Abstract
Retapamulin had the lowest rate of spontaneous mutations by single-step passaging and the lowest parent and selected mutant MICs by multistep passaging among all drugs tested for all Staphylococcus aureus strains and three Streptococcus pyogenes strains which yielded resistant clones. Retapamulin has a low potential for resistance selection in S. pyogenes, with a slow and gradual propensity for resistance development in S. aureus.
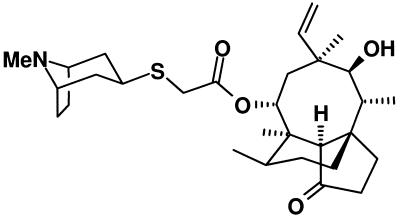
Pleuromutilins are a new class of antimicrobials which inhibit protein synthesis by interacting at a unique site on the 70S ribosome and demonstrate excellent in vitro activity against gram-positive and some gram-negative bacteria (2, 5, 9). This study used multi- and single-step passage studies to test the ability of retapamulin (Fig. 1), compared to those of mupirocin, fusidic acid (only against Staphylococcus aureus strains), cephalexin, erythromycin, linezolid, vancomycin, and quinupristin-dalfopristin, to select for resistance in 12 Staphylococcus aureus and 10 Streptococcus pyogenes strains.
FIG. 1.
Chemical structure of retapamulin.
S. aureus strains comprised three methicillin- and quinolone-susceptible, four methicillin- and quinolone-resistant, three vancomycin-intermediate, and two vancomycin-resistant (VRSA) strains. The 10 S. pyogenes strains comprised two macrolide-susceptible strains, two erm(B)-, three mef(A)-, and two erm(TR)-positive strains, and one strain with a mutation in the L4 ribosomal protein (68KGT insertion). Retapamulin and mupirocin powders were obtained from GlaxoSmithKline, Collegeville, Pa., and other drugs were obtained from their respective manufacturers. Initial MICs were determined by the CLSI agar dilution method (7).
Multipassage resistance selection was done as described previously (3, 6). Daily passages were continued until a more-than-four-fold increase in the MIC was found (minimum passage number, 14; maximum passage number, 50). If MICs of ≥32 μg/ml were found, subculturing in the presence of an antibiotic ceased. Prolonged selection for the full 50 days was conducted for three random staphylococcal strains and all three streptococcal strains showing retapamulin resistance development. The stability of acquired resistance was determined by MIC determination after 10 daily passages on drug-free agar.
The frequency of spontaneous single-passage mutations was determined as described previously (3, 6). Pulsed-field gel electrophoresis was used to confirm the identities of all parents and clones (3, 6).
Genes encoding the L3 ribosomal protein were amplified and sequenced from all parents and from clones for which an elevation in the retapamulin MIC was observed by the multipassage study. Eight S. aureus and seven S. pyogenes single-passage mutants were randomly selected for L3 analysis. The genes encoding ribosomal proteins L4 and L22 and domains II and V of 23S rRNA were amplified and sequenced for all S. aureus and S. pyogenes macrolide-resistant parents and randomly selected macrolide-resistant clones obtained by multipassage (10, 11). For five selected S. aureus fusidic acid-resistant clones and parent strains, sequencing analysis of the fusA gene, encoding the EF-G protein, was performed, and the presence of the fusB determinant was tested (8). The mechanism of mupirocin resistance was tested with five selected S. aureus and all resistant S. pyogenes clones by sequencing portions of the ileS gene, encoding isoleucyl-tRNA synthetase (IRS) (1).
The multipassage results with S. aureus are presented in Table 1. Retapamulin MICs rose from 0.03 to 0.125 μg/ml (parents) to 0.5 to 2 μg/ml after 14 to 20 days for 12/12 strains (3 strains chosen for prolonged selection for 50 days had MICs that rose to 4 to 16 μg/ml) (Table 1); quinupristin-dalfopristin MICs rose from 0.25 to 0.5 μg/ml (parents) to 2 to >4 μg/ml after 14 to 28 days for 12/12 strains; erythromycin MICs rose from 0.5 to 1 μg/ml to 16 to >64 μg/ml after 11 to 17 days for 5/5 strains; linezolid MICs rose from 2 to 4 μg/ml to 16 to >32 μg/ml after 11 to 46 days for 8/12 strains; cephalexin MICs rose from 2 to 8 μg/ml to 32 to 64 μg/ml after 4 to 18 days for 4/4 strains tested; mupirocin MICs rose from 0.25 to 32 μg/ml to 4 to >64 μg/ml after 4 to 14 days for 12/12 strains; and fusidic acid MICs rose from 0.5 to 8 μg/ml to 32 to >64 μg/ml after 4 to 14 days for 12/12 strains. Subculturing in the presence of vancomycin raised the vancomycin MIC of the Hershey VRSA strain from 32 to 2,048 μg/ml after 5 days (4). Among the retapamulin-selected clones, two with raised retapamulin MICs showed cross-resistance (defined as an ≥8-fold increase in MIC) to erythromycin. Five of eight strains with raised linezolid MICs had cross-resistance to retapamulin, and one quinupristin-dalfopristin-resistant clone had a raised retapamulin MIC.
