Abstract
During human immunodeficiency virus type 1 (HIV-1) infection, disease progression correlates with the occurrence of variants using the coreceptor CXCR4 for cell entry. In contrast, apathogenic simian immunodeficiency virus (SIV) from African green monkeys (SIVagm), specifically the molecular virus clone SIVagm3mc, uses CCR5, Bob, and Bonzo as coreceptors throughout the course of infection. The influence of an altered coreceptor usage on SIVagm3mc replication was studied in vitro and in vivo. The putative coreceptor binding domain, the V3 region of the surface envelope (SU) glycoprotein, was replaced by the V3 loop of a CD4- and CXCR4-tropic HIV-1 strain. The resulting virus, termed SIVagm3-X4mc, exclusively used CD4 and CXCR4 for cell entry. Consequently, its in vitro replication was inhibited by SDF-1, the natural ligand of CXCR4. Surprisingly, SIVagm3-X4mc was able to replicate in vitro not only in interleukin-2- and phytohemagglutinin-stimulated but also in nonstimulated peripheral blood mononuclear cells (PBMCs) from nonhuman primates. After experimental infection of two pig-tailed macaques with either SIVagm3-X4mc or SIVagm3mc, the coreceptor usage was maintained during in vivo replication. Cell-associated and plasma viral loads, as well as viral DNA copy numbers, were found to be comparable between SIVagm3mc and SIVagm 3-X4mc infections, and no pathological changes were observed up to 14 months postinfection. Interestingly, the V3 loop exchange rendered SIVagm3-X4mc susceptible to neutralizing antibodies present in the sera of SIVagm3-X4mc- and SIVagm3mc-infected pig-tailed macaques. Our study describes for the first time a successful exchange of a V3 loop in nonpathogenic SIVagm resulting in CD4 and CXCR4 usage and modulation of virus replication in nonstimulated PBMCs as well as sensitivity toward neutralization.
Cell entry of human immunodeficiency virus (HIV) and simian immunodeficiency virus (SIV) is mediated by the association of the viral surface envelope (SU) glycoprotein with the cellular receptor CD4 and subsequent interactions with one of several chemokine receptors (6, 18). During cell entry of HIV type 1 (HIV-1), CD4 binding triggers conformational changes in the envelope (Env) proteins, resulting in the exposure of a conserved chemokine receptor binding domain of the SU protein. A second conformational change induced by chemokine receptor binding results in fusion peptide exposure and, ultimately, in fusion between the viral and host cell membranes (52). The V3 loop in the third variable region of gp120-SU is known to be involved in coreceptor binding of HIV-1 (13). Similarly, the V3 loops in the SU proteins of HIV-2 (1, 28) and of SIVmac from rhesus macaques (Macaca mulatta [31]) also influence the coreceptor specificity and cell tropism of the respective viruses. Whether the corresponding V3 region in gp130-SU of SIVagm from African green monkeys (AGM; genus Chlorocebus) also influences the coreceptor specificity of SIVagm (39) from the AGM (Chlorocebus aethiops) has not been tested.
The main coreceptors used by HIV-1 are CCR5 and CXCR4 (13). A number of alternative coreceptors have been described (50). In the course of infection, CCR5-using virus variants dominate in virus isolates obtained early after infection and persist throughout all stages of disease. CXCR4-using or, in some cases, dual-tropic (CCR5- and CXCR4-using) virus variants emerge later during disease (6). The emergence of HIV-1 variants able to use CXCR4 or several other coreceptors is correlated with a rapid decline in the number of peripheral CD4+ T cells and progression to AIDS (14). In comparison to HIV-1, HIV-2 is generally promiscuous in its coreceptor usage and tends to use alternative coreceptors besides CCR5 and CXCR4 (18). It is intriguing that, in contrast to HIV-1 or HIV-2, SIVs from phylogenetically distinct groups, like SIVmac and SIVagm, mainly use CCR5 for cell entry but usually not CXCR4 (11, 18). A known exception is SIVmnd(GB-1), isolated from a mandrill (Papio sphinx), which mainly uses CXCR4 as a coreceptor (47). Besides CCR5, several orphan receptors have been reported to support SIV entry in vitro (19, 45), especially Bob and Bonzo (15). The relevance of the usage of these coreceptors for replication and/or pathogenesis in vivo remains largely unknown, although it has recently been shown that Bob and Bonzo usage is of limited importance for SIVmac replication in vivo (42). As CXCR4 usage does not develop during the progression of disease in SIVmac-infected macaques (10), it is conceivable that a CXCR4 switch is not important for SIVmac pathogenesis. It is, however, striking that SIV rarely uses CXCR4 for cell entry because (i) macaque-, mangabey-, and AGM-derived CXCR4 receptors mediate infection by HIV (10, 17, 37), which shows that these receptors can function as coreceptors during lentiviral cell entry, and (ii) CXCR4-tropic SIVmac-HIV-1 hybrid viruses, the so-called SHIVs, replicate efficiently and induce a rapid decline in the number of peripheral CD4-positive lymphocytes in infected macaques (22, 35).
For HIV-2, as for HIV-1, it has been shown that a shift in coreceptor usage from CCR5 to CXCR4 is associated with an increase in the net positive charge of the V3 loop (28). Single amino acid substitutions increasing the net positive charge of the V3 loop of the SIVmac SU protein led to altered coreceptor usage but did not allow efficient utilization of CXCR4 (38). In addition to SIVcpz from chimpanzees (Pan troglodytes) and SIVsm from sooty mangabeys (Cercocebus atys), SIVagm is one of the well-studied primate lentiviruses and belongs to a phylogenetically distinct group. In spite of 30 to 40% of adult AGM being infected in the wild (29), they do not develop any symptoms reminiscent of an acquired immunodeficiency or suffer from a decline in peripheral CD4-positive lymphocytes (12). Two nonpathogenic molecular SIVagm clones, SIVagmSab1.4 and SIVagmTYO, revealed a strong preference for CCR5, Bob, and Bonzo usage (15, 19).
To assess the replication properties and the pathogenicity of an SIVagm variant able to use CXCR4 as a coreceptor for cell entry, we modified SIVagm3mc (2) to yield a CXCR4-using variant called SIVagm3-X4mc. Like SIVagm3mc (3), SIVagm3-X4mc did not cause disease in pig-tailed (PT) macaques (Macaca nemestrina), as presented here. However, in contrast to SIVagm3mc, SIVagm3-X4mc acquired new properties, including replication in nonstimulated AGM and PT macaque peripheral blood mononuclear cells (PBMCs), replicated efficiently in experimentally infected PT macaques under maintenance of CD4 and CXCR4 usage, and was highly sensitive to neutralizing antibodies present in the sera of SIVagm3mc- and SIVagm3-X4mc-infected PT macaques.
MATERIALS AND METHODS
Plasmid construction.
