Abstract
The symptoms of PTSD and pain frequently co-occur following a traumatic event; however, very little is known about how these two conditions are associated with physical and psychosocial functioning. The current study intended to first examine the differential association of co-occurring pain complaints and PTSD symptoms with disability in the domains of psychosocial and physical functioning, and second, to test whether perceived life control is a mediator of these relationships. All participants experienced a motor vehicle accident (MVA) and reported pain due to accident-related injuries (n=183). Structural equation modeling was used to develop two models hypothesizing a relationship between PTSD symptomatology, pain severity, and perceived life control. Separate models were constructed for psychosocial and physical functioning, based on the hypothesis that pain and PTSD would be differentially related to disability in these two domains. Results suggested that more severe PTSD symptoms and greater pain complaints were related to psychosocial impairment, however, only pain was significantly related to impairment in physical functioning. Perceptions of life control were shown to further explain these interrelationships.
Keywords: Post-traumatic stress disorder, Chronic pain, Life control, Physical functioning, Psychosocial functioning
It is well established that chronic pain and post-traumatic stress disorder (PTSD) commonly co-occur in the aftermath of a traumatic event (Asmundson et al., 1998; Beckham et al., 1997; Benedikt and Kolb, 1986; Chibnall and Duckro, 1994). For example, up to 75% of individuals with PTSD following a motor vehicle accident (MVA) also report chronic pain (Hickling et al., 1992). In addition, co-occurring pain and PTSD has been linked to psychosocial (Beck et al., 2003) and physical impairment (Geisser et al., 1996). However, no study has examined the possibility that pain and PTSD are differentially associated with impairment in these two domains. Exploring this possibility would add to our understanding about how pain and PTSD separately interfere with functioning and would help to inform treatments for trauma survivors. The current study sought to examine the differential relationship of pain and PTSD with psychosocial and physical impairment. In addition, perceived life control was examined as a mediator of these relationships.
Sharp and Harvey (2001) proposed a model that suggests that there are factors common to pain and PTSD that work to maintain both conditions. Based on this idea, a factor such as this (e.g. a specific cognitive appraisal) could help explain how pain and PTSD are related to functioning in the aftermath of a trauma. Cognitive appraisals have often been used to explicate the relationship between an individual’s situation and related consequences, such as behavioral responses and emotional states (Lazarus and Folkman, 1984). For example, Turk et al. (1995) found that cognitive appraisals of life control mediate the relationship between chronic pain and depression. This study suggests that it is not the experience of chronic pain that directly results in depression, rather it provides evidence for the existence of an indirect pathway in which pain influences depressive symptoms via perceptions of life control.
Perceived life control is a cognitive appraisal that has been shown to be significantly associated with PTSD symptoms (Bolstad and Zinbarg, 1997; Regehr et al., 1999), increased pain severity, and physical disability (Kerns et al., 1985; LaChapelle et al., 2001; Rudy et al., 1989; Turk and Rudy, 1988). In addition, perceived life control has been found to be related to distress and disability (e.g. Spinhoven et al., 1989; Casella and Motta, 1990). On a related note, general perceptions of control appear to be more important in explaining current functioning among trauma survivors, relative to control felt during the trauma or controllability over future events (Kushner et al., 1992). These findings provide evidence for a possible pathway in which pain and PTSD are related to psychosocial and physical impairment via perceived life control.
Thus, the current study had two aims: (1) to examine the differential association of pain and PTSD symptoms with psychosocial and physical impairment, and (2) to test whether perceived life control is a mediator of these relationships. To address these aims, two models were created so that psychosocial and physical functioning could be examined separately in a cross-sectional sample of 183 MVA survivors.
1. Method
1.1. Procedure
Participants were recruited as part of a larger study on the assessment and treatment of PTSD. They were referred by physicians, psychologists, social workers, physical therapists, massage therapists, chiropractors, and other healthcare professionals. Additionally, some participants volunteered for the project after seeing advertisements in local newspapers. When potential participants contacted the project in order to volunteer, they went through a brief phone screening conducted by the second author, in which the client’s appropriateness for the project was assessed (i.e. they had been involved in a traumatic MVA). Volunteers who were found to be appropriate for the project were invited to an in-person interview. All participants were interviewed individually by trained doctoral students in clinical psychology and also completed a series of self-report measures.
