Abstract
The efficiency with which different measles virus (MV) strains enter cells through the immune cell-specific protein SLAM (CD150) or other receptors, including the ubiquitous protein CD46, may influence their pathogenicity. We compared the cell entry efficiency of recombinant MV differing only in their attachment protein hemagglutinin (H). We constructed these viruses with an additional gene expressing an autofluorescent reporter protein to allow direct detection of every infected cell. A virus with a wild-type H protein entered cells through SLAM two to three times more efficiently than a virus with the H protein of the attenuated strain Edmonston, whereas cell entry efficiency through CD46 was lower. However, these subtle differences were amplified at the cell fusion stage because the wild-type H protein failed to fuse CD46-expressing cells. We also proved formally that a mutation in H protein residue 481 (asparagine to tyrosine) results in improved CD46-specific entry. To define the selective pressure exerted on that codon, we monitored its evolution in different H protein backgrounds and found that several passages in CD46-expressing Vero cells were necessary to shift it in the majority of the MV RNA. To verify the importance of these observations for human infections, we examined MV entry into peripheral blood mononuclear cells and observed that viruses with asparagine 481 H proteins infect these cells more efficiently.
Measles, caused by wild-type measles viruses (MV), is one of the leading causes of infant death in developing countries (6). The immune suppression that accompanies measles significantly enhances an individual's susceptibility to secondary infections, and these account for most of the morbidity and mortality associated with the disease (2). Vaccination with the live attenuated strain Edmonston (MV-Edm) prevents measles-related fatalities and only rarely results in the development of mild symptoms. Cell entry may have a central role in MV pathology; wild-type and attenuated MV strains may enter cells through different receptors.
CD46, a ubiquitous regulator of complement activation, was identified as an MV receptor by using the attenuated strain MV-Edm (8, 24). More recently, it was shown that the signaling lymphocytic activation molecule (SLAM) mediates cell entry of several wild-type MV strains (11, 13, 27, 38) and that three different morbilliviruses (MV, canine distemper virus, and rinderpest virus) all use SLAM (human, canine, and bovine, respectively) as a port of entry (39). High levels of SLAM are expressed by activated T cells, immature thymocytes, memory T cells, and a proportion of B cells (7, 35). SLAM expression has also been observed on dendritic cells (26, 29). Finally, monocytes freshly isolated from the peripheral blood express minimal amounts of SLAM but become SLAM positive after incubation with phytohemagglutinin, bacterial lipopolysaccharide, or MV (22).
The immune cell expression of SLAM and its conservation as a receptor between different morbilliviruses suggest that SLAM-dependent viral entry may be essential for the initial phase of MV dissemination. Nevertheless, CD46-dependent entry may also be relevant. It was recently shown that certain wild-type MV isolated on human lymphocytes may use CD46 as a cellular receptor (20). In any case, for the systemic infection phase, the ubiquitous protein CD46 may be necessary (8, 24).
The question of the relative importance of SLAM and CD46 for the entry and dissemination of wild-type and attenuated MV strains has not yet been addressed in detail; the existence of many differences between clinical MV isolates and tissue culture-adapted viruses makes the interpretation of comparative studies difficult. This difficulty has been overcome by the use of genetically modified MV. To allow the direct analysis of effects occurring at cell entry, recombinant MV with a constant Edmonston genomic backbone and variable envelope genes have been constructed (9, 15). These studies have confirmed the importance of the H gene for tropism but also suggested that receptor selectivity of cell entry may not be very strict; a recombinant MV with a wild-type H protein (wtF strain) was shown to enter Vero cells efficiently (15) even if these cells do not express SLAM.
To gain more insights on the determinants of MV entry efficiency, we have constructed MV recombinants having subtle differences in their H proteins. These differences included position 481, an asparagine in many wild-type strains but a tyrosine in MV-Edm, a strain that interacts efficiently with CD46 (1, 18). In addition, five nearby residues (positions 473 to 477) identified by a peptide-scanning approach (28) were also mutated, alone or in combination with position 481. As a control, the H gene of the wild-type strain wtF (15) was exchanged for the Edmonston H gene. All the recombinant viruses expressed an autofluorescent reporter protein to allow the visualization of infected cells independently of a cytopathic effect. The cell entry efficiency, fusion properties, and stability of these recombinant viruses were characterized in cell lines expressing either one or the other receptor and in human peripheral blood mononuclear cells (PBMC), important target cells for MV acute infections.
MATERIALS AND METHODS
Plasmids.
The parental plasmids pCG-H (4) and pCG-HwtF (15) code for the H proteins of the MV-Edm and the MV wild-type F strains, respectively. Plasmid pCG-HN481 was constructed by altering the MV-Edm TAC triplet, encoding tyrosine (Y, one-letter code), in position 481 of H to AAT, encoding asparagine (N), by using the Quick-Change system (Stratagene). In construct pCG-H5A, H residues 473 to 477 were mutated from IPRFK to AGAAA (one-letter amino acid code) by PCR amplification of two fragments with primer pairs inserting the altered sequences containing a unique NarI restriction site. The fragments were cloned into PacI- and SpeI-opened pCG-H. Primer pairs were 5′-GGTAGTTAATTAAAACTTAGG-3′ and 5′-TGCGGCGCCTGCCCCACTCCAATGTG-3′ for the PacI-NarI fragment and 5′-GCAGGCGCCGCAGCTGTTAGTCCCTACCTCTTC-3′ and 5′-CACACTAGTGGGTATGCC-3′ for the NarI-SpeI fragment (mutated sequence in bold, restriction sites underlined).
For construction of pCG-H5A+N481 the NarI-SpeI fragment was amplified by using pCG-HN481 as the template and primer 5′-GCAGGCGCCGCAGCTGTTAGTCCCAATCTCTTCA-3′ and cloned into NarI- and SpeI-opened pCG-H5A vector. The integrity of all constructs was verified by sequencing. The cDNAs encoding the various H proteins were transferred from the pCG constructs into a PacI- and SpeI-opened full-length infectious cDNA clone of the MV-Edm strain, p(+)MVgreen-H/XhEGF (34), encoding the green fluorescent protein (GFP) in an additional transcription unit upstream of N, resulting in p(+)MVgreen-H, p(+)MVgreen-H5A, p(+)MVgreen-HN481, p(+)MVgreen-H5A+N481, and p(+)MVgreen-HwtF.
Cell culture, transfections, and cell fusion assay.
