Abstract
Objective
To evaluate the impact of a school-based diabetes mellitus prevention program on low-income fourth-grade Mexican American children.
Design
A randomized controlled trial with 13 intervention and 14 control schools.
Setting
Elementary schools in inner-city neighborhoods in San Antonio, Tex.
Participants
Eighty percent of participants were Mexican American and 94% were from economically disadvantaged households. Baseline and follow-up measures were collected from 1419 (713 intervention and 706 control) and 1221 (619 intervention and 602 control) fourth-grade children, respectively.
Intervention
The Bienestar Health Program consists of a health class and physical education curriculum, a family program, a school cafeteria program, and an after-school health club. The objectives are to decrease dietary saturated fat intake, increase dietary fiber intake, and increase physical activity.
Main Outcome Measures
The primary end point was fasting capillary glucose level, and the secondary end points were percentage of body fat, physical fitness level, dietary fiber intake, and dietary saturated fat intake. Fasting capillary glucose level, bioelectric impedance, modified Harvard step test, three 24-hour dietary recalls, weight, and height were collected at baseline and 8 months later.
Results
Children in the intervention arm attended an average of 32 Bienestar sessions. Mean fasting capillary glucose levels decreased in intervention schools and increased in control schools after adjusting for covariates (−2.24 mg/dL [0.12 mmol/L]; 95% confidence interval, −6.53 to 2.05 [−0.36 to 0.11 mmol/L]; P = .03). Fitness scores (P = .04) and dietary fiber intake (P = .009) significantly increased in intervention children and decreased in control children. Percentage of body fat (P = .56) and dietary saturated fat intake (P = .52) did not differ significantly between intervention and control children.
Conclusion
This intervention showed some positive results, but additional research is needed to examine long-term benefits, translation, and cost-effectiveness.
Mexican American adults have a greater prevalence of diagnosed (9.3%) and undiagnosed (4.5%) diabetes mellitus than African Americans (8.2% and 3.5%) and non-Hispanic whites (4.8% and 2.5%).1 Recent studies2,3 report an increasing number of Mexican American children being diagnosed as having type 2 diabetes mellitus. Common findings in studies with Mexican American children were that most were unaware of their disease, most were overweight, and all came from low-income households.
Overweight,4–7 a low level of physical activity,8–10 high saturated fat intake,11 and low dietary fiber intake12 are modifiable risk factors for type 2 diabetes mellitus. These risk factors are reported to be more common in Mexican American children than in non-Hispanic white children. Mexican American children have more centralized adiposity, a higher body mass index, and thicker skinfolds than non-Hispanic white children.13–15 Mexican American children consume more portions of dietary fat and fewer portions of fruits and vegetables than are recommended by national standards.16,17 Latino children have lower physical activity levels than other US children.18–20 Because diabetes mellitus is highly prevalent in Mexican American adults and is increasing in Mexican American youth and because diabetes mellitus risk factors are more common in Mexican American children, a prudent response is to implement and evaluate programs aimed at preventing or delaying the onset of type 2 diabetes mellitus in this high-risk group of children. This study, therefore, tested the efficacy of the Bienestar Health Program (“well-being” in Spanish). The primary end point was fasting capillary glucose (FCG) concentration, and the secondary end points were percentage of body fat, fitness levels, dietary fiber intake, and dietary saturated fat intake.
METHODS
STUDY PARTICIPANTS
The participating school district has 67 elementary schools. Of the 67 schools, 44 were available to participate (Figure). A total of 3096 fourth-grade students were enrolled in the 44 available schools. All fourth-grade children, regardless of race and ethnicity, were invited to participate. The following students were excluded from data analysis: (1) those in elementary schools with previous exposure to Bienestar (20 schools), (2) students in alternative schools (3 schools), (3) those older than 12 years (4 students), (4) students previously diagnosed as having type 1 or type 2 diabetes mellitus (1 student), and (5) students with extreme dietary values (29 students). Students with 3-day average calorie intakes of less than 800 and greater than 4800 were excluded from this analysis (baseline and follow-up).21
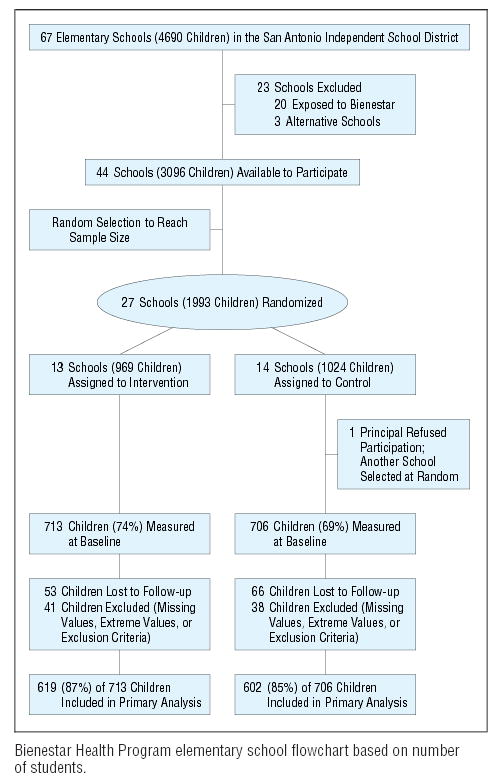
Bienestar Health Program elementary school flowchart based on number of students.