1.2. Participants
Given the high co-occurrence of PTSD and pain after a MVA (Hickling and Blanchard, 1992), this study’s sample consisted of participants who had been involved in a MVA and were currently experiencing pain as a result of accident-related injuries. Two-hundred and eighty-two participants volunteered as part of a larger study of the assessment and treatment of PTSD following a MVA. Based on criteria for the larger study, 14 individuals were excluded because they were over age 65 (n=2), diagnosed with significant cognitive impairment (n=3), or endorsed current substance abuse or dependence (n=9). Of the remaining 268 participants, not all were experiencing pain as a result of accident-related injuries. To be classified as having pain, individuals needed to report significant lifestyle limitations or to report that they were currently seeking medical care (e.g. utilizing prescription pain medication at least 3 days/week, receiving physical therapy, massage therapy, or chiropractic care, etc.) for pain related to injuries sustained during their MVA. Eighty-five participants were excluded from the current sample because they were not experiencing pain (n=82) or because the pain they were experiencing was not the result of the MVA (n=3). The final sample for this study included 183 participants (137 females, 46 males). All participants reported that they experienced a MVA at least 1 month prior to assessment and reported feelings of fear, helplessness, or horror that they experienced at the time of the MVA (Criterion A for PTSD;APA, 2000).
The sample had a mean age of 41.60 (SD=10.41) and the majority (81.4%) indicated that they were Caucasian. Forty-eight percent of the sample was married. Thirty-two percent of the sample reported working full time. With respect to educational attainment, 22% (n=40) had a high school degree or less, 36% (n=65) had attended some college, 35% (n=64) had a 2- or 4-year college degree, and 1% (n=14) had a masters or doctoral degree. Fifty percent had an annual income of $30,000 or less. Specifically, 19% (n=33) made less than $10,000, 12% (n=21) made $10-20,000, 18% (n=31) made $20-30,000, 14% (n=24) made $30-40,000, 16% (n=28) made $40-50,000, 8% (n=14) made $50-60,000, and 12% (n=20) made $60,000 or more annually. Twelve participants did not provide information regarding their income. Participants tended to report being on medication, with 87.4% (n=160) reporting that they were currently using prescription medication for anxiety or depression and 60.1% (n=110) reporting that they were currently taking prescription pain medication. Participants had on average experienced their MVA 27.84 months (SD=44.14) prior to the study. Because this variable was substantially, positively skewed, a log transformation was performed on the data (Tabachnick and Fidell, 2001). The transformed variable was used for all subsequent analyses.
All participants indicated that their pain started immediately after the accident, and the majority of participants indicated pain complaints associated with musculoskeletal or soft tissue injury (77.6%, n=142). Also, the majority of participants reported having multiple pain sites, with 55% (n=101) reporting six or more pain sites (range 1-9 pain sites). Participants indicated experiencing neck/shoulder pain (82%, n=150), painful jaw (30%, n=55), right hand/arm pain (53%, n=97), left hand/arm pain (49%, n=89), right foot/leg pain (50%, n=91), left foot/leg pain (48%, n=88), and headaches (70%, n=128). Seventy-four percent (n=136) indicated general back pain, while 72% (n=131) specified that they had lower back pain.
1.3. Measures
1.3.1. Symptoms of PTSD
The Clinician Administered PTSD Scale (CAPS) is a structured interview designed to assess the frequency and intensity of the 17 symptoms of PTSD in the past month (Blake et al., 1990). The frequency and intensity of each symptom are rated on a 5-point Likert scale, where 0 indicates that the symptom has not occurred or is not distressing to the individual and 4 indicates that the symptom occurs nearly every day or is severely distressing. Frequency and intensity scores are multiplied for each of the 17 items and summed to calculate a total score for the CAPS. Five rationally derived severity score ranges have been proposed for interpreting the CAPS total: 0-19=few symptoms, 20-39=mild/subthreshold PTSD, 40-59=moderate/threshold PTSD, 60-79=severe PTSD, and >80=extreme PTSD (Weathers et al., 2001). As reviewed by Weathers et al. (2001), the CAPS has excellent support for its reliability, with alpha coefficients generally ranging from 0.73 to 0.98. Two- to three-day test-retest reliability was found to range from 0.78 to 0.87 (Weathers et al., 2001). In the current study, the CAPS was administered by trained doctoral students to assess the symptoms related to the experience of a MVA. All interviews were videotaped and 31% (n=57) were randomly selected and rated by an independent reviewer to establish inter-rater reliability for CAPS total, which was excellent (α=0.97).