TABLE 1.
Multipassage resistance selection results with S. aureus
| Strain | Antibiotica | Initial MIC (μg/ml) | Selected resistance
|
Retest MIC after 10 antibiotic-free subcultures
|
Detected resistance mechanismb | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| MIC | No. of passages | REP | MUP | FA | CEP | ERY | LIN | VAN | Q/D | ||||
| SA040 | REP | 0.125 | 2 | 16 | 2 | 0.5 | 0.5 | 4 | 0.5 | 8 | 2 | 0.5 | L3 mutations (G152D, D159Y) |
| MUP | 0.25 | 4 | 14 | 0.125 | 2 | 0.5 | 2 | 2 | 4 | 2 | 0.25 | IRS mutation (G593V) | |
| FA | 1 | 32 | 6 | 0.125 | 0.25 | 32 | 4 | 2 | 4 | 1 | 0.125 | EF-G mutation (P404R) | |
| CEP | 4 | 64 | 8 | 0.06 | 0.25 | 0.5 | 32 | 8 | 4 | 2 | 0.25 | NT | |
| ERY | 1 | 32 | 11 | 0.125 | 0.5 | 0.5 | 4 | 64 | 8 | 1 | 0.5 | L4 mutations (Q67K, G69E) | |
| LIN | 4 | 32 | 11 | 0.25 | 0.25 | 1 | 4 | 2 | >32 | 2 | 0.25 | — | |
| QD | 0.25 | 2 | 24 | 0.125 | 0.5 | 0.5 | 4 | 16 | 8 | 2 | 2 | NT | |
| SA099 | REP | 0.06 | 0.5 | 14 | 0.5 | 0.25 | 0.5 | 4 | 8 | 8 | 1 | 0.5 | — |
| MUP | 0.25 | 32 | 11 | 0.125 | 16 | 0.5 | 8 | 2 | 4 | 2 | 0.25 | IRS mutations (G591D, G593D) | |
| FA | 0.5 | 32 | 14 | 0.125 | 0.25 | 32 | 4 | 1 | 4 | 2 | 0.25 | EF-G mutation (R464C) | |
| CEP | 4 | 32 | 6 | 0.125 | 0.5 | 1 | 32 | 4 | 4 | 1 | 0.25 | NT | |
| ERY | 1 | 16 | 14 | 0.125 | 0.25 | 0.5 | 8 | 8 | 4 | 2 | 0.5 | — | |
| LIN | 4 | >32 | 31 | 1 | 0.25 | 0.5 | 4 | 1 | >32 | 2 | 0.5 | — | |
| QD | 0.25 | 2 | 14 | 0.125 | 0.25 | 0.5 | 4 | 8 | 4 | 2 | 2 | NT | |
| SA104 | REP | 0.125 | 1 | 20 | 1 | 0.5 | 0.5 | 32 | 4 | 8 | 1 | 0.5 | L3 mutation (G152D) |
| MUP | 0.5 | 4 | 14 | 0.125 | 2 | 0.5 | 64 | 2 | 4 | 1 | 0.25 | IRS mutation (Q709R) | |
| FA | 0.5 | 32 | 4 | 0.125 | 0.5 | 32 | 32 | 2 | 4 | 1 | 0.125 | EF-G mutation (F437Y) | |
| ERY | 0.5 | >32 | 17 | 0.125 | 0.25 | 0.25 | 64 | >32 | 4 | 1 | 0.25 | — | |
| LIN | 4 | 32 | 23 | 0.25 | 0.25 | 0.5 | 64 | 2 | 32 | 2 | 0.25 | — | |
| QD | 0.25 | 2 | 20 | 0.125 | 0.25 | 0.5 | 4 | 32 | 4 | 1 | 4 | NT | |
| SA138 | REP | 0.06 | 1 | 19 | 0.5 | 0.25 | 1 | >64 | >32 | 8 | 1 | 0.5 | L3 mutation (G152D) |
| REP | 0.06 | 16 | 50 | 16 | NT | NT | NT | NT | NT | NT | NT | L3 mutations (G152D, D159Y) | |
| MUP | 0.25 | 32 | 14 | 0.06 | 32 | 0.5 | 64 | >32 | 4 | 2 | 0.25 | NT | |
| FA | 0.5 | 32 | 6 | 0.06 | 0.25 | 64 | >64 | >32 | 4 | 1 | 0.25 | NT | |