DESIGN
The Bienestar Health Program is an ongoing randomized controlled trial. The method of randomization was based on cluster (school) sampling. Faculty from the University of Texas at San Antonio were hired as independent consultants to conduct the randomization process. Using a random-number table, 27 of the 44 schools were assigned to either intervention (n = 13) or control (n = 14). After assignment, school principals were informed, and their commitment was confirmed. One principal declined the invitation, but a principal from another school selected at random agreed to participate. The principals were asked not to inform students, parents, and school staff of the intervention assignment.
After the 27 schools were identified, Bienestar staff sent parents a letter and a consent/assent form. These documents explained to parents that their children’s schools could be assigned to receive either a health examination alone or a health examination and a school health program. The documents also explained to parents that students would receive $5 at baseline and $5 at follow-up for participating in the health examination. Only children who returned written informed consent forms signed by their parent or guardian and who assented to the study participated in program evaluation, and all children participated in program implementation. All program implementation and data collection were conducted on the school campuses. Consent forms were provided in English and Spanish and were written at a fourth-grade level. The institutional review board of the University of Texas Health Science Center at San Antonio approved the study protocol.
PROGRAM DESCRIPTION
To develop a model for effective behavior modification, a theoretical framework capable of effecting substantial change in children’s thoughts, affect, and social environment was necessary. Social cognitive theory22 and social ecological theory23 were selected to provide the theoretical framework for the Bienestar Health Program. According to social cognitive theory, personal factors (health knowledge and beliefs), social systems (family, peers, and teachers), and behaviors (dietary saturated fat intake, dietary fiber intake, and physical activity) must be impacted to affect health outcomes. According to social ecological theory, changing the physical context (classroom, playground, school cafeteria, and home) is important too. Another framework used to develop this program was cultural appropriateness.24–26 The cultural relevance of the Bienestar Health Program was ensured through the use of bilingual culturally and contextually relevant themes.
The objective of the Bienestar Health Program is to provide children with 50 sessions of health programming distributed throughout 7 months (October 1, 2001, to April 26, 2002). The health sessions were used to transmit to children 3 health behavior messages shown to be associated with diabetes mellitus control (decrease dietary saturated fat intake, increase dietary fiber intake, and increase physical activity in children). These behaviors were taught and reinforced through classroom, home, school cafeteria, and after-school care educational activities (Table 1). Physical education teachers, parents, school cafeteria staff, and after-school caretakers were asked to encourage less dietary saturated fat intake, more dietary fiber intake, and more physical activity; to have less dietary saturated fat, more dietary fiber, and more physical activity available; and to be role models for the children. Children were asked to set goals aimed at accomplishing the targeted behaviors and to keep records of their accomplishments. Children were also asked to encourage their peers and adult caretakers to practice the 3 health behaviors. The 4 components of the Bienestar Health Program cohesively addressed the individual, relevant social groups, culture, and a health promotion environment that supports behaviors consistent with diabetes mellitus prevention.
Table 1.
Descriptions and Schedules of the Bienestar Health Program
| Program | Description | Schedules |
|---|---|---|
| Bienestar health and physical education Class (includes teacher’s health and physical education manuals and a student’s health workbook; also includes a pretest and a posttest, transparencies, and extension lessons) | The health curriculum is based on thematic instruction and experiential and multicultural learning; the 13 lessons cover nutrition, physical activity, self-esteem, self-control, and diabetes mellitus; the physical education curriculum is aimed at promoting an active lifestyle through 32 different physical activities | Health and physical education classes are held 45 min/d, 5 d/wk; 1 d is health education and 4 d are physical activities |
| Bienestar health club (includes an instructor’s manual and a student’s workbook) | The aim of the 26 sessions is to reinforce classroom learning and to promote leisure-time physical activity; student participation is voluntary, and parents are encouraged to attend; cooking classes, physical activities, aerobics, games, dancing, singing, and arts and crafts are some of the activities | Club meetings are held weekly after school for 1 h (3–4 pm) |
| Bienestar family fun fiesta (includes an instructor’s manual and a parent’s workbook) | Four activities: cooking demonstrations (nutrition and weight), salsa dancing (exercise and weight), a loteria (bingo) game (nutrition), and the wheel of health game (exercise) | Parent meetings are promoted at each school and are held every other month(6–7 pm) |
| Bienestar school food service (includes an instructor’s manual and a cafeteria staff workbook) | Seven lesson plans designed to improve the nutrition knowledge of food service staff and to persuade students during the lunch period to choose and eat more fruits and vegetables and less fatty foods | One lesson per month; each lesson is 30 min (8:15–8:45 am) during staff break; lunch visits to persuade children are once a week |
Parents and students who practiced the targeted behaviors were rewarded with “Bienestar coupons” denominated in dollar amounts as an incentive. At the end of a semester, a “tiendita” or little store was held at each school. Participants could purchase merchandise (donated clothes, household appliances, school supplies, toys, sporting goods, and gift certificates) with their Bienestar coupons.
OUTCOME MEASURES
The primary end point was FCG concentration, and the secondary end points were percentage of body fat, physical fitness level, and dietary fiber and dietary saturated fat intake. Outcome measures were collected at the beginning and end of the school year (September 4, 2001, and April 29, 2002). Temporary staff, separate from programs and masked to the intervention, were hired and trained to collect the data. Students were asked to fast overnight so that school district nurses and Bienestar medical assistants could collect FCG samples in the morning. Levels of FCG were measured by collecting a blood drop from a student’s fingerstick. The blood drop was placed on a reagent strip and inserted into a blood glucose monitoring system (Glucometer Elite XL; Bayer Corp, Mishawaka, Ind). Students with an FCG level less than 110 mg/dL (<6.1 mmol/L) were given a written notice explaining to the parents that the student’s diabetes mellitus test result was normal. Students with an FCG level of 110 mg/dL or greater (≥6.1 mmol/L) (positive screening results)27 were referred to a physician for further testing. This study was conducted before the new American Diabetes Association guidelines28 for diagnosing diabetes mellitus were published.