The construction and complete sequence of the proviral plasmid clone pSIVagm3 (SIVagm3mc [GenBank accession no. M30931]; numbering starting at nucleotide 1 [A1] of the R region of the long terminal repeat [LTR]) have been described previously (3). Plasmid pSN3.9 was constructed by inserting the subgenomic region from SacI (A5386) to NarI (A222) containing the 3′ half of provirus pSIVagm3mc into the plasmid pBluescript (Stratagene, Heidelberg, Germany) (16). Plasmid pSIVagm3-X4mc was generated by precise replacement of the V3 loop of SIVagm3mc (amino acids 6726 to 6827) in pSIVagm3 by the V3 loop of HIV-1 strain BH10 (amino acids 6465 to 6572; GenBank accession no. M15654; numbering starting at nucleotide 1 [B1] of the R region of the LTR) using fusion PCR techniques according to the method of Horton et al. (27). The HIV-1 Env expression construct pTr712 (51) harboring a C-terminally truncated variant of the T-cell-tropic HIV-1 Env strain BH10 (44), a gift from V. Bosch (Deutsches Krebsforschungszentrum, Heidelberg, Germany), was used as a template for the PCR. To generate subclone pSN3.9V3 containing the replaced V3 loop, three subgenomic fragments were amplified using the primers A6199(+) (CCACTTTGCCGTGTGTCCAGAACAAG) and A6724(−) (GTAACTGTTAGATTGTAATG) (the 5′ fragment), A6828(+) (CACTTCCAGGGCAACTGGAG) and A7427(−) (GCCTAGGAACCCTAGCACGAACGGG) (the 3′ fragment), and A6705/B6464(+) (CATTACAATCTAACAGTTACTTGCACAAGACCCAACAACAATAC) and A6847/B6572(−) (CTCCAGTTGCCCTGGAAGTGACAATGTGCTTGTCTCATATTTCC) (the central fragment). (Italicized letters indicate the overhanging portion of the primer that is homologous to the portion of the respective genome.) After digestion by BsrGI and Bst1107 (A6297 and A7376), the fused amplification product was subcloned into the plasmid pSN3.9KpnI, which was generated by digestion by KpnI (A5972 and A8736) of pSN3.9 and by cloning the 3′ half of the provirus pSIVagm3mc into pGEM-7Zf(+) (Boehringer Ingelheim Bioproducts Partnership, Ingelheim, Germany). The chimeric KpnI (A5972 and A8736) fragment harboring the exchanged V3 loop was reinserted into pSN3.9, resulting in the 3′ half plasmid pSN3.9V3. An additional restriction site was inserted by cloning a linker oligonucleotide into the AatII site of pSN3.9V3 containing the HindIII restriction site [Linker(+), CCCGGAAGCTTCGCTAGGACGT; Linker(−), CCTAGCGAAGCTTCCGGGACGT). The resulting plasmid, as well as pSIVagm3mc, was digested with SacI (A5382) and HindIII. The chimeric 3′ half plasmid was ligated with the 5′ half plasmid of pSIVagm3mc to generate full-length viral DNA. The PCR-derived inserts were sequenced to ensure that only the intended changes were present.
Cells, virus stocks, and titration.
The human osteosarcoma cell line (HOS)-derived GHOST cell panel (provided by M. Dittmar, Heinrich-Pette-Institut, Hamburg, Germany) expressing one of the various coreceptors in addition to human CD4 and a Tat-dependent green fluorescent protein were cultivated as described previously (8). The human T-cell lines Molt4/8 and C8166 were maintained in RPMI 1640 medium containing 10% fetal calf serum. For the generation of virus stocks, Molt4.8 cells were transfected with 10 μg of the full-length proviral construct pSIVagm3mc or pSIVagm3-X4mc using a DMRIE-C (Gibco-BRL Invitrogen, Karlsruhe, Germany)-mediated transfection procedure. The virus was harvested after the induction of syncytia. Viral stocks were aliquoted and frozen at −80°C. To determine the 50% tissue culture infective doses (TCID50), the stocks were diluted in threefold steps using RPMI 1640 medium, and eight 50-μl aliquots of each sample were used for the titration of viruses infectious for C8166 T cells. Immunoperoxidase staining was performed to detect SIV antigen-expressing cells using sera from an SIVagm3mc-infected PT macaque as described previously (48). The titer was calculated using a Poisson distribution fitting model.
Infectivity assays.
For replication assays, PBMCs were isolated from SIV-seronegative AGM and PT macaques by Ficoll-Hypaque density gradient centrifugation and either infected immediately—i.e., nonstimulated—or incubated for 2 days in the presence of 10 μg of phytohemagglutinin (PHA) (Wellcome, Dartford, United Kingdom)/ml and 200 U of recombinant interleukin 2 (IL-2)/ml (Eurocetus, Frankfurt, Germany) before infection (multiplicity of infection [MOI] = 0.1). After overnight incubation, the cells were washed, and supernatants were removed regularly for titration in C1866 cells (see above). To assess coreceptor usage, GHOST cells were seeded in 48-well dishes and infected with virus at an MOI of 10 in a total volume of 0.2 ml of medium. After overnight incubation, the cells were washed and cultivated in 0.5 ml of fresh Dulbecco's modified Eagle's medium. Three days after infection, the supernatants were assayed for the detection of p27 core protein. The cells were washed and fixed in paraformaldehyde at a final concentration of 1% and then analyzed by a FACScan flow cytometer (Becton Dickinson, Heidelberg, Germany) for endogenous green fluorescent protein expression. Viral p27 was quantified by antigen capture enzyme-linked immunosorbent assay (ELISA) using standard protocols. Inactivated supernatants (0.2% Tween 20) were titrated on ELISA plates coated with monoclonal antibody (AG3.0) specific for SIVagm p27 (Jon Allen, Southwest Foundation, San Antonio, Texas). Captured protein was detected by using serum taken from a SIVagm3mc-infected PT macaque and in a second step by incubating the serum with goat anti-human immunoglobulin G-peroxidase conjugate (Sigma-Aldrich, Taufkirchen, Germany). Units of p27 were calculated by comparison with a standard curve generated by titration of a standard SIVagm supernatant. Low-level infection in all GHOST cells was due to the low level of endogenous expression of either CXCR4 or Bonzo (19).
Coreceptor inhibition assay.
To block the coreceptor CXCR4 for viral cell entry, the stromal-cell-derived factor 1α (SDF-1α) (R&D Systems, Wiesbaden, Germany) was added to C8166 T cells 2 h prior to infection. The final inhibitor concentrations used were 0.5, 2, and 5 μg of SDF-1α/ml, and the inhibitors were maintained at the same concentrations throughout the duration of the cultures. C8166 cells were cultured in 96-well plates at 2 × 105 per well and were infected at an MOI of 0.1 in duplicate. The culture supernatants (150 μl) were harvested at various time points for measurement of reverse transcriptase (RT). A commercial diagnostic kit (Lenti-RT Activity Assay; Cavidi Tech, Uppsala, Sweden) was used for the measurement of RT.
Animals, infections, and specimen collection.
All animal experiments were performed in accordance with paragraph 8 of the German Animal Protection Law in compliance with EC Directive 86/609, which makes it an offense to carry out any scientific procedure on an animal except under license. SIV-negative PT macaques were injected intravenously with 106 TCID50 of the respective virus stocks. Plasma and PBMCs from heparinized blood were separated immediately by Ficoll-Hypaque density centrifugation. A portion of the PBMCs were used for the limiting-dilution coculture assay, for virus reisolation, and for analysis by FACScan. The rest were stored at −80°C as 5 × 105-cell pellets for subsequent PCR studies. Plasma was clarified of cells by centrifugation, and 200-μl aliquots were frozen at −80°C until they were used for the quantitative RT-PCR (qRT-PCR) assay. Serum was also clarified of cells by centrifugation and stored at −20°C. EDTA blood samples were used for analysis of absolute numbers of leukocytes per microliter of blood using a hematology analyzer (Coulter [Krefeld, Germany] Counter JT).
Fluorescence-activated cell sorter (FACS) analysis.
Lymphocyte subsets from PT macaques and AGM were analyzed by FACScan (Becton Dickinson, Heidelberg, Germany). Ten microliters of each of the monoclonal antibodies Leu3a-phycoerythrin (PE) (CD4) (Becton Dickinson), Leu2a-fluorescein isothiocyanate (CD8) (Becton Dickinson), 12G5-PE (CXCR4) (Becton Dickinson), FN50-fluorescein isothiocyanate (CD69) (Becton Dickinson), and 2A3-PE (CD25) (Becton Dickinson) was incubated with 2 × 105 PBMCs in phosphate-buffered saline (PBS)-0.1% sodium azide for 20 min in the dark on ice. Following staining, the PBMCs were washed with PBS-0.1% NaN3-10% fetal calf serum and fixed with 1% paraformaldehyde.
Virus reisolation and measurement of cell-associated virus load.
For virus reisolation, PBMCs were cocultivated with 5 × 106 C8166 T cells for 28 days and monitored for the presence of SIVagm replication by RT assay using a commercial test kit (Boehringer Mannheim, Mannheim, Germany). Virus stocks were collected and titrated to determine the TCID50. The cell-associated virus load was determined by limiting-dilution coculture. Fivefold dilutions of PBMCs, starting with 106 PBMCs, were cocultivated with 106 C8166 T cells in triplicate in 24-well plates. After 21 days, the cells were tested for infection by immunoperoxidase staining. The number of infected cells/106 PBMCs was then calculated with a Poisson distribution fitting model.
