Abstract
1 The absorption, protein binding, clearance and absolute bioavailability of tenidap sodium were studied after single and multiple dosing.
2 Thirteen healthy male volunteers received a single 120 mg oral dose of tenidap sodium and a 20 mg intravenous infusion of deuterated tenidap ([D3]-tenidap) on day 1. This was followed by a 6-day washout period (days 2-7) and then further daily doses of oral tenidap sodium 120 mg for 21 consecutive days (days 8-28) with an additional 20 mg intravenous infusion of [D3]-tenidap on day 28. Twelve subjects were eligible for pharmacokinetic evaluation.
3 Following multiple oral doses, the half-life of tenidap is approximately 23 h.
4 Following single and multiple dose administration, the absolute bioavailability is 85%.
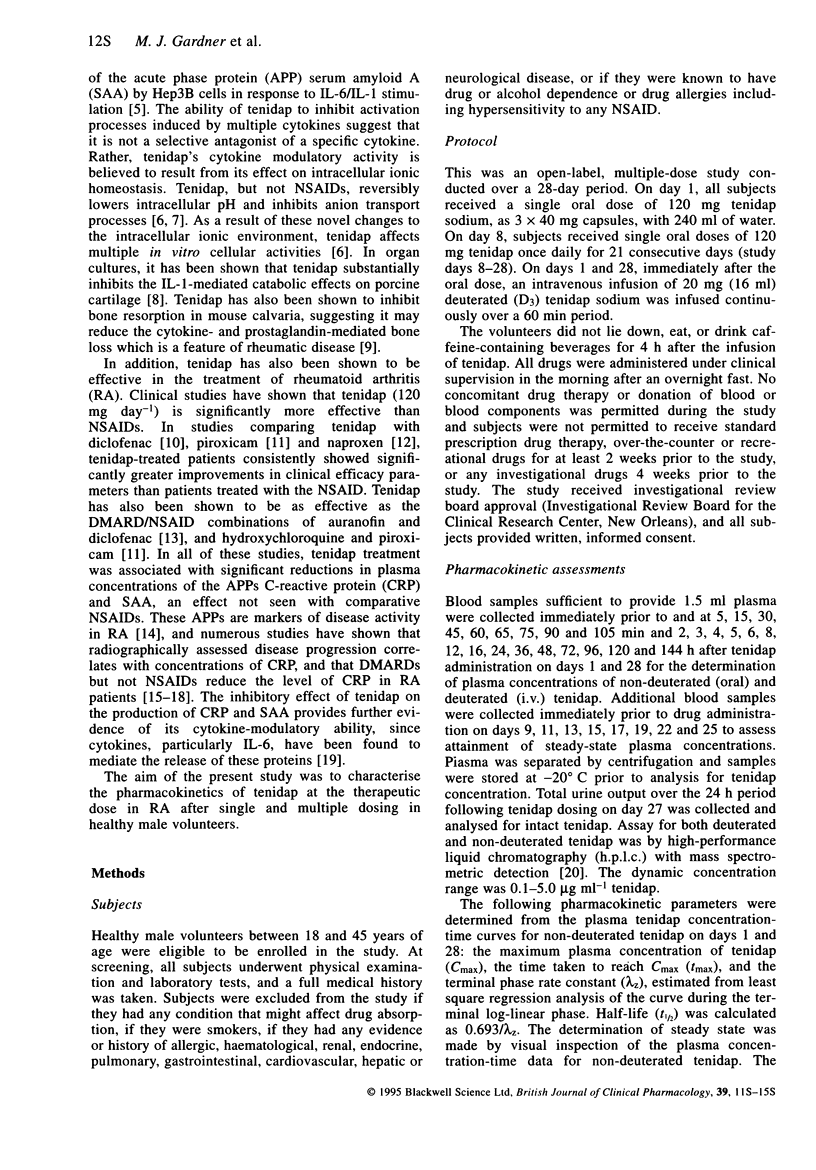
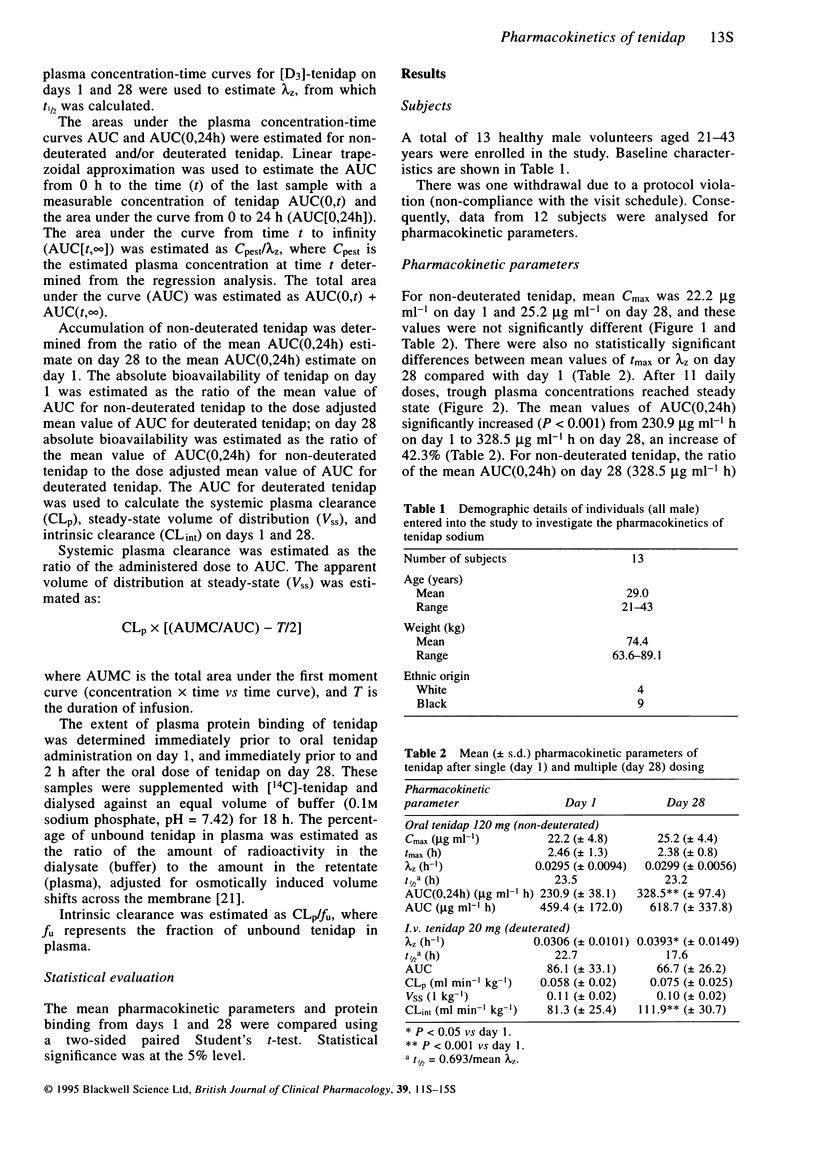
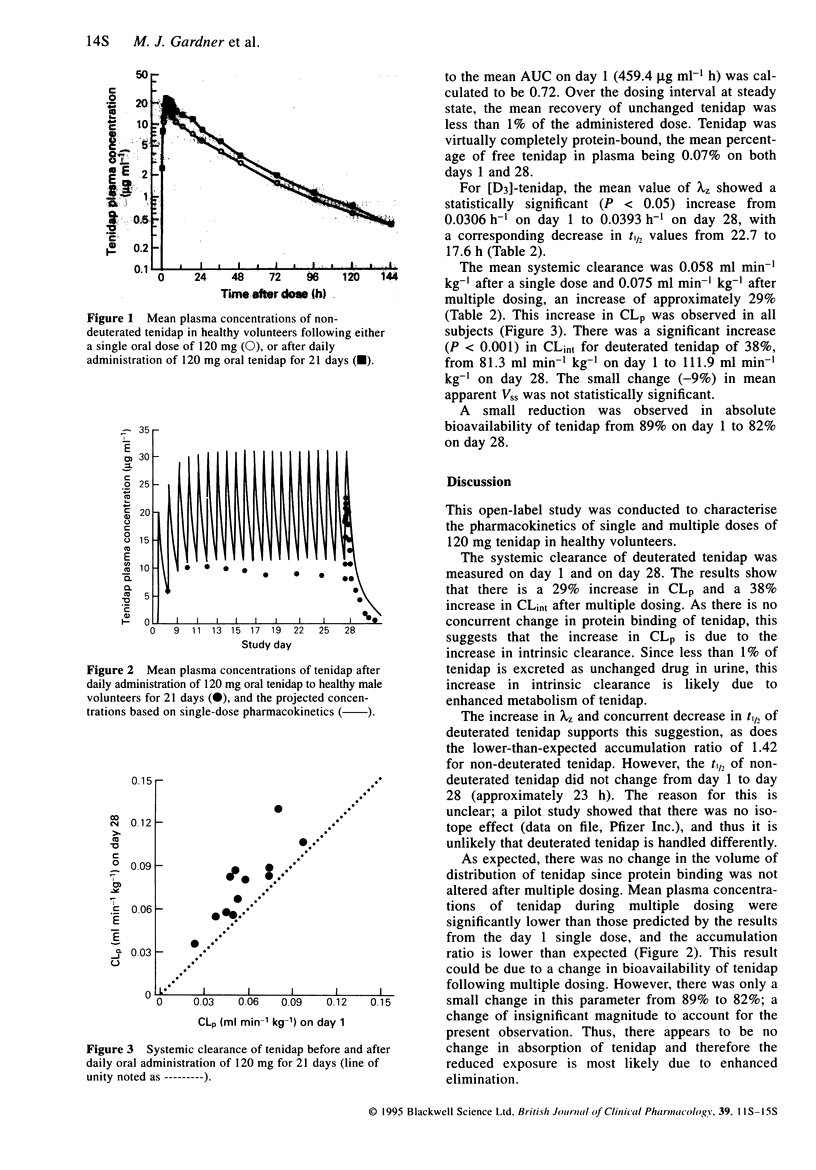
5 Systemic clearance of [D3]-tenidap was 29% greater on day 28 than on day 1 indicating a significant increase in intrinsic clearance (CLint) of tenidap since protein binding of tenidap in plasma did not change during the study. Consistent with the increase in systemic clearance, the half-life of [D3]-tenidap decreased and the ratio of AUC(0,24h) day 28/AUC day 1 following oral dosing was less than one. Tenidap is subject to extensive hepatic metabolism, so the increase in CLint may indicate that tenidap induces its own metabolism.
6 Steady-state was achieved by the eleventh day of dosing. Since numerous studies in patients with rheumatoid arthritis have shown that multiple dosing with tenidap is clinically efficacious, this suggests that the pharmacokinetic differences observed between the first and twenty-first day of multiple tenidap dosing do not influence the clinical response.