| QD | 0.25 | 2 | 16 | 0.125 | 0.5 | 0.5 | >64 | >32 | 4 | 2 | 1 | NT | |
| SA238 | REP | 0.06 | 0.5 | 20 | 0.5 | 0.25 | 0.5 | 64 | 2 | 4 | 1 | 0.25 | L3 mutation (G144D) |
| MUP | 0.25 | 64 | 4 | 0.125 | 32 | 0.5 | 64 | 2 | 4 | 4 | 0.25 | IRS mutation (V588F) | |
| FA | 0.5 | 32 | 4 | 0.125 | 0.25 | 32 | 64 | 2 | 4 | 2 | 0.25 | EF-G mutation (G452C) | |
| ERY | 0.5 | >64 | 14 | 0.06 | 0.5 | 1 | >64 | >64 | 4 | 2 | 0.5 | L4 mutations (G69A, T70P) | |
| LIN | 4 | >32 | 22 | 0.25 | 0.25 | 0.5 | 64 | 2 | 32 | 2 | 0.25 | — | |
| QD | 0.25 | 2 | 25 | 0.125 | 0.25 | 1 | >64 | 16 | 4 | 2 | 2 | NT | |
| SA248 | REP | 0.06 | 1 | 14 | 2 | 0.25 | 0.5 | >64 | >32 | 8 | 0.5 | 0.5 | L3 mutations (G152D, D159Y) |
| MUP | 0.25 | 8 | 14 | 0.06 | 8 | 1 | 64 | >64 | 4 | 0.5 | 0.25 | NT | |
| FA | 1 | 32 | 5 | 0.125 | 0.25 | 32 | >64 | >32 | 4 | 0.5 | 0.5 | NT | |
| QD | 0.25 | 4 | 14 | 0.25 | 0.5 | 0.5 | >64 | >32 | 8 | 1 | 8 | NT | |
| SA262 | REP | 0.06 | 1 | 16 | 2 | 0.25 | 0.5 | >64 | >32 | 4 | 2 | 1 | L3 mutation (S153Y) |
| MUP | 0.25 | >64 | 9 | 0.125 | >64 | 0.5 | >64 | >32 | 4 | 2 | 1 | NT | |
| FA | 1 | 32 | 4 | 0.125 | 0.25 | 32 | >64 | >32 | 4 | 1 | 1 | NT | |
| LIN | 4 | >32 | 22 | 2 | 0.25 | 0.5 | 64 | >32 | 32 | 2 | 2 | NT | |
| QD | 0.5 | >4 | 14 | 0.5 | 0.25 | 0.5 | >64 | >32 | 8 | 2 | 8 | — | |
| SA505 | REP | 0.06 | 0.5 | 16 | 0.5 | 0.25 | 0.5 | 4 | 1 | 4 | 4 | 0.5 | L3 mutation (G152D) |
| REP | 0.06 | 4 | 50 | 4 | NT | NT | NT | NT | NT | NT | NT | L3 mutations (G152D, D159Y) | |
| MUP | 0.25 | 32 | 11 | 0.125 | 32 | 0.5 | 2 | 2 | 4 | 4 | 0.5 | IRS mutation (I604N) | |
| FA | 1 | 64 | 4 | 0.125 | 0.25 | 64 | 2 | 1 | 4 | 4 | 0.25 | EF-G mutation (G452S) | |
| CEP | 2 | 64 | 18 | 0.125 | 0.5 | 0.5 | 64 | 2 | 2 | 4 | 0.25 | NT | |
| ERY | 0.5 | 64 | 13 | 0.125 | 0.25 | 1 | >64 | 64 | 4 | 2 | 0.5 | — | |
| QD | 0.25 | 2 | 18 | 0.125 | 0.25 | 0.5 | 4 | 4 | 4 | 8 | 1 | NT | |
| SA506 | REP | 0.06 | 0.5 | 15 | 0.5 | 0.5 | 0.5 | >64 | >32 | 2 | 2 | 0.5 | L3 mutation (S158L) |
| MUP | 0.25 | 8 | 14 | 0.06 | 16 | 1 | 64 | >32 | 4 | 8 | 1 | NT | |
| FA | 0.5 | 64 | 4 | 0.125 | 0.25 | 64 | >64 | >32 | 2 | 8 | 0.5 | NT | |
| LIN | 2 | 16 | 46 | 0.5 | 0.25 | 0.25 | 64 | >64 | 16 | 4 | 1 | NT | |
| QD | 0.25 | 2 | 24 | 0.125 | 0.25 | 0.25 | >64 | >32 | 2 | 4 | 2 | NT | |