Dietary fiber intake and percentage of energy intake from saturated fat were assessed using a 24-hour dietary recall protocol. Studies29,30 have found dietary recalls to be reliable and valid in children in this age group. Three 24-hour dietary recalls, including 2 weekdays and a Sunday or holiday, were collected and recorded by trained staff. Because most children in this study participated in the federal school lunch program, 2 of 3 meals a day are provided by school cafeterias during weekdays, and all meals are provided by parents during weekends.
Bienestar staff training focused on interviewing and measuring techniques. The interviewing technique consisted of a script for dialogue, prompting methods, and recording methods. The measuring technique consisted of food models and measuring utensils used to increase portion size accuracy. Dietary intake data were entered for analysis using nutrition calculation software (Nutrition Data System for Research, version 4.02; Nutrition Coordinating Center, University of Minnesota, Minneapolis).
Physical fitness rather than physical activity was assessed because recall questionnaires in children younger than 10 years are less reliable and less valid than those in older children31,32 and because short-term recall questionnaires may reveal seasonal instead of usual physical activity. In the present study, physical fitness was measured using a modified Harvard step test. The step test consists of connecting a heart rate monitor (Polar Vantage XL; Polar Electric Co, Port Washington, NY) transmitter to the lower part of the child’s chest and connecting a monitor to the wrist. A baseline heart rate is recorded, then the child is asked to start stepping onto and off (both feet) a stool 30 cm high, 42 cm wide, and 38 cm deep for 5 minutes. The student is paced at 30 cycles per minute. Heart rates were recorded 0, 1, and 2 minutes after the child either completely finished the exercise or stopped the exercise prematurely. A physical fitness score was calculated from the total time of exercise (in seconds) multiplied by 100 and divided by the sum of 3 heart rate values measured 0, 1, and 2 minutes after exercise.20
Body fat was measured using bioelectric impedance analysis (Tanita Corporation of America Inc, Arlington Heights, Ill) and body mass index. Bioelectric impedance analysis was used for body fat measurement because body fatness has been shown to relate closely to atherogenic and diabetogenic risk factors in children33 and because body mass index may not represent true body fatness in prepubertal children.34 The children, in indoor clothing, were asked to remove their shoes and socks and step on the metal box. Within 30 seconds, the instrument prints out percentage of body fat and weight. Students, in indoor clothing and barefooted, also had their height measured using a wall stop measuring tape (stadiometer) (Seca Bodymeter 206; Seca Corp, Hanover, Md). Body mass index was calculated as weight in kilograms divided by the square of height in meters using the Quetelet Index measure.
MEASURES OF STUDENT AND SCHOOL CHARACTERISTICS
Information on student age, sex, and ethnic background and the percentage of students classified as economically disadvantaged (eligible for free lunch) were collected from student self-report and cross-checked with information provided by the school. Parents or guardians of students were also asked to complete a questionnaire at baseline. Information collected from parents or guardians included family health history, parental education, family income, and self-reported health status. Finally, information was collected to assess differences between schools. Each school’s level of performance on the Texas Academic Assessment Systems was obtained from the Texas Education Agency Web site. The levels of performance were categorized as “exemplary,” “recognized,” “acceptable,” and “low.” Information was also gathered on the percentage of students who identified themselves as Mexican American or Hispanic and the percentage of students classified as being economically disadvantaged based on free school lunch program eligibility.
STATISTICAL ANALYSIS
Because randomization and implementation of the health intervention occurred at the school level, we used mixed models to adjust the clustering effect controlling for the dependency at the student level.35 This approach effectively models outcomes at the individual level in terms of student- and school-level covariates while concurrently estimating and adjusting for the intraclass correlation present in the data. We used hierarchical linear and nonlinear modeling software (HLM 5; Scientific Software International, Lincolnwood, Ill) to conduct the mixed-models analyses.36
All regression analyses were conducted using the intent-to-treat method, with students analyzed in their originally assigned treatment condition regardless of midyear transferring and attendance at Bienestar program activities. The change in the 5 outcome variables from baseline to follow-up was the dependent variable, and sex, ethnicity, and age were the student-level covariates. Height change from baseline to follow-up was included in all models to control for differential growth effect. The baseline value of the outcome variable was also included in all models. For dietary intake outcomes, total daily caloric intake (mean) at baseline was added to the regression as a covariate in addition to other covariates. All student-level covariates were originally allowed to vary randomly. In most cases, only the baseline value of the outcome variable varied randomly across schools.
Three school-level contextual variables (percentage disadvantaged, percentage Mexican American, and Texas Academic Assessment Systems level) that provided an indication of the social and cultural characteristics of the schools involved were included as covariates. In the original analyses, they were all entered into the regression models as school-level covariates to control for their potential effects on intervention outcomes. School-level contextual variables were then eliminated from the model if they did not contribute significantly to variations in the differences in the outcome variables. We estimated the differences in changes in the outcome variables and their 95% confidence intervals (95% CIs), adjusting for student- and school-level covariates. We included only statistically significant fixed and random variables in the final models.
RESULTS
PARTICIPATION LEVEL
Of 1993 fourth-grade students available from 27 elementary schools, 1419 (71%) returned signed parent consent and student assent forms. The response rate in the intervention schools (74%) was 4.6% (95% CI, 0.07%–8.0%) higher than that in control schools (69%) (Figure). Because there was no evidence that students and parents were aware of their assignments, it was unclear why the response rate was different.