Keywords: tenidap dosing, pharmacokinetics, metabolism, protein binding
Full text
PDF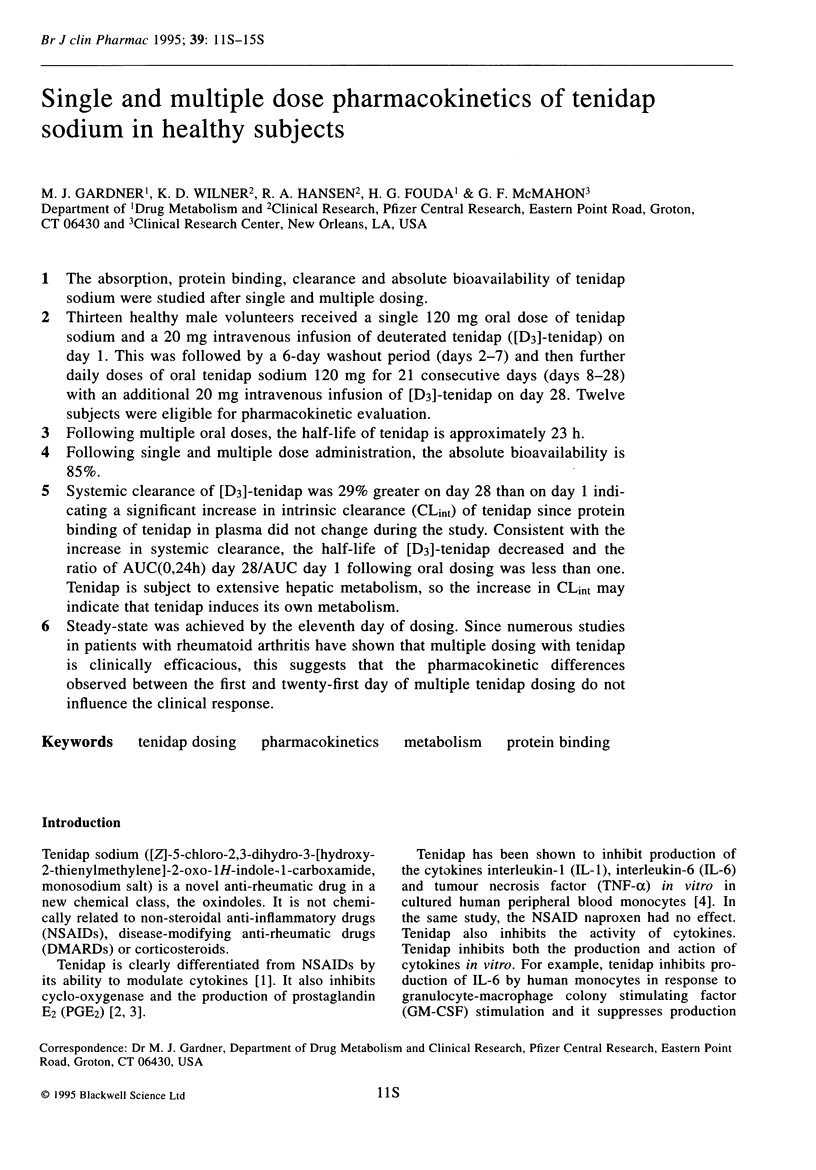
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Amos R. S., Constable T. J., Crockson R. A., Crockson A. P., McConkey B. Rheumatoid arthritis: relation of serum C-reactive protein and erythrocyte sedimentation rates to radiographic changes. Br Med J. 1977 Jan 22;1(6055):195–197. doi: 10.1136/bmj.1.6055.195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Avery M. J., Mitchell D. Y., Falkner F. C., Fouda H. G. Simultaneous determination of tenidap and its stable isotope analog in serum by high-performance liquid chromatography/atmospheric pressure chemical ionization tandem mass spectrometry. Biol Mass Spectrom. 1992 Jul;21(7):353–357. doi: 10.1002/bms.1200210706. [DOI] [PubMed] [Google Scholar]
- Bertilsson L., Tomson T. Clinical pharmacokinetics and pharmacological effects of carbamazepine and carbamazepine-10,11-epoxide. An update. Clin Pharmacokinet. 1986 May-Jun;11(3):177–198. doi: 10.2165/00003088-198611030-00001. [DOI] [PubMed] [Google Scholar]
- Boudinot F. D., Jusko W. J. Fluid shifts and other factors affecting plasma protein binding of prednisolone by equilibrium dialysis. J Pharm Sci. 1984 Jun;73(6):774–780. doi: 10.1002/jps.2600730617. [DOI] [PubMed] [Google Scholar]
- Chatham W. W., Swaim R., Frohsin H., Jr, Heck L. W., Miller E. J., Blackburn W. D., Jr Degradation of human articular cartilage by neutrophils in synovial fluid. Arthritis Rheum. 1993 Jan;36(1):51–58. doi: 10.1002/art.1780360109. [DOI] [PubMed] [Google Scholar]
- Dawes P. T., Fowler P. D., Clarke S., Fisher J., Lawton A., Shadforth M. F. Rheumatoid arthritis: treatment which controls the C-reactive protein and erythrocyte sedimentation rate reduces radiological progression. Br J Rheumatol. 1986 Feb;25(1):44–49. doi: 10.1093/rheumatology/25.1.44. [DOI] [PubMed] [Google Scholar]
- Dingle J. T., Leeming M. R., Martindale J. J. Effect of tenidap on cartilage integrity in vitro. Ann Rheum Dis. 1993 Apr;52(4):292–299. doi: 10.1136/ard.52.4.292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Emery P., Luqmani R. The validity of surrogate markers in rheumatic disease. Br J Rheumatol. 1993 Jun;32 (Suppl 3):3–8. doi: 10.1093/rheumatology/32.suppl_3.3. [DOI] [PubMed] [Google Scholar]
