Abstract
Anidulafungin is an echinocandin with activity against Candida species and Aspergillus species. Adult dosages under study are 50 mg/day for esophageal candidiasis and 100 mg/day for invasive candidiasis and aspergillosis. Little is known, however, about the safety and pharmacokinetics of anidulafungin in children. A multicenter, ascending-dosage study of neutropenic pediatric patients was therefore conducted. Patients were divided into two age cohorts (2 to 11 years and 12 to 17 years) and were enrolled into sequential groups to receive 0.75 or 1.5 mg/kg of body weight/day. Blood samples were obtained following the first and fifth doses. Anidulafungin was assayed in plasma, and pharmacokinetic parameters were determined. Safety was assessed using National Cancer Institute (NCI) common toxicity criteria. Pharmacokinetic parameters were determined for 12 patients at each dosage (0.75 mg/kg/day or 1.5 mg/kg/day). Concentrations and drug exposures were similar for patients between age cohorts, and weight-adjusted clearance was consistent across age. No drug-related serious adverse events were observed. One patient had fever (NCI toxicity grade of 3), and one patient had facial erythema, which resolved with slowing the infusion rate. Anidulafungin in pediatric patients was well tolerated and can be dosed based on body weight. Pediatric patients receiving 0.75 mg/kg/day or 1.5 mg/kg/day have anidulafungin concentration profiles similar to those of adult patients receiving 50 or 100 mg/day, respectively.
Anidulafungin is a novel antifungal agent of the echinocandin class with activity against Candida and Aspergillus species (2, 3, 6, 8, 9, 11-15, 18, 19). This drug has been studied with adult patients at dosages ranging from 50 to 100 mg/day for the treatment of esophageal candidiasis, invasive candidiasis, and candidemia, where it has been demonstrated to be well tolerated (4, 5). A population pharmacokinetic analysis of plasma samples from 225 adult patients treated with anidulafungin demonstrated a two-compartment model with first-order elimination kinetics (5). Weight and gender are covariates in this model but have only a small impact on the plasma concentrations of anidulafungin. Dose modifications because of weight or gender differences in adults are therefore not required for anidulafungin (5). Although much is known about the pharmacokinetic properties of anidulafungin in adults, very little information regarding its properties in pediatric patients is known.
Among the immunocompromised pediatric patients at high risk for development of invasive fungal infections are hospitalized children who have become neutropenic as a result of chemotherapy or other therapeutic interventions, such as hematopoietic stem cell transplantation (1, 18).
The present study was conducted to assess the safety, tolerability, and pharmacokinetics of anidulafungin administered empirically to neutropenic children at high risk for invasive mycoses.
MATERIALS AND METHODS
Objectives and study design.
This was a multicenter, open-label, dosage-escalation study designed to determine the safety, tolerability, and pharmacokinetics of intravenous anidulafungin administered as early empirical therapy for the prevention of invasive fungal infections in immunocompromised hospitalized children with neutropenia.
Key enrollment criteria.
Children, 2 to 17 years of age, with neutropenia resulting from cytotoxic chemotherapy or aplastic anemia were eligible to participate in the study if the expected duration of neutropenia was to be at least 10 days. Neutropenia was defined as an absolute neutrophil count (ANC) of <500 neutrophils/mm3 or an ANC of <1,000 neutrophils/mm3 that was expected to fall below 500 neutrophils/mm3 within 72 h. A total of 24 patients meeting all entry criteria were to be enrolled equally into two age cohorts, 2 to 11 and 12 to 17 years of age.
Major exclusion criteria included proven invasive fungal infection at study entry, prior treatment with systemic antifungal agents other than oral nonabsorbable azoles, previous exposure to anidulafungin, serum levels of aspartate aminotransferase or alanine aminotransferase more than 5 times the upper limit of normal, serum levels of total bilirubin more than 2.5 times the upper limit of normal, or an estimated creatinine clearance less than 30 ml/min.
The appropriate institutional review boards at each of the five participating centers approved the study. Prior to the start of the study, written, informed consent was obtained from each patient or guardian.
Study drug administration.
The dosages of anidulafungin studied with these children were extrapolated from adult studies. A pediatric dosage of 0.75 mg/kg of body weight/day was chosen to represent the anidulafungin concentration-time profile achieved following the administration of 50 mg/day to adults. The 1.5 mg/kg/day dosage was chosen to represent the anidulafungin concentration-time profile achieved following the administration of 100 mg/day to adults. A weight-based dosage with children is consistent with the pharmacokinetic properties of anidulafungin, i.e., the distributive volume is a function related to patient weight and elimination is by degradation (5, 7). Weight-based dosages used in the present study are consistent with algorithms reported for dosage adjustments from children to adults (16).
