Abstract
Nipah virus (NiV), a member of the Paramyxoviridae family, causes a zoonotic infection in which the reservoir, the fruit bat, may pass the infection to pigs and eventually to humans. In humans, the infection leads to encephalitis with >40 to 70% mortality. We have previously shown that polyclonal antibody directed to either one of two glycoproteins, G (attachment protein) or F (fusion protein), can protect hamsters from a lethal infection. In the present study, we have developed monoclonal antibodies (MAbs) to both glycoproteins and assessed their ability to protect animals against lethal NiV infection. We show that as little as 1.2 μg of an anti-G MAb protected animals, whereas more than 1.8 μg of anti-F MAb was required to completely protect the hamsters. High levels of either anti-G or anti-F MAbs gave a sterilizing immunity, whereas lower levels could protect against a fatal infection but resulted in an increase in anti-NiV antibodies starting 18 days after the viral challenge. Using reverse transcriptase PCR, the presence of NiV in the different organs could not be observed in MAb-protected animals. When the MAbs were given after infection, partial protection (50%) was observed with the anti-G MAbs when the animals were inoculated up to 24 h after infection, but administration of the anti-F MAbs protected some animals (25 to 50%) inoculated later during the infection. Our studies suggest that immunotherapy could be used for people who are exposed to NiV infections.
A consequence of recent ecological changes, such as deforestation, has been the zoonotic transmission of pathogens from their natural reservoir to humans and domestic livestock. In jumping from one species to another, zoonoses often become more pathogenic (2), and although the newly emerged pathogen may cause only limited outbreaks in its new host, if transmission is efficient, a global epidemic may ensue (13). Strategies of prevention (vaccination) and treatment for such zoonoses have thus become a priority. The development of vaccines is extremely expensive, and it may be difficult to convince populations to be vaccinated against a potentially dangerous pathogen that has made little impact globally. An alternative approach is the utilization of passive immunity. This has been used in the treatment and prevention of a number of diseases for more than a century (1) and with the recent advances in biotechnology may be a more appropriate strategy for particular emergent pathogens.
Nipah virus (NiV), a member of the Paramyxovirus genus, was first identified in an epidemic in pigs and humans in Malaysia in 1998 (4). It was shown to be closely related to Hendra virus, which was first isolated in Australia in 1994 (17). As these two viruses are distinct from previously characterized paramyxoviruses, it has been proposed that they be grouped in the henipavirus family (10, 21, 22, 26). The reservoir or natural host of NiV is thought to be the fruit bat (5, 25), and pigs are probably infected by fruit contaminated by the bats. Infection in pigs is both respiratory and neurological (11, 15). Humans infected by contact with these infected animals suffer from a severe, rapidly progressive encephalitis with a high mortality rate (24). Nipah virus could be detected in a number of organs, including the brain, where virus antigen was observed in the neurons.
Evidence of NiV in other Asian countries has been shown by serological studies in Cambodia (18), and this has been confirmed by NiV isolation from fruit bats in Cambodia (19). Thus, the virus is widespread in Asia in areas where this species of fruit bat is found. Since 2001, an increasing number of NiV cases in humans in Bangladesh have been identified, although the pig has not been shown to be the intermediate host. There is some evidence of transmission between family members (12). Thus, NiV infections are much more widespread than previously recognized and so it is necessary to reevaluate strategies to prevent or treat this disease. We have recently shown that immunization with either one of the NiV glycoproteins (G [attachment protein] or F [fusion protein]) protects hamsters from a fatal infection (9). Further, passive administration of serum against either the G or F glycoprotein also protected the animals from a lethal challenge. To develop a strategy for prevention or treatment of NiV infections, we developed a bank of monoclonal antibodies (MAbs) directed against the two NiV glycoproteins. On the basis of their in vitro neutralizing activity, we selected MAbs to be tested in a hamster model. In the present study we show that the selected MAbs can protect hamsters from a lethal infection. Further, the MAbs may be given for up to 4 days after infection and still protect the animals.
MATERIALS AND METHODS
Cells and viruses.