Measurement of plasma virus load and proviral load.
Viral RNA was quantified using a real-time qRT-PCR assay monitored in real time using the Prism 7700 detector (PE Applied Biosystems, Foster City, Calif.) as described previously (26). Briefly, RNA was isolated using the High Pure Viral RNA kit (Roche Molecular Biochemicals, Mannheim, Germany) eluting in 50 μl of RNase-free water. The primers SIVagmf (CAG ATG CTC GCT GGC TTG TA) and SIVagmr (GCC ACC CAG GTT AGG CTA ACC) were specific for the LTR of SIVagm3mc. The fluorogenic probe SIVagmp (6-carboxyfluorescein [FAM]-AAC ACC CAG GCT CAA GCT GGT CTC CTA GT-TAMRA [6-carboxytetramethylrhodamine]) hybridizes to a region 6 bp 5′of SIVagmf. PCRs were performed in MicroAmp Optical 96-well plates (PE Applied Biosystems), and the products were subjected to one-step RT-PCR cycling. Samples were tested in triplicate, and the number of RNA copies was determined by comparison with a standard curve obtained using known amounts of SIVagm RNA.
Proviral DNA was also quantified by real-time PCR as described previously (26). DNA was isolated using the QIAamp DNA Blood Mini Kit (Qiagen, Hilden, Germany). The same primers and fluorogenic probe described above were used. Samples were tested in triplicate, and the number of DNA copies was determined by comparison with a standard curve obtained using known amounts of DNA.
ELISA.
Whole inactivated SIVagm3 dissolved in water was dried (overnight; 37°C) on flexible ELISA plates at a predetermined optimal concentration. The ELISA was then performed using a standard protocol with titrated sera as described previously (4). Briefly, the coated plates were washed with washing buffer (0.05% Tween 20-0.01% NaN3 in PBS) and incubated with blocking buffer (2% milk powder in PBS) followed by the addition of titrated sera diluted in blocking buffer plus 0.05% Tween 20. After incubation for 1 h at 37°C, the plates were washed and incubated with goat anti-human immunoglobulin G-peroxidase conjugate (Sigma, Deisenhofen, Germany) diluted 1:1,000. Finally, the plates were washed and incubated with substrate buffer (1 ml of o-phenylendediamine per ml of PBS [pH 6] plus 0.025% H2O2), after which the reaction was stopped with 1 M H2SO4 and the optical density at 492 nm was measured.
Measurement of neutralizing antibodies.
Twenty-five microliters (each) of different dilutions of heat-inactivated sera was incubated (four replicates per dilution) with 25 μl of the respective virus with a titer of 2 × 103 TCID50. After 60 min of incubation at 37°C, 150 μl of medium containing 2 × 103 C8166 T cells was added to each well of a microtiter plate. The plates were incubated for 7 days at 37°C. A well was scored positive for the presence of SIVagm (negative for neutralization) when p27 core protein was detected in the supernatant as described above. Titers were expressed as the 50% neutralizing dosage (ND50) by analyzing the number of wells showing complete neutralization using the method of Spearman and Kärber.
Nucleotide sequence analysis.
Twenty-six weeks after inoculation, sequence analyses were performed to verify the sequence of the V3 loop. DNA was isolated from PBMCs of the infected PT macaques using the QIAamp DNA Blood Mini Kit, and a V3 loop-specific PCR was performed using the primers A6646(+) (CCCAGATATGGCAGAAACATAGAG) and A7079(−) (CTTCGTACCATTACACGGATTATGG). The amplified fragments were cloned into the TOPO-TA cloning vector (Invitrogen, Leek, The Netherlands), and several clones from each reaction were completely sequenced.
RESULTS
Generation of infectious CXCR4-tropic SIVagm3-X4mc by exchanging the V3 loop in gp130-SU of SIVagm3mc for that of HIV-1 BH10.
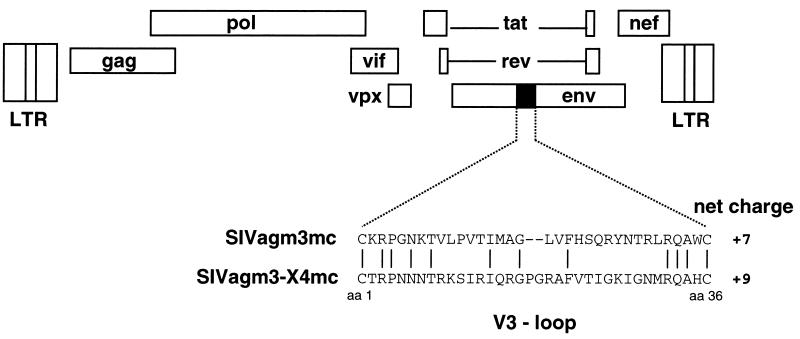
A 34-amino-acid peptide in gp130-SU of SIVagm3mc was putatively assigned as the V3 loop based on its sequence homology with the V3 loop of HIV-1 as well as the presence of two flanking cysteines (39, 49). It was assumed that the exact exchange of the SIVagm3mc V3 loop for that of HIV-1 BH10 would result in the generation of infectious virus able to use CD4 and CXCR4 for cell entry. This would imply that both V3 loops were generally equivalent in structure and function. Plasmid pSIVagm3-X4mc (Fig. 1), constructed as described in Materials and Methods, comprised a full-length viral genome flanked by two LTRs. The plasmid harbored the V3 loop of HIV-1 BH10 from nucleotides 6465 to 6572 in place of the assigned V3 loop of the parental virus, SIVagm3mc, from nucleotides 6726 to 6827. The V3 loop insertion was verified by sequencing. The transfection of pSIVagm3-X4 into human Molt4.8 T cells and the subsequent transfer of the supernatant onto C8166 T cells resulted in production of infectious virus particles with maximum titers of 8.9 × 106 TCID50 (data not shown).
FIG. 1.
Viral genome structure of SIVagm3-X4mc. The viral genome structure of SIVagm3mc, which is identical to that of SIVagm3-X4mc, is shown as open boxes. The solid box represents the V3 loop of gp130-SU. Aligned below are the sequences of the SIVagm3mc V3 loop and of the HIV-1 BH10 V3 loop, which replaces the V3 loop of SIVagm3mc in variant SIVagm3-X4mc. The vertical lines connect those amino acids which are identical in SIVagm3mc and SIVagm3-X4mc. The net charges of both V3 loop sequences are indicated.
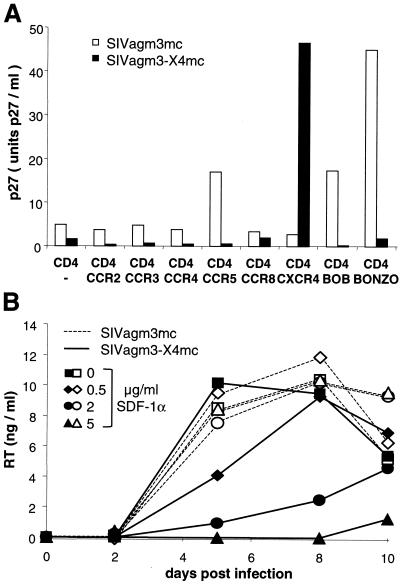
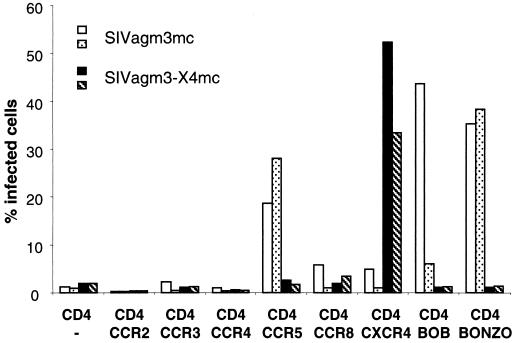
To study the coreceptor utilization of SIVagm3-X4mc in comparison to that of the parental SIVagm3mc, various GHOST cell lines were infected with identical TCID50 of the respective virus variants. The GHOST cell lines expressed either CD4 alone or CD4 in conjunction with one of several chemokine coreceptors (Fig. 2A). The level of infection was measured by detection of p27-Gag in the supernatant of infected cells and/or by FACS analysis detecting HIV-2 LTR-driven endogenous gfp expression. As shown in Fig. 2A, SIVagm3mc infected predominantly the CD4-positive GHOST cells expressing the coreceptor CCR5, Bob, or Bonzo. In contrast, SIVagm3-X4mc infected only the CD4- and CXCR4-positive GHOST cells. To confirm this result, replication studies were performed in C8166 cells in the absence or presence of human SDF-1, the natural ligand of CXCR4. As shown in Fig. 2B, the replication of SIVagm3mc was not affected by increasing doses of SDF-1 (0.5 to 5 μg/ml). In contrast, the replication of SIVagm3-X4mc was inhibited by SDF-1 in a dose-dependent manner, as expected for a CD4- and CXCR4-using lentivirus. These results indicated that the coreceptor utilization of SIVagm3mc was successfully altered from CCR5, Bob, or Bonzo to CXCR4 by a V3 loop exchange, resulting in infectious SIVagm3-X4mc.