Vero cells (American Type Culture Collection) and B95.8 cells (gift of Paul Rota, Centers for Disease Control, Atlanta, Ga.) were maintained in Dulbecco's modified Eagle's medium (Gibco) containing 10% fetal bovine serum, penicillin, and streptomycin (DMEM-10) at 37°C and 5% CO2. The rescue helper cell line 293-3-46 (30) was maintained in DMEM-10 supplemented with 1 mg of G418/ml. CHO-SLAM cells (38) were grown in RPMI 1640 (Gibco) containing 10% fetal bovine serum, penicillin, and streptomycin (RPMI-10) at 37°C and 5% CO2. CHO-SLAM cells were maintained in RPMI-10 medium with 1 mg of G418/ml.
Vero and CHO-SLAM cells were transiently transfected with Lipofectamine 2000 (Gibco) according to the manufacturer's protocol. For the cell fusion assay, target cells (105 cells in 15-mm-diameter wells) were cotransfected with 0.2 μg of pCG-F (4), 0.8 μg of plasmid DNA encoding the appropriate H, and 0.5 μg of plasmid DNA encoding the luciferase gene under the control of the bacteriophage T7 polymerase promoter, pTM-luc. This plasmid was constructed by subcloning the luciferase gene of pGL2-control (Promega) into pTM1 (23). For background determination, cells were transfected with 1 μg of pCG-H and 0.5 μg of pTM-luc. In parallel, separate 15-mm dishes of Vero and CHO-SLAM cells were infected with an optimal dose of an attenuated vaccinia virus expressing the T7 RNA polymerase (MVA-T7) in 0.5 ml of Opti-MEM I reduced-serum medium (Gibco). Four hours posttransfection or postinfection, both cell populations were trypsinized, combined in 1 ml of the appropriate medium, seeded into two 15-mm wells (0.5 ml/well), and incubated at 37°C for another 18 h.
Cell fusion-dependent luciferase expression was determined by using the luciferase assay system (Promega). Briefly, cells were incubated with 100 μl of lysis buffer (Promega) per well for 5 min at 4°C on a rocker, followed by 15 min of centrifugation of the lysate at 20,000 × g and 4°C. Then 20 μl of the postnuclear supernatants was transferred into a reader plate, and after addition of 100 μl of substrate, luciferase activity was determined in a luminometer. High background levels were sometimes noticed, especially when using CHO cells.
Surface biotinylation and Western blotting.
Vero and CHO-SLAM cells (105) were seeded into 15-mm dishes and transfected the next day with 1 μg of plasmid DNA encoding an H protein or mock transfected as a control. Twenty-four hours posttransfection, the cells were washed two times with 1 ml of ice-cold phosphate-buffered saline (PBS; Gibco), and surface proteins were labeled with 0.5 ml of ice-cold PBS containing 0.5 mg of biotin (Pierce) per ml for 30 min at 4°C. Unbound biotin was quenched by 30 min of incubation at 4°C in 1 ml of ice-cold PBS containing 10 mg of glycine per ml. The cells were lysed in 250 μl of radioimmunoprecipitation assay (RIPA) buffer (10 mM Tris [pH 7.8], 1% deoxycholate, 1% Triton X-100, 0.1% sodium dodecyl sulfate [SDS], 150 mM sodium chloride, protease inhibitor complete mix [Boehringer]) for 15 min at 4°C, and the lysates were subjected to centrifugation at 4°C for 15 min at 20,000 × g. Then 20 μl of the resulting postnuclear fraction was directly mixed with an equal volume of SDS loading buffer (130 mM Tris [pH 6.8], 20% glycerol, 10% SDS, 0.02% bromophenol blue, 10% β-mercaptoethanol).
These samples (10 μl) were fractionated on an SDS-polyacrylamide gel as indicated, blotted to polyvinylidene difluoride membranes (Millipore), probed with rabbit anti-H cytoplasmic tail (Hcyt) antiserum (5), and subjected to enhanced chemiluminescence detection (Amersham). For precipitation of biotinylated H protein, 50 μl of protein A-coated agarose beads (Bio-Rad) was washed three times in 1 ml of RIPA buffer and then mixed with 200 μl of the postnuclear supernatant and 1 μl of Hcyt antiserum, followed by overnight incubation at 4°C under rotation. The agarose beads were then washed three times in 1 ml of RIPA buffer prior to resuspension in 30 μl of loading buffer and boiling for 2 min at 100°C to elute bound proteins. Samples (20 μl) were fractionated on an SDS-polyacrylamide gel as indicated, blotted to polyvinylidene difluoride membranes (Millipore), and probed with peroxidase-coupled streptavidin, followed by enhanced chemiluminescence detection (Amersham).
Recovery, propagation, and titers of recombinant MV.
All viruses were recovered basically as described before (30). Three days posttransfection, the 293-3-46 cells were transferred to a 10-cm dish. The cells transfected with p(+)MVgreen-H and p(+)MVgreen-H5A were overlaid with Vero cells, and those transfected with p(+)MVgreen-HN481, p(+)MVgreen-H5A+N481, and p(+)MVgreen-HwtF were overlaid with B95.8 cells. Five to 10 days posttransfection, MVgreen-H and all its derivatives were recovered. To prepare virus stocks, Vero cells (80% confluent in a T75 flask) were infected with the viruses and incubated at 37°C until the majority of cells were positive for GFP expression. Virus was harvested in 2 ml of Opti-MEM I by two repeated freeze-thaw cycles and separated from cells by 3 min of centrifugation at 1,500 × g.
To verify the sequence of the stocks, total RNA was isolated from cells by using the RNeasy-kit from Qiagen and subjected to reverse transcription (RT) with random primers and the Superscript II RTase (Gibco) according to the manufacturer's protocol. PCR amplification was performed with the Expand High-Fidelity system (Roche Biochemicals) and primers 7996forward (5′-GCCTAATCTGAGCAGCAA-3′) and 9368reverse (5′-CTGTAAGCGTGAGGGAC-3′), binding to sequences in the H and the L gene, respectively. The resulting PCR fragment was directly sequenced over the relevant positions.
To assay the fusion competence of the recombinant MV, Vero and CHO-SLAM cells (105 in a 15-mm dish) were infected with 103 50% tissue culture infectious doses (TCID50) diluted in 0.5 ml of Opti-MEM I for 1 h at 37°C. The cells were washed with 1 ml of PBS and overlaid with 0.5 ml of the appropriate medium. Syncytium formation on Vero and CHO-SLAM cells was monitored by fluorescence microscopy.