Baseline and follow-up FCG levels were collected from 1419 (713 intervention and 706 control) and 1221 (619 intervention and 602 control) fourth-grade children, respectively (Figure). Sample sizes for the other outcome measures varied slightly. The 198 students missing were either lost to follow-up (119 students) or excluded from analysis because of missing values, extreme values, or exclusion criteria (79 students).
At baseline, there were no statistically significant differences in student characteristics between control and intervention schools except for intervention schools tending to have a higher percentage of Mexican American students (P = .02). At baseline, there were no statistically significant differences in outcome measures between intervention and control schools except for physical fitness measures (fitness score, 65.93 for control schools and 63.90 for intervention schools; P = .001 after adjusting for sex, ethnicity, and age). Potential bias that could be introduced by differences in attrition rates between control and intervention schools was examined. No difference in attrition due to student sex, ethnicity, or treatment condition was found.
HOUSEHOLD AND STUDENT CHARACTERISTICS
Household demographic questionnaires were completed and returned by 956 of 1434 families who had signed parent consent forms. The annual household income averaged $11000 for intervention schools and $12000 for control schools. The average number of persons living in a household was 5 for intervention and control schools. Twenty-one percent of intervention schools and 18% of control schools had households with single parents. Mother’s level of education was similar for both groups. For each group, 82% of mothers had a high school education or less and 18% had some college education or more. Fifty-five percent of questionnaire respondents from intervention schools and 60% from control schools reported having a fair to poor health status. Family members responding to the questionnaire reported that 55% of children from intervention schools and 60% from control schools had a first- or second-degree relative with diabetes mellitus. See Table 2 for student characteristics.
Table 2.
Baseline Characteristics of Students and Schools in the Bienestar Study
| Characteristic | Control Students (n = 706) | Intervention Students (n = 713) |
|---|---|---|
| Student level | ||
| Age, mean (SD), y | 9.77 (0.49) | 9.79 (0.53) |
| Height, mean (SD), cm | 136.83 (7.23) | 136.91 (7.20) |
| Body mass index, mean (SD), kg/m2 | 20.32 (4.77) | 20.60 (5.09) |
| Sex, % | ||
| M | 51 | 50 |
| F | 49 | 50 |
| Ethnicity, % | ||
| Asian | 6.2 | 5.5 |
| African American | 13.1 | 7.0 |
| Mexican American | 76.7 | 82.5 |
| Other ethnic groups | 4.0 | 5.0 |
| School level* | ||
| Disadvantaged students, mean (SD), % | 95.10 (4.01) | 94.40 (7.18) |
| Mexican American students, mean (SD), % | 86.90 (21.54) | 78.90 (20.36) |
| TAAS performance rating level, mean (SD) | 2.60 (0.96) | 2.60 (0.93) |
Abbreviation: TAAS, Texas Academic Assessment Systems.
Averaged across 13 intervention schools and 14 control schools, respectively.
EVALUATION OF PROGRAM IMPLEMENTATION
Bienestar and school staff delivered 652 sessions of Bienestar programming to the 13 elementary schools in the intervention arm (average of 50 sessions per school): 87 school cafeteria sessions, 26 parent activities, 222 health club sessions, 118 lunch visits, and 199 health and physical education classes. On average, during the 7-month intervention period, a student attended 32 Bienestar sessions.
OUTCOME MEASURES
There was a significant difference in change in FCG levels in intervention and control school students (adjusted difference, −2.24 mg/dL [−0.12 mmol/L]; 95% CI, −6.53 to 2.05 mg/dL [−0.36 to 0.11 mmol/L]; P = .03). The FCG levels decreased in intervention schools and increased in control schools after adjusting for covariates.
At baseline, students in intervention schools had lower fitness scores than those in control schools. At follow-up, however, students in intervention schools increased their fitness scores by 1.81 points, and control students decreased their fitness scores by −0.73 points. The adjusted difference in fitness score change between intervention and control students was significant (1.87 points; 95% CI, −1.44 to 5.17 points; P = .04).
Favorable changes were also observed in intervention students’ dietary fiber intake. After adjusting for covariates, students in intervention schools reportedly consumed significantly higher amounts of dietary fiber than their control counterparts (approximately 1 g/d; 95% CI, −0.53 to 2.51 g/d; P<.009). There were no statistically significant differences in changes in percentage of body fat and percentage of energy intake from saturated fat between intervention and control students (Table 3).
Table 3.
Differences in Bienestar Outcome Values From Baseline to Follow-up Between Students in Control and Intervention Schools*
| Variable | Students, No. | Baseline Value, Mean (SD) | Follow-up Value, Mean (SD) | Crude Change | Adjusted Difference (95% Confidence Interval)† | PValue |
|---|---|---|---|---|---|---|
| FCG, mg/dL‡ | ||||||
| Control | 713 | 89.47 (9.1) | 89.99 (9.7) | 0.52 | ||
| Intervention | 706 | 87.72 (8.3) | 87.53 (9.6) | −0.20 | −2.24 (−4.20 to −0.28) | .03 |
| Body fat, %ठ| ||||||
| Control | 602 | 26.79 (10.8) | 26.09 (10.9) | −0.71 | ||
| Intervention | 619 | 27.96 (11.5) | 26.86 (11.1) | −1.10 | 0.18 (−0.45 to 0.81) | .56 |
| Physical fitness score‡§|| | ||||||
| Control | 602 | 65.93 (12.6) | 65.20 (15.0) | −0.73 | ||
| Intervention | 619 | 63.90 (14.4) | 65.71 (13.8) | 1.81 | 1.87 (0.09 to 3.65) | .04 |
| Dietary fiber intake, g‡ | ||||||
| Control | 569 | 10.79 (4.8) | 10.65 (4.7) | −0.15 | ||
| Intervention | 581 | 11.15 (5.2) | 11.53 (4.7) | 0.38 | 0.99 (0.30 to 1.68) | .009 |
| Energy intake from saturated fat, % | ||||||
| Control | 569 | 38.01 (7.1) | 36.66 (6.8) | −1.35 | ||
| Intervention | 581 | 37.53 (7.5) | 35.97 (7.3) | −1.56 | −0.68 (−2.01 to 0.65) | .34 |
Abbreviation: FCG, fasting capillary glucose.