| SA508 | REP | 0.125 | 2 | 14 | 2 | 0.5 | 8 | 8 | >32 | 2 | 8 | 0.5 | L3 mutation (S158L) |
| MUP | 0.5 | 32 | 12 | 0.125 | 32 | 4 | 8 | >64 | 2 | 4 | 0.25 | NT | |
| FA | 8 | >64 | 4 | 0.25 | 0.5 | >64 | 8 | >32 | 2 | 8 | 0.25 | NT | |
| CEP | 8 | 32 | 4 | 0.125 | 0.5 | 8 | 16 | >32 | 2 | 4 | 0.25 | NT | |
| LIN | 2 | 16 | 45 | 1 | 0.25 | 8 | 4 | >32 | 16 | 4 | 0.5 | NT | |
| QD | 0.25 | 2 | 28 | 0.25 | 1 | 16 | 8 | >32 | 2 | 4 | 2 | NT | |
| SA509 | REP | 0.06 | 2 | 14 | 2 | 32 | 0.5 | >64 | >32 | 4 | 2 | 1 | L3 deletion (153S) and mutation (D159Y) |
| MUP | 32 | >64 | 4 | 0.06 | >64 | 0.5 | >64 | >32 | 4 | >256 | 0.5 | NT | |
| FA | 0.5 | 64 | 4 | 0.06 | 32 | 64 | >64 | >32 | 2 | 2 | 0.5 | NT | |
| LIN | 2 | 16 | 28 | 1 | 32 | 0.5 | >64 | >32 | 32 | 1,024 | 1 | NT | |
| VAN | 2,048 | 2,048 | 7 (no change) | 0.06 | 32 | 0.5 | >64 | >32 | 4 | 1,024 | 0.5 | NT | |
| QD | 0.5 | 4 | 18 | 0.06 | >64 | 1 | >64 | >32 | 4 | 2 | 4 | NT | |
| SA510 | REP | 0.03 | 0.5 | 15 | 0.5 | 0.25 | 0.5 | >64 | >32 | 4 | 64 | 0.5 | — |
| REP | 0.03 | 16 | 50 | 8 | NT | NT | NT | NT | NT | NT | NT | L3 mutation (G155R) | |
| MUP | 0.25 | 16 | 14 | 0.06 | 16 | 0.5 | >64 | >32 | 4 | >64 | 0.5 | NT | |
| FA | 1 | >64 | 4 | 0.06 | 0.125 | >64 | >64 | >32 | 4 | 64 | 0.5 | NT | |
| VAN | 32 | 2,048c | 13 | 0.06 | 0.125 | 0.5 | >64 | >32 | 4 | 1,024 | 0.5 | NT | |
| QD | 0.25 | 4 | 14 | 0.125 | 0.25 | 1 | >64 | >32 | 4 | 2 | 4 | NT | |
Abbreviations: REP, retapamulin; MUP, mupirocin; FA, fusidic acid; CEP, cephalexin; ERY, erythromycin; LIN, linezolid; VAN, vancomycin; and Q/D, quinupristin-dalfopristin.
—, mechanism not detected; NT, not tested.
Increase in MIC of more than fourfold (MIC = 256) obtained after two passages.
The results of multipassage studies with S. pyogenes are presented in Table 2. Retapamulin MICs rose from 0.016 to 0.03 μg/ml (parent) to 0.125 to 0.25 μg/ml (clones) for 3/10 strains after 26 to 48 days, and quinupristin-dalfopristin MICs rose from 0.125 to 0.25 μg/ml (parent) to 2 μg/ml in 38 days for 1 strain. Erythromycin [erm(B)-positive strains excluded] MICs rose from 0.06 to 16 μg/ml to 0.5 to >64 μg/ml for 8/8 strains after 4 to 50 days, and mupirocin MICs rose from 0.06 to 0.25 μg/ml to 1 to >32 μg/ml after 9 to 20 days for 10/10 strains (Table 2). No cross-resistance was observed.