1.3.2. Pain complaints and life control
To measure the constructs of pain severity and perceived life control, the current study used the pain severity and life control subscales of the Multidimensional Pain Inventory (MPI; Kerns et al., 1985). The MPI is a self-report measure developed to address multiple facets of the pain experience and related constructs (Kerns et al., 1985). The pain severity subscale contains three items and the life control subscale includes four items. Items are rated on a 6-point Likert scale with 0 indicating ‘not at all’ and 6 indicating ‘extremely.’ Scores for these subscales are calculated by summing the scores for their respective items and dividing by the number of items within the subscale. Scores are then transformed into t-scores (M=50; SD=10, ranging 0-100) based on means and standard deviations of over 700 heterogeneous chronic pain patients (transformation procedure presented in Rudy, 1989). Rudy (1989) suggests that t-scores that range from 30 to 70 represent the scores of an ‘average’ pain patient. The MPI has been shown to have good internal consistency and test-retest reliability (Kerns et al., 1985). Alpha coefficients calculated from the current sample were 0.89 for pain severity and 0.81 for life control.
1.3.3. Physical and psychosocial impairment
The sickness impact profile (SIP) was used to assess perceived health status (Bergner et al., 1976). The SIP is a 136-item measure that is divided into two subscales, which assess physical and psychosocial impairment. Participants are asked to indicate which items describe their current state of health. The physical subscale includes 45 items that refer to body care and management, mobility, and ambulation. The psychosocial subscale includes 38 items that refer to emotional behavior, social interaction, alertness behavior, and communication. Scores for the subscales are calculated by summing the scale values for items endorsed and then dividing by the total possible score for each subscale. Therefore, scores for the subscales can range from 0 to 100, with higher scores indicating greater dysfunction. It has been suggested that scores above 20 indicate significant dysfunction (Bergner et al., 1981; Deyo, 1986). The SIP has been shown to have good internal consistency (Bergner et al., 1981) and test-retest reliability (Deyo, 1986). In the current sample, the α coefficient was 0.88 for physical impairment and 0.87 for psychosocial impairment.
1.4. Data analytic approach
In the current study, two models were developed. One model explored the association of pain and PTSD with psychosocial impairment, and the other examined the relationship between these variables and physical impairment. Paths were specified in both models in order to address the two aims of the study. To address the first aim, direct paths were specified from PTSD symptoms and pain severity to psychosocial/physical impairment. To address the second aim of the study, indirect paths from PTSD symptoms and pain severity to psychosocial/physical impairment via life control were specified.
Descriptive statistics were calculated to examine univariate distributions of all of the variables. Skew and kurtosis levels were within acceptable limits (less than 2.0 and 4.0, respectively) for all of the variables (Tabachnick and Fidell, 2001) and no univariate outliers were detected (Kline, 1998). Means, standard deviations, and correlations among the models’ main variables were calculated (Table 1). Means on these measures, suggest that this sample is experiencing moderate levels of PTSD symptomatology (Weathers et al., 2001), low perceived life control (but still within the normal range for a pain patient; Rudy, 1989), low pain severity (but still within the normal range for a pain patient; Rudy, 1989), high levels of psychosocial impairment, and moderate physical impairment (Bergner et al., 1981; Deyo, 1986). All correlations among these variables were found to be less than 0.85, which is a suggested upper limit for correlations between two variables indicating multicollinearity (Kline, 1998).
Table 1.
Means, standard deviations, and bivariate correlations for model variables
| Variable | 1 | 2 | 3 | 4 | M | SD |
|---|---|---|---|---|---|---|
| 1. Pain severity | 43.56 | 14.16 | ||||
| 2. CAPS total | 0.35** | 48.40 | 25.72 | |||
| 3. Psychosocial impairment | 0.53** | 0.57** | 24.84 | 18.70 | ||
| 4. Physical impairment | 0.60** | 0.23** | 0.61** | 12.77 | 11.07 | |
| 5. Life control | -0.48** | -0.45** | -0.63** | -0.43** | 49.74 | 7.54 |
Pain severity=pain severity subscale of the Multidimensional Pain Inventory. CAPS total=total score on the Clinician Administered PTSD Scale. Psychosocial impairment=psychosocial impairment subscale of the Sickness Impact Profile. Physical impairment=physical impairment subscale of the Sickness Impact Profile. Life control=life control subscale of the Multidimensional Pain Inventory.
p<0.05
p<0.001.
In an effort to identify and model any existing relationships between relevant demographic variables, pain severity, and CAPS total, correlations among these variables were calculated (Table 2). Given power restrictions, not all demographic variables were included this analysis. Age, gender (coded 0=male, 1=female), ethnicity (coded 0=Caucasian, 1=other ethnicities), education level (coded 0=less than a college degree, 1=at least a college degree), income (coded 0=$30,000 or less, 1=more than $30,000), number of months post-MVA, and number of pain sites were included in this correlational examination. Although data was available on employment for the sample, this variable was not included given its clear conceptual overlap with psychosocial and physical impairment. Similarly, psychotropic and pain medication status were not included because of their conceptual overlap with pain severity and PTSD symptoms. Correlations, presented in Table 2, revealed that age, education, and number of pain sites were significantly related to pain severity. Education, ethnicity, and number of months post-MVA were found to be significantly related to PTSD symptoms. These relationships were included in subsequent analyses. The significant relationships between number of pain sites and ethnicity, and ethnicity and number of months post-MVA were also represented in the final models.