Sample sizes vary slightly for each regression equation owing to missing data.
Adjusted difference is the difference in change score in the intervention group compared with the control group after controlling for sex, ethnicity, age, height change, and baseline value of outcome measures (baseline total energy intake was adjusted for dietary fiber intake and percentage of energy intake from saturated fat) and school covariate(s).
Baseline values for outcome measures were allowed to vary at random.
Percentage of disadvantaged students in the school was retained as a school-level covariate.
The school’s performance rating level, based on the Texas Academic Assessment Systems, was retained as a school-level covariate.
COMMENT
The Bienestar Health Program is a culturally appropriate school-based diabetes mellitus prevention program aimed at reducing the risk associated with type 2 diabetes mellitus in low-income Mexican American children. During a 7-month period, Bienestar students showed more favorable changes in FCG, dietary fiber, and fitness levels than control students.
Positive results may have been the outcome of culturally appropriate material, multiple systems of delivery, and the frequency of contacts. Theory suggests that children from ethnic populations may improve their understanding of learning material if the curriculum uses examples and content from his or her own culture to illustrate key concepts, principles, and generalizations.37 A second factor that may explain positive results was the delivery system. The Bienestar intervention was delivered through 4 social systems that were designed to have an effect on children’s health behaviors. Programs with added social support and peer pressure have been shown to improve compliance and health outcomes.38 Finally, positive results may have occurred because of the frequency of program exposures. Students averaged 32 sessions of health education programming per school year. To produce statistically significant physiologic effects, a health intervention may need up to 20 sessions of programming a year.39,40
Decreasing dietary fat intake was one of the program’s objectives, and although dietary fat intake did not decrease statistically significantly, the FCG level did. Our review of the literature showed that in nondiabetic populations, glucose metabolism might be more closely related to dietary fiber intake than to dietary fat intake. A study41 of healthy youth showed that dietary intake of fruits and vegetables, and not dietary fat, was related to insulin sensitivity. A study42 of diabetic youth, on the other hand, showed a relationship between decreased dietary fat intake and type 2 diabetes mellitus control. Similarly, studies of healthy adults showed that glucose metabolism is more closely related to dietary fiber12,43,44 than to dietary fat,45–47 and studies of diabetic adults showed that glucose metabolism is more closely related to dietary fat40,48,49 than to dietary fiber.50,51 These findings suggest that dietary interventions might need to be tailored differently according to whether the goal is diabetes mellitus prevention or treatment.
Another risk factor that was not modified substantially in this study was body fat. Weight management seems to be the single most important lifestyle factor for the prevention of type 2 diabetes mellitus in adults.4,5,7 Although weight loss to decrease the risk of diabetes mellitus may be feasible in adults, it may be more difficult in prepubertal children, who go through yearly increases in body weight and body fat as part of their normal growth and development.52 However, even without weight loss, diabetes mellitus prevention may still be feasible as a result of the direct impact of physical activity on FCG concentration.53 A meta-analysis54 of controlled clinical trials in adults showed that exercise exerted a favorable effect on type 2 diabetes mellitus even without weight loss.
Although the Bienestar Health Program had a favorable effect on FCG concentration, fitness levels, and mean dietary fiber intake, it is unknown whether these outcomes will be sustained over time. To eventually prevent diabetes mellitus, at-risk children most likely need to incorporate healthy eating behaviors and physical activity as lifetime habits. In the Bienestar Health Program, the goal is to develop in children a positive belief related to healthful food choices and physical activity and to increase social support for both. If a child develops positive beliefs about food choices and physical activity and has parents, peers, teachers, cafeteria personnel, school administrators, and after-school caretakers constantly encouraging and supporting these beliefs, then these foundations should result in children sustaining healthy behaviors into adolescence. Continued measurements during the next 4 years will test the validity of these assumptions.
What This Study Adds
The number of new cases of type 2 diabetes mellitus in low-income children is growing. High levels of modifiable risk factors associated with type 2 diabetes mellitus (high fat intake, low fiber intake, low physical activity levels, and obesity) have also been reported in low-income children. The Bienestar Health Program was developed to reduce or prevent type 2 diabetes mellitus in low-income children. The success of the program is credited to the coordinated approach and the collaboration among students, parents, teachers, coaches, school administrators, school nurses, and cafeteria staff.