Virus titers were determined by 50% endpoint dilution assays performed as follows. Serial dilutions (10-fold) of virus samples were made in DMEM-5, and 50 μl of each dilution was used to infect eight replicate 6-mm wells containing 7,500 Vero cells in 50 μl of DMEM-5 overnight at 37°C. The next day, 150 μl of DMEM-5 was added, and four days postinfection, the wells were scored for the presence of green light-emitting cells, and the log10 TCID50 was calculated by the method of Kärber (16).
Determination of the genomic stability of recombinant MV in Vero cells.
The identity of H codon 481 of viruses MVgreen-HN481, MVgreen-H5A+N481, and MVgreen-HwtF was determined upon propagation of these viruses in Vero cells. A 35-mm dish of Vero cells was initially infected at a multiplicity of infection (MOI) of 0.1 with the indicated viruses and incubated at 37°C. When more than 80% of all cells were infected, they were collected by scraping into 1 ml of fresh medium. Cell-associated virus was isolated by one freeze-thaw cycle, and the cell debris were removed by centrifugation. Then 50 μl of the clarified virus preparation was used for the next round of infection. At the indicated passage number, RNA was isolated from the infected cells, and RT-PCR was performed. The PCR fragment was then sequenced in both directions over the position of interest, and the percentage of revertants was determined from the electropherogram.
Determination of viral entry efficiency.
Vero and CHO-SLAM cells (105 in a 15-mm dish) were infected in duplicate with the indicated viruses at an MOI of 0.01 as determined on Vero cells. Two hours postinfection, the medium was replaced by DMEM-10 supplemented with a fusion-inhibiting peptide (Z-d-Phe-Phe-Gly-OH [Bachem]) at a concentration of 200 μM, and incubation at 37°C was continued for 28 h. Experiments were evaluated only if the duplicates had similar results by counting the number of infected cells expressing GFP in defined areas.
Preparation, infection, and analysis of human PBMC.
Blood (20 ml) was collected in heparin-coated tubes and diluted with an equal volume of warm PBS containing 2% fetal calf serum (PBS-2). The PBMC were separated from the erythrocytes by centrifugation of 20 ml of blood/PBS-2 on a Ficoll-Paque layer (25 ml; Pharmacia) at 800 × g for 30 min (Sorvall), transferred to a new 50-ml conical tube, and washed three times in 30 ml of PBS-2. The cell number was adjusted to 107 cells/ml by addition of RPMI-10 containing 2.5 μg of phytohemagglutinin (PHA; Sigma) and 1,000 U of human granulocyte-macrophage colony-stimulating factor (GM-CSF) (Immunex, Seattle, Wash.) per ml, and 50 μl was seeded into each well of 96-well plates.
One day postisolation, the PBMC were infected in duplicate with the viruses at an MOI of 0.1 and incubated at 37°C. Viruses were diluted in 50 μl of Opti-MEM I and applied directly to the cells maintained in RPMI-10 medium, resulting in a total volume of 100 μl. Two hours postinfection, 100 μl of RPMI-10 containing 3.75 μg of PHA and 1,500 U of GM-CSF per ml were added to each well. At the indicated time points, each well was divided into samples of approximately 105 cells and transferred into V-shaped 96-well plates. The cells were washed in 200 μl of ice-cold PBS-2 and incubated for 1 h in 100 μl of PBS-2 containing 2 μl of phycoerythrin-conjugated CD4-, CD8-, or CD14-specific monoclonal antibodies. The cells were washed three times with 200 μl of ice-cold PBS-2 and fixed in 500 μl of PBS-2 containing 1% paraformaldehyde. Marker and GFP expression by 104 cells was analyzed by two-color fluorescence-activated cell sorting. Background was determined by using mock-infected cells.
RESULTS
Efficiency of different H proteins in supporting cell fusion through SLAM and CD46.
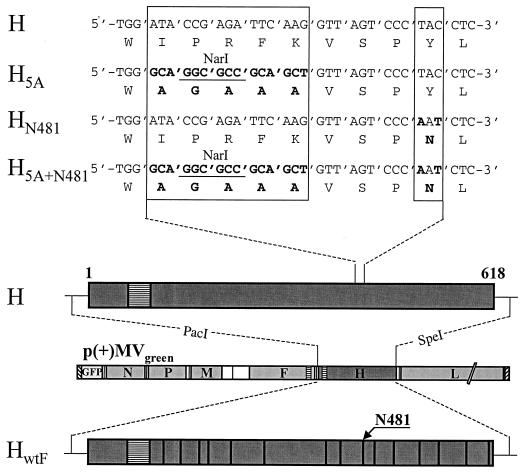
Certain H protein residues have been reported to influence the ability of MV-Edm to interact with CD46. To test how these residues influence cell fusion, we generated expression vectors encoding mutated forms of the MV-Edm H protein. Mutations included residues 473 to 477 (H5A), a tyrosine-to-asparagine exchange at position 481 (HN481), and the combination of both modifications, resulting in construct H5A+N481 (Fig. 1, top). The unaltered MV-Edm H protein and a wild-type protein (HwtF) were used as controls. HwtF differs from H in 15 residues (15) (Fig. 1, bottom). These constructs were analyzed in standard Vero cells (CD46 positive, SLAM negative) and in CD46-negative CHO-SLAM cells (38).
FIG. 1.
H proteins expressed in this study. Top, sequences of a relevant portion of the H protein of MV-Edm (H) and of three mutants thereof (H5A, HN481, and H5A+N481). Nucleotide and amino acid sequences (one-letter code) from residues 472 to 482 are shown. Mutated residues 473 to 477 and 481 are in bold and framed. Bottom, diagrams of the H proteins of MV-Edm (H) and wild-type F (HwtF, dark gray boxes), and of plasmid p(+)MVgreen (light gray box, center). In the proteins, the transmembrane segments are represented by horizontally hatched boxes, and residues diverging from the H sequence are indicated by vertical lines (single residues). Plasmid p(+)MVgreen contains a cDNA copy of the full-length MV genome with a GFP gene inserted in an additional transcription unit (white box on the left).