Anidulafungin was administered intravenously to two dosage groups within each age cohort. The low-dosage group received a loading dose of 1.5 mg/kg infused over 90 min on day 1 that was not to exceed a total dose of 100 mg and daily maintenance dosages of 0.75 mg/kg infused over 45 min that were not to exceed 50 mg each day. The high-dosage group received a loading dose of 3 mg/kg infused over 180 min on day 1 that was not to exceed a total dose of 200 mg and daily maintenance doses of 1.5 mg/kg infused over 90 min that were not to exceed 100 mg each day. Anidulafungin was administered to each patient once daily at approximately the same time each day. The duration of treatment was between 5 and 28 days. Patients were to receive study drug for at least 5 days and until one of the following criteria were met: recovery from neutropenia (ANC > 500 neutrophils/mm3), initiation of empirical antifungal therapy per local standard of care, proven invasive fungal infection, or until 28 days of anidulafungin therapy was administered, whichever occurred first.
Anidulafungin was not administered to the high-dosage group until after safety and pharmacokinetic data obtained from all patients in the low-dosage group were reviewed independently by the investigators and the industrial sponsor. Restrictions on dosage escalation included no more than two patients in the corresponding age cohort in the low-dosage group experiencing non-infusion-related toxicity with an intensity of National Cancer Institute (NCI) common toxicity criteria (CTC) (10) grade 3 or above and no more than two patients in the corresponding age cohort in the low-dosage group experiencing infusion-related dyspnea with an intensity of grade 3 or above.
Pharmacokinetic sampling.
On days 1 and 5, venous blood samples (3 ml) were drawn into heparinized collection tubes from sites other than the injection site up to 2 h before, immediately after the completion of, and 3, 6, 12, and 24 h after the start of the anidulafungin infusion. Trough concentrations of anidulafungin were determined from venous blood samples drawn up to 2 h before the start of anidulafungin infusion on days 3, 7, and 28 or the last day of administration. Collection tubes were immediately placed on ice and, within 30 min, were centrifuged (1,500 × g for 10 min) at approximately 4°C. Plasma was stored in transfer tubes at −80°C until analyzed.
Anidulafungin assay.
Plasma samples were assayed for anidulafungin by use of a validated liquid chromatography-tandem mass spectrometry method (MDS Pharma Services, Montreal, Quebec, Canada). The method was validated in the linear range from 0.100 to 20.0 μg/ml, which was extended to 40 μg/ml by use of a 10-fold dilution. Overall precision of the method using quality control samples, as measured by relative standard deviation, was less than or equal to 9.8%. Overall accuracy, as measured by the percentage of theoretical recovery for anidulafungin, ranged from 97.5% to 106%. The accuracy for the twofold diluted control was 98.1%. Anidulafungin is stable in plasma stored at −20°C for up to 114 days and at −80°C for up to 14 months (Prevalere Life Sciences, Inc., Whitesboro, NY).
Pharmacokinetic measures.
Pharmacokinetic parameters for anidulafungin were determined following the loading dose (day 1) and at steady state (day 5) for each patient from plasma concentration data using noncompartmental methods (WinNonlin Professional version 4.1; Pharsight Corp., Mountain View, CA). Pharmacokinetic measures were maximum observed plasma concentration (Cmax), area under the plasma concentration-time curve (AUC) through 24 h after the first dose (AUC0-24) or at steady state (AUCss) calculated by the linear trapezoidal rule, clearance (CL) calculated by dividing dose by AUC, volume of distribution at steady state (Vss) calculated by multiplying the dose by the ratio of the area under the first moment curve to the square of AUC, and terminal elimination half-life (t1/2) calculated from a linear regression of the log-linear portion of the log concentration-time curve. Trough concentrations of anidulafungin were summarized by collection day.
Safety measures.
Safety of anidulafungin was assessed from the frequency, intensity, and relationship to study drug of adverse events throughout the study. These included daily vital sign measurements (body temperature, blood pressure, and heart rate) and the results of clinical laboratory tests (hematology and serum chemistry) that were performed before anidulafungin administration on day 1, on days 3 and 5 of the study, and then twice weekly while patients received anidulafungin. An electrocardiogram was performed before anidulafungin administration on day 1 and within 1 h after anidulafungin administration on day 5. These were interpreted by an independent central laboratory (Cardiabase, Nice, France). Prior and concomitant medications were recorded for each patient. Adverse events were graded according to the NCI CTC and reported as mild (CTC grade 1), moderate (CTC grade 2), or severe (CTC grades 3 or 4).
Microbiology measures.
Duplicate aerobic screening blood cultures obtained from all patients were evaluated to exclude candidemia within 24 h before study entry. Cultures were obtained once daily for febrile patients and as clinically indicated for all others.
Efficacy measures.