- Heinrich P. C., Castell J. V., Andus T. Interleukin-6 and the acute phase response. Biochem J. 1990 Feb 1;265(3):621–636. doi: 10.1042/bj2650621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Laliberte R., Perregaux D., Svensson L., Pazoles C. J., Gabel C. A. Tenidap modulates cytoplasmic pH and inhibits anion transport in vitro. II. Inhibition of IL-1 beta production from ATP-treated monocytes and macrophages. J Immunol. 1994 Sep 1;153(5):2168–2179. [PubMed] [Google Scholar]
- Loose L. D., Sipe J. D., Kirby D. S., Kraska A. R., Weiner E. S., Shanahan W. R., Leeming M. R., Farrow P., Stack C. B., Ting N. Reduction of acute-phase proteins with tenidap sodium, a cytokine-modulating anti-rheumatic drug. Br J Rheumatol. 1993 Jun;32 (Suppl 3):19–25. doi: 10.1093/rheumatology/32.suppl_3.19. [DOI] [PubMed] [Google Scholar]
- Mallya R. K., de Beer F. C., Berry H., Hamilton E. D., Mace B. E., Pepys M. B. Correlation of clinical parameters of disease activity in rheumatoid arthritis with serum concentration of C-reactive protein and erythrocyte sedimentation rate. J Rheumatol. 1982 Mar-Apr;9(2):224–228. [PubMed] [Google Scholar]
- McNiff P., Svensson L., Pazoles C. J., Gabel C. A. Tenidap modulates cytoplasmic pH and inhibits anion transport in vitro. I. Mechanism and evidence of functional significance. J Immunol. 1994 Sep 1;153(5):2180–2193. [PubMed] [Google Scholar]
- Moilanen E., Alanko J., Asmawi M. Z., Vapaatalo H. CP-66,248, a new anti-inflammatory agent, is a potent inhibitor of leukotriene B4 and prostanoid synthesis in human polymorphonuclear leucocytes in vitro. Eicosanoids. 1988;1(1):35–39. [PubMed] [Google Scholar]
- Sipe J. D., Bartle L. M., Loose L. D. Modification of proinflammatory cytokine production by the antirheumatic agents tenidap and naproxen. A possible correlate with clinical acute phase response. J Immunol. 1992 Jan 15;148(2):480–484. [PubMed] [Google Scholar]
- van Leeuwen M. A., van der Heijde D. M., van Rijswijk M. H., Houtman P. M., van Riel P. L., van de Putte L. B., Limburg P. C. Interrelationship of outcome measures and process variables in early rheumatoid arthritis. A comparison of radiologic damage, physical disability, joint counts, and acute phase reactants. J Rheumatol. 1994 Mar;21(3):425–429. [PubMed] [Google Scholar]


