Abstract
Objective To determine the efficacy and safety of the anticoagulant fondaparinux in older acute medical inpatients at moderate to high risk of venous thromboembolism.
Design Double blind randomised placebo controlled trial.
Setting 35 centres in eight countries.
Participants 849 medical patients aged 60 or more admitted to hospital for congestive heart failure, acute respiratory illness in the presence of chronic lung disease, or acute infectious or inflammatory disease and expected to remain in bed for at least four days.
Interventions 2.5 mg fondaparinux or placebo subcutaneously once daily for six to 14 days.
Outcome measure The primary efficacy outcome was venous thromboembolism detected by routine bilateral venography along with symptomatic venous thromboembolism up to day 15. Secondary outcomes were bleeding and death. Patients were followed up at one month.
Results 425 patients in the fondaparinux group and 414 patients in the placebo group were evaluable for safety analysis (10 were not treated). 644 patients (75.9%) were available for the primary efficacy analysis. Venous thrombembolism was detected in 5.6% (18/321) of patients treated with fondaparinux and 10.5% (34/323) of patients given placebo, a relative risk reduction of 46.7% (95% confidence interval 7.7% to 69.3%). Symptomatic venous thromboembolism occurred in five patients in the placebo group and none in the fondaparinux group (P = 0.029). Major bleeding occurred in one patient (0.2%) in each group. At the end of follow-up, 14 patients in the fondaparinux group (3.3%) and 25 in the placebo group (6.0%) had died.
Conclusion Fondaparinux is effective in the prevention of asymptomatic and symptomatic venous thromboembolic events in older acute medical patients. The frequency of major bleeding was similar for both fondaparinux and placebo treated patients.
Introduction
Many acutely ill medical patients, such as those with congestive heart failure, respiratory illness, and infectious or inflammatory disease, are potentially at risk of venous thromboembolism.1-5 Most patients who die from pulmonary embolism as a complication of being admitted to hospital are medical patients.6 Despite these observations, uncertainty remains about the baseline risk for venous thromboembolism as well as the effectiveness of thromboprophylaxis in these patients. This uncertainty has limited the systematic application of thromboprophylaxis in this population.7-11 So far only one placebo controlled study has been reported that used bilateral venography to evaluate the presence of venous thromboembolism.12
Fondaparinux, a synthetic, selective inhibitor of factor Xa, effectively reduces postoperative venous thromboembolism after orthopaedic surgery.13 We carried out a placebo controlled study of fondaparinux in acute medical patients to determine its efficacy and to better document and understand the risk for thrombosis in this large patient group.
Methods
We considered for inclusion in our study acutely ill patients with congestive heart failure class III/IV (New York Heart Association classification), acute respiratory illness in the presence of chronic lung disease, or clinically diagnosed acute infections or inflammatory disorders such as arthritis, connective tissue diseases, or inflammatory bowel disease. Patients had to be at least 60 years old and expected to remain in bed for at least four days.
Exclusion criteria were a high risk for bleeding; acute bacterial endocarditis; cerebral metastasis; recent haemorrhagic or ischaemic stroke; brain, spinal, or ophthalmological surgery; an indwelling intrathecal or epidural catheter; a serum creatinine level > 180 μmol/l in a well hydrated patient; documented hypersensitivity to contrast media; anticipated intubation for more than 24 hours; use of antithrombotics within 48 hours before randomisation; an indication for anticoagulant prophylaxis or therapy; or life expectancy of less than one month. Written informed consent was obtained from the patients before randomisation.
Study design
Patients were randomly assigned by investigators to receive once daily subcutaneous injections of either 2.5 mg fondaparinux sodium (Arixtra; GlaxoSmithKline) or placebo, within 48 hours of admission to hospital. Randomisation was carried out using a predefined central randomisation list, balanced in blocks of four. The code was revealed to the investigators on completion of the study.