Table 2.
Bivariate correlations of demographic variables with CAPS total and pain severity
| Variable | CAPS total | Pain severity | 1 | 2 | 3 | 4 | 5 | 6 |
|---|---|---|---|---|---|---|---|---|
| 1. Age | 0.07 | 0.16* | ||||||
| 2. Gender | 0.11 | 0.12 | 0.02 | |||||
| 3. Ethnicity | 0.19** | 0.10 | -0.02 | -0.08 | ||||
| 4. Education | -0.16* | -0.22** | -0.11 | -0.04 | -0.13 | |||
| 5. Income | 0.03 | -0.10 | 0.17* | -0.01 | -0.14 | 0.07 | ||
| 6. Months post-MVA | -0.28** | 0.07 | 0.09 | -0.02 | -0.25** | 0.07 | -0.07 | |
| 7. Number of pain sites | 0.09 | 0.37** | -0.05 | 0.09 | 0.20** | -0.08 | -0.11 | 0.08 |
Point-biserial correlations were calculated for all correlations involving the dichotomous variables ethnicity, gender, and education; all others are Pearson product moment correlations. Pain severity=pain severity subscale of the Multidimensional Pain Inventory. CAPS total=total score on the Clinician Administered PTSD Scale.
p<0.05
p<0.001.
Model fit was evaluated using the criteria set forth by Hu and Bentler (1999), which suggests that for a model to have a good fit, the comparative fit index (CFI) and the Tucker-Lewis index (TLI) should be greater than 0.95, and the root mean square error of approximation (RMSEA) should be less than 0.06 (Hu and Bentler, 1999). Kline (1998) also suggests that a good fitting model generally has a χ2/df of less than 3.0.
In order to further elaborate on the relationship between variables included in the models, direct, indirect, and total effects were examined (Baron and Kenny, 1986; Kline, 1998). Direct effects were calculated in order to determine the association of trauma sequelae (PTSD and pain severity) with disability (psychosocial or physical impairment). Indirect effects were calculated in an effort to describe the extent to which life control mediates the relationship between trauma sequelae and disability. Total effects were calculated to quantify the full association of trauma sequelae (including direct and indirect effects) with disability.
2. Results
2.1. Psychosocial impairment
With respect to the model that examined psychosocial impairment, the overall fit indices suggested a good fit: CFI=0.98; TLI=0.96; RMSEA=0.04; χ2(22)=27.24, n.s.; χ2/df=1.24. This model accounted for 32% of the variance in life control and 53.3% of the variance in psychosocial impairment (Fig. 1). As shown in Fig. 1, results revealed a significant, positive association between pain severity and psychosocial impairment (β=0.24, p<0.001) and between PTSD symptoms and psychosocial impairment (β=0.33, p<0.001).
Fig. 1.
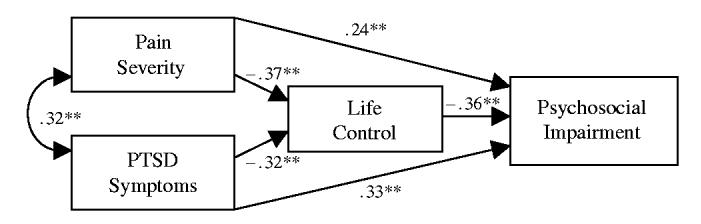
Model for psychosocial impairment with standardized parameter estimates. The standardized parameter estimates for the demographic covariates are not depicted. They are as follows: Age and pain severity β=0.12, n.s.; pain sites and pain severity β=0.31, p<0.001; pain sites and ethnicity β=0.19, p<0.05; Education and pain severity β= -0.19, p<0.05; education and PTSD symptoms β= -0.13, n.s.; ethnicity and PTSD symptoms β=0.13, n.s.; ethnicity and months since MVA β= -0.26, p<0.001; months since MVA and PTSD symptoms β= -0.28, p<0.001. *p<0.05, **p<.001.
In order to address the first aim of the study in this model, the direct effects of PTSD symptoms and pain severity on psychosocial impairment were calculated. This provided an evaluation of the relationship between trauma sequelae and psychosocial impairment. The direct effects indicated that PTSD symptoms and pain severity were significantly related to psychosocial impairment (Table 3).
Table 3.