The positive effect of lifestyle changes on FCG levels is encouraging. Two other randomized controlled trials55,56 have also shown the positive effects of lifestyle changes on glucose metabolism. In one study,55 79 healthy adults with underlying insulin resistance were randomly assigned to either an intensive behavior modification program or a control group. Individuals in the intensive program, compared with their control counterparts, had substantial improvement in insulin sensitivity during the 4-month study. Similar to the present findings, parallel improvement in fitness and dietary fiber intake occurred, but no improvements in total and saturated fat intakes were reported among the program participants. The second study was the Diabetes Prevention Program study,56 in which 3234 nondiabetic adults with elevated fasting and postload glucose levels were randomized to receive placebo, metformin, or lifestyle changes. After average follow-up of 2.8 years, the incidence of diabetes mellitus was 11.0, 7.8, and 4.8 cases per 100 person-years in the placebo, metformin, and lifestyle groups, respectively. These studies again show the promising effects of lifestyle changes on controlling diabetes mellitus.
In conclusion, the Bienestar Health Program is a culturally appropriate school-based diabetes mellitus prevention program aimed at low-income Mexican American children and their families residing in an urban area. The program, in a randomized controlled trial, statistically significantly increased fitness scores and dietary fiber intakes and decreased FCG levels. Although these positive results are encouraging, further research is needed to examine long-term effects, translation to other high-risk populations, and cost-effectiveness.
Footnotes
This study was supported in part by grant DK59213-03 from the National Institutes of Health–National Institute of Diabetes and Digestive and Kidney Disease, Bethesda, Md, and by the University Health System, San Antonio.
References
- 1.Harris MI, Goldstein DE, Flegal KM, et al. Prevalence of diabetes, impaired fasting glucose, and impaired glucose tolerance in US adults: the third National Health Nutrition Examination Survey. Diabetes Care. 1998;21:518–524. doi: 10.2337/diacare.21.4.518. [DOI] [PubMed] [Google Scholar]
- 2.Neufeld ND, Chen YI, Raffel LJ. Early presentation of type 2 diabetes in Mexican-American youth. Diabetes Care. 1998;21:80–86. doi: 10.2337/diacare.21.1.80. [DOI] [PubMed] [Google Scholar]
- 3.Hale DE, Danney MM. Non-insulin dependent diabetes in the Hispanic youth [abstract] Diabetes. 1998;47:A82. [Google Scholar]
- 4.Wing RR, Polley BA, Venditti E, Lang W, Jakicic JM. Lifestyle intervention in overweight individuals with a family history of diabetes. Diabetes Care. 1998;21:350–359. doi: 10.2337/diacare.21.3.350. [DOI] [PubMed] [Google Scholar]
- 5.O’Sullivan JB. Body weight and subsequent diabetes mellitus. JAMA. 1982;248:949–952. [PubMed] [Google Scholar]
- 6.Knowler WC, Pettitt DJ, Savage PJ, Bennett PH. Diabetes incidence in Pima Indians: contributions of obesity and parental diabetes. Am J Epidemiol. 1981;113:144–156. doi: 10.1093/oxfordjournals.aje.a113079. [DOI] [PubMed] [Google Scholar]
- 7.Long SD, O’Brien K, MacDonald KG, et al. Weight loss in severely obese subjects prevents the progression of impaired glucose tolerance to type II diabetes. Diabetes Care. 1994;17:372–375. doi: 10.2337/diacare.17.5.372. [DOI] [PubMed] [Google Scholar]
- 8.Mayer-Davis JE, D’Agostino R, Karter AJ, et al. Intensity and amount of physical activity in relation to insulin sensitivity: the Insulin Resistance Atherosclerosis Study. JAMA. 1998;279:669–674. doi: 10.1001/jama.279.9.669. [DOI] [PubMed] [Google Scholar]
- 9.Helmrich S, Raglund D, Leung W, Paffewnbarger R. Activity and reduced occurrence of non–insulin-dependent diabetes mellitus. N Engl J Med. 1991;325:147–152. doi: 10.1056/NEJM199107183250302. [DOI] [PubMed] [Google Scholar]
- 10.Manson J, Rimm E, Stampfer MJ, et al. Physical activity and incidence of non–insulin-dependent diabetes mellitus in women. Lancet. 1991;338:774–778. doi: 10.1016/0140-6736(91)90664-b. [DOI] [PubMed] [Google Scholar]
- 11.Grunfield C, Baird K, Kahn C. Maintenance of 3T3-L1 cell in culture media constraining saturated fatty acids decreases insulin binding and insulin action. Biochem Biophys Res Commun. 1981;103:219–226. doi: 10.1016/0006-291x(81)91682-x. [DOI] [PubMed] [Google Scholar]
- 12.Salmeron J, Manson JE, Stampfer MJ, Colditz GA, Wing AL, Willett WC. Dietary fiber, glycemic load, and risk of non–insulin-dependent diabetes mellitus in women. JAMA. 1997;277:472–477. doi: 10.1001/jama.1997.03540300040031. [DOI] [PubMed] [Google Scholar]
- 13.Baumgartner RN, Roche AF, Guo S, Chumlea WC, Ryan AS. Fat patterning and centralized obesity in Mexican-American children in the Hispanic Health and Nutrition Examination Survey (HHANES 1982–1984) Am J Clin Nutr. 1990;51:936S–943S. [Google Scholar]