A limited analysis of efficacy of anidulafungin was performed as a secondary end point of this study. The clinical outcome for each patient was categorized by the investigator as success (if the patient recovered from neutropenia without investigator-diagnosed deeply invasive fungal infection), failure (if the patient required systemic antifungal therapy for investigator-diagnosed breakthrough proven invasive fungal infection), or indeterminate (if anidulafungin was discontinued for reasons other than failure).
Analysis populations.
Data from all patients who received at least one dose of anidulafungin were analyzed for safety and tolerability and, secondarily, for efficacy. Data from all patients who received anidulafungin and who provided blood samples were included in summaries of the pharmacokinetic profiles. Safety and pharmacokinetic parameters were summarized by age cohort within each dosage group.
RESULTS
Patients.
Twenty-five patients, 12 in the 2- to 11-year old cohort and 13 in the 12- to 17-year old cohort, were enrolled in four centers; all received at least one dose of anidulafungin. The median age (range) of all patients enrolled was 13 years (2 to 16 years). The median ages (ranges) of the younger cohorts were 9 years (3 to 11 years) and 8 years (2 to 11 years) for the low- and high-dosage groups, respectively. The median age (range) for both the low- and the high-dosage group of the older cohort was 14 years (13 to 16 years). The median weights of the younger cohorts were 26.6 and 34.8 kg for the low- and high-dosage groups, respectively, and 58.7 and 56.4 kg, respectively, for the older cohorts in the corresponding dosage groups (Table 1).
TABLE 1.
Demography and baseline characteristics
| Characteristic | Value for:
|
||||
|---|---|---|---|---|---|
| Low-dosage group (n = 13)
|
High-dosage group (n = 12)
|
All patients (n = 25) | |||
| Ages 2-11 yr (n = 6) | Ages 12-17 yr (n = 7) | Ages 2-11 yr (n = 6) | Ages 12-17 yr (n = 6) | ||
| Median age in yr (range) | 9 (3-11) | 14 (13-16) | 8 (2-11) | 14 (13-16) | 13 (2-16) |
| Gender (M:F)a | 3:3 | 3:4 | 3:3 | 4:2 | 13:12 |
| Race (n) | |||||
| Asian | 0 | 0 | 1 | 0 | 1 |
| Black/African-American | 0 | 2 | 1 | 2 | 5 |
| White | 3 | 4 | 4 | 2 | 13 |
| Hispanic/Latino | 2 | 1 | 0 | 2 | 5 |
| Other | 1 | 0 | 0 | 0 | 1 |
| Median wt in kg (range) | 26.6 (15.2-56.2) | 58.7 (48.1-99.2) | 34.8 (15.8-41.2) | 56.4 (22.0-86.0) | 42.8 (15.2-99.2) |
| Comorbid diseases (n) | |||||
| Acute lymphocytic leukemia | 1 | 2 | 1 | 0 | 4 |
| Acute myelogenous leukemia | 1 | 3 | 2 | 0 | 6 |
| Chronic myelogenous leukemia | 1 | 0 | 0 | 0 | 1 |
| Lymphoma | 0 | 0 | 1 | 0 | 1 |
| Sarcoma | 0 | 1 | 0 | 0 | 1 |
| Neuroblastoma | 1 | 0 | 0 | 0 | 1 |
| Aplastic anemia | 0 | 1 | 1 | 4 | 6 |
| Inherited immunodeficiency | 1 | 0 | 0 | 1 | 2 |
M, male; F, female.
The mean duration of treatment was 8.7 days (1 to 23 days). Twenty-three (92%) patients received study drug for at least 5 days; one patient who received one dose of study drug was replaced, and one patient received study drug for 4 days.
All patients had an ANC of <500 neutrophils/mm3 before receiving their first dose of study drug. As shown in Table 1, the most common hematological baseline diseases were acute myelogenous leukemia, aplastic anemia, and acute lymphocytic leukemia. The most common types of hematopoietic stem cell transplants were nonmyeloablative and matched unrelated (five patients each). Two patients received myeloablative transplants: one patient received a transplant from a matched, related donor, and one patient received an autologous transplant. Three patients received unrelated cord blood transplants. There was no discernible pattern of distribution of baseline diseases across the dosage groups or age cohorts, with the exception that four patients with aplastic anemia were in the 12- to 17-year old cohort and were coincidentally enrolled in the high-dosage group.
Pharmacokinetic profile of anidulafungin.