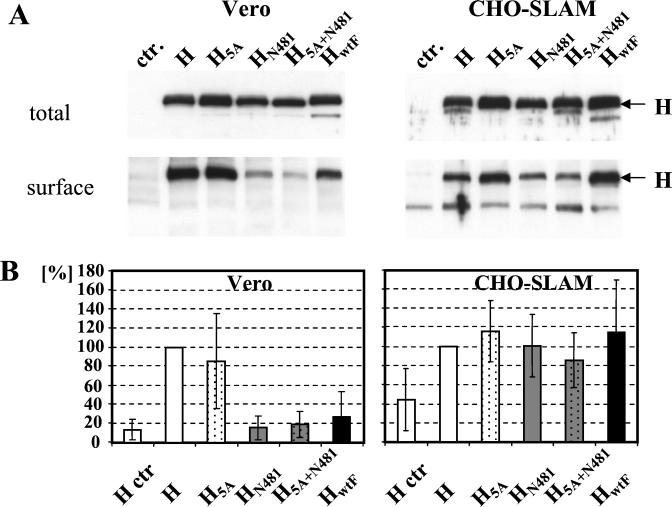
To verify expression of these proteins, Vero and CHO-SLAM cells were transfected with the plasmids. Prior to lysis, the transfected cells were biotinylated at 4°C to label surface-exposed proteins. Total H expression was studied by Western blot analysis of cell extracts (Fig. 2A, upper panel), and surface-exposed H protein was analyzed by immunoprecipitation followed by detection of biotinylated protein (Fig. 2A, lower panel). Although the five plasmids expressed similar levels of H protein in both cell lines, cell surface localization of HN481 and H5A+N481 was markedly reduced in Vero cells and to a lesser degree also in CHO-SLAM cells compared to H and H5A. In contrast, HwtF surface expression was reduced in Vero and increased in CHO-SLAM cells compared to H.
FIG. 2.
Expression (A) and cell fusion support activity (B) of different H proteins. (A) Total and cell surface H protein expression in Vero and CHO-SLAM cells transfected with the plasmids. Twenty-four hours posttransfection, surface proteins were labeled with 0.5 mg of biotin per ml, and after intensive washing, the cells were lysed. Upper panels, total lysates analyzed by Western blot. Lower panels, surface-exposed (biotinylated) H proteins. The H proteins were detected by using streptavidin-coupled peroxidase after immunoprecipitation with the Hcyt antiserum and separation on a gel. (B) Cell-cell fusion support activity of different H proteins on Vero and CHO-SLAM cells. For details of the quantitative fusion assays, see the text. The results of four experiments, each performed in duplicate, are shown; the standard deviation is indicated by error bars. Results are normalized to the value with Edmonston H.
We then tested whether the recombinant H proteins maintained cell fusion competence on both cell lines (Fig. 2B). Cell fusion was assessed in a cocultivation assay based on T7 polymerase-dependent expression of the luciferase gene. Vero and CHO-SLAM cells were cotransfected with cytomegalovirus promoter-driven plasmids encoding the H and the fusion (F) protein and a T7 promoter-driven plasmid encoding the luciferase gene. Subsequently, the transfected cells were mixed with cells infected with an attenuated vaccinia virus expressing the T7 polymerase (MVA-T7). As a control, the H and the luciferase plasmids were transfected without the F plasmid. Luciferase activity in cells transfected with H and F was set to 100% (Fig. 2B).
The fusion support activity of the H mutants was significantly different on the two cell lines. All H proteins with an asparagine at position 481 (HN481, H5A+N481, and HwtF) were inefficient in fusing Vero cells (Fig. 2B, left panel) but efficient in fusing CHO-SLAM cells (Fig. 2B, right panel). Despite lower surface expression levels, the fusogenicity of HN481 and H5A+N481 was comparable to that of HwtF in both cell lines. This suggests that receptor usage by these proteins may be responsible for the observed effects and that the different levels of surface expression are not rate limiting.
Recombinant MV recovery and efficiency of dissemination through SLAM and CD46.
To study these H proteins in the viral context, we generated four recombinant MV in addition to the available MVgreen-H. To be in the position of directly detecting all infectious centers by live cell microscopy, we inserted a GFP gene in the genome of all four new recombinant viruses. This is important because propagation of wild-type MV in Vero cells is initially noncytolytic (17). In a full-length MV-Edm cDNA expressing GFP from an additional transcription unit (10) (Fig. 1, bottom), the Edm H gene was replaced by another H gene. Following the MV recovery protocol (30), viruses were isolated from syncytia formed with Vero (MVgreen-H and MVgreen-H5A) or B95.8 cells (MVgreen-HN481, MVgreen-H5A+N481, and MVgreen-HwtF) in the overlay.
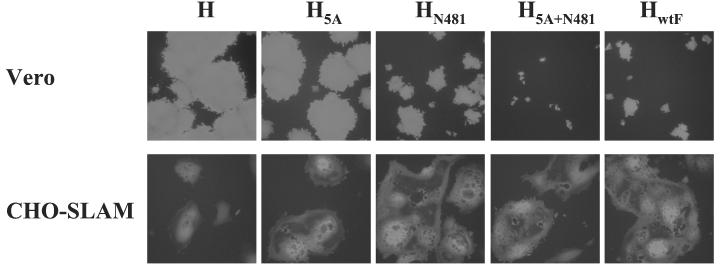
We initially analyzed dissemination, which depends not only on cell entry efficiency but also on the subsequent efficacy of cell fusion. We infected the two cell lines used for the H protein expression experiments with the recombinant MV. Figure 3 shows an analysis of GFP expression in confluent Vero cells (Fig. 3, upper panels) and CHO-SLAM cells (Fig. 3, lower panels). Significant differences in syncytium formation were observed depending on the virus used and the cell line infected. While MVgreen-H and MVgreen-H5A induced large syncytia of similar sizes in Vero cells, MVgreen-HN481 and MVgreen-HwtF were less potent and induced only small syncytia by 30 h postinfection (Fig. 3, top row) and at later time points (data not shown). In the case of MVgreen-H5A+N481, the fusion activity was completely abolished.
FIG. 3.
Cell-cell fusion activity of recombinant MV differing only in the H protein. Vero and CHO-SLAM cells were infected with the indicated viruses at an MOI of 0.1, and infection was monitored by fluorescent microscopy 30 h later on Vero cells and 48 h later on CHO-SLAM cells.
Infection of CHO-SLAM cells with MVgreen-HN481, MVgreen-H5A+N481, and MVgreen-HwtF resulted in efficient cell fusion, whereas MVgreen-H and MVgreen-H5A showed a slightly weaker fusogenicity. The pronounced differences in fusogenicity of MVgreen-HN481, MVgreen-H5A+N481, and MVgreen-HwtF on Vero and CHO-SLAM cells suggest that the H protein-receptor interaction is the major determinant for the lateral spread of the infection through cell fusion in tissue culture. In this context, it is important to note that notwithstanding reduced cell fusion competence, MVgreen-HN481, MVgreen-H5A+N481, and MVgreen-HwtF replicated relatively efficiently in Vero cells. At 96 h postinfection, their titers, as measured by counting fluorescent infectious centers, were only 5- to 10-fold lower than those of MVgreen-H and MVgreen-H5A (data not shown).