TABLE 2.
Multipassage resistance selection results with S. pyogenes
| Strain | Antibiotica | Initial MIC (μg/ml) | Selected resistance
|
Retest MIC after 10 antibiotic-free subcultures
|
Detected resistance mechanismb | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| MIC | No. of passages | Retapamulin | Quin/Dalfo | Cephalexin | Erythromycin | Linezolid | Mupirocin | Vancomycin | ||||
| 2094 | Retapamulin | 0.016 | 0.125 | 26 | 0.125 | 0.5 | 0.5 | 4 | 1 | 0.25 | 0.5 | — |
| Quin/Dalfo | 0.25 | 2 | 38 | 0.016 | 0.5 | 1 | 8 | 4 | 0.25 | 0.5 | — | |
| Erythromycin | 4 | >64 | 4 | 0.03 | 0.5 | 1 | 16 | 2 | 0.25 | 0.5 | NT | |
| Mupirocin | 0.25 | 32 | 12 | 0.016 | 0.25 | 1 | 4 | 2 | 16 | 0.5 | — | |
| 2042 | Erythromycin | 4 | 32 | 4 | 0.03 | 0.125 | 1 | 16 | 1 | 0.125 | 0.5 | NT |
| Mupirocin | 0.125 | >32 | 9 | 0.03 | 0.125 | 1 | 8 | 1 | >32 | 0.5 | — | |
| 2011 | Erythromycin | 16 | >64 | 33 | 0.03 | 0.125 | 0.5 | >64 | 1 | 0.125 | 0.5 | NT |
| Mupirocin | 0.125 | 2 | 14 | 0.03 | 0.125 | 0.5 | 16 | 1 | 2 | 0.5 | — | |
| 1714 | Retapamulin | 0.03 | 0.25 | 44 | 0.125 | 0.25 | 0.5 | 16 | 2 | 0.25 | 0.5 | — |
| Erythromycin | 8 | 64 | 7 | 0.03 | 0.125 | 0.5 | 16 | 2 | 0.25 | 0.5 | NT | |
| Mupirocin | 0.25 | >32 | 14 | 0.03 | 0.125 | 0.5 | 16 | 2 | >32 | 0.5 | — | |
| 2393 | Erythromycin | 16 | >64 | 33 | 0.03 | 0.125 | 0.5 | 16 | 1 | 0.06 | 0.5 | NT |
| Mupirocin | 0.06 | 1 | 14 | 0.03 | 0.125 | 0.5 | 16 | 2 | 0.5 | 0.5 | — | |
| 2132 | Erythromycin | 0.06 | 0.5 | 24 | 0.03 | 0.125 | 0.5 | 0.5 | 1 | 0.125 | 0.5 | — |
| Mupirocin | 0.06 | 4 | 14 | 0.016 | 0.125 | 0.5 | 0.06 | 0.5 | 4 | 0.5 | — | |
| 2022 | Erythromycin | 0.125 | 1 | 50 | 0.03 | 0.125 | 0.5 | 1 | 2 | 0.125 | 0.5 | NT |
| Mupirocin | 0.25 | >2 | 20 | 0.016 | 0.125 | 0.5 | 0.125 | 1 | 2 | 0.5 | — | |
| 237 | Erythromycin | 1 | 8 | 50 | 0.03 | 0.5 | 0.5 | 8 | 2 | 0.125 | 0.5 | — |
| Mupirocin | 0.25 | 32 | 13 | 0.03 | 0.25 | 1 | 1 | 2 | 16 | 0.5 | — | |
| 2368 | Mupirocin | 0.06 | 1 | 14 | 0.016 | 0.125 | 0.5 | >64 | 1 | 0.5 | 0.5 | — |
| 2620 | Retapamulin | 0.016 | 0.125 | 48 | 0.125 | 0.125 | 0.5 | >64 | 1 | 0.125 | 0.5 | L3 mutation (N149K) |
| Mupirocin | 0.06 | 1 | 14 | 0.016 | 0.125 | 0.5 | >64 | 1 | 0.5 | 0.5 | — | |
Quin/Dalfo, quinupristin-dalfopristin.
—, mechanism not detected; NT, mechanisms not tested.
Pulsed-field gel electrophoresis confirmed that all selected strains were identical or closely related.