Vero-E6, BHK21, and HeLa cells were maintained in Dulbecco's modified Eagle's medium (DMEM) (GIBCO BRL) containing 10% fetal calf serum (FCS) (GIBCO BRL), l-glutamine, penicillin, streptomycin, and HEPES. Sp2o/Ag14 cells were maintained in RPMI glutamax I (GIBCO BRL) supplemented with 10% FCS, nonessential amino acids, penicillin, streptomycin, and HEPES.
NiV is classified as a class 4 agent, and all virus manipulations were carried out in the biosafety level 4 (BSL-4) laboratory of Jean Mérieux in Lyon, France. NiV isolated from the cerebrospinal fluid of a patient was a generous gift from Kaw Bing Chua (University of Malaya, Kuala Lumpur, Malaysia). Virus stocks were prepared in the BSL-4 laboratory by infecting Vero-E6 cells with a multiplicity of infection of 0.01 PFU per cell, and virus was recovered 48 h postinfection, aliquoted, and stored at −80°C. The virus stock was made following the fourth passage on Vero cells after the first virus isolation. The virus titer, measured by six-well plaque assay as previously described (9), was 2 × 106 PFU/ml.
Stocks of vaccinia virus and recombinant viruses were grown in BHK21 cells. Cells were infected at 0.01 PFU per cell, and the cells were harvested 3 days later, sonicated, and stored at −80°C. Virus was titrated in Vero cells.
Preparation and characterization of anti-NiV hybridomas.
Six-week-old female BALB/c (H-2d) mice purchased from IFFA-Credo (Domaine des Oncins, France) were first immunized twice (1 month apart) with plasmid DNA pV1J-NiV.G or pV1J-NiV.F (1.5 μg plasmid) by gene gun immunization into the shaved abdominal epidermis of the mice with a Helio gene gun system (Bio-Rad, Ivry sur Seine, France) at a helium pressure setting of 300 lb/in2. Three months later, mice were immunized with vaccinia virus recombinants expressing the corresponding G or F Nipah virus glycoprotein by intraperitoneal inoculation. After a further 3 months and 3 days prior to the fusion step, the mice were inoculated intraperitoneally on three consecutive days with irradiated NiV-infected Vero cells (100 μg for each inoculation). The day after the last immunization, spleen cells of mice were taken and fused with myeloid cells Sp2o/Ag14 using standard procedures.
Hybridomas secreting NiV-specific antibodies were selected by enzyme-linked immunosorbent assay (ELISA) using NiV-infected Vero cell extracts. The specificity (G or F NiV glycoproteins) of antibodies was verified by FACScan analysis (Becton Dickinson) against HeLa cells expressing G or F Nipah virus glycoprotein.
Ascitic fluid was produced in BALB/c mice. The concentration and isotype of anti-NiV monoclonal antibodies in ascitic fluid samples were measured and determined by ELISA using mouse immunoglobulin standards (Clonotyping System-AP; Southern Biotechnology Associates, Inc., Birmingham, Ala.). Neutralizing activities of anti-Nipah virus antibodies were measured by a virus neutralization assay.
Infection of hamsters.
Seven- to 8-week-old golden hamsters (Mesocritus auratus) were infected by intraperitoneal injection of NiV after anesthetization with isoflurane (Aerrane; Baxter S.A.). The dose inoculated was 100 50% lethal doses (LD50) (750 PFU). The LD50 was previously determined with the same NiV stock. The NiV dose causing mortality of 50% of the hamsters was calculated on the basis of the method of Reed and Muench (18a). The animals were housed in ventilated containers equipped with HEPA filters in the BSL-4 laboratory, and animals were individually identified by using microchips.
Passive antibody transfer.
To observe the potential prophylaxis of the anti-NiV MAbs, hamsters were inoculated with the indicated amounts of ascitic fluid samples by intraperitoneal injection 1 day prior to and 1 hour after inoculation with 100 LD50 of NiV. In studies to determine the protection after infection, a single dose of MAbs was inoculated 1 hour and 1, 2, 3, or 4 days after infection.