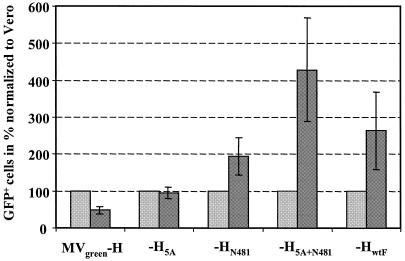
Efficiency of recombinant MV entry through SLAM and CD46.
To assess more directly the entry efficiency of these viruses, we blocked lateral viral spread through cell fusion by addition of a fusion-inhibiting peptide. We used a low MOI (0.01) and counted the GFP-expressing cells in a defined area at 30 h postinfection. The number of infected Vero cells was arbitrarily set to 100% for each virus (Fig. 4). The entry efficiency of MVgreen-H was reduced approximately twofold in CHO-SLAM cells, and MVgreen-H5A entered both cell lines with similar efficiency. In contrast, MVgreen-HN481, MVgreen-H5A+N481, and MVgreen-HwtF entered CHO-SLAM cells approximately 2 times, 4 times, and 2.5 times more efficiently, respectively, than Vero cells. Thus, MV expressing a wild-type H protein or an H protein with asparagine 481 enters cells preferably but not exclusively via the SLAM receptor. In summary, all viruses do enter cells via both receptors, but with slightly different efficiencies.
FIG. 4.
Relative entry efficiency of recombinant MV differing only in their H proteins in cells expressing different receptors. Vero cells (light gray columns) and CHO-SLAM cells (dark gray columns) were infected. Two hours postinfection, the cells were washed, and medium containing the fusion-inhibiting peptide at a concentration of 200 μM was added to prevent viral spread by cell-to-cell fusion. Entry efficiency was quantified 28 h later by counting the GFP-expressing (green fluorescent) cells in a defined area. The counts in Vero cells were set to 100% for each virus. The results of three experiments, each performed in duplicate, are shown; the standard deviation is indicated by error bars.
Evolution of recombinant MV with asparagine 481 in Vero cells.
It was suggested that adaptation of wild-type viruses to growth on indicator Vero cells is causally linked to mutation of H protein residue 481 from asparagine to tyrosine (18). To assess this hypothesis, we performed serial passages in Vero cells of recombinant viruses with an asparagine codon (AAT) at position 481. We then monitored the sequence of this codon after different numbers of passages in the expectation that a tyrosine codon (TAT) would be selected eventually.
Cells were initially infected at an MOI of 0.1 and harvested when the cytopathic effect was well advanced. Ten subsequent passages, each resulting in an approximately 100-fold amplification of infectivity, were performed. At passages 5, 7, and 10, total cellular RNA was isolated and subjected to RT-PCR. The PCR product was sequenced, and the percentage of A residues in the first position of codon 481 was determined from the electropherogram. Remarkably, N481 (AAT) in MVgreen-HN481 remained stable over 10 passages on Vero cells. However, in MVgreen-HwtF and MVgreen-H5A+N481, A-to-T mutations were detected in the first residue of codon 481 in 40 and 60%, respectively, of the viral genomes at passage 7 and in 60 and 90%, respectively, at passage 10 (Table 1). Thus, a slow but progressive shift towards tyrosine at codon 481 was observed in two of three cases. This shift was accompanied by a progressive increase in the fusion competence of the viruses (data not shown). No other sequence alterations were found either in the third position of the 481 codon or in the region of the 5A mutation in the H5A+N481 region sequenced. These data suggest that selective pressure slowly drives wild-type MV to enter Vero cells through CD46.
TABLE 1.
Percentage of genomes with T in the first position of protein H codon 481 during serial passage on Vero cells
| MV strain | % of genomes with T in first position at passage:
|
||
|---|---|---|---|
| 5 | 7 | 10 | |
| MVgreen-H | >95 | >95 | >95 |
| MVgreen-HN481 | <15 | <15 | <15 |
| MVgreen-H5A+N481 | <15 | 60 | 90 |
| MVgreen-HwtF | <15 | 40 | 60 |
Recombinant MV with a wild-type H protein efficiently infects human PBMC.
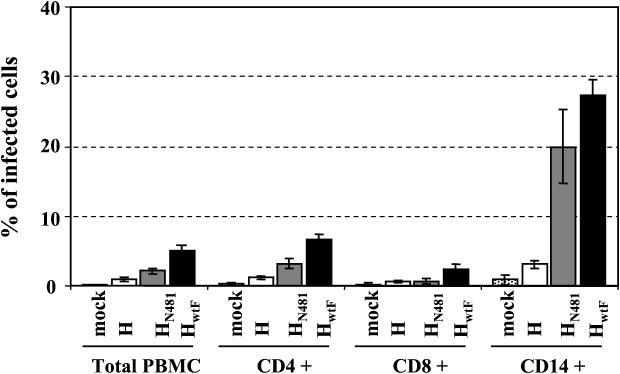
PBMC were isolated from total blood and stimulated, and 1 day after seeding in 96-well plates they were infected with the same amount of MVgreen-H, MVgreen-HN481, or MVgreen-HwtF as determined by 50% endpoint dilution assays on Vero cells. One day postinfection with an MOI of 0.1, GFP expression was analyzed in total PBMC or CD4-, CD8-, and CD14-positive subpopulations (Fig. 5). MVgreen-HwtF was consistently the most efficient in infecting all cell types examined, CD14-positive monocytes and CD4- or CD8-positive T lymphocytes (Fig. 5, black columns). Data obtained at later time points confirmed this trend (not shown).
FIG. 5.
Percentage of GFP-positive cells in total PBMC and in the CD4, CD8, and CD14 populations after infection with three recombinant MV. Human PBMC were seeded into a 96-well dish and stimulated with phytohemagglutinin and GM-CSF. Cells were mock infected (dotted columns) or infected with MV-H (white columns), MV-HN481 (gray columns), or MV-HwtF (black columns), harvested, and divided into four samples that were stained with phycoerythrin-coupled monoclonal antibodies against the indicated cell markers. The samples were analyzed for phycoerythrin staining and GFP expression. For each analysis, 104 events were counted. The standard deviation is indicated by error bars.