Changes in the L3 protein occurred in 10/12 S. aureus strains and also in strains SA138, SA505, and SA510 after prolonged selection for 50 days. Five strains had double mutations in L3, with retapamulin MICs of 1 to 16 μg/ml, and eight strains had single substitutions, with retapamulin MICs ranging from 0.5 to 16 μg/ml (Table 1). Of three S. pyogenes clones with raised retapamulin MICs of 0.125 to 0.5 μg/ml, one strain had an altered L3 protein (Table 2). Among selected macrolide-resistant S. aureus strains, two strains had double alterations in the L4 protein, with MICs raised from 1 to 32 and 0.5 to >64 μg/ml. In the other three S. aureus and two S. pyogenes macrolide-resistant strains, no changes in the L4 or L22 protein or 23S rRNA were observed (Tables 1 and 2). In five fusidic acid-resistant S. aureus clones, two had changes in the EF-G protein associated with MIC increases from 1 to 64 and 0.5 to 32 μg/ml (Table 1). No strain had fusB. Five mupirocin-resistant S. aureus clones had changes in the IRS protein, and no changes were observed in S. pyogenes IRS (Tables 1 and 2).
The results of single-passage studies with S. aureus (4× MIC and 8× MIC) can be seen in Table 3. Resistance frequencies ranging from 2× MIC to 8× MIC in S. aureus were as follows: for retapamulin, 6.7 × 10−5 to <1.0 × 10−9; for mupirocin, 1.0 × 10−5 to 6.7 × 10−10; for fusidic acid, >1.5 × 10−4 to 1.2 × 10−6; for cephalexin, 4.0 × 10−6 to 3.0 × 10−8; for erythromycin, 2.2 × 10−6 to <2.5 × 10−9; for linezolid, 2.5 × 10−5 to <1.1 × 10−9; for vancomycin, <1.0 × 10−6 to <1.0 × 10−9; and for quinupristin-dalfopristin, 7.5 × 10−4 to <1.0 × 10−9.
TABLE 3.
Single-step-passage mutation frequencies for retapamulin and comparators in 12 S. aureus strains
| Selecting drug | No. of strains tested | MIC range (μg/ml) | Range of spontaneous mutation frequencies at:
|
|
|---|---|---|---|---|
| 4× MIC | 8× MIC | |||
| Retapamulin | 12 | 0.03-0.25 | 5.0 × 10−6-<1.0 × 10−9 | <5.0 × 10−8-<1.0 × 10−9 |
| Cephalexin | 3 | 2-4 | 1.3 × 10−6-2.0 × 10−7 | 1.3 × 10−6-3.0 × 10−8 |
| Erythromycin | 5 | 0.5-1 | 2.2 × 10−6-4.4 × 10−7 | 2.2 × 10−6-<2.5 × 10−9 |
| Fusidic acid | 12 | 2-8 | >1.5 × 10−4-2.6 × 10−6 | 7.5 × 10−5-1.2 × 10−6 |
| Linezolid | 12 | 2-4 | 3.9 × 10−7-<1.1 × 10−9 | <3.3 × 10−9-<1.1 × 10−9 |
| Mupirocin | 11 | 0.25-0.5 | 1.3 × 10−6-6.7 × 10−9 | 1.2 × 10−6-6.7 × 10−10 |
| Quinupristin-dalfopristin | 12 | 0.25-0.5 | 2.2 × 10−6-<1.4 × 10−9 | 6.0 × 10−7-<1.0 × 10−9 |
| Vancomycin | 10 | 1-8 | <1.0 × 10−6-<1.0 × 10−9 | <1.0 × 10−6-<1.0 × 10−9 |
In single-step passage studies with S. pyogenes (Table 4), single-step S. pyogenes mutation frequencies at concentrations from 1× MIC to 8× MIC were as follows: for retapamulin, 3.3 × 10−4 to <1.7 × 10−10; for mupirocin, 7.0 × 10−5 to <1.2 × 10−10; for cephalexin, 2.5 × 10−7 to <3.3 × 10−10; for erythromycin, <1.2 × 10−4 to <2.9 × 10−10; for linezolid, <1.4 × 10−9 to <3.3 × 10−10; for vancomycin, <1.7 × 10−5 to <1.4 × 10−10; and for quinupristin-dalfopristin, <3.3 × 10−5 to <2.5 × 10−10.
TABLE 4.