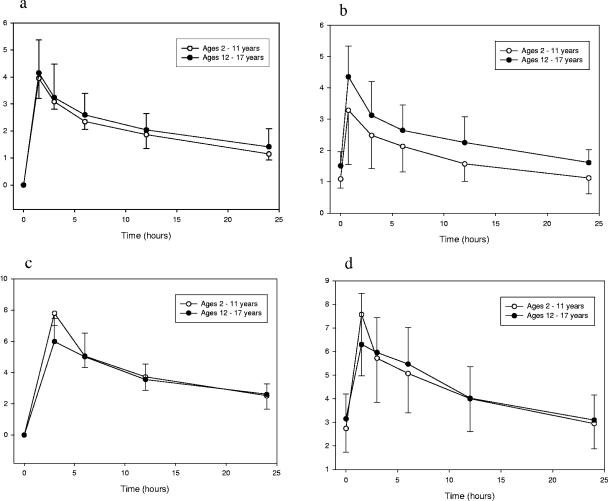
The pharmacokinetic profile of anidulafungin was determined from 320 plasma concentrations obtained from 24 children. Anidulafungin plasma concentration-time curves following the first and fifth doses are presented for each dosage group in Fig. 1. The pharmacokinetic parameters following the loading dose and at steady state are shown in Tables 2 and 3, respectively.
FIG. 1.
(a) Anidulafungin plasma concentration-time profiles in children with compromised immunity and neutropenia after receiving a 1.5-mg/kg anidulafungin loading dose. (b) Steady-state anidulafungin plasma concentration-time profiles in these patients after receiving maintenance dosages of 0.75 mg/kg/day of anidulafungin (day 5). (c) Anidulafungin plasma concentration-time profiles in children with compromised immunity and neutropenia after receiving a 3.0-mg/kg anidulafungin loading dose. (d) Steady-state anidulafungin plasma concentration-time profiles for these patients after receiving maintenance dosages of 1.5 mg/kg/day of anidulafungin (day 5).
TABLE 2.
Single-dose pharmacokinetic profile of anidulafungin in children with compromised immunity and neutropenia
| Parameter | Value for group with dose
|
Value for all patients (n = 24)
|
||||
|---|---|---|---|---|---|---|
| 1.5 mg/kg (n = 12)
|
3.0 mg/kg (n = 12)
|
|||||
| Ages 2-11 yr (n = 6) | Ages 12-17 yr (n = 6) | Ages 2-11 yr (n = 6) | Ages 12-17 yr (n = 6) | 1.5 mg/kg (n = 12) | 3.0 mg/kg (n = 12) | |
| Cmax (mg/ml) | ||||||
| Mean (SD) | 3.95 (0.74) | 4.10 (1.11) | 7.80 (0.76) | 5.99 (1.50) | 4.02 (0.9) | 6.90 (1.13) |
| Range | 3.04-4.91 | 2.98-6.08 | 6.93-8.97 | 4.06-7.88 | 2.98-6.08 | 4.06-8.97 |
| AUC0-24 (mg·h/ml) | ||||||
| Mean (SD) | 46.3 (8.70) | 49.6 (14.6) | 92.3 (11.9) | 87.2 (23.6) | 48.0 (11.6) | 89.7 (18.0) |
| Range | 34.7-54.1 | 40.0-78.7 | 77.4-107.5 | 56.1-119.2 | 34.7-78.7 | 56.1-119.2 |
| t1/2 (h) | ||||||
| Mean (SD) | 17.3 (3.7) | 24.3 (8.7) | 18.3 (6.7) | 20.8 (4.8) | 20.8 (6.2) | 19.5 (5.8) |
| Range | 14.7-24.7 | 13.3-36.0 | 14.2-31.8 | 17.4-29.3 | 13.3-36 | 14.2-31.8 |
| CL/kg (liters/h/kg) | ||||||
| Mean (SD) | 0.0208 (0.0052) | 0.0143 (0.0062) | 0.0200 (0.0058) | 0.0181 (0.0078) | 0.0175 (0.0057) | 0.0191 (0.0068) |
| Range | 0.0145-0.0275 | 0.0054-0.0199 | 0.0102-0.0266 | 0.0116-0.0316 | 0.0054-0.0275 | 0.0102-0.0316 |
| Vss (liters/kg) | ||||||
| Mean (SD) | 0.488 (0.086) | 0.430 (0.133) | 0.474 (0.036) | 0.523 (0.193) | 0.459 (0.110) | 0.499 (0.115) |
| Range | 0.399-0.602 | 0.267-0.610 | 0.421-0.529 | 0.375-0.857 | 0.267-0.610 | 0.375-0.857 |
TABLE 3.