Standardized direct, indirect, and total effects for models of psychosocial and physical impairment
| Exogenous variable | Endogenous variable |
|
|---|---|---|
| Psychosocial impairment | Physical impairment | |
| Pain severity | ||
| Direct effect | 0.24* | 0.51* |
| Indirect effect via life control | 0.14* | 0.07** |
| Total effect | 0.38* | 0.58* |
| PTSD symptoms | ||
| Direct effect | 0.33* | -0.03 |
| Indirect effect via life control | 0.12* | N/A |
| Total effect | 0.45* | 0.03 |
p<0.05
p<0.001.
The second aim of the study was evaluated in this model by calculating the indirect effect of pain severity on psychosocial impairment via life control and the indirect effect of PTSD symptoms on psychosocial impairment via life control. These analyses were used to examine whether life control mediates the relationship between trauma sequelae and psychosocial impairment. As shown in Table 3, there was a significant indirect effect of pain severity on psychosocial impairment via life control (z=4.10, p<0.001), and of PTSD symptoms on psychosocial impairment via life control (z=3.81, p<0.001). These findings suggest that perceived life control is one path by which symptoms of PTSD and pain are associated with psychosocial impairment.
The calculation of the total effects for this model took into account the direct effect of pain severity and PTSD symptoms on psychosocial impairment as well as the indirect effects via life control. Results showed a significant total effect of pain severity on psychosocial impairment, and a significant total effect of PTSD symptoms on psychosocial impairment (see Table 3). These results suggest that PTSD symptomatology and pain are both related to psychosocial impairment following a MVA.
2.2. Physical impairment
The overall fit indices of the model that examined physical impairment suggested a good fit: CFI=0.96; TLI=0.92; RMSEA=0.05; χ2(22)=30.84, n.s.; χ2/df = 1.40. This model accounted for 31.4% of the variance in life control and 37.7% of the variance in physical impairment (Fig. 2). As shown in Fig. 2, results revealed a significant, positive association between pain severity and physical impairment (β=0.51, p<0.001). However, the path from PTSD symptoms to physical impairment was not significant (β=-0.03, n.s.).
Fig. 2.
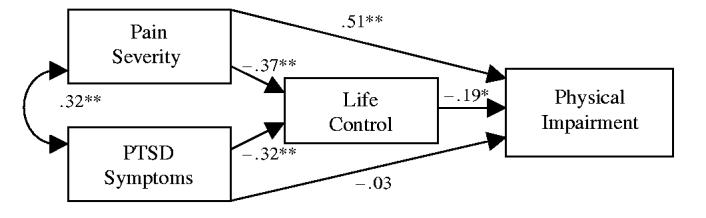
Model for physical impairment with standardized parameter estimates. The standardized parameter estimates for the demographic covariates are not depicted. They are as follows: age and pain severity β=0.12, n.s.; pain sites and pain severity β=0.30, p<0.001; pain sites and ethnicity β=0.19, p<0.05; education and pain severity β= -0.19, p<0.05; Education and PTSD symptoms β= -0.14, n.s.; ethnicity and PTSD symptoms β=0.13, n.s.; ethnicity and months since MVA β= -0.26, p<0.001; months since MVA and PTSD symptoms β= -0.28, p<0.001. *p<0.05, **p<0.001.
In order to address the first aim of the study in the physical impairment model, the direct effects of PTSD symptoms and pain severity on physical impairment were calculated. This provided an evaluation of the relationship between trauma sequelae (i.e. pain and PTSD symptoms) and physical impairment. Results suggested that pain severity alone was directly related to physical impairment. PTSD symptoms were not significantly related to physical impairment (Table 3).
The second aim of the study was evaluated in the physical impairment model by calculating the indirect effect of pain severity on physical impairment via life control. This analysis was used to examine whether life control mediates the relationship between pain severity and physical impairment. The indirect effect of PTSD symptoms on physical impairment via life control was not calculated because the direct and total effect of PTSD symptoms on physical impairment were found to be non-significant (Table 3). However, as shown in Table 3, there was a significant indirect effect of pain severity on physical impairment via life control (z=-2.42, p<0.05).
The total effect of pain severity and physical impairment was calculated in order to evaluate the entire relationship between these variables. This calculation took into the account the direct effect of pain severity on physical impairment as well as the indirect effects via life control. Results showed that there was a significant total effect of pain severity on physical impairment (see Table 3). These results suggest that pain is related to physical impairment following a MVA.
3. Discussion
This study showed that PTSD symptomatology and pain severity were related to impairment in psychosocial functioning, specifically social interaction, emotional behavior, and communication. However, after controlling for the relationship between PTSD symptoms and pain, only pain was significantly related to physical impairment (e.g. mobility, ambulation). Interestingly, perceived life control was found to be one mechanism by which PTSD symptomatology and pain severity were indirectly associated with psychosocial impairment and by which pain severity was indirectly related to physical impairment.