- 14.Strauss RS, Pollack HA. Epidemic increase in childhood overweight, 1986–1998. JAMA. 2001;286:2845–2848. doi: 10.1001/jama.286.22.2845. [DOI] [PubMed] [Google Scholar]
- 15.Kaplowitz H, Martorell R, Mendoza FS. Fatness and fat distribution in Mexican-American children and youths from the Hispanic Health and Nutrition Examination Survey. Am J Hum Biol. 1989;1:631–648. doi: 10.1002/ajhb.1310010514. [DOI] [PubMed] [Google Scholar]
- 16.Murphy SP, Castillo RO, Martorell R, Mendoza FS. An evaluation of food group intakes by Mexican-American children. J Am Diet Assoc. 1990;90:388–393. [PubMed] [Google Scholar]
- 17.Krebs-Smith SM, Cook AD, Subar AF, Cleveland L, Friday J, Kahle LL. Fruit and vegetable intakes of children and adolescents in the United States. Arch Pediatr Adolesc Med. 1996;150:81–86. doi: 10.1001/archpedi.1996.02170260085014. [DOI] [PubMed] [Google Scholar]
- 18.McKenzie TL, Sallis JF, Nader PR, Broyles S, Nelson JA. Anglo- and Mexican-American preschoolers at home and at recess: activity patterns and environmental influences. J Dev Behav Pediatr. 1992;13:173–180. [PubMed] [Google Scholar]
- 19.Wolf AM, Gortmaker SL, Cheung L, Gray HM, Herzog DB, Colditz GA. Activity, inactivity, and obesity: racial, ethnic, and age differences among schoolgirls. Am J Public Health. 1993;83:1625–1627. doi: 10.2105/ajph.83.11.1625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Trevino RP, Marshall RM, Hale DE, Rodriguez R, Baker G, Gomez J. Diabetes risk factors in low-income Mexican-American children. Diabetes Care. 1999;22:202–207. doi: 10.2337/diacare.22.2.202. [DOI] [PubMed] [Google Scholar]
- 21.Pellett PL. Food energy requirements in humans. Am J Clin Nutr. 1990;51:711–722. doi: 10.1093/ajcn/51.5.711. [DOI] [PubMed] [Google Scholar]
- 22.Bandura A. Social Foundations of Thought and Action: A Social Cognitive Theory. Englewood Cliffs, NJ: Prentice-Hall International Inc; 1986.
- 23.McLeroy KR, Bibeau D, Steckler A, Glanz K. An ecological perspective on health promotion programs. Health Educ Q. 1988;15:351–377. doi: 10.1177/109019818801500401. [DOI] [PubMed] [Google Scholar]
- 24.Vygotsky LS. The problem of the cultural development of the child. J Genet Psychol. 1929;35:415–432. [Google Scholar]
- 25.Garza RT, Lipton JP. Theoretical perspectives on Chicano personality development. Hisp J Behav Sci. 1982;4:407–432. [Google Scholar]
- 26.Bruss MB, Morris J, Dannison L. Prevention of childhood obesity: sociocultural and familial factors. J Am Diet Assoc. 2003;103:1042–1045. doi: 10.1016/s0002-8223(03)00472-3. [DOI] [PubMed] [Google Scholar]
- 27.American Diabetes Association. Screening for type 2 diabetes. Diabetes Care. 2003;26(suppl 1):S21–S24. doi: 10.2337/diacare.26.2007.s21. [DOI] [PubMed] [Google Scholar]
- 28.American Diabetes Association. Screening for type 2 diabetes. Diabetes Care. 2004;27(suppl 1):S11–S14. doi: 10.2337/diacare.27.2007.s11. [DOI] [PubMed] [Google Scholar]
- 29.Frank GC, Berenson GS, Schilling PE, Moore MC. Adapting the 24-hour recall for epidemiological studies of school children. J Am Diet Assoc. 1977;71:26–31. [PubMed] [Google Scholar]
- 30.Carter RI, Sharbaugh CO, Stapeli CA. Reliability and validity of the 24-hour recall. J Am Diet Assoc. 1981;79:542–547. [PubMed] [Google Scholar]
- 31.Sallis JF, Buono MJ, Roby JJ, Micale FG, Nelson JA. Seven-day recall and other physical activity self-reports in children and adolescents. Med Sci Sports Exerc. 1993;25:99–108. doi: 10.1249/00005768-199301000-00014. [DOI] [PubMed] [Google Scholar]
- 32.Saris WH. Habitual physical activity in children: methodology and findings in health and disease. Med Sci Sports Exerc. 1986;18:253–263. doi: 10.1249/00005768-198606000-00001. [DOI] [PubMed] [Google Scholar]
- 33.Gutin B, Islam S, Manos T, Cucuzzo N, Smith C, Stachura ME. Relation of percentage of body fat and maximal aerobic capacity to risk factors for atherosclerosis and diabetes in black and white seven- to eleven-year-old children. J Pediatr. 1994;125:847–852. doi: 10.1016/s0022-3476(05)81997-3. [DOI] [PubMed] [Google Scholar]
- 34.Daniels SR, Khoury PR, Morrison JA. The utility of body mass index as a measure of body fatness in children and adolescents: differences by race and gender. Pediatrics. 1997;99:804–807. doi: 10.1542/peds.99.6.804. [DOI] [PubMed] [Google Scholar]
- 35.Murray DM. Design and Analysis of Group-Randomized Trials. Vol 27. New York, NY: Oxford University Press; 1998.
- 36.Raudenbush SW, Bryk AS, Cheong YF. HLM 5: Hierarchical Linear and Nonlinear Modeling. 2nd ed. Chicago, III: Scientific Software International Inc; 2001.
- 37.Erickson F. Culture in society and in educational practices. In: Banks JA, McGee Banks C, eds. Multicultural Education: Issues and Perspectives. 3rd ed. Boston, Mass: Allyn & Bacon; 1977.