Study of NiV infection in hamsters.
For each experiment, infected hamsters were observed for clinical signs (prostration, neurological signs) and variations in temperature (microchip) and weight until the end of the study. Blood samples were taken regularly from each animal by eye puncture after anesthetization with isoflurane, and the sera were frozen at −80°C until testing by ELISA and virus neutralization.
Tissue specimens, including blood, brain, lung, heart, liver, spleen, and kidney specimens, were collected from terminally ill hamsters or hamsters at specific times after infection. Tissues were frozen at −80°C for reverse transcriptase PCR (RT-PCR) analysis. A small fragment of tissue was mechanically crushed (Minibeadbeater; Biospec, Bartlesville, OK) for 7 min in a 2-ml tube containing 0.3 ml of sterile glass beads and 0.5 ml of lysis buffer RLT-β-mercaptoethanol from an RNeasy mini kit (QIAGEN, Inc., Valencia, CA). RNA from tissues was then extracted using this kit following the manufacturer's instructions. The extracts were resuspended in 50-μl samples of RNase-free water, aliquoted, and stored at −80°C before RT-PCR amplification was carried out.
Virus neutralization assays.
NiV-specific neutralizing antibodies were assayed using twofold dilutions of ascitic fluid samples or antisera. Diluted antisera or ascitic fluid samples were incubated with virus (25 PFU/well in 96-well microtiter plates) for 60 min at 37°C in Dulbecco's modified Eagle's medium supplemented with 2% FCS. A total of 2.5 × 104 Vero cells were then added to each well as indicator cells, and the 96-well microtiter plates were incubated for 4 to 6 days at 37°C. Neutralizing titers are defined as the reciprocal dilution of sera or ascitic fluid samples that completely inhibited the cytopathic effect.
ELISA.
Microtiter plates (96-well plates) (Dominic Dutscher) were coated with 100 μl/well NiV antigen or with 100 μl of diluted NiV N protein produced in a baculovirus system and incubated overnight at 4°C. Wells were blocked by incubation with 3% skim milk in phosphate-buffered saline (PBS) for 30 min at 37°C (200 μl per well). Between each step, the wells were washed three times with PBS containing 0.05% Tween 20. The bound antibodies were detected after incubation with the appropriate anti-mouse immunoglobulin G (IgG) γ-specific (Sigma-Aldrich, France) or anti-hamster IgG-specific (Sigma-Aldrich, France) antibodies conjugated to peroxidase for 30 min at 37°C. The ELISA products were developed by using OPD (o-phenylenediamine dihydrochloride) (Sigma-Aldrich, France) peroxidase substrate and stopped with HCl. The optical density was read at 492 nm.
RT-PCR.
RT-PCR was conducted in one step by using high-fidelity PCR enzyme blend (Roche Applied Science, Germany) following the manufacturer's instructions. Amplified sequences and oligonucleotide primers used were a nucleoprotein (NP) gene fragment (105 bp) with the forward primer Ni-NP1209 (5′-GCAAGAGAGTAATGTTCAGGCTAGAG-3′) and the reverse primer Ni-NP1314 (5′-CTGTTCTATAGGTTCTTCCCCTTCAT-3′) previously described (9). NP gene fragments were amplified for the detection of NiV in hamster tissue samples.
RESULTS
Selection of anti-NiV MAbs.
We prepared a bank of MAbs directed against the NiV G and F glycoproteins and subsequently characterized them so as to select a number of MAbs to test as potential prophylactic and therapeutic agents. They were initially evaluated for their in vitro neutralizing activities to both Nipah and Hendra viruses. The anti-G MAbs neutralized only NiV, whereas some anti-F MAbs neutralized both viruses. A full description of these MAbs will be described elsewhere. Four MAbs, two anti-G MAbs (Nip GIP 1.7 and Nip 3B10) and two anti-F MAbs (Nip GIP 35 and Nip GIP 3), were selected for their high neutralizing activities in vitro and were used for the study in passive protection experiments. The properties