Based on these findings, it appeared that psychosocial and physical impairment were associated with different aspects of post-trauma problems. Psychosocial impairment was directly related to both PTSD symptom severity and pain while physical impairment was only related to pain severity. Although previous studies have suggested that PTSD and pain both are jointly related to affective distress and physical disability (Beck et al., 2003; Beckham et al., 1997; Geisser et al., 1996), no previous study has examined the unique predictors of psychosocial versus physical impairment. Although some authors have speculated that pain and PTSD operate synergistically (Sharp and Harvey, 2001), the current results suggest that this may only be the case with respect to psychosocial difficulties and not with respect to physical functioning difficulties. This helps to inform Sharp and Harvey’s (2001) model of PTSD and pain, which hypothesizes that there may be a number of common factors shared by both conditions that influence their maintenance. For example, the anxiety associated with PTSD symptomatology might increase perceptions of pain, leading to reduced physical activity and increased disability. Likewise, because pain is a continual reminder of the traumatic event, individuals with PTSD and pain might avoid activities that they believe will cause pain, which might lead to increased physical disability. Because this study failed to find an association between PTSD symptom severity and physical impairment, it seems as if the components that might be related to the co-occurrence of these conditions do not necessarily affect physical impairment.
Additionally, one’s perception of life control appeared to be an important factor in understanding the relationship among these constructs. In particular, greater levels of PTSD symptomatology and pain were associated with less perceived control, which was associated with greater psychosocial impairment. The physical functioning model revealed that more severe pain was associated with diminished perceived control, which was related to greater physical disability. Given the cross-sectional nature of the data, it is not possible to establish causal relationships in the current study; however, it appears that one’s general perception of life control has an important role in his or her functioning. In future studies, longitudinal data can help to determine whether diminished life control is a cause or a consequence of PTSD and pain symptomatology. It is possible that these variables influence one another in a feed-forward fashion to contribute to impairment and disability. It is important to note that the current study examined general perceptions of control, as opposed to perceived control during the trauma or controllability over future events, further supporting the idea that general perceptions of control are important in understanding functioning in the aftermath of a traumatic event (e.g. Bolstad and Zinbarg, 1997; Kushner et al., 1992; Regehr et al., 1999).
Taken together, these results provide evidence for two possible pathways that explain the association of PTSD symptoms and pain with psychosocial and physical disability: a direct pathway and an indirect pathway via perceptions of life control. The recognition of these two pathways has potential treatment implications. Treatments that are designed to address post-trauma functioning may want to consider how PTSD symptoms and pain jointly contribute to psychosocial outcomes. However, treatments whose primary function is to reduce physical disability might want to focus their efforts on reducing a person’s perceptions of pain because the current study’s results suggest that pain severity alone relates to physical impairment. Furthermore, addressing a client’s perceptions of control over his or her life may be an indirect way to improve both psychosocial and physical functioning impairments.
Although this study addresses a gap in the literature on pain and PTSD, it has two main limitations: the cross-sectional nature of the data, and the homogeneity of the sample. First, because all data was gathered at one time point, conclusions about the causal nature of the relationships found in this study cannot be made. The observed relationships revealed in this study may provide a basis for future work aimed at determining the causality of these relationships. Longitudinal data would be needed to address this issue in future studies.
Second, given the relative homogeneity of the sample, the observed relationships revealed in the results may be overestimated, and the generalizability of the findings may be limited (Tabachnick and Fidell, 2001). For example, all participants experienced a traumatic MVA, which limits conclusions drawn from the results to a MVA population. It may be that the relationship between trauma sequelae and impairment varies based on the type of trauma experienced (e.g. combat exposure, assault). Also, this sample was primarily help-seeking, that is, they contacted the project because they were experiencing distress due to psychological and/or physical difficulties. This might limit the generalizability of the findings to distressed individuals. Furthermore, the demographics of the sample are reflective of a primarily white, female population. It may be that the overwhelmingly female representation in the study influenced some of the results, such as the non-significant relationship between gender and PTSD symptoms, which prior literature would suggest should be present (Blanchard and Hickling, 2004). However, although this sample appears to be unique, it is in fact representative of a typical MVA, help-seeking population. In general, more women experience PTSD following a traumatic event (Kessler et al., 1995), and white females tend to be most highly represented in other samples of MVA survivors (Blanchard and Hickling, 2004). Thus, this study provides relevant information for better understanding the impairments suffered by individuals who may be seeking help with pain and post-trauma symptoms following a MVA. However, future research in the area of pain and PTSD will help to clarify whether relationships demonstrated in this study also hold for heterogeneous samples and samples drawn from other trauma populations.