- 38.Perri MG, McAllister DA, Gange JJ, Nezu AM. Effects of four maintenance programs on the long-term management of obesity. J Consult Clin Psychol. 1988;56:529–534. doi: 10.1037//0022-006x.56.4.529. [DOI] [PubMed] [Google Scholar]
- 39.Resnicow K, Robinson TN, Frank E. Advances and future directions for school-based health promotion research: commentary on the CATCH intervention trial. Prev Med. 1996;25:378–383. doi: 10.1006/pmed.1996.0070. [DOI] [PubMed] [Google Scholar]
- 40.Swinburn BA, Metcalf PA, Ley SJ. Long-term (5-year) effects of a reduced fat diet intervention in individuals with glucose intolerance. Diabetes Care. 2001;24:619–624. doi: 10.2337/diacare.24.4.619. [DOI] [PubMed] [Google Scholar]
- 41.Lindquist CH, Gower BA, Goran MI. Role of dietary factors in ethnic differences in early risk of cardiovascular disease and type 2 diabetes. Am J Clin Nutr. 2000;71:725–732. doi: 10.1093/ajcn/71.3.725. [DOI] [PubMed] [Google Scholar]
- 42.Pinhas-Hamiel O, Standiford D, Hamiel D, Dolan LM, Cohen R, Zeitler PS. The type 2 family: a setting for development and treatment of adolescent type 2 diabetes mellitus. Arch Pediatr Adolesc Med. 1999;153:1063–1067. doi: 10.1001/archpedi.153.10.1063. [DOI] [PubMed] [Google Scholar]
- 43.Salmeron J, Ascherio A, Rimm EB, et al. Dietary fiber, glycemic load, and risk of NIDDM in men. Diabetes Care. 1997;20:545–550. doi: 10.2337/diacare.20.4.545. [DOI] [PubMed] [Google Scholar]
- 44.Ludwig DS, Pereira MA, Kroenke CH, et al. Dietary fiber, weight gain, and cardiovascular disease risk factors in young adults. JAMA. 1999;282:1539–1546. doi: 10.1001/jama.282.16.1539. [DOI] [PubMed] [Google Scholar]
- 45.Mayer EJ, Newman B, Quesenberry CP, Selby JV. Usual dietary fat intake and insulin concentrations in healthy women twins. Diabetes Care. 1993;16:1459–1469. doi: 10.2337/diacare.16.11.1459. [DOI] [PubMed] [Google Scholar]
- 46.van Dam RM, Willett WC, Rimm EB, Stampfer MJ, Hu FB. Dietary fat and meat intake in relation to risk of type 2 diabetes in men. Diabetes Care. 2002;25:417–424. doi: 10.2337/diacare.25.3.417. [DOI] [PubMed] [Google Scholar]
- 47.Lovejoy JC, Smith SR, Champagne CM, et al. Effects of diets enriched in saturated (palmitic), monounsaturated (oleic), or trans (elaidic) fatty acids on insulin sensitivity and substrate oxidation in healthy adults. Diabetes Care. 2002;25:1283–1288. doi: 10.2337/diacare.25.8.1283. [DOI] [PubMed] [Google Scholar]
- 48.Marshall JA, Hoag S, Shetterly S, Hamman E. Dietary fat predicts conversion from impaired glucose tolerance to NIDDM. Diabetes Care. 1994;17:50–55. doi: 10.2337/diacare.17.1.50. [DOI] [PubMed] [Google Scholar]
- 49.Tsunehara CH, Leonetti DL, Fujimoto WY. Diet of second-generation Japanese-American men with and without non–insulin-dependent diabetes. Am J Clin Nutr. 1990;52:731–738. doi: 10.1093/ajcn/52.4.731. [DOI] [PubMed] [Google Scholar]
- 50.Jenkins DJA, Kendall CWC, Augustin LSA, et al. Effect of wheat bran on glycemic control and risk factors for cardiovascular disease in type 2 diabetes. Diabetes Care. 2002;25:1522–1528. doi: 10.2337/diacare.25.9.1522. [DOI] [PubMed] [Google Scholar]
- 51.Garg A, Bantle JP, Henry RR, et al. Effects of varying carbohydrate content of diet in patients with non–insulin-dependent diabetes mellitus. JAMA. 1994;271:1421–1428. doi: 10.1001/jama.1994.03510420053034. [DOI] [PubMed] [Google Scholar]
- 52.Knittle JL, Timmers K, Ginsberg-Fellner F, Brown RE, Datz DP. The growth of adipose tissue in children and adolescents. J Clin Invest. 1979;63:239–246. doi: 10.1172/JCI109295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Bunt JC, Salbe AD, Harper IT, Hanson RL, Tataranni AP. Weight, adiposity, and physical activity as determinants of an insulin sensitivity index in Pima Indian children. Diabetes Care. 2003;26:2524–2530. doi: 10.2337/diacare.26.9.2524. [DOI] [PubMed] [Google Scholar]
- 54.Boule NG, Haddad E, Kenny GP, Wells GA, Sigal RJ. Effects of exercise on glycemic control and body mass in type 2 diabetes mellitus. JAMA. 2001;286:1218–1227. doi: 10.1001/jama.286.10.1218. [DOI] [PubMed] [Google Scholar]
- 55.McAuley KA, Williams SM, Mann JI, et al. Intensive lifestyle changes are necessary to improve insulin sensitivity. Diabetes Care. 2002;25:445–452. doi: 10.2337/diacare.25.3.445. [DOI] [PubMed] [Google Scholar]
- 56.Diabetes Prevention Program Research Group. Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N Engl J Med. 2002;346:393–403. doi: 10.1056/NEJMoa012512. [DOI] [PMC free article] [PubMed] [Google Scholar]