Treatment was scheduled until days 6 to 14, and the primary efficacy outcome was deep vein thrombosis detected by routine bilateral venography on days 6 to 15 along with symptomatic venous thromboembolism up to day 15. Patients were examined for deep vein thrombosis by routine bilateral ascending venography of the legs between days 6 and 15 and no more than one calendar day after the last administration of study drug, or earlier if deep vein thrombosis was clinically suspected. Symptomatic pulmonary embolism was to be confirmed by a high probability lung scan, pulmonary angiography, or helical computed tomography, or at autopsy.14 In the absence of autopsy, death was classified due to pulmonary embolism if it occurred suddenly and was otherwise unexplained. Patients were followed up for one month: venous thromboembolism, bleeding, or death was recorded. Extended prophylaxis was at the discretion of the investigators.
Study drugs
Study drugs were provided in identical boxes, consisting of 15 prefilled single dose syringes, each containing either active drug (2.5 mg fondaparinux sodium in 0.5 ml saline) or placebo (0.5 ml isotonic saline). Investigators were blinded to treatment assignment for the duration of the study.
The use of aspirin or non-steroidal anti-inflammatory drugs was discouraged. Graduated compression stockings and physiotherapy were allowed.
Outcome measures
The primary efficacy outcome was the composite of deep vein thrombosis detected by routine bilateral venography on days 6 to 15, and symptomatic venous thromboembolism up to day 15.
The primary safety outcome was major bleeding during treatment and two days thereafter and was defined as fatal bleeding, bleeding in a critical location, bleeding leading to surgical intervention, or overt bleeding associated with a drop in haemoglobin concentration of ≥ 20 g/l or leading to transfusion of two or more units of red blood cells. Secondary safety outcomes were death and minor bleeding. Minor bleeding was defined as clinically relevant overt bleeding not meeting the criteria for major bleeding.
Efficacy and safety outcomes were adjudicated by a central independent committee whose members were unaware of treatment assignment. Accumulated safety data were regularly reviewed by an independent committee.
Statistical analysis
On the basis of the single reported placebo controlled study that used venography, we expected a venous thromboembolism rate in the placebo group of between 10% and 14%.12 We calculated the sample size using a two sided type one error of 5%, a power of 85%, an incidence of venous thromboembolism of 12% in the placebo group, and an assumed risk reduction of 60%. Based on the expected 30% of patients with no or inadequate venograms, our study required at least 800 patients.
The primary efficacy analysis was carried out on all randomised patients with an available efficacy assessment up to day 15. The safety analyses included all patients who had received at least one dose of study drug. We carried out the analyses using a two sided Fisher's exact test and considered a P value of < 0.05 as statistically significant. We calculated relative risk reductions, with 95% confidence intervals. Incidences of the primary efficacy outcome were also calculated according to predefined categorical covariates (congestive heart failure, acute respiratory illness, or acute infectious or inflammatory disease separately). We compared survival rates using the log rank test.
Results
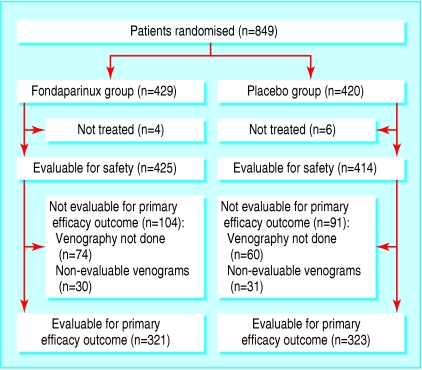
Between March 2002 and January 2003, 849 patients from 35 centres in eight countries were randomised to our study (fig 1). Four patients in the fondaparinux group and six in the placebo group were not treated. All treated patients received the allocated study treatment. Thus 425 patients in the fondaparinux group and 414 in the placebo group were evaluable for safety analysis. Treatment lasted for a median of 7 days (range 1-15 days) in the fondaparinux group and 7 days (range 1-13 days) in the placebo group. A total of 644 patients (75.9%) were available for the primary efficacy analysis. Reasons for ineligibility for this analysis were failure to obtain a venogram (16.0%) or an inadequate venogram (7.3%). Baseline characteristics were similar between the two groups (table 1).
Fig 1.
Flow of patients through trial
Table 1.