The cell type infected most efficiently was monocytes: 27.4% (±2.2%) of these cells expressed the reporter protein GFP one day after infection with MVgreen-HwtF, compared to 20.0% (±5.3%) after MVgreen-HN481 infection and to less than 4% after infection with MVgreen-H (Fig. 5, CD14+ cells). Since the MOI of all the viruses was 0.1, the number of infected monocytes exceeded about 2.5 times that expected for MVgreen-HwtF. An approximately twofold excess in infections was measured for MVgreen-HN481 and an approximately 2.5-fold deficit in infections was measured for MVgreen-H. These shifts from the titer in Vero cells correlated well with those measured when comparing titers in Vero and CHO-SLAM cells (Fig. 4). Thus, it appears possible that in monocytes as well as in CD4- and CD8-positive T lymphocytes, SLAM is the main functional receptor.
DISCUSSION
We show here that recombinant viruses differing only in their H protein enter cells expressing different receptors with slightly different efficiencies. MV with a wild-type H protein or with an H protein with an asparagine at position 481 enter CHO cells expressing SLAM two to three times more efficiently than they do Vero cells expressing CD46. In contrast, a virus with the MV-Edm H protein enters CD46-expressing cells about twice as efficiently as it enters SLAM-expressing cells. Those are small differences in relative entry efficiency, but since viruses with asparagine 481 do not efficiently fuse cells expressing CD46, their infections have minimal cytopathic effects. In contrast, all other combinations of viruses and cells result in efficient cell fusion and strong cytopathic effects.
H protein adaptation to more efficient CD46-dependent entry.
Sequence comparison of MV strains identified asparagine 481 as a conserved residue among many wild-type strains and tyrosine 481 in attenuated viruses (18). Therefore, it was suggested that residue 481 may have a pivotal role in MV binding to CD46 and in attenuation. A role in binding was confirmed experimentally (14). Moreover, it was shown that five passages in human HEp-2 or simian Vero cells often but not always result in selection of MV with a tyrosine at position 481 (25).
We have documented here the evolution of three MV genomes with an asparagine at position 481 during their passage in Vero cells. These viruses were propagated in cell-associated form, the standard mode of MV passaging. At each of the 10 passages, an approximately 100-fold amplification of the inoculum was estimated. Under these experimental conditions, slow but progressive enrichment of MV RNA with a tyrosine codon at H position 481 was observed in the population of genomes amplified from infected cells. The polyploid nature of MV particles (31) may account at least in part for the slow evolution. Interestingly, this shift was selected more efficiently in the two viruses with several differences from the Edmonston H protein sequence than in the virus in which asparagine 481 was situated in the standard Edmonston H protein context. These viruses, especially MVgreen-H5A+N481, significantly gained fusogenicity after Vero cell passaging.
Another interesting observation is that transport of HN481 and the H5A+N481 to the cell surface is inefficient in Vero and to a lesser degree also in CHO-SLAM cells. In contrast, the wild-type H protein, also encoding an asparagine in position 481, is transported more efficiently to the cell surface on both cell lines. This suggests that the Edmonston and the wtF H proteins may have slightly different overall structures and that asparagine 481 in the structural context of Edmonston H may interfere with optimal folding. Altogether, these observations suggest that the wtF H protein conformation has been selected during evolution to support an efficient receptor switch.
The fact that, even after 10 passages, mutation of asparagine 481 of MV-HN481 was below the detection level raises the possibility that other changes in this viral genome have occurred and may positively impact adaptation to efficient growth in Vero cells. Detection of these changes is beyond the purpose of this work, but in another study changes in the MV proteins involved in replication were detected after Vero cell adaptation (36). On the other hand, Nielsen et al. (25) recently noticed that passage in HEp-2 cells of certain wild-type viruses more often leads to N481Y conversion than passage on Vero cells, indicating that different host cells may exert different selective pressures on receptor adaptation of H.
MV with asparagine 481 H proteins enter cells efficiently through CD46.
That wild-type MV strains and MV-Edm enter cells efficiently through SLAM and that their infections cause large syncytia is well established (11, 13, 38). Similarly, several groups have observed that MV-Edm enters and fuses cells efficiently through CD46 (3, 8, 21, 24). It was, however, suggested that wild-type MV may enter cells very inefficiently if at all through CD46. This suggestion is based not only on the lack of cytopathic effects of wild-type MV in Vero cells (14, 18, 38) but also on the measurement of the entry efficiency of vesicular stomatitis virus (VSV) pseudotyped with a wild-type or the Edmonston H protein in rodent cells expressing CD46 (37). Nevertheless, the fact that MV can be isolated from patients upon passage in Vero cells does indicate that wild-type viruses can enter these cells. Importantly, during the initial passages in Vero cells, there is no detectable syncytium formation, indicating that clinical isolates are inefficient in inducing cell-cell fusion (17).
Our study, based on the use of recombinant MV expressing an autofluorescent protein, making infection easily detectable at the single-cell stage, revealed that entry of viruses with asparagine 481 in Vero cells is only slightly reduced compared to entry of viruses with tyrosine 481. Moreover, our H protein transient-expression studies confirm previous observations that proteins with asparagine 481 are only minimally cytopathic in Vero cells (14, 18). Thus, the lack of CD46-dependent cytopathogenicity of wild-type MV appears to be due principally to less efficient cell fusion and only in part to less efficient cell entry. This interpretation is consistent with observations by Johnston et al. (15), who detected efficient entry and replication but minimal cytopathic effects of a recombinant MV expressing the H protein of wtF in Vero cells. Moreover, Manchester et al. (20) showed that anti-CD46 antibodies can be used to partially compete with PBMC infection by certain MV strains isolated on human B lymphocytes. However, Tatsuo et al. (37) showed that the envelope proteins of the wild-type strain KA conferred 100- to 1,000-fold less efficient entry to an envelope-free VSV recombinant in rodent cell lines expressing CD46 than the envelope proteins of the Edmonston strain.
A possible interpretation of these observations is that different wild-type MV strains may have a considerably different efficiency of CD46-dependent entry. A second possibility is that, in Vero cells, an unidentified receptor accounts for the relatively efficient entry of viruses with the asparagine 481 residue. Finally, it is conceivable that the MV glycoproteins do not retain all their functional characteristics important for cell entry when the internal components of MV are not present, as is the case in the VSV pseudotypes.