Single-step-passage mutation frequencies for retapamulin and comparators in 10 S. pyogenes strains
| Selecting drug | No. of strains tested | MIC range (μg/ml) | Range of spontaneous mutation frequencies at:
|
|
|---|---|---|---|---|
| 4× MIC | 8× MIC | |||
| Retapamulin | 10 | 0.016-0.03 | <8.3 × 10−10-<1.7 × 10−10 | <8.3 × 10−10-<1.7 × 10−10 |
| Cephalexin | 10 | 0.5-1 | <1.2 × 10−9-<3.3 × 10−10 | <1.2 × 10−9-<3.3 × 10−10 |
| Erythromycin | 8 | 0.06-16 | <6.7 × 10−5-<7.7 × 10−10 | <1.2 × 10−8-<2.9 × 10−10 |
| Linezolid | 10 | 1-2 | <1.4 × 10−9-<3.3 × 10−10 | <1.4 × 10−9-<3.3 × 10−10 |
| Mupirocin | 10 | 0.06-0.25 | 1.5 × 10−6-<1.0 × 10−9 | 1.0 × 10−6-<1.2 × 10−10 |
| Quinupristin-dalfopristin | 10 | 0.125-0.25 | <3.3 × 10−9-<2.5 × 10−10 | <3.3 × 10−9-<2.5 × 10−10 |
| Vancomycin | 10 | 0.5-1 | <3.3 × 10−9-<1.4 × 10−10 | <2.0 × 10−9-<1.4 × 10−10 |
Of eight selected single-step-passaged S. aureus clones tested for L3 alterations, two had substitutions, either S158L or S161Y. No alteration in L3 protein was observed in seven randomly selected S. pyogenes strains.
Retapamulin had a lower frequency of spontaneous resistance against S. aureus than all other drugs tested except linezolid. For S. pyogenes, retapamulin had the lowest single-step resistance frequency compared to the other compounds. In our studies, retapamulin had the lowest MICs by multipassage for S. aureus and S. pyogenes. Although clones with increased retapamulin MICs were obtained with all 12 S. aureus strains, the highest retapamulin MIC was only ≤2 μg/ml. While no genetic evidence could be found, cross-resistance between linezolid-, quinupristin-dalfopristin-, and erythromycin-resistant clones and clones with raised retapamulin MICs may represent the ribosomal targeting of all four drugs, albeit at different target sites (8).
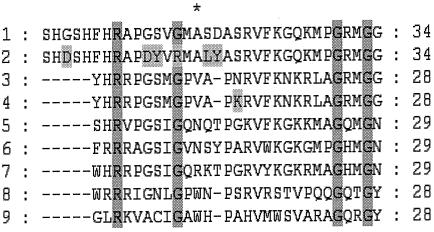
Previous investigations (2, 9) have revealed that pleuromutilin resistance develops in a slow, stepwise manner associated with a change of Asn to Asp at position 149 in ribosomal protein L3 (Escherichia coli numbering). Our study revealed few mutations which affected retapamulin susceptibility, and these mutations ap-peared in a very conservative region whose amino acid residues are very well preserved in different organisms (Fig. 2). S. aureus multipassage mutants had double and single amino acid substitutions or no alterations in the L3 protein (Table 1). Double and single mutations were associated with MICs of 1 to 2 μg/ml and 0.5 to 2 μg/ml, respectively. Three clones selected for prolonged selection for 50 days (parent strains SA138, SA505, and SA510) yielded mutants with retapamulin MICs ranging from 4 to 16 μg/ml, each with an additional mutation in L3 (Table 1). This suggests that resistance development in retapamulin is a slow, multistep process and that mutations accumulate gradually in the presence of drug pressure, similar to the case for tiamulin (2). Kosowska and coworkers also observed that prolonged selection led to high rates of resistance development for linezolid, quinupristin-dalfopristin, and telithromycin (6). It is unknown how the other comparators in this study would perform if subjected to similar prolonged selection. Only one strain of three multipassage S. pyogenes clones had an amino acid substitution in L3 (Table 2).
FIG. 2.
Mutations found in S. aureus and S. pyogenes multi- and single-passage mutants with reduced susceptibilities to retapamulin. The figures shows an alignment of various ribosomal protein L3 sequences in the regions flanking the mutations. The positions of the characterized mutations in S. aureus and S. pyogenes mutants are highlighted in a shade of gray; position 149 in E. coli and analogous positions in other sequences crucial for developing resistance are indicated with an asterisk; and positions of amino acid identity are highlighted in dark gray. Sequences: 1, parental S. aureus strain starting from amino acid position 142; 2, selected S. aureus mutant starting from position 142; 3, parental S. pyogenes strain starting from position 137; 4, selected S. pyogenes mutant starting from position 137; 5, E. coli starting from position 139; 6, Brachyspira hyodysenteriae and Brachyspira pilosicoli starting from position 139; 7, Deinococcus radiodurans starting from position 134; 8, Haloarcula marismortui starting from position 232; and 9, Saccharomyces cerevisiae starting from position 245.