Baseline characteristics of older medical patients randomised to the anticoagulant fondaparinux or placebo. Values are numbers (percentages) unless stated otherwise
| Characteristic | Fondaparinux group (n=429) | Placebo group (n=420) |
|---|---|---|
| Mean (SD) age (years), range | 75.0 (8.3), 60 to 93 | 74.4 (8.3), 53 to 96* |
| Men | 174 (40.6) | 186 (44.3) |
| Women | 255 (59.4) | 234 (55.7) |
| Mean (SD) weight (kg), range | 70.1 (15.2), 32 to 111 | 70.1 (16.8), 35 to 150 |
| Mean (SD) body mass index | 25.9 (5.5) | 25.8 (5.7) |
| Reason for admission to hospital: | ||
| Congestive heart failure (class III/IV)† | 106 (24.7) | 106 (25.2) |
| Acute respiratory disease | 74 (17.2) | 93 (22.1) |
| Acute infectious or inflammatory disease | 107 (24.9) | 107 (25.5) |
| More than one reason | 142 (33.1) | 114 (27.1) |
| Risk factors for venous thrombembolism: | ||
| Age ≥75 years | 223 (52.0) | 216 (51.4) |
| History of venous thrombembolism‡ | 18 (4.2) | 21 (5.0) |
| Previous or current cancer | 62 (14.5) | 69 (16.4) |
One patient recruited out of prespecified range in placebo group (enrolled at age 53) was not included in primary efficacy population.
According to New York Heart Association.
Deep vein thrombosis or pulmonary embolism.
Incidence of venous thromboembolism
Overall, 5.6% (18/321) of patients in the fondaparinux group and 10.5% (34/323) of patients in the placebo group had venous thrombembolism detected by routine bilateral venography and symptomatic venous thrombembolism up to day 15 (relative risk reduction 46.7%, 95% confidence interval 7.7% to 69.3%, P = 0.029: table 2). Consistent reductions were shown in the incidence of total, proximal, and distal deep vein thrombosis. Five fatal cases of pulmonary emboli occurred during the study, all in the placebo group. Two of the five were confirmed by autopsy, the others were assumed to be due to pulmonary emboli, as no other plausible cause was found.
Table 2.
Venous thromboembolic events in older (≥60 years) medical patients randomised to the anticoagulant fondaparinux or placebo. Values are numbers unless stated otherwise
| Primary efficacy outcome | Fondaparinux group | Placebo group |
|---|---|---|
| Venous thromboembolic events: | ||
| Any | 18 | 29 |
| Proximal deep vein thrombosis | 5 | 7 |
| Distal deep vein thrombosis | 13 | 22 |
| Symptomatic deep vein thrombosis | 0 | 0 |
| Non-fatal pulmonary embolism | 0 | 0 |
| Fatal pulmonary embolism | 0 | 5 |
| Total No (%) | 18/321 (5.6) | 34/323 (10.5) |
| No (%) of any symptomatic venous thrombembolism up to day 32: | ||
| Symptomatic deep vein thrombosis | 0 | 0 |
| Non-fatal pulmonary embolism | 1 | 4 |
| Fatal pulmonary embolism | 3 | 7 |
| Total No (%) | 4/429 (1) | 11/420 (3) |
The incidence of venous thrombembolism on venography and symptomatic venous thromboembolism was reduced in fondaparinux recipients with only congestive heart failure from 12.2% (10/82) to 9.0% (7/78), only acute respiratory illness from 5.5% (4/73) to 1.6% (1/63), only acute infectious or inflammatory disease from 11.4% (10/88) to 5.2% (4/77), and in patients with more than one reason for admission to hospital from 12.5% (10/80) to 5.8% (6/103).
Ten additional case of pulmonary embolism occurred during follow-up (four in the fondaparinux group). Of these, five were fatal (three in the fondaparinux group).
Safety outcomes
Major bleeding occurred in one patient (0.2%) in each group during the study, both related to overt bleeding and a drop in haemoglobin concentration of ≥ 20 g/l or transfusion of ≥ 2 units of blood (table 3). Minor bleeds were observed in 11 patients (2.6%) in the fondaparinux group and four (1.0%) in the placebo group.
Table 3.