In conclusion, this study found that PTSD symptoms and pain severity were related to impairment in psychosocial functioning, however, only pain was significantly related to physical impairment. Perceptions of life control were shown to further explain these interrelationships. The current study provided support for one factor, perceptions of life control, which facilitates an indirect relationship between symptoms of PTSD and pain and functioning. Future work in this area would benefit from exploring other factors, such as cognitive attributions, perceptions of social support, or coping styles, which might also be important in understanding psychosocial and physical disability.
Acknowledgements
This report was the basis of a prelim at the University at Buffalo—SUNY by Sarah Palyo under the direction of J. Gayle Beck. We express appreciation for helpful comments to Jennifer Read who was the other reader on Ms. Palyo’s committee.
Footnotes
E-mail addresses: spalyo@buffalo.edu (S.A. Palyo), jgbeck@buffalo.edu (J.G. Beck).
This work was supported in part by grants from the National Institute of Mental Health (MH64777) and University at Buffalo (IRCAF 24623).
References
- American Psychiatric Association . The diagnostic and statistical manual of mental disorders. Washington, DC: 2000. [Google Scholar]
- Asmundson GJ, Norton GR, Allerdings MD, Norton PJ, Larsen DK. Posttraumatic stress disorder and work-related injury. J Anxiety Disord. 1998;12:57–69. doi: 10.1016/s0887-6185(97)00049-2. [DOI] [PubMed] [Google Scholar]
- Baron RM, Kenny DA. The moderator-mediator variable distinction in social psychological research: conceptual, strategic, and statistical considerations. J Pers Soc Psychol. 1986;51:1173–82. doi: 10.1037//0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- Beck JG, Gudmundsdottir B, Shipherd JC. PTSD and emotional distress symptoms measured after a motor vehicle accident: relationships with pain coping profiles. J Psychopathol Behav Assess. 2003;25:219–27. doi: 10.1023/a:1025817111293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beckham JC, Crawford AL, Feldman ME, Kirby AC, Hertzberg MA, Davidson JT, Davidson JR, Moore SD. Chronic posttraumatic stress disorder and chronic pain in vietnam combat veterans. J Psychosom Res. 1997;43:379–89. doi: 10.1016/s0022-3999(97)00129-3. [DOI] [PubMed] [Google Scholar]
- Benedikt RA, Kolb LC. Preliminary findings on chronic pain and posttraumatic stress disorder. Am J Psychiatry. 1986;143:908–10. doi: 10.1176/ajp.143.7.908. [DOI] [PubMed] [Google Scholar]
- Bergner M, Bobbitt RA, Kressel S, Pollard WE, Gilson BS, Morris JR. The sickness impact profile: conceptual formulation and methodology for the development of a health status measure. Int J Health Serv. 1976;6:393–415. doi: 10.2190/RHE0-GGH4-410W-LA17. [DOI] [PubMed] [Google Scholar]
- Bergner M, Bobbitt RA, Carter WB, Gilson BS. The sickness impact profile: development and final revision of a health status measure. Med Care. 1981;19:787–805. doi: 10.1097/00005650-198108000-00001. [DOI] [PubMed] [Google Scholar]
- Blake D, Weathers F, Nagy L, Kaloupek D, Klauminzer G, Charney D, Keane TM. Clinician administered PTSD scale (CAPS) National Center for Post-Traumatic Stress Disorder, Behavioral Science Division; Boston, MA: 1990. [Google Scholar]
- Blanchard EB, Hickling EJ. After the crash: psychological assessment and treatment of survivors of motor vehicle accidents. American Psychological Association; Washington, DC: 2004. [Google Scholar]
- Bolstad BR, Zinbarg RE. Sexual victimization, generalized perception of control, and Posttraumatic Stress Disorder symptom severity. J Anxiety Disord. 1997;11:523–40. doi: 10.1016/s0887-6185(97)00028-5. [DOI] [PubMed] [Google Scholar]
- Casella L, Motta RW. Comparison of characteristics of Vietnam veterans with and without posttraumatic stress disorder. Psychol Rep. 1990;67:595–605. doi: 10.2466/pr0.1990.67.2.595. [DOI] [PubMed] [Google Scholar]
- Chibnall JT, Duckro PN. Post-traumatic stress disorder in chronic post-traumatic headache patients. Headache. 1994;34:357–61. doi: 10.1111/j.1526-4610.1994.hed3406357.x. [DOI] [PubMed] [Google Scholar]