Receptor usage in acute measles.
The observations presented here are consistent with SLAM receptor usage by wild-type MV in immune cells, followed by usage of a ubiquitous protein, possibly CD46, in later infection stages. The switch in H residue 481 is not necessary to allow virus spread but may decisively alter the dissemination kinetics.
Monocytes are major targets for MV infection (12, 32, 33), and our finding that a recombinant MV with a wild-type H protein preferentially infects CD14-positive circulating cells is in line with this fact. However, it was initially observed that freshly isolated monocytes do not express SLAM (7, 35), and therefore it was unclear if SLAM-dependent entry could occur in these cells. Minagawa et al. (22) recently observed that simple stimuli, including phytohemagglutinin, lipopolysaccharides, and also infection with active or UV-inactivated MV, induce SLAM expression on monocytes. Moreover, they showed that an anti-SLAM antibody greatly reduced monocyte infection by a wild-type strain, confirming the preferential use of the SLAM as a receptor in these cells. Therefore, it appears likely that SLAM is the molecule mediating MV entry in monocytes.
It is important to recall that CD46 is expressed on all human cells except erythrocytes (19). It is unknown why entry through CD46 is inefficient in immune cells, but the experiments presented here clearly indicate that the MV with the most efficient CD46 entry is the one that infects human PBMC least efficiently. In contrast, the recombinant with a wild-type H protein does infect PBMC efficiently, and a recombinant virus with asparagine 481 in an otherwise Edmonston-like H gene has intermediate entry efficiency. These data are consistent with the relevance of SLAM-dependent entry but not CD46-dependent entry for PBMC infection.
Acknowledgments
We thank Sompong Vongpunsawad for excellent technical support, Yusuke Yanagi for the CHO-SLAM cells, Anthea Hammond for a plasmid, and Mark Federspiel, Steve Russell, and Peter Staehli for comments on the manuscript.
This work was supported by grants from the Mayo, Siebens, and Eisenberg Foundations.
REFERENCES
- 1.Bartz, R., U. Brinckmann, L. M. Dunster, B. Rima, V. Ter Meulen, and J. Schneider-Schaulies. 1996. Mapping amino acids of the measles virus hemagglutinin responsible for receptor (CD46) downregulation. Virology 224:334-337. [DOI] [PubMed] [Google Scholar]
- 2.Borrow, P., and M. B. Oldstone. 1995. Measles virus-mononuclear cell interactions. Curr. Top. Microbiol. Immunol. 191:85-100. [DOI] [PubMed] [Google Scholar]
- 3.Buchholz, C. J., U. Schneider, P. Devaux, D. Gerlier, and R. Cattaneo. 1996. Cell entry by measles virus: long hybrid receptors uncouple binding from membrane fusion. J. Virol. 70:3716-3723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Cathomen, T., C. J. Buchholz, P. Spielhofer, and R. Cattaneo. 1995. Preferential initiation at the second AUG of the measles virus F mRNA: a role for the long untranslated region. Virology 214:628-632. [DOI] [PubMed] [Google Scholar]
- 5.Cathomen, T., H. Y. Naim, and R. Cattaneo. 1998. Measles viruses with altered envelope protein cytoplasmic tails gain cell fusion competence. J. Virol. 72:1224-1234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Clements, C. J., and F. T. Cutts. 1995. The epidemiology of measles: thirty years of vaccination. Curr. Top. Microbiol. Immunol. 191:13-33. [DOI] [PubMed] [Google Scholar]
- 7.Cocks, B. G., C. C. Chang, J. M. Carballido, H. Yssel, J. E. de Vries, and G. Aversa. 1995. A novel receptor involved in T-cell activation. Nature 376:260-263. [DOI] [PubMed] [Google Scholar]
- 8.Dorig, R. E., A. Marcil, A. Chopra, and C. D. Richardson. 1993. The human CD46 molecule is a receptor for measles virus (Edmonston strain). Cell 75:295-305. [DOI] [PubMed] [Google Scholar]
- 9.Duprex, W. P., I. Duffy, S. McQuaid, L. Hamill, S. L. Cosby, M. A. Billeter, J. Schneider-Schaulies, V. ter Meulen, and B. K. Rima. 1999. The H gene of rodent brain-adapted measles virus confers neurovirulence to the Edmonston vaccine strain. J. Virol. 73:6916-6922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Duprex, W. P., S. McQuaid, L. Hangartner, M. A. Billeter, and B. K. Rima. 1999. Observation of measles virus cell-to-cell spread in astrocytoma cells by using a green fluorescent protein-expressing recombinant virus. J. Virol. 73:9568-9575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Erlenhoefer, C., W. J. Wurzer, S. Loffler, S. Schneider-Schaulies, V. ter Meulen, and J. Schneider-Schaulies. 2001. CD150 (SLAM) is a receptor for measles virus but is not involved in viral contact-mediated proliferation inhibition. J. Virol. 75:4499-4505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Esolen, L. M., B. J. Ward, T. R. Moench, and D. E. Griffin. 1993. Infection of monocytes during measles. J. Infect. Dis. 168:47-52. [DOI] [PubMed] [Google Scholar]
- 13.Hsu, E. C., C. Iorio, F. Sarangi, A. A. Khine, and C. D. Richardson. 2001. CDw150 (SLAM) is a receptor for a lymphotropic strain of measles virus and may account for the immunosuppressive properties of this virus. Virology 279:9-21. [DOI] [PubMed] [Google Scholar]
- 14.Hsu, E. C., F. Sarangi, C. Iorio, M. S. Sidhu, S. A. Udem, D. L. Dillehay, W. Xu, P. A. Rota, W. J. Bellini, and C. D. Richardson. 1998. A single amino acid change in the hemagglutinin protein of measles virus determines its ability to bind CD46 and reveals another receptor on marmoset B cells. J. Virol. 72:2905-2916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Johnston, I. C., V. ter Meulen, J. Schneider-Schaulies, and S. Schneider-Schaulies. 1999. A recombinant measles vaccine virus expressing wild-type glycoproteins: consequences for viral spread and cell tropism. J. Virol. 73:6903-6915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kärber, G. 1931. Beitrag zur kollektiven Behandlung pharmakologischer Reihenversuche. Arch. Exp. Pathol. Pharmakol. 162:480-483. [Google Scholar]