Multiple-dose pharmacokinetic profile of anidulafungin in children with compromised immunity and neutropenia
| Parameter | Value for group with dose
|
Value for all patients (n = 24)
|
||||
|---|---|---|---|---|---|---|
| 0.75 mg/kg/day (n = 12)
|
1.50 mg/kg/day (n = 12)
|
|||||
| Ages 2-11 yr (n = 6) | Ages 12-17 yr (n = 6) | Ages 2-11 yr (n = 6) | Ages 12-17 yr (n = 6) | 0.75 mg/kg/day (n = 12) | 1.5 mg/kg/day (n = 12) | |
| Cmax (mg/ml) | ||||||
| Mean (SD) | 3.32 (1.66) | 4.35 (0.98) | 7.57 (2.59) | 6.88 (1.67) | 3.83 (1.32) | 7.23 (2.13) |
| Range | 0.91-5.98 | 3.1-5.57 | 5.22-12.3 | 3.71-8.66 | 0.91-5.98 | 3.71-12.3 |
| AUCss (mg·h/ml) | ||||||
| Mean (SD) | 41.1 (15.8) | 56.2 (15.6) | 96.1 (38.0) | 102.9 (29.0) | 48.6 (15.7) | 99.5 (33.5) |
| Range | 16.5-57.8 | 31.8-79.8 | 43.2-155.7 | 50.3-134.1 | 16.5-79.8 | 43.2-155.7 |
| t1/2 (h) | ||||||
| Mean (SD) | 20.3 (7.9) | 26.0 (10.2) | 18.9 (3.5) | 21.1 (5.2) | 23.1 (9.0) | 19.9 (4.3) |
| Range | 13.9-35.1 | 12.0-38.9 | 13.6-24.1 | 15.0-27.8 | 12.0-38.9 | 13.6-27.8 |
| CL/kg (liters/h/kg) | ||||||
| Mean (SD) | 0.0217 (0.0123) | 0.0133 (0.0031) | 0.0163 (0.0048) | 0.0156 (0.0079) | 0.0175 (0.0077) | 0.0159 (0.0063) |
| Range | 0.0113-0.0446 | 0.0095-0.018 | 0.0094-0.0231 | 0.0096-0.0311 | 0.0095-0.0446 | 0.0094-0.0311 |
| Vss (liters/kg) | ||||||
| Mean (SD) | 0.575 (0.243) | 0.499 (0.231) | 0.419 (0.066) | 0.449 (0.166) | 0.537 (0.237) | 0.434 (0.116) |
| Range | 0.337-0.962 | 0.163-0.803 | 0.319-0.5 | 0.314-0.73 | 0.163-0.962 | 0.314-0.730 |
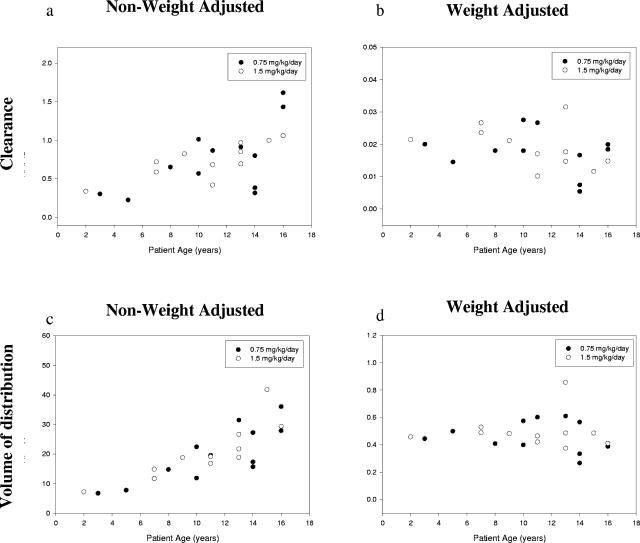
Exposure to anidulafungin increased in a manner consistent with dose proportionality within both age cohorts. Maximum anidulafungin plasma concentrations occurred immediately after administration; steady-state plasma concentrations were achieved after administering the loading dose. Trough anidulafungin plasma concentrations remained constant throughout the study, ranging from approximately 0.5 to 3 mg/ml for patients in the low-dosage group and from approximately 1 to 5 mg/ml for patients in the high-dosage group. The mean steady-state values of CL, Vss, and t1/2 were 0.018 liters/h/kg, 0.54 liters/kg, and 22.9 h, respectively, for patients receiving 0.75 mg/kg/day versus 0.016 liters/h/kg, 0.43 liters/kg, and 19.9 h, respectively, for patients receiving 1.5 mg/kg/day. Interpatient variability in CL and Vss is explained by body weight but not patient age (Fig. 2).
FIG. 2.
Non-weight-adjusted (a) and weight-normalized (b) anidulafungin clearance versus patient age on day 1 of infusion, and non-weight-adjusted (c) and weight-normalized (d) anidulafungin volume of distribution versus patient age.
Safety and tolerability.