FIG. 2.
Coreceptor usage of SIVagm3-X4mc and SIVagm3mc. (A) GHOST cells expressing CD4 alone or in conjunction with one of various coreceptors as indicated were infected at an MOI of 10 with SIVagm3-X4mc or SIVagm3mc. p27 antigen was quantified in the cell culture supernatants 3 days later as described in Materials and Methods. p27 levels below 5 U/ml were counted as negative and assumed to result from low-level infections due to a low level of endogenous CXCR4 or Bonzo expression in all GHOST cells used (19). Similar results were obtained in two independent experiments, and the results from one representative experiment are shown. (B) Inhibition of SIVagm3-X4mc replication in the presence of SDF-1α. C8166 cells were infected at an MOI of 0.1 with either SIVagm3mc or SIVagm3-X4mc. The cells were maintained in the absence or in the presence of various concentrations of SDF-1α. Replication was followed by RT assays at various times after infection as indicated.
In vitro replication of SIVagm3-X4mc in IL-2-PHA-activated and nonstimulated PBMCs from PT macaques and AGM.
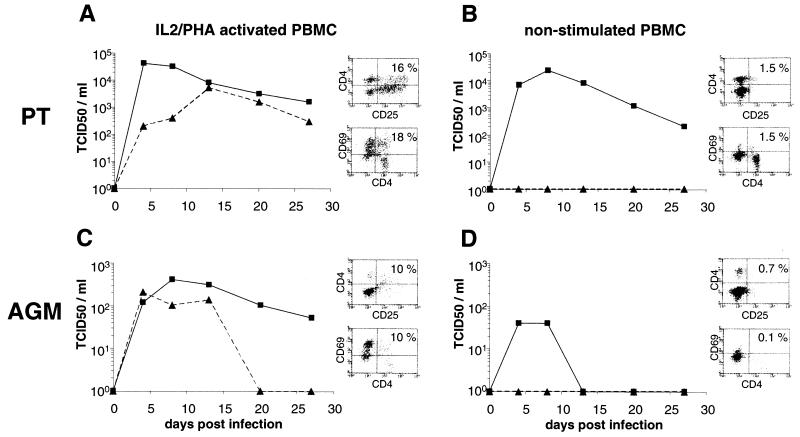
The in vitro replication properties of SIVagm3-X4mc were compared with those of the parental SIVagm3mc in PBMCs from PT macaques or AGM. The presence of cells permissive for SIVagm3-X4mc replication was verified by measuring CD4 and CXCR4 expression; 91 to 95% of the CD4-positive T lymphocytes from AGM and PT macaques, respectively, expressed the coreceptor CXCR4 (data not shown). PBMCs were infected at an MOI of 0.1, and the TCID50 in the supernatants were determined by titration in C8166 T cells. As shown in Fig. 3A and C, SIVagm3-X4mc replicated in IL-2-PHA-stimulated PT macaque and AGM PBMCs to maximum titers similar to those of SIVagm3mc. The maximum titers of SIVagm3mc were slightly lower than those of SIVagm3-X4mc. In accordance with previous results (16), SIVagm3mc did not replicate in nonstimulated PBMCs (Fig. 3B and D). Surprisingly, SIVagm3-X4mc was able to replicate in nonstimulated PT macaque and AGM PBMCs (Fig. 3B and D) to levels similar to those observed in the respective IL-2-PHA-stimulated PBMCs. Using FACS analysis, the stimulation status of the PBMCs was measured immediately prior to infection by monitoring the percentage of CD69-positive and CD25-positive cells; 16 and 18% of the stimulated PT macaque lymphocytes were CD4-CD25 positive and CD4-CD69 positive, respectively, and 10% of the stimulated AGM lymphocytes were CD4-CD25 positive and CD4-CD69 positive. In contrast, 1.5% of the nonstimulated PT macaque lymphocytes were CD4-CD25 positive or CD4-CD69 positive, and nonstimulated AGM lymphocytes contained 0.7% CD4-CD25-positive and 0.1% CD4-CD69-positive cells. In summary, SIVagm3-X4mc replicated in stimulated as well as in nonstimulated AGM and PT macaque PBMCs.
FIG. 3.
In vitro replication of SIVagm3mc and SIVagm3-X4mc. PBMCs from PT macaques (A and B) and AGM (C and D) were infected at an MOI of 0.1 with SIVagm3mc (▴) and SIVagm3-X4mc (▪). Replication was followed in IL-2-PHA-stimulated PBMCs (A and C) or nonstimulated PBMCs (B and D) by measuring the TCID50 in C8166 T cells at various time points after infection as indicated. The stimulation status of the cells was monitored by FACS analysis using a double stain for CD4-CD69 or CD4-CD25 on the day of infection. The FACS diagrams show the percentages of double-positive PBMCs (upper right boxes) for each infection.
Absence of pathogenicity in PT macaques chronically infected with SIVagm3-X4mc.
To evaluate the in vivo replication of SIVagm3-X4mc, two PT macaques (PT236 and PT6502) were infected with 106 TCID50 of SIVagm3-X4mc. As a control, two PT macaques (PT232 and PT7337) were infected with 106 TCID50 of the parental virus, SIVagm3mc. An initial decline in the number of peripheral blood CD4-positive and CD8-positive lymphocytes was observed in the peripheral blood of both SIVagm3mc- and SIVagm3-X4mc-infected PT macaques. However, the absolute numbers of peripheral CD4-positive lymphocytes (2 × 103, 1.5 × 103, 1.9 × 103 to 3.6 × 103, and 0.6 × 103 to 1.2 × 103 lymphocytes/μl of blood for PT macaques PT232, PT7337, PT236, and PT6502, respectively) and CD8-positive lymphocytes (2.5 × 103, 1.5 × 103, 1.2 × 103 to 3.9 × 103, and 0.8 × 103 to 2.1 × 103 for PT macaques PT232, PT7337, PT236, and PT6502, respectively) returned to normal levels after 2 to 4 weeks of infection (data not shown). During 14 months of observation, none of the SIVagm3mc- or SIVagm3-X4mc-infected PT macaques showed any clinical signs of disease.