Bleeding complications during study treatment of older (≥60 years) medical patients randomised to the anticoagulant fondaparinux or placebo
| Bleeding complication | Fondaparinux group (n=425) | Placebo group (n=414) |
|---|---|---|
| Major bleeding: | ||
| Fatal | 0 | 0 |
| Requiring surgical intervention | 0 | 0 |
| In a critical location | 0 | 0 |
| Overt bleeding plus a decrease in haemoglobin concentration ≥20 g/L (<48 hours) or transfusion of ≥2 units | 1 | 1 |
| Total No (%) | 1 (0.2) | 1 (0.2) |
| Minor bleeding | 11 (2.6) | 4 (1.0) |
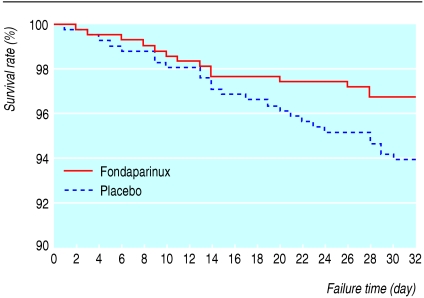
At one month, 14 (3.3%) patients in the fondaparinux group and 25 (6.0%) in the placebo group had died (P = 0.06) (fig 2, table 4).
Fig 2.
Survival estimates of older (≥60 years) acute medical patients treated with the anticoagulant fondaparinux or placebo. Log rank test on difference, P=0.06
Table 4.
Mortality up to day 32 in older (≥60 years) medical patients randomised to the anticoagulant fondaparinux or placebo
| Variable | Fondaparinux group (n=425) | Placebo group (n=414) |
|---|---|---|
| Death from any cause: | ||
| Fatal pulmonary embolism | 3 | 7 |
| Fatal bleeding* | 2 | 1 |
| Other causes | 9 | 17 |
| Total No (%) | 14 (3) | 25 (6) |
None occurred during study treatment.
Discussion
Daily subcutaneous injections of 2.5 mg fondaparinux for 6-14 days almost halved the rate of venous thromboembolism in older (≥ 60 years) acute medical patients admitted to hospital and requiring bed rest for heart, lung, or infectious or inflammatory disorders. No patients in the fondaparinux group and five in the placebo group had symptomatic fatal or non-fatal pulmonary embolism (P = 0.029). This reduction in venous thromboembolism was achieved with a minimal risk of major bleeding complications.
The relative risk reduction with fondaparinux in this double blind trial is consistent with results obtained by the high dosage low molecular weight heparin group in the placebo controlled study that used venography.12 These results add to the efficacy data supporting the general applicability of fondaparinux in the prevention as well as treatment of venous thromboembolism.13,14
The two aspects of our trial design that required greatest consideration were the clinical selection criteria for patient eligibility and the choice of placebo as comparator for fondaparinux. Older medical inpatients are a clinically diverse group. Thrombosis risks are well known after surgical interventions, but when our study was designed few recent studies had evaluated this risk in older people admitted to hospital with other acute or chronic conditions. Guidelines are available on prophylaxis in high risk inpatients but a need for universal prophylaxis has not been shown.15 No simple and easily applied selection criteria exist, and audits of general medical inpatients indicate that thrombosis prevention is not systematically applied or well grounded on risk factor assessment.7,10,16
Clinical events are not rare in medical patients (around 10% of deaths are due to pulmonary embolism17,18) but are in thromboprophylaxis studies.12,19 Clinical events are rare in this type of study as venogaphy is a sensitive and specific screening tool (more so than duplex Doppler ultrasound).
Venography is able to diagnose a higher frequency of deep vein thrombosis and smaller thrombi (presumably at an earlier stage). This technique is the ideal choice. Earlier and more accurate diagnosis has advantages for patients, with therapy starting before disease progression. As a result, clinical venous thrombembolism is rare in patients in whom venography studies are undertaken. We have concluded in favour of fondaparinux for two reasons, firstly because the surrogate end point of venographic deep vein thrombosis is strongly correlated to clinical deep vein thrombosis, clinical pulmonary embolism,16 and fatal pulmonary embolism.20 Secondly, we found a significant reduction in the clinical secondary end point of fatal pulmonary embolism. Similar conclusions have been made in studies in both this area and other areas on the basis of surrogate end points16,20 and by the American College of Chest Physicians.15 We do not think that our conclusions are unjustified on the basis of our findings.