All patients experienced at least one adverse event; most of these events were mild or moderate in severity. The most common adverse events regardless of relationship to study drug experienced by at least 5 (20%) patients were fever in 11 (44%) patients; graft-versus-host disease, mucosal inflammation, and vomiting in 6 (24%) patients each; and cough, hypertension, and hypomagnesemia in 5 (20%) patients each.
In the 0.75-mg/kg dosage group, three (12%) patients experienced adverse events that led to discontinuation of anidulafungin. These included two fevers unrelated to study drug and one grand mal seizure attributed to imipenem-cilastatin. Four (16%) patients experienced adverse events considered by the investigator to be possibly or probably related to anidulafungin. These events included feeling abnormal, facial erythema and rash, elevation in serum blood urea nitrogen, and fever and hypotension.
Five (20%) patients in the low-dosage group experienced 13 serious adverse events; all events were considered by the investigators to be unrelated or likely unrelated to anidulafungin. All but one serious adverse event in the low-dosage group (septic shock that was reported on day −2) occurred off therapy, that is, from 1 to 48 days after the last administration of anidulafungin. All serious adverse events in the low-dosage group occurred as single events, and none were attributed to study drug by the investigators. One patient in the low-dosage group died within 30 days after the last administration of anidulafungin from multiorgan failure secondary to Pseudomonas aeruginosa sepsis that was considered to be unrelated to participation in the clinical study.
One patient (a 16-year-old boy) in the low-dosage group experienced moderate facial erythema and rash at the start of study drug infusion, which were not accompanied by additional adverse events of wheezing or hypotension. The erythema and rash resolved within 1.5 h after interruption of the study drug. Subsequent resumption and 10 other infusions of anidulafungin occurred without recurrence of these adverse events in this patient. No other infusion or injection site reactions were reported among any of the other patients who received anidulafungin.
No patients in the 1.5-mg/kg dosage group experienced adverse events that led to discontinuation of anidulafungin or that were considered by the investigators to be possibly or probably related to the drug. Five (20%) patients in this high-dosage group experienced a total of 12 serious events, none of which were considered to be related to anidulafungin administration. Most of these adverse events were reported to occur in children in the 2- to 11-year cohort, and all but one event (neuropathy reported on day 11) were reported between 3 and 27 days following the last dose of anidulafungin. All serious adverse events in the high-dosage group occurred as single events, with the exception of two patients who experienced respiratory failure.
Two patients died within 30 days after the last administration of study drug (21 and 26 days, respectively); the primary causes of death were multisystem organ failure secondary to pseudomonas sepsis and respiratory failure, respectively. Both deaths were unrelated to anidulafungin per investigator attribution. A third patient died from progression of acute myelogenous leukemia 99 days after the last administration of study drug.
Changes from baseline hematology values were attributed to changes in underlying disease or therapy and generally improved during the study. No patient had concurrent values of more than one clinical laboratory parameter of potential clinical concern that suggested impaired hepatic or renal function.
No clinically significant changes from baseline in cardiac conduction, cardiac rhythm, or repolarization parameters were observed during anidulafungin treatment. No central tendency effect upon QTc interval was identified. For all patients, the use of prior and concomitant medications was consistent with underlying disease and treatment.
Efficacy.
No patient in the study was diagnosed with an invasive fungal infection.
DISCUSSION
This was the first pediatric study to evaluate the pharmacokinetics, safety, and tolerability of anidulafungin. With the exception of one infusion-related event associated with erythema and dyspnea, the results from this study demonstrate that anidulafungin was well tolerated by these pediatric patients. In addition, no untoward trends in serum chemistry, hematology, or electrocardiographic studies were observed for any of the dosage groups or age cohorts.
In this study, plasma concentrations and exposures of anidulafungin observed with children receiving weight-adjusted dosages of 0.75 mg/kg/day and 1.5 mg/kg/day were consistent with dose proportionality and were similar to those observed with adults who were treated for esophageal candidiasis and candidemia with 50 mg/day and 100 mg/day of anidulafungin, respectively (5). As also seen with adults, steady-state anidulafungin plasma concentrations were achieved in children after the first loading dose, which was twice the amount of each successive maintenance dose. Steady-state anidulafungin plasma concentrations in children and adults receiving the lower dosage (0.75 mg/kg/day and 50 mg/day, respectively) remained above 1 mg/liter; doubling the dosage in children and adults (to 1.5 mg/kg/day and to 100 mg/day, respectively) doubled the steady-state anidulafungin plasma concentration to above 2 mg/liter (5). Corresponding values of AUCss in children and adults also doubled, from approximately 50 mg · h/liter to 100 mg · h/liter. The mean elimination half-life of anidulafungin approximated 20 h for each age cohort in each dosage group. This 20-h t1/2 for children is comparable to the 26.5-h t1/2 for adults (5) and supports once-daily dosing in the pediatric population as administered to adults in clinical studies.