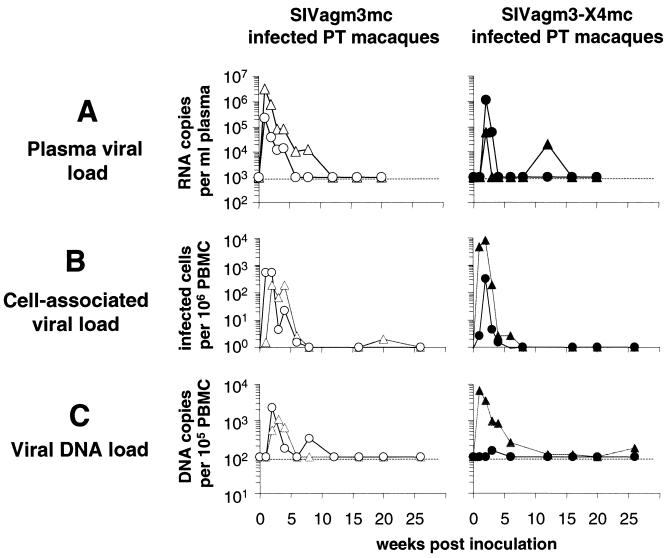
To characterize the infection kinetics in vivo, the viral loads (RNA in plasma or viral DNA in cells) and the number of productively infected cells were measured. The courses of the plasma viral load development as determined by real-time PCR are shown in Fig. 4A. The initial plasma viral load became detectable at week 1 in SIVagm3mc-infected PT macaques and at week 2 in the SIVagm3-X4mc-infected animals. Peak levels ranged from 6 × 104 to 3 × 106 RNA copies/ml of plasma, followed by a decrease to below the detection limit of 103 RNA copies/ml of plasma. The number of productively infected cells, as measured by coculture with C8166 T cells, similarly showed an early peak (191 to 8,173 infected cells/106 PBMCs) (Fig. 4B). As shown in Fig. 4C, the number of PBMCs carrying viral DNA as measured by real-time PCR also followed a pattern similar to that of the plasma viral load by peaking at 1 to 3 weeks postinfection and dropping below the detection limit of 102 DNA copies/105 PBMCs by weeks 6 to 12 and thereafter. Peak values ranged from 146 to 6,661 viral DNA copies/105 PBMCs. To summarize, an initial peak of viremia was observed in SIVagm3mc- and SIVagm3-X4mc-infected PT macaques, followed by the establishment of chronic infections. Astonishingly, no significant differences between the infection profiles of SIVagm3mc- and SIVagm3-X4mc-infected PT macaques were observed.
FIG. 4.
Viral loads during the course of infection of PT macaques with SIVagm3-X4mc (PT236 [▴]; PT6502 [•]) or SIVagm3mc (PT232 [▵]; PT7337 [○]). (A) Plasma viral loads in PT macaques were measured as the number of RNA copies per milliliter of plasma (real-time quantitative RT-PCR) for a period of 20 weeks following the inoculation of virus. The detection limit of the assay was 102 RNA copies/ml of plasma (dashed lines). (B) Cell-associated viral loads in the peripheral blood of infected PT macaques were measured as the number of productively infected cells/106 PBMCs. Ficoll gradient-purified PT macaque PBMCs were diluted to various extents and cocultured with C8166 T cells. Data were obtained for a period of 26 weeks postinoculation. (C) Viral DNA loads in infected PT macaques were measured as the number of DNA copies/105 PBMCs (real-time quantitative PCR) for a period of 26 weeks postinoculation. The detection limit was 102 DNA copies per 105 PBMCs (dashed lines).
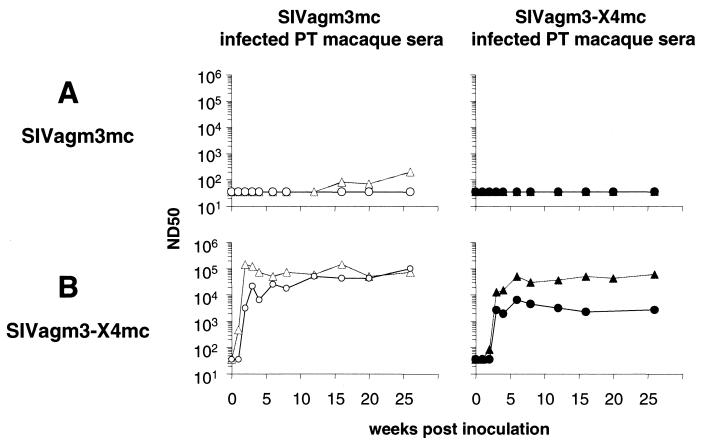
Exquisite sensitivity of SIVagm3-X4mc to neutralizing antibodies.
In order to examine the humoral immune response in the infected PT macaques, binding and neutralizing antibodies were measured. Three of the four infected PT macaques seroconverted at week 3 and maintained a sustained SIVagm-specific antibody response for 26 weeks as measured by SIVagm-specific ELISA. One of the SIVagm3-X4mc-infected PT macaques (PT6502) seroconverted later and maintained a very low level of antibodies (data not shown). Neutralizing antibodies against SIVagm3mc or SIVagm3-X4mc were measured using C8166 T cells. No neutralization activity (ND50) against SIVagm3mc was detected in the sera of PT macaques PT7337, PT236, and PT6502, and a very small increase in neutralizing antibodies was detected in the serum of PT macaque PT232 (Fig. 5A). In contrast, high neutralization activity, above 103 ND50, was detected against SIVagm3-X4mc in the sera of both SIVagm3mc- and SIVagm3-X4mc-infected PT macaques (Fig. 5B). The neutralizing titers measured reached a plateau after 2 to 3 weeks of infection and remained stable over 26 weeks. The peak values were 1.4 × 105 ND50 in serum from PT macaque PT232, 1 × 105 ND50 in serum from PT7337, and 6 × 104 ND50 in PT236 serum to 6.4 × 103 ND50 in PT6502 serum, indicating high titers of SIVagm3-X4mc neutralizing antibodies. This demonstrated that infection of cells with SIVagm3-X4mc in vitro is highly sensitive to neutralizing antibodies present in sera from PT macaques infected by SIVagm3-X4mc or SIVagm3mc. It also revealed that high levels of neutralizing antibodies are induced by both SIVagm3 variants.
FIG. 5.
Detection of neutralizing antibodies in sera from SIVagm3mc- and SIVagm3-X4mc-infected PT macaques against SIVagm3-X4mc or SIVagm3mc. The neutralization of SIVagm3mc (A) and SIVagm3-X4mc (B) infections by sera of PT macaques infected with SIVagm3mc (PT232 [▵]; PT7337 [○]) and with SIVagm3-X4mc (PT236 [▴]; PT6502 [•]) is shown. Neutralizing activity was measured in C8166 T cells as described in Materials and Methods. The titers are the reciprocal serum dilutions at which 50% of the cells were protected from virus infection (ND50). ND50 values below the detection limit were arbitrarily assigned the value of 35.
Conserved coreceptor usage of SIVagm3mc and SIVagm3-X4mc during in vivo replication.
To evaluate a potential change in coreceptor usage during in vivo replication, virus was isolated by cocultivating PBMCs from the infected PT macaques with C8166 T cells. The coreceptor usage of isolated virus was tested by infecting various CD4-positive GHOST cells. As shown in Fig. 6, isolates obtained 1 and 3 weeks postinfection from SIVagm3mc- or SIVagm3-X4mc-infected PT macaques used CCR5, Bob, and Bonzo or CXCR4 as coreceptors, respectively. Thus, the coreceptor usage of each of the virus variants used for infection was maintained in vivo. To monitor potential V3 loop sequence changes, we performed a sequence analysis at 26 weeks postinfection, i.e., at the end of the observation period. DNA was purified from PMBCs of SIVagm3mc- or SIVagm3-X4mc-infected PT macaques and used to amplify the V3 loop-encoding viral genome regions. All 11 sequences derived from both SIVagm3mc-infected PT macaques, all 11 sequences derived from PT macaque PT236 infected with SIVagm3-X4mc, and 10 out of 11 sequences derived from PT macaque PT6502 infected with SIVagm3-X4mc showed the original V3 loop sequence of the respective virus construct used for infection (data not shown). In only 1 out of 11 sequences cloned from PBMC DNA of PT macaque PT6502, a single amino acid substitution, namely G→R at amino acid position 29 of the V3 loop, was observed. This sequence change altered the net charge of the SIVagm3-X4mc V3 loop from +9 to +10 (data not shown), suggesting that the respective V3 loop would also allow the usage of CXCR4, as V3 loops known to mediate CXCR4 usage generally have a positive charge. These data show that the coreceptor usage of SIVagm3mc and SIVagm3-X4mc is maintained during in vivo replication.
FIG. 6.