What is already known on this topic
Most patients who die from pulmonary embolism as a complication of being admitted to hospital are medical patients
The effectiveness of thromboprophylaxis in these patients is uncertain
What this study adds
Fondaparinux is effective in the prevention of venous thromboembolism in acutely ill older (≥ 60 years) medical patients
We believed that our study could best contribute to the improvement of clinical practice if we applied simple and easily generalisable patient selection criteria to general medical inpatients (age ≥ 60 years, recent and continuing bed rest, and presence of a heart, lung, or infectious or inflammatory disorder), without further risk factor assessment. Since these criteria differed from those applied by others, our trial depended on a placebo group to measure baseline risk and risk reduction by active therapy.12,16 Investigators excluded patients prescribed or thought to need thromboprophylaxis. This might explain why the 10.5% thromboembolism rate at baseline observed was below previous levels of 20% in early studies and 15% in the placebo controlled trial.12,15 Therefore our simple case selection criteria defined a group of patients at moderate risk in which prophylaxis is clearly effective and justified. Hence we believe that our results can be generalised to all medical inpatients with these diagnoses. Moreover, these criteria can be easily applied and audited.
Our results are likely to be valid, because of randomised treatment assignment, the use of a double blind design, the objective diagnosis of venous thromboembolism, and the central adjudication of study outcomes while unaware of treatment assignment. These features minimised the potential for bias.
Two thirds of the clinically apparent events and half of the fatal pulmonary emboli were observed after the initial 6-14 day study period. This is similar to the observation in one trial and supports the need to evaluate extended prophylaxis in medical patients.12 Our results when added to those obtained with low molecular weight heparins12,15 establish the value of thromboprophylaxis in older medical inpatients at moderate to high risk of venous thromboembolism. The challenge now is to translate shown efficacy into effectiveness through local clinical practice guidelines, practice audit, and practice feedback.
Supplementary Material
 ARTEMIS group members are on bmj.com
ARTEMIS group members are on bmj.com
Contributors: All authors developed the protocol, interpreted the data, and wrote the manuscript. MHP supervised the statistics. JFME and AWAL ensured the protocol adhered to guidelines issued by the European Agency for the Evaluation of Medicinal Products and Food and Drug Administration, recruited the clinical investigators who treated the patients, and gathered data. ATC is guarantor for the paper.
Funding: Sanofi-Synthelabo (France) and NV Organon (Netherlands) sponsored the study and carried out on-site monitoring of all participants. The steering committee had the final responsibility for the study protocol, case report forms, statistical analysis plan, progress of the study and analysis, as well as the reporting of the data. The sponsors had an opportunity to comment on the manuscripts before submission, but the final version was the sole responsibility of the authors.
Competing interests: ATC, BLD, ASG, MRL, WT, and AGGT participated as investigators, consultants, or both for NV Organon and Sanofi-Synthelabo. JFME and AWAL are employees of NV Organon. BLD has served as an investigator or consultant for AstraZeneca, Bristol-Myers Squibb, Boehringer Ingelheim, and Pharmacia. ASG has served as an investigator, consultant, or advisory board member for Bristol-Myers Squibb, AstraZeneca, Aventis, Bayer, and Progen. MRL has served as an investigator and advisory board member for AstraZeneca, Britol-Myers Squibb, Mitsubishi Pharma Europe, Yamanouchi Pharma, and Bayer. AGGT is a consultant for Bristol-Myers Squibb.
Ethical approval: The institutional review boards of each centre approved the protocol.