Anidulafungin plasma concentrations and pharmacokinetic parameters were comparable between age cohorts within each dosage group, supporting weight-adjusted dosages for children older than 2 years of age. Body weight of pediatric patients, but not patient age, affected anidulafungin CL and Vss. These findings were expected because anidulafungin is nonenzymatically degraded in the body. Elimination of anidulafungin is not dependent upon renal function, hepatic function, or possible age-dependent metabolic processes (5, 7). Thus, pediatric body weight is the only consideration in achieving anidulafungin plasma concentrations comparable to those observed with adults.
The results of this study cannot be extrapolated to other echinocandins. For example, caspofungin is subject to biotransformation by metabolism and requires a dosage adjustment based upon a calculation of body surface area rather than a weight-adjusted scale. This is due largely to a reduced t1/2 for children relative to that for adults (17).
Both the 0.75- and 1.5-mg/kg daily doses of empirically administered anidulafungin were well tolerated in the neutropenic children who participated in this study. There were no discernible patterns of toxicity or evidence of a dose-response relationship between dosage groups in adverse-event intensity or attribution, the frequency of serious adverse events or adverse events leading to discontinuation of study drug, or the number of patient deaths. Anidulafungin was not associated with hepatic or renal impairment in these children with neutropenia. In this small study, no central tendency effect upon QTc interval was identified.
Infusion-related toxicity consisting of flushing and dyspnea without hypoxia was observed to occur in one older child in the high-dosage group. The symptoms rapidly improved upon stopping the infusion and administration of diphenhydramine. The symptoms observed with this patient were reminiscent of the “red man syndrome,” due to vancomycin-mediated systemic histamine release. The infusion was resumed after the symptoms abated, and no subsequent adverse events were reported. This suggests that infusion-related flushing and dyspnea may be managed without discontinuing anidulafungin and with close observation, supportive care, and careful reinstitution of the infusion.
Although the efficacy of anidulafungin was not a primary component of this study, no child in this study at high risk for invasive fungal infections was diagnosed with a breakthrough fungal infection.
In conclusion, anidulafungin dosages of 0.75 mg/kg/day and 1.5 mg/kg/day demonstrate concentration-time profiles similar to those of adult patients receiving 50 or 100 mg/day, respectively. Anidulafungin at these dosages was found to be well tolerated in neutropenic children older than 2 years of age and should be considered in future clinical trials designed to study the prevention and treatment of invasive fungal infections in pediatric patients at high risk for these mycoses.
Acknowledgments
This work was supported in part by grants to the individual sites and in part by the Intramural Research Program of the National Cancer Institute.
REFERENCES
- 1.Benjamin, D. K., Jr., W. C. Miller, S. Bayliff, L. Martel, K. A. Alexander, and P. L. Martin. 2002. Infections diagnosed in the first year after pediatric stem cell transplantation. Pediatr. Infect. Dis. J. 21:227-234. [DOI] [PubMed] [Google Scholar]
- 2.Chavez, M., S. Bernal, A. Valverde, M. J. Gutierrez, G. Quindos, and E. M. Mazuelos. 1999. In-vitro activity of voriconazole (UK-109,496), LY303366 and other antifungal agents against oral Candida spp. isolates from HIV-infected patients. J. Antimicrob. Chemother. 44:697-700. [DOI] [PubMed] [Google Scholar]
- 3.Cuenca-Estrella, M., E. Mellado, T. M. Diaz-Guerra, A. Monzon, and J. L. Rodriguez-Tudela. 2000. Susceptibility of fluconazole-resistant clinical isolates of Candida spp. to echinocandin LY303366, itraconazole and amphotericin B. J. Antimicrob. Chemother. 46:475-477. [DOI] [PubMed] [Google Scholar]
- 4.Dowell, J. A., M. Stogniew, D. Krause, T. Henkel, and I. E. Weston. 2005. Assessment of the safety and pharmacokinetics of anidulafungin when administered with cyclosporine. J. Clin. Pharmacol. 45:227-233. [DOI] [PubMed] [Google Scholar]
- 5.Dowell, J. A., W. Knebel, T. Ludden, M. Stogniew, D. Krause, and T. Henkel. 2004. Population pharmacokinetic analysis of anidulafungin, an echinocandin antifungal. J. Clin. Pharmacol. 44:590-598. [DOI] [PubMed] [Google Scholar]
- 6.Espinel-Ingroff, A. 1998. Comparison of in vitro activities of the new triazole SCH56592 and the echinocandins MK-0991 (L-743,872) and LY303366 against opportunistic filamentous and dimorphic fungi and yeasts. J. Clin. Microbiol. 36:2950-2956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Groll, A. H., D. Mickiene, R. Petraitiene, V. Petraitis, C. A. Lyman, J. S. Bacher, S. C. Piscitelli, and T. J. Walsh. 2001. Pharmacokinetic and pharmacodynamic modeling of anidulafungin (LY303366): reappraisal of its efficacy in neutropenic animal models of opportunistic mycoses using optimal plasma sampling. Antimicrob. Agents Chemother. 45:2845-2855. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Klepser, M. E., E. J. Ernst, M. E. Ernst, S. A. Messer, and M. A. Pfaller. 1998. Evaluation of endpoints for antifungal susceptibility determinations with LY303366. Antimicrob. Agents Chemother. 42:1387-1391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Moore, C. B., K. L. Oakley, and D. W. Denning. 2001. In vitro activity of a new echinocandin, LY303366, and comparison with fluconazole, flucytosine and amphotericin B against Candida species. Clin. Microbiol. Infect. 7:11-16. [DOI] [PubMed] [Google Scholar]
- 10.National Institutes of Health. 1999. Common toxicity criteria for adverse events, v2.0. [Online.] National Institutes of Health, Bethesda, Md. http://ctep.cancer.gov/reporting/.