- Deyo RA. Comparative validity of the Sickness Impact Profile and shorter scales for functional assessment in low-back pain. Spine. 1986;11:951–4. doi: 10.1097/00007632-198611000-00017. [DOI] [PubMed] [Google Scholar]
- Geisser ME, Roth RS, Bachman JE, Eckert TA. The relationship between symptoms of Post-traumatic Stress Disorder and pain, affective disturbance and disability among patients with accident and non-accident related pain. Pain. 1996;66:207–14. doi: 10.1016/0304-3959(96)03038-2. [DOI] [PubMed] [Google Scholar]
- Hickling EJ, Blanchard EB. Post-traumatic stress disorder and motor vehicle accidents. J Anxiety Disord. 1992;6:285–91. [Google Scholar]
- Hickling EJ, Blanchard EB, Silverman DJ, Schwarz SP. Motor vehicle accidents, headaches and post-traumatic stress disorder: assessment findings in a consecutive series. Headache. 1992;32:147–51. doi: 10.1111/j.1526-4610.1992.hed3203147.x. [DOI] [PubMed] [Google Scholar]
- Hu L, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: conventional criteria versus new alternatives. Struct Equation Mod. 1999;6:1–55. [Google Scholar]
- Kerns RD, Turk DC, Rudy TE. The West Haven Yale multidimensional pain inventory (WHYMPI) Pain. 1985;23:345–56. doi: 10.1016/0304-3959(85)90004-1. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Sonnega A, Bromet E, Hughes M, Nelson CB. Post-traumatic stress disorder in the National Comorbidity Survey. Arch Gen Psychiatry. 1995;52:1048–60. doi: 10.1001/archpsyc.1995.03950240066012. [DOI] [PubMed] [Google Scholar]
- Kline RB. Principles and practice of structural equation modeling. The Guilford Press; New York: 1998. [Google Scholar]
- Kushner MG, Riggs DS, Foa EB, Miller SM. Perceived controllability and the development of Posttraumatic Stress Disorder (PTSD) in crime victims. Behav Res Ther. 1992;31:105–10. doi: 10.1016/0005-7967(93)90048-y. [DOI] [PubMed] [Google Scholar]
- LaChapelle DL, Hadjistavrophoulos HD, McCreary DR, Asmundson GJ. Contributions of pain-related adjustment and perceptions of control to coping strategy use among cervical sprain patients. Eur J Pain. 2001;5:405–13. doi: 10.1053/eujp.2001.0261. [DOI] [PubMed] [Google Scholar]
- Lazarus RS, Folkman S. Stress, appraisal and coping. Springer; New York: 1984. [Google Scholar]
- Regehr CR, Cadell S, Jansen K. Perceptions of control and long-term recovery from rape. Am J Orthopsychiatry. 1999;69:110–5. doi: 10.1037/h0080386. [DOI] [PubMed] [Google Scholar]
- Rudy TE. Multiaxial assessment of pain, multidimensional pain inventory: computer program user’s manual version 2.0. Pittsburgh, PA: 1989. [Google Scholar]
- Rudy TE, Turk DC, Zaki HS, Curtin HD. An empirical taxometric alternative to traditional classification of temporomandibular disorders. Pain. 1989;36:311–20. doi: 10.1016/0304-3959(89)90090-0. [DOI] [PubMed] [Google Scholar]
- Sharp TJ, Harvey AG. Chronic pain and posttraumatic stress disorder: mutual maintenance? Clin Psychol Rev. 2001;21:857–77. doi: 10.1016/s0272-7358(00)00071-4. [DOI] [PubMed] [Google Scholar]
- Spinhoven P, Ter Kuile MM, Lissen AC, Gazendam B. Pain coping strategies in a Dutch population of chronic low back pain patients. Pain. 1989;37:77–83. doi: 10.1016/0304-3959(89)90155-3. [DOI] [PubMed] [Google Scholar]
- Tabachnick BG, Fidell LS. Using multivariate statistics. Allyn and Bacon; Boston, MA: 2001. [Google Scholar]
- Turk DC, Rudy TE. Toward an empirically derived taxonomy of chronic pain patients: integration of psychological assessment data. J Consulting Clin Psychol. 1988;56:233–8. doi: 10.1037//0022-006x.56.2.233. [DOI] [PubMed] [Google Scholar]
- Turk DC, Okifuji A, Scharff L. Chronic pain and depression: role of perceived impact and perceived control in different age cohorts. Pain. 1995;61:93–101. doi: 10.1016/0304-3959(94)00167-D. [DOI] [PubMed] [Google Scholar]
- Weathers FW, Keane T, Davidson J. Clinician-administered PTSD scale: a review of the first ten years of research. Depress Anxiety. 2001;13:132–56. doi: 10.1002/da.1029. [DOI] [PubMed] [Google Scholar]