- 17.Kouomou, D. W., and T. F. Wild. 2002. Adaptation of wild-type measles virus to tissue culture. J. Virol. 76:1505-1509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lecouturier, V., J. Fayolle, M. Caballero, J. Carabana, M. L. Celma, R. Fernandez-Munoz, T. F. Wild, and R. Buckland. 1996. Identification of two amino acids in the hemagglutinin glycoprotein of measles virus (MV) that govern hemadsorption, HeLa cell fusion, and CD46 downregulation: phenotypic markers that differentiate vaccine and wild-type MV strains. J. Virol. 70:4200-4204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Liszewski, M. K., T. W. Post, and J. P. Atkinson. 1991. Membrane cofactor protein (MCP or CD46): newest member of the regulators of complement activation gene cluster. Annu. Rev. Immunol. 9:431-455. [DOI] [PubMed] [Google Scholar]
- 20.Manchester, M., D. S. Eto, A. Valsamakis, P. B. Liton, R. Fernandez-Munoz, P. A. Rota, W. J. Bellini, D. N. Forthal, and M. B. Oldstone. 2000. Clinical isolates of measles virus use CD46 as a cellular receptor. J. Virol. 74:3967-3974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Manchester, M., M. K. Liszewski, J. P. Atkinson, and M. B. Oldstone. 1994. Multiple isoforms of CD46 (membrane cofactor protein) serve as receptors for measles virus. Proc. Natl. Acad. Sci. USA 91:2161-2165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Minagawa, H., K. Tanaka, N. Ono, H. Tatsuo, and Y. Yanagi. 2001. Induction of the measles virus receptor SLAM (CD150) on monocytes. J. Gen. Virol. 82:2913-2917. [DOI] [PubMed] [Google Scholar]
- 23.Moss, B., O. Elroy-Stein, T. Mizukami, W. A. Alexander, and T. R. Fuerst. 1990. Product review. New mammalian expression vectors. Nature 348:91-92. [DOI] [PubMed] [Google Scholar]
- 24.Naniche, D., G. Varior-Krishnan, F. Cervoni, T. F. Wild, B. Rossi, C. Rabourdin-Combe, and D. Gerlier. 1993. Human membrane cofactor protein (CD46) acts as a cellular receptor for measles virus. J. Virol. 67:6025-6032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Nielsen, L., M. Blixenkrone-Moller, M. Thylstrup, N. J. Hansen, and G. Bolt. 2001. Adaptation of wild-type measles virus to CD46 receptor usage. Arch. Virol. 146:197-208. [DOI] [PubMed] [Google Scholar]
- 26.Ohgimoto, S., K. Ohgimoto, S. Niewiesk, I. M. Klagge, J. Pfeuffer, I. C. Johnston, J. Schneider-Schaulies, A. Weidmann, V. ter Meulen, and S. Schneider-Schaulies. 2001. The haemagglutinin protein is an important determinant of measles virus tropism for dendritic cells in vitro. J. Gen. Virol. 82:1835-1844. [DOI] [PubMed] [Google Scholar]
- 27.Ono, N., H. Tatsuo, Y. Hidaka, T. Aoki, H. Minagawa, and Y. Yanagi. 2001. Measles viruses on throat swabs from measles patients use signaling lymphocytic activation molecule (CDw150) but not CD46 as a cellular receptor. J. Virol. 75:4399-4401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Patterson, J. B., F. Scheiflinger, M. Manchester, T. Yilma, and M. B. Oldstone. 1999. Structural and functional studies of the measles virus hemagglutinin: identification of a novel site required for CD46 interaction. Virology 256:142-151. [DOI] [PubMed] [Google Scholar]
- 29.Polacino, P. S., L. M. Pinchuk, S. P. Sidorenko, and E. A. Clark. 1996. Immunodeficiency virus cDNA synthesis in resting T lymphocytes is regulated by T cell activation signals and dendritic cells. J. Med. Primatol. 25:201-209. [DOI] [PubMed] [Google Scholar]
- 30.Radecke, F., P. Spielhofer, H. Schneider, K. Kaelin, M. Huber, C. Dotsch, G. Christiansen, and M. A. Billeter. 1995. Rescue of measles viruses from cloned DNA. EMBO J. 14:5773-5784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Rager, M., S. Vongpunsawad, W. P. Duprex, and R. Cattaneo. 2002. Polyploid measles virus with hexameric genome length. EMBO J. 21:2364-2372. [DOI] [PMC free article] [PubMed]
- 32.Roscic-Mrkic, B., R. A. Schwendener, B. Odermatt, A. Zuniga, J. Pavlovic, M. A. Billeter, and R. Cattaneo. 2001. Roles of macrophages in measles virus infection of genetically modified mice. J. Virol. 75:3343-3351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Salonen, R., J. Ilonen, and A. Salmi. 1988. Measles virus infection of unstimulated blood mononuclear cells in vitro: antigen expression and virus production preferentially in monocytes. Clin. Exp. Immunol. 71:224-228. [PMC free article] [PubMed] [Google Scholar]
- 34.Schneider, U., F. Bullough, S. Vongpunsawad, S. J. Russell, and R. Cattaneo. 2000. Recombinant measles viruses efficiently entering cells through targeted receptors. J. Virol. 74:9928-9936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Sidorenko, S. P., and E. A. Clark. 1993. Characterization of a cell surface glycoprotein IPO-3, expressed on activated human B and T lymphocytes. J. Immunol. 151:4614-4624. [PubMed] [Google Scholar]
- 36.Takeda, M., A. Kato, F. Kobune, H. Sakata, Y. Li, T. Shioda, Y. Sakai, M. Asakawa, and Y. Nagai. 1998. Measles virus attenuation associated with transcriptional impediment and a few amino acid changes in the polymerase and accessory proteins. J. Virol. 72:8690-8696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Tatsuo, H., K. Okuma, K. Tanaka, N. Ono, H. Minagawa, A. Takade, Y. Matsuura, and Y. Yanagi. 2000. Virus entry is a major determinant of cell tropism of Edmonston and wild-type strains of measles virus as revealed by vesicular stomatitis virus pseudotypes bearing their envelope proteins. J. Virol. 74:4139-4145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Tatsuo, H., N. Ono, K. Tanaka, and Y. Yanagi. 2000. SLAM (CDw150) is a cellular receptor for measles virus. Nature 406:893-897. [DOI] [PubMed] [Google Scholar]
- 39.Tatsuo, H., N. Ono, and Y. Yanagi. 2001. Morbilliviruses use signaling lymphocyte activation molecules (CD150) as cellular receptors. J. Virol. 75:5842-5850. [DOI] [PMC free article] [PubMed] [Google Scholar]