Abstract
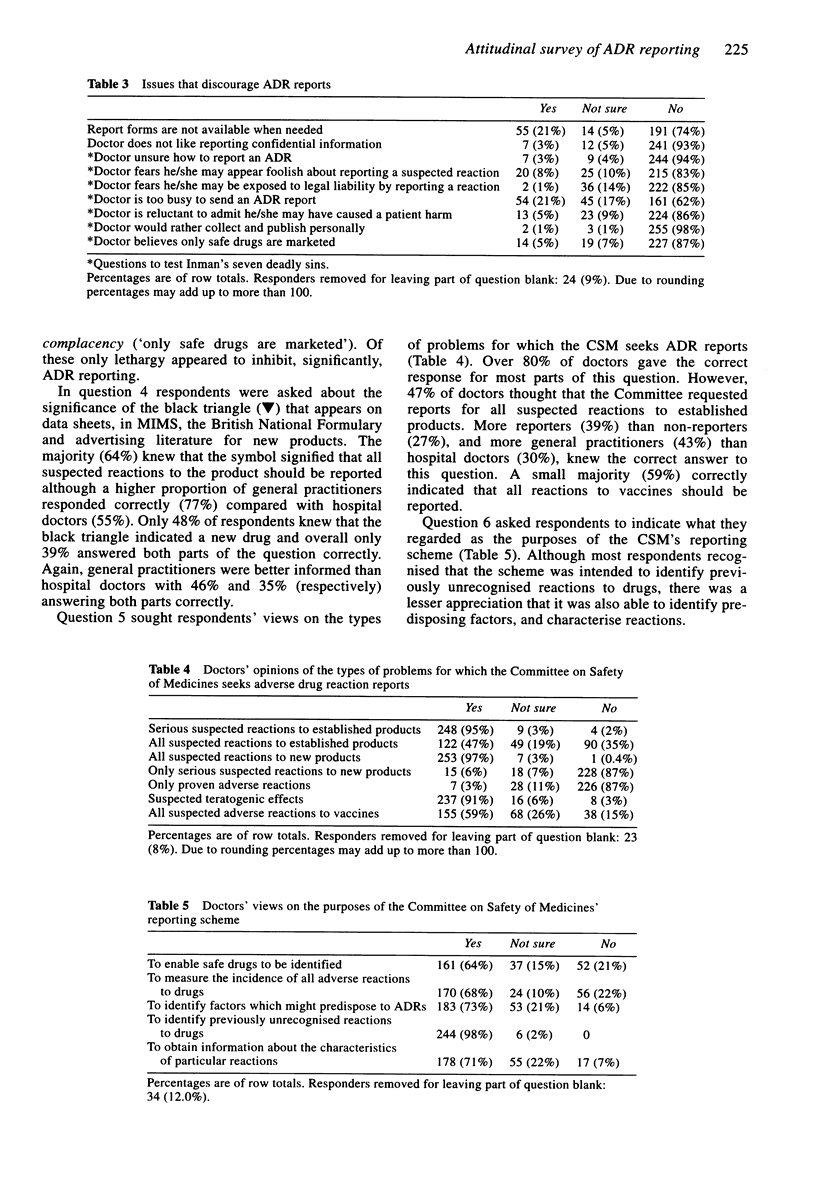
1. Attitudes of doctors to the Committee on Safety of Medicines' (CSM) adverse drug reaction (ADR) reporting scheme were investigated in order to assess their understanding of the purposes of the scheme and to identify reasons for failing to report suspected adverse drug reactions. 2. A postal questionnaire and letter of invitation were sent to 500 doctors who were randomly selected from the 1992 Medical Directory. A reminder letter and a second copy of the questionnaire were sent to non-responders after 4 weeks. 3. 284 (57%) responded to the questionnaire. Of these, 179 (63%) stated that they had previously reported an ADR to the CSM or a pharmaceutical manufacturer. 77% of general practitioners stated that they had reported one or more ADRs compared with 55% of hospital doctors. 4. Reasons for under-reporting included lack of time, lack of report forms and the misconception that absolute confidence in the diagnosis of an adverse reaction was important in the decision to send in a report. 5. An investigation of seven commonly proposed reasons for under-reporting showed that on the whole they did not apply. 6. Most doctors knew the types of reactions that the Committee on Safety of Medicines seeks reports for but only 38% knew the precise meaning of the Committee on Safety of Medicines' black triangle symbol. There also seemed to be confusion about some of the purposes of the adverse drug reaction reporting scheme. 7. The number of reporting doctors is much higher than has previously been estimated.(ABSTRACT TRUNCATED AT 250 WORDS)
Full text
PDF


Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Bateman D. N., Sanders G. L., Rawlins M. D. Attitudes to adverse drug reaction reporting in the Northern Region. Br J Clin Pharmacol. 1992 Nov;34(5):421–426. [PMC free article] [PubMed] [Google Scholar]
- Koch-Weser J., Sidel V. W., Sweet R. H., Kanarek P., Eaton A. E. Factors determining physician reporting of adverse drug reactions. Comparison of 2000 spontaneous reports with surveillance studies at the Massachusetts General Hospital. N Engl J Med. 1969 Jan 2;280(1):20–26. doi: 10.1056/NEJM196901022800105. [DOI] [PubMed] [Google Scholar]
- Rawlins M. D. Spontaneous reporting of adverse drug reactions. I: the data. Br J Clin Pharmacol. 1988 Jul;26(1):1–5. doi: 10.1111/j.1365-2125.1988.tb03356.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rogers A. S., Israel E., Smith C. R., Levine D., McBean A. M., Valente C., Faich G. Physician knowledge, attitudes, and behavior related to reporting adverse drug events. Arch Intern Med. 1988 Jul;148(7):1596–1600. [PubMed] [Google Scholar]
- Speirs C. J., Griffin J. P., Weber J. C., Glen-Bott M. Demography of the UK adverse reactions register of spontaneous reports. Health Trends. 1984 Aug;16(3):49–52. [PubMed] [Google Scholar]