Mechanisms of resistance for macrolides and fusidic acid (Tables 1 and 2) have been described before. For mupirocin, the new mutations G591D, G593D, and I604N are within the essential binding site, but the significance of the Q709R mutation is unclear (Table 1).
Our results suggest that retapamulin has a low potential for resistance development which is less than or comparable to that of mupirocin and fusidic acid, two topical agents commonly used for the treatment of uncomplicated S. aureus and S. pyogenes skin and soft tissue infections. This hypothesis requires validation by experimental and clinical testing.
Acknowledgments
We thank NARSA via Focus Technologies (Herndon, VA) for provision of the Michigan VRSA and VISA strains.
This study was supported by a grant from GlaxoSmithKline Pharmaceuticals, Collegeville, Pa.
REFERENCES
- 1.Antonio, M., N. McFerran, and M. J. Pallen. 2002. Mutations affecting the Rossman fold of isoleucyl-tRNA synthetase are correlated with low-level mupirocin resistance in Staphylococcus aureus. Antimicrob. Agents Chemother. 46:438-442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Böck, A., F. Turnowsky, and G. Högenauer. 1982. Tiamulin resistance mutations in Escherichia coli. J. Bacteriol. 151:1253-1260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bogdanovich, T., L. M. Ednie, S. Shapiro, and P. C. Appelbaum. 2005. Antistaphylococcal activity of ceftobiprole, a new broad-spectrum cephalosporin. Antimicrob. Agents Chemother. 49:4210-4219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bozdogan, B., L. M. Ednie, K. Credito, K. Kosowska, and P. C. Appelbaum. 2004. Derivatives of a vancomycin-resistant Staphylococcus aureus strain isolated at Hershey Medical Center. Antimicrob. Agents Chemother. 12:4762-4765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hunt, E. 2000. Pleuromutilin antibiotics. Drugs Future 25:1163-1168. [Google Scholar]
- 6.Kosowska, K., D. B. Hoellman, G. Lin, C. Clark, K. Credito, P. McGhee, B. Dewasse, B. Bozdogan, S. Shapiro, and P. C. Appelbaum. 2005. Antipneumococcal activity of ceftobiprole, a novel broad-spectrum cephalosporin. Antimicrob. Agents Chemother. 49:1932-1942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.National Committee for Clinical Laboratory Standards. 2003. Methods for dilution antimicrobial susceptibility tests for bacteria that grow aerobically, 6th ed. Approved standard M7-A6. National Committee for Clinical Laboratory Standards, Wayne, Pa.
- 8.O'Neill, A. J., A. R. Larsen, A. S. Henriksen, and I. A. Chopra. 2004. A fusidic acid-resistant epidemic strain of Staphylococcus aureus carries the fusB determinant, whereas fusA mutations are prevalent in other resistant isolates. Antimicrob. Agents Chemother. 48:3594-3597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Pringle, M., J. Poehlsgaard, B. Vester, and K. S. Long. 2004. Mutations in ribosomal protein L3 and 23S ribosomal RNA at the peptidyl transferase centre are associated with reduced susceptibility to tiamulin in Brachyspira spp. isolates. Mol. Microbiol. 54:1295-1306. [DOI] [PubMed] [Google Scholar]
- 10.Prunier, A. L., H. N. Trong, D. Tande, C. Segond, and R. Leclercq. 2005. Mutation of L4 ribosomal protein conferring unusual macrolide resistance in two independent clinical isolates of Staphylococcus aureus. Microb. Drug Resist. 11:18-20. [DOI] [PubMed] [Google Scholar]
- 11.Tait-Kamradt, A., T. Davies, P. C. Appelbaum, F. Depardieu, P. Courvalin, J. Petitpas, L. Wondrack, A. Walker, M. R. Jacobs, and J. Sutcliffe. 2000. Two new mechanisms of macrolide resistance in clinical strains of Streptococcus pneumoniae from Eastern Europe and North America. Antimicrob. Agents Chemother. 44:3395-3401. [DOI] [PMC free article] [PubMed] [Google Scholar]