References
- 1.Anderson FA Jr, Wheeler HB, Goldberg RJ, Hosmer DW, Patwardhan NA, Jovanovic B, et al. A population-based perspective of the hospital incidence and case-fatality rates of deep vein thrombosis and pulmonary embolism. The Worcester DVT study. Arch Intern Med 1991;151: 933-8. [PubMed] [Google Scholar]
- 2.Kniffin WD Jr, Baron JA, Barrett J, Birkmeyer JD, Anderson FA Jr. The epidemiology of diagnosed pulmonary embolism and deep venous thrombosis in the elderly. Arch Intern Med 1994;154: 861-6. [PubMed] [Google Scholar]
- 3.Weinmann EE, Salzman EW. Deep-vein thrombosis. N Engl J Med 1994;331: 1630-41. [DOI] [PubMed] [Google Scholar]
- 4.Heit JA, O'Fallon WM, Petterson TM, Lohse CM, Silverstein MD, Mohr DN, et al. Relative impact of risk factors for deep vein thrombosis and pulmonary embolism: a population-based study. Arch Intern Med 2002;162: 1245-8. [DOI] [PubMed] [Google Scholar]
- 5.Baglin TP, White K, Charles A. Fatal pulmonary embolism in hospitalised medical patients. J Clin Pathol 1997;50: 609-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cohen AT, Edmondson RA, Phillips MJ, Ward VP, Kakkar VV. The changing pattern of venous thrombembolic disease. Haemostasis 1996;26: 65-71. [DOI] [PubMed] [Google Scholar]
- 7.Ageno W, Squizzato A, Ambrosini F, Dentali F, Marchesi C, Mera V, et al. Thrombosis prophylaxis in medical patients: a retrospective review of clinical practice patterns. Haematologica 2002;87: 746-50. [PubMed] [Google Scholar]
- 8.Alikhan R, Wilmott R, Agrawal S, Desouza N, Gera A, Zaw H, et al. Use of thromboprophylaxis in nonsurgical patients: survey of a London teaching hospital. Blood 2001:98: 271a (abstract 1142). [Google Scholar]
- 9.Cohen AT. Venous thromboembolic disease management of the nonsurgical moderate- and high-risk patient. Semin Hematol 2000;37(suppl.5): 19-22. [DOI] [PubMed] [Google Scholar]
- 10.Mismetti P, Laporte S. Thromboprophylaxis in acute medical patients: need for an implementation strategy. Haematologica 2002;87: 673-5. [PubMed] [Google Scholar]
- 11.Hampton KK. Venous thromboembolic risk and prevention in acute medical illness. Int J Clin Pract 2003;57: 424-7. [PubMed] [Google Scholar]
- 12.Samama MM, Cohen AT, Darmon JY, Desjardins L, Eldor A, Janbon C, et al. A comparison of enoxaparin with placebo for the prevention of venous thromboembolism in acutely ill patients. N Engl J Med 1999;341: 793-800. [DOI] [PubMed] [Google Scholar]
- 13.Turpie AGG, Bauer KA, Eriksson BI, Lassen MR. Fondaparinux vs enoxaparin for the prevention of venous thromboembolism in major orthopedic surgery. A meta-analysis of 4 randomized double-blind studies. Arch Intern Med 2002;162: 1833-40. [DOI] [PubMed] [Google Scholar]
- 14.The Matisse Investigators. Subcutaneous fondaparinux versus intravenous unfractionated heparin in the initial treatment of pulmonary embolism. N Engl J Med 2003;349: 1695-702. [DOI] [PubMed] [Google Scholar]
- 15.Geerts WH, Heit JA, Clagett GP, Pineo GF, Colwell CW, Anderson FA Jr, et al. Prevention of venous thromboembolism. Chest 2001;119: S132-75. [DOI] [PubMed] [Google Scholar]
- 16.Mismetti P, Laporte-Simitsidis S, Tardy B, Cucherat M, Buchmuller A, Juillard-Delsart D, et al. Prevention of venous thromboembolism in internal medicine with unfractionated or low-molecular-weight heparins: a meta-analysis of randomized clinical trials. Thromb Haemost 2000;83: 14-9. [PubMed] [Google Scholar]
- 17.Lindblad B, Sternby NH, Bergqvist D. Incidence of venous thromboembolism verified by necropsy over 30 years. BMJ 1991;302: 709-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sandler DA, Martin JF. Autopsy proven pulmonary embolism in hospital patients: are we detecting enough deep vein thrombosis? J R Soc Med 1989;82: 203-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Leizorovicz A, Cohen AT, Turpie AG, Olsson CG, Vaitkus PT, Goldhaber SZ, et al. A randomized placebo controlled trial of dalteparin for the prevention of venous thromboembolism in 3706 acutely ill medical patients: the PREVENT medical thromboprophylaxis study trial. Circulation 2004;110: 8749. [DOI] [PubMed] [Google Scholar]
- 20.Collins R, Scrimgeour A, Yusuf S, Peto R. Reduction in fatal pulmonary embolism and venous thrombosis by perioperative administration of subcutaneous heparin. Overview of results of randomised trials in general, orthopaedic, and urologic surgery. N Engl J Med 1988;318: 1162-73. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.