- 11.Ostrosky-Zeichner, L., J. H. Rex, P. G. Pappas, R. J. Hamill, R. A. Larsen, H. W. Horowitz, W. G. Powderly, N. Hyslop, C. A. Kauffman, J. Cleary, J. E. Mangino, and J. Lee. 2003. Antifungal susceptibility survey of 2,000 bloodstream Candida isolates in the United States. Antimicrob. Agents Chemother. 47:3149-3154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Petraitiene, R., V. Petraitis, A. H. Groll, M. Candelario, T. Sein, A. Bell, C. A. Lyman, C. L. McMillian, J. Bacher, and T. J. Walsh. 1999. Antifungal activity of LY303366, a novel echinocandin B, in experimental disseminated candidiasis in rabbits. Antimicrob. Agents Chemother. 43:2148-2155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Petraitis, V., R. Petraitiene, A. H. Groll, A. Bell, D. P. Callender, T. Sein, R. L. Schaufele, C. L. McMillian, J. Bacher, and T. J. Walsh. 1998. Antifungal efficacy, safety, and single-dose pharmacokinetics of LY303366, a novel echinocandin B, in experimental pulmonary aspergillosis in persistently neutropenic rabbits. Antimicrob. Agents Chemother. 42:2898-2905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Petraitis, V., R. Petraitiene, A. H. Groll, T. Sein, R. L. Schaufele, C. A. Lyman, A. Francesconi, J. Bacher, S. C. Piscitelli, and T. J. Walsh. 2001. Dosage-dependent antifungal efficacy of V-echinocandin (LY303366) against experimental fluconazole-resistant oropharyngeal and esophageal candidiasis. Antimicrob. Agents Chemother. 45:471-479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Pfaller, M. A., F. Marco, S. A. Messer, and R. N. Jones. 1998. In vitro activity of two echinocandin derivatives, LY303366 and MK-0991 (L-743,792), against clinical isolates of Aspergillus, Fusarium, Rhizopus, and other filamentous fungi. Diagn. Microbiol. Infect. Dis. 30:251-255. [DOI] [PubMed] [Google Scholar]
- 16.Ritschel, W. A. 1992. Handbook of basic pharmacokinetics—including clinical applications. Drug Intelligence Publications, Hamilton, Ill.
- 17.Walsh, T. J., P. C. Adamson, N. L. Seibel, P. M. Flynn, M. N. Neely, C. Schwartz, A. Shad, S. L. Kaplan, M. M. Roden, J. A. Stone, A. Miller, S. K. Bradshaw, S. X. Li, C. A. Sable, and N. A. Kartsonis. Pharmacokinetics, safety, and tolerability of caspofungin in children and adolescents. Antimicrob. Agents Chemother. 49:4536-4545. [DOI] [PMC free article] [PubMed]
- 18.Zaoutis, T. E., H. M. Greves, E. Lautenbach, W. B. Bilker, and S. E. Coffin. 2004. Risk factors for disseminated candidiasis in children with candidemia. Pediatr. Infect. Dis. J. 23:635-641. [DOI] [PubMed] [Google Scholar]
- 19.Zhanel, G. G., J. A. Karlowsky, G. A. Harding, T. V. Balko, S. A. Zelenitsky, M. Friesen, A. Kabani, M. Turik, and D. J. Hoban. 1997. In vitro activity of a new semisynthetic echinocandin, LY-303366, against systemic isolates of Candida species, Cryptococcus neoformans, Blastomyces dermatitidis, and Aspergillus species. Antimicrob. Agents Chemother. 41:863-865. [DOI] [PMC free article] [PubMed] [Google Scholar]