Coreceptor utilization of SIVagm3mc and SIVagm3-X4mc isolated from infected PT macaques. The coreceptor utilization of virus isolates obtained from PT macaques infected with SIVagm3mc or SIVagm3-X4mc was analyzed using GHOST cells. Isolates were obtained by cocultivation of PBMCs from infected PT macaques with C8166 T cells. Infected GHOST cells were analyzed by FACS as described in Materials and Methods. One isolate (open bars) from PT macaque PT7337 infected with SIVagm3mc was obtained 1 week postinoculation. The following three isolates were obtained 3 weeks postinoculation: PT232 infected with SIVagm3mc (stippled bar) and PT236 (solid bar) and PT6502 (hatched bar) infected with SIVagm3-X4mc.
DISCUSSION
The putative V3 loop of SIVagm3mc was replaced by that of the CXCR4-tropic HIV-1 strain BH10, resulting in the replicating variant SIVagm3-X4mc, which is able to use CD4 in conjunction with CXCR4 for cell entry. Previously, V3 loops had been exchanged only between different strains of HIV-1 (46) or between HIV-1 and HIV-2 (36). However, a replacement of the V3 loop in SIVmac by that of HIV-1 did not result in replication-competent viruses (32). Moreover, an increase in the net charge of the amino acids located in the V3 loop of SIVmac by amino acid substitutions did not allow efficient utilization of CXCR4 (38). The results described here indicate that a functional exchange of the V3 loop is possible between SIVagm and HIV-1, two phylogenetically distant primate lentiviruses. The V3 loop switch resulted in a change of coreceptor usage from CCR5, Bob, and Bonzo (SIVagm3mc) to CXCR4 (SIVagm3-X4mc). Coreceptors other than CXCR4 were no longer used by SIVagm3-X4mc. This suggests that the putative V3 region of SIVagm, which corresponds to the sequence of the V3 loop of HIV-1, is a determinant of SIVagm coreceptor usage.
Recently, Owen et al. (40) reported that one primary SIVagm isolate obtained from an AGM utilized CXCR4 as a coreceptor for cell entry. In contrast to HIV-2 strains, this SIVagm isolate replicated only to a small extent in CD4- and CXCR4-expressing cells but to normal levels in CD4- and CCR5-expressing cells (40). Generally, however, CXCR4 has not been found to be used as coreceptor for laboratory-adapted SIVagm strains in a number of previous studies. For example, the coreceptor preferentially used by the pathogenic cloned variant SIVagm9063-2 was CCR5 (20). In addition, the coreceptor specificities of two apathogenic clones of SIVagm tested so far, namely, SIVagmSab1.4 and SIVagmTYO, revealed a preference for CCR5, Bob, and Bonzo (15, 19). In agreement with these observations, SIVagm isolates derived from a long-term naturally infected AGM also used the coreceptor CCR5 and showed no switch in coreceptor usage to CXCR4 (R. R. König and K. Cichutek, unpublished observation). This is also consistent with reports that variants of SIVmne from PT macaques, which evolve during the course of disease progression in vivo, recognize CCR5 and Bob but not CXCR4 (30). This shows that CXCR4 coreceptor use of SIVagm and SIVmne in PT macaques is very unusual in wild-type strains, supporting the reasoning underlying the assessment of the properties of an engineered CD4- and CXCR4-tropic SIVagm variant such as SIVagm3-X4mc, as reported here. Remarkably, the CXCR4 coreceptor usage of SIVagm3-X4mc remained constant during 26 weeks postinfection of two PT macaques based upon tested virus isolates 3 weeks postinoculation and sequence analysis of the V3 loop 26 weeks postinfection. Although second-site mutations outside the V3 loop could have occurred, it is not very likely that they would alter the coreceptor specifity. Analyses of HIV-1 Env chimeras containing the V3 loop of an SIVmac/HIV-1 hybrid virus indicate that the V3 loop is the major determinant of CXCR4 specificity (25). Moreover, it has been previously shown that the HIV-2 V3 loop determines the coreceptor usage of CCR5 and CXCR4 (28). Our results indicate that in vivo usage of CXCR4 in PT macaque lymphocytes is possible for an extended period of time.
As expected, SIVagm3-X4mc was able to replicate in IL-2-PHA-stimulated PBMCs from AGM and from PT macaques in vitro. Surprisingly, and in contrast to SIVagm3mc, SIVagm3-X4mc was also able to replicate in nonstimulated PBMCs, a property usually associated with the acutely pathogenic and enteropathic SIVsmm-Pbj from sooty mangabeys (21). As SIVagm3-X4mc differs from the parental SIVagm3mc only in the V3 loop, this may suggest that the SIVagm3-X4mc V3 loop triggers an intracellular signal which enables virus replication. Chemokine receptor signaling events were previously shown to play a role in postentry events necessary for further viral replication (9). Along this line, activation of signaling pathways triggered through chemokine receptors (34, 43) may modulate the activation status of cells and, as a consequence, promote replication of SIVagm3-X4mc.
As shown here, the kinetics of virus replication were not significantly different in four PT macaques infected by SIVagm3mc or SIVagm3-X4mc. SIVagm3mc showed a replication profile in the two PT macaques similar to that in AGM, as reported previously (4). The viral DNA load in the PT macaques decreased after a few weeks from a maximum of 104 viral DNA copies/105 PBMCs to below the detection limit of the PCR assay used (102 viral DNA copies/105 PBMCs). AGM experimentally infected with SIVagm3mc revealed low viral loads of 2.1 to 5.1 copies/105 PBMCs (5), in agreement with the observations reported here. The viral loads of SIVagm3mc and SIVagm3-X4mc are therefore low, albeit comparable with those found in many asymptomatic HIV-1-infected patients (23).
The change of coreceptor usage from CCR5, Bob, and Bonzo in SIVagm3mc to CXCR4 in SIVagm3-X4mc did not change the apathogenic nature of the virus, at least in the time frame of the study. SIVagm3-X4mc remained apathogenic, despite the high percentage of permissive CD4- and CXCR4-positive PT macaque lymphocytes available for in vivo replication. A higher percentage of CD4-positive human lymphocytes was found to express CXCR4 rather than CCR5 (33). In addition, CCR5 expression is primarily limited to human memory T cells (CD45RO+), and the CXCR4 receptor was found only on naive human T cells (CD45RO−) (7). This shift of the target cell population to different lymphocyte subsets could have been expected to have an influence on disease progression. Although it is assured that SIVagm3-X4mc uses target cells different from those used by SIVagm3mc, our findings suggest that differential coreceptor utilization of SIVagm does not alter viral pathogenesis.
An unexpected finding was the exquisite sensitivity of SIVagm3-X4mc to neutralizing antibodies. It is possible that the alteration of the V3 loop sequence led to exposure of the V3 loop and adjacent regions containing epitopes accessible to neutralizing antibodies. Previously, Hoffman et al. (24) showed that the Env protein of a CXCR4-using and CD4-independent variant of HIV-1 and -IIIB exists in a partially activated state in which the coreceptor binding site is exposed and functional. This exposure also resulted in an increased sensitivity to neutralizing antibodies. In addition, the relative resistance to neutralization of primary isolates compared with T-cell line-adapted (TCLA) strains of HIV-1 is likely to be based on the conformation of gp120-SU. The CD4 binding site of gp120-SU of primary isolates is thought to be more completely masked by the V1 and V2 loops than that of TCLA viruses. Thus, the TCLA strain-derived gp120-SU may be biased toward an “open” state. Consequently, the V3 loop may be more exposed (41). We therefore propose that the introduction of the HIV-1 V3 loop in gp130-SU of SIVagm leads to a conformational change in gp130-SU and exposure of epitopes recognized by neutralizing antibodies. As our data show, these antibodies are induced by SIVagm3mc as well as by SIVagm3-X4mc, but only SIVagm3-X4mc allows their detection in neutralization assays.
Acknowledgments
We thank N. Norley, J. Seidl, M. Schütze, S. Raupp, R. Wenig, and D. Bauer for excellent technical assistance; M. Selbert for expert automatic sequencing; and M. Engelstädter, J. Stitz, and M. Bobkova for constructive discussions.
This work was supported by grant 10/9-2 from the DFG.
