloski BR, Logemann JA, Shanahan TK. Oropharyngeal swallow efficiency as a representative measure of swallowing function. J Speech Hear Res. 1994;37:314–325. doi: 10.1044/jshr.3702.314. [DOI] [PubMed] [Google Scholar]
- 2.Hamlet S, Choi J, Zormweier M, Shamsa F, Stachler R, Muz J, Jones L. Normal adult swallowing of liquid, viscous material: Scintigraphic data on bolus transit and oropharyngeal residues. Dysphagia. 1996;11:41–47. doi: 10.1007/BF00385799. [DOI] [PubMed] [Google Scholar]
- 3.Cook IJ, Weltman MD, Wallace K, Shaw DW, McKay E, Smart RC, Butler SP. Influence of aging on oral-pharyngeal bolus transit and clearance during swallowing: scintigraphic study. Am J Physiol. 1994;266:G972–G977. doi: 10.1152/ajpgi.1994.266.6.G972. [DOI] [PubMed] [Google Scholar]
- 4.Hamlet SL, Wilson S, Stachler RJ, Salwen WA, Muz J, Heilbrun LK. Scintigraphic assessment of swallow efficiency postlaryngectomy. Laryngoscope. 1994;104:1159–1162. doi: 10.1288/00005537-199409000-00019. [DOI] [PubMed] [Google Scholar]
- 5.Shaw DW, Williams RBH, Cook IJ, Wallace KL, Weltman MD, Collins PJ, McKay E, Smart R, Simula ME. Oropharyngeal scintigraphy: a reliable technique for the quantitative evaluation of oral-pharyngeal swallowing. Dysphagia. 2004;19:36–42. doi: 10.1007/s00455-003-0033-7. [DOI] [PubMed] [Google Scholar]
- 6.Ali GN, Cook IJ, Laundl TM, Wallace KL, de Carle DJ. Influence of altered tongue contour and position on deglutitive pharyngeal and UES function. Am J Physiol. 1997;273(5 Pt 1):G1071–G1076. doi: 10.1152/ajpgi.1997.273.5.G1071. [DOI] [PubMed] [Google Scholar]
- 7.Rosner B. Fundamentals of Biostatistics. 5th Duxbury Press; Pacific Grove, CA: 2000. [Google Scholar]
- 8.Bland JM, Altman DG. Statistical methods for assessing agreement between two methods of clinical measurement. Lancet. 1986;1:307–310. [PubMed] [Google Scholar]