REFERENCES
- 1.Albert, J., P. Stalhandske, S. Marquina, J. Karis, R. A. Fouchier, E. Norrby, and F. Chiodi. 1996. Biological phenotype of HIV type 2 isolates correlates with V3 genotype. AIDS Res. Hum. Retrovir. 12:821-828. [DOI] [PubMed] [Google Scholar]
- 2.Baier, M., C. Garber, C. Muller, K. Cichutek, and R. Kurth. 1990. Complete nucleotide sequence of a simian immunodeficiency virus from African green monkeys: a novel type of intragroup divergence. Virology 176:216-221. [DOI] [PubMed] [Google Scholar]
- 3.Baier, M., A. Werner, K. Cichutek, C. Garber, C. Muller, G. Kraus, F. J. Ferdinand, S. Hartung, T. S. Papas, and R. Kurth. 1989. Molecularly cloned simian immunodeficiency virus SIVagm3 is highly divergent from other SIVagm isolates and is biologically active in vitro and in vivo. J. Virol. 63:5119-5123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Beer, B., M. Baier, J. zur Megede, S. Norley, and R. Kurth. 1997. Vaccine effect using a live attenuated nef-deficient simian immunodeficiency virus of African green monkeys in the absence of detectable vaccine virus replication in vivo. Proc. Natl. Acad. Sci. USA 94:4062-4067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Beer, B., J. Scherer, J. zur Megede, S. Norley, M. Baier, and R. Kurth. 1996. Lack of dichotomy between virus load of peripheral blood and lymph nodes during long-term simian immunodeficiency virus infection of African green monkeys. Virology 219:367-375. [DOI] [PubMed] [Google Scholar]
- 6.Berger, E. A., P. M. Murphy, and J. M. Farber. 1999. Chemokine receptors as HIV-1 coreceptors: roles in viral entry, tropism, and disease. Annu. Rev. Immunol. 17:657-700. [DOI] [PubMed] [Google Scholar]
- 7.Bleul, C. C., L. Wu, J. A. Hoxie, T. A. Springer, and C. R. Mackay. 1997. The HIV coreceptors CXCR4 and CCR5 are differentially expressed and regulated on human T lymphocytes. Proc. Natl. Acad. Sci. USA 94:1925-1930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cecilia, D., V. N. KewalRamani, J. O'Leary, B. Volsky, P. Nyambi, S. Burda, S. Xu, D. R. Littman, and S. Zolla-Pazner. 1998. Neutralization profiles of primary human immunodeficiency virus type 1 isolates in the context of coreceptor usage. J. Virol. 72:6988-6996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Chackerian, B., E. M. Long, P. A. Luciw, and J. Overbaugh. 1997. Human immunodeficiency virus type 1 coreceptors participate in postentry stages in the virus replication cycle and function in simian immunodeficiency virus infection. J. Virol. 71:3932-3939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Chen, Z., A. Gettie, D. D. Ho, and P. A. Marx. 1998. Primary SIVsm isolates use the CCR5 coreceptor from sooty mangabeys naturally infected in west Africa: a comparison of coreceptor usage of primary SIVsm, HIV-2, and SIVmac. Virology 246:113-124. [DOI] [PubMed] [Google Scholar]
- 11.Chen, Z., P. Zhou, D. D. Ho, N. R. Landau, and P. A. Marx. 1997. Genetically divergent strains of simian immunodeficiency virus use CCR5 as a coreceptor for entry. J. Virol. 71:2705-2714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cichutek, K., and S. Norley. 1993. Lack of immune suppression in SIV-infected natural hosts. AIDS 7(Suppl. 1):S25-S35. [PubMed] [Google Scholar]
- 13.Cocchi, F., A. L. DeVico, A. Garzino-Demo, A. Cara, R. C. Gallo, and P. Lusso. 1996. The V3 domain of the HIV-1 gp120 envelope glycoprotein is critical for chemokine-mediated blockade of infection. Nat. Med. 2:1244-1247. [DOI] [PubMed] [Google Scholar]
- 14.Connor, R. I., K. E. Sheridan, D. Ceradini, S. Choe, and N. R. Landau. 1997. Change in coreceptor use correlates with disease progression in HIV-1-infected individuals. J. Exp. Med. 185:621-628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Deng, H. K., D. Unutmaz, V. N. KewalRamani, and D. R. Littman. 1997. Expression cloning of new receptors used by simian and human immunodeficiency viruses. Nature 388:296-300. [DOI] [PubMed] [Google Scholar]
- 16.Dittmar, M. T., K. Cichutek, P. N. Fultz, and R. Kurth. 1995. The U3 promoter region of the acutely lethal simian immunodeficiency virus clone smmPBj1.9 confers related biological activity on the apathogenic clone agm3mc. Proc. Natl. Acad. Sci. USA 92:1362-1366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Dumonceaux, J., C. Chanel, S. Valente, L. Quivet, P. Briand, and U. Hazan. 1999. Mutations in the env gene of human immunodeficiency virus type 1 NDK isolates and the use of African green monkey CXCR4 as a co-receptor in COS-7 cells. J. Gen. Virol. 80:1975-1982. [DOI] [PubMed] [Google Scholar]
- 18.Edinger, A. L., J. E. Clements, and R. W. Doms. 1999. Chemokine and orphan receptors in HIV-2 and SIV tropism and pathogenesis. Virology 260:211-221. [DOI] [PubMed] [Google Scholar]
- 19.Edinger, A. L., T. L. Hoffman, M. Sharron, B. Lee, B. O'Dowd, and R. W. Doms. 1998. Use of GPR1, GPR15, and STRL33 as coreceptors by diverse human immunodeficiency virus type 1 and simian immunodeficiency virus envelope proteins. Virology 249:367-378. [DOI] [PubMed] [Google Scholar]
- 20.Edinger, A. L., J. L. Mankowski, B. J. Doranz, B. J. Margulies, B. Lee, J. Rucker, M. Sharron, T. L. Hoffman, J. F. Berson, M. C. Zink, V. M. Hirsch, J. E. Clements, and R. W. Doms. 1997. CD4-independent, CCR5-dependent infection of brain capillary endothelial cells by a neurovirulent simian immunodeficiency virus strain. Proc. Natl. Acad. Sci. USA 94:14742-14747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Fultz, P. N., D. C. Anderson, H. M. McClure, S. Dewhurst, and J. I. Mullins. 1990. SIVsmm infection of macaque and mangabey monkeys: correlation between in vivo and in vitro properties of different isolates. Dev. Biol. Stand. 72:253-258. [PubMed] [Google Scholar]
- 22.Harouse, J. M., A. Gettie, R. C. Tan, J. Blanchard, and C. Cheng-Mayer. 1999. Distinct pathogenic sequela in rhesus macaques infected with CCR5 or CXCR4 utilizing SHIVs. Science 284:816-819. [DOI] [PubMed] [Google Scholar]
- 23.Ho, D. D., T. Moudgil, and M. Alam. 1989. Quantitation of human immunodeficiency virus type 1 in the blood of infected persons. N. Engl. J. Med. 321:1621-1625. [DOI] [PubMed] [Google Scholar]
- 24.Hoffman, T. L., C. C. LaBranche, W. Zhang, G. Canziani, J. Robinson, I. Chaiken, J. A. Hoxie, and R. W. Doms. 1999. Stable exposure of the coreceptor-binding site in a CD4-independent HIV-1 envelope protein. Proc. Natl. Acad. Sci. USA 96:6359-6364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hoffman, T. L., E. B. Stephens, O. Narayan, and R. W. Doms. 1998. HIV type I envelope determinants for use of the CCR2b, CCR3, STRL33, and APJ coreceptors. Proc. Natl. Acad. Sci. USA 95:11360-11365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Holzammer, S., E. Holznagel, A. Kaul, R. Kurth, and S. Norley. 2001. High virus loads in naturally and experimentally SIVagm-infected African green monkeys. Virology 283:324-331. [DOI] [PubMed] [Google Scholar]
- 27.Horton, R. M., H. D. Hunt, S. N. Ho, J. K. Pullen, and L. R. Pease. 1989. Engineering hybrid genes without the use of restriction enzymes: gene splicing by overlap extension. Gene 77:61-68. [DOI] [PubMed] [Google Scholar]
- 28.Isaka, Y., A. Sato, S. Miki, S. Kawauchi, H. Sakaida, T. Hori, T. Uchiyama, A. Adachi, M. Hayami, T. Fujiwara, and O. Yoshie. 1999. Small amino acid changes in the V3 loop of human immunodeficiency virus type 2 determines the coreceptor usage for CXCR4 and CCR5. Virology 264:237-243. [DOI] [PubMed] [Google Scholar]
- 29.Kanki, P. J., J. Alroy, and M. Essex. 1985. Isolation of T-lymphotropic retrovirus related to HTLV-III/LAV from wild-caught African green monkeys. Science 230:951-954. [DOI] [PubMed] [Google Scholar]
- 30.Kimata, J. T., J. J. Gosink, V. N. KewalRamani, L. M. Rudensey, D. R. Littman, and J. Overbaugh. 1999. Coreceptor specificity of temporal variants of simian immunodeficiency virus Mne. J. Virol. 73:1655-1660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kirchhoff, F., K. Mori, and R. C. Desrosiers. 1994. The “V3” domain is a determinant of simian immunodeficiency virus cell tropism. J. Virol. 68:3682-3692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kirchhoff, F., H. G. Morrison, M. G. Murray, P. Rennert, and R. C. Desrosiers. 1994. SIVmac expressing hybrid envelope proteins containing HIV-1 V3 and/or C4 sequences is not competent for replication. AIDS Res. Hum. Retrovir. 10:309-313. [DOI] [PubMed] [Google Scholar]
- 33.Lee, B., M. Sharron, L. J. Montaner, D. Weissman, and R. W. Doms. 1999. Quantification of CD4, CCR5, and CXCR4 levels on lymphocyte subsets, dendritic cells, and differentially conditioned monocyte-derived macrophages. Proc. Natl. Acad. Sci. USA 96:5215-5220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Liu, Q. H., D. A. Williams, C. McManus, F. Baribaud, R. W. Doms, D. Schols, E. De Clercq, M. I. Kotlikoff, R. G. Collman, and B. D. Freedman. 2000. HIV-1 gp120 and chemokines activate ion channels in primary macrophages through CCR5 and CXCR4 stimulation. Proc. Natl. Acad. Sci. USA 97:4832-4837. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Liu, Z. Q., S. Muhkerjee, M. Sahni, C. McCormick-Davis, K. Leung, Z. Li, V. H. Gattone, C. Tian, R. W. Doms, T. L. Hoffman, R. Raghavan, O. Narayan, and E. B. Stephens. 1999. Derivation and biological characterization of a molecular clone of SHIV(KU-2) that causes AIDS, neurological disease, and renal disease in rhesus macaques. Virology 260:295-307. [DOI] [PubMed] [Google Scholar]
- 36.Mamounas, M., D. J. Looney, R. Talbott, and F. Wong-Staal. 1995. An infectious chimeric human immunodeficiency virus type 2 (HIV-2) expressing the HIV-1 principal neutralizing determinant. J. Virol. 69:6424-6429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Marx, P. A., and Z. Chen. 1998. The function of simian chemokine receptors in the replication of SIV. Semin. Immunol. 10:215-223. [DOI] [PubMed] [Google Scholar]
- 38.Meister, S., C. Otto, A. Papkalla, M. Krumbiegel, S. Pohlmann, and F. Kirchhoff. 2001. Basic amino acid residues in the V3 loop of simian immunodeficiency virus envelope alter viral coreceptor tropism and infectivity but do not allow efficient utilization of CXCR4 as entry cofactor. Virology 284:287-296. [DOI] [PubMed] [Google Scholar]
- 39.Muller, M. C., N. K. Saksena, E. Nerrienet, C. Chappey, V. M. Herve, J. P. Durand, P. Legal-Campodonico, M. C. Lang, J. P. Digoutte, A. J. Georges, et al. 1993. Simian immunodeficiency viruses from central and western Africa: evidence for a new species-specific lentivirus in tantalus monkeys. J. Virol. 67:1227-1235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Owen, S. M., S. Masciotra, F. Novembre, J. Yee, W. M. Switzer, M. Ostyula, and R. B. Lal. 2000. Simian immunodeficiency viruses of diverse origin can use CXCR4 as a coreceptor for entry into human cells. J. Virol. 74:5702-5708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Parren, P. W., J. P. Moore, D. R. Burton, and Q. J. Sattentau. 1999. The neutralizing antibody response to HIV-1: viral evasion and escape from humoral immunity. AIDS 13(Suppl. A):S137-S162. [PubMed] [Google Scholar]
- 42.Pohlmann, S., N. Stolte, J. Munch, P. Ten Haaft, J. L. Heeney, C. Stahl-Hennig, and F. Kirchhoff. 1999. Co-receptor usage of BOB/GPR15 in addition to CCR5 has no significant effect on replication of simian immunodeficiency virus in vivo. J. Infect. Dis. 180:1494-1502. [DOI] [PubMed] [Google Scholar]
- 43.Popik, W., and P. M. Pitha. 2000. Inhibition of CD3/CD28-mediated activation of the MEK/ERK signaling pathway represses replication of X4 but not R5 human immunodeficiency virus type 1 in peripheral blood CD4+ T lymphocytes. J. Virol. 74:2558-2566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Ratner, L., W. Haseltine, R. Patarca, K. J. Livak, B. Starcich, S. F. Josephs, E. R. Doran, J. A. Rafalski, E. A. Whitehorn, K. Baumeister, et al. 1985. Complete nucleotide sequence of the AIDS virus, HTLV-III. Nature 313:277-284. [DOI] [PubMed] [Google Scholar]
- 45.Rucker, J., A. L. Edinger, M. Sharron, M. Samson, B. Lee, J. F. Berson, Y. Yi, B. Margulies, R. G. Collman, B. J. Doranz, M. Parmentier, and R. W. Doms. 1997. Utilization of chemokine receptors, orphan receptors, and herpesvirus-encoded receptors by diverse human and simian immunodeficiency viruses. J. Virol. 71:8999-9007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Sato, H., K. Kato, and Y. Takebe. 1999. Functional complementation of the envelope hypervariable V3 loop of human immunodeficiency virus type 1 subtype B by the subtype E V3 loop. Virology 257:491-501. [DOI] [PubMed] [Google Scholar]
- 47.Schols, D., and E. De Clercq. 1998. The simian immunodeficiency virus mnd(GB-1) strain uses CXCR4, not CCR5, as coreceptor for entry in human cells. J. Gen. Virol. 79:2203-2205. [DOI] [PubMed] [Google Scholar]
- 48.Siegel, F., R. Kurth, and S. Norley. 1995. Neither whole inactivated virus immunogen nor passive immunoglobulin transfer protects against SIVagm infection in the African green monkey natural host. J. Acquir. Immune Defic. Syndr. Hum. Retrovirol. 8:217-226. [DOI] [PubMed] [Google Scholar]
- 49.Siegel, F., S. Norley, S. Hartung, and R. Kurth. 1992. B-cell epitope mapping of the entire SIVagm envelope glycoprotein including fine mapping of immunogenic regions. J. Acquir. Immune Defic. Syndr. 5:583-590. [PubMed] [Google Scholar]
- 50.Unutmaz, D., V. N. KewalRamani, and D. R. Littman. 1998. G protein-coupled receptors in HIV and SIV entry: new perspectives on lentivirus-host interactions and on the utility of animal models. Semin. Immunol. 10:225-236. [DOI] [PubMed] [Google Scholar]
- 51.Wilk, T., T. Pfeiffer, and V. Bosch. 1992. Retained in vitro infectivity and cytopathogenicity of HIV-1 despite truncation of the C-terminal tail of the env gene product. Virology 189:167-177. [DOI] [PubMed] [Google Scholar]
- 52.Wyatt, R., P. D. Kwong, E. Desjardins, R. W. Sweet, J. Robinson, W. A. Hendrickson, and J. G. Sodroski. 1998. The antigenic structure of the HIV gp120 envelope glycoprotein. Nature 393:705-711. [DOI] [PubMed] [Google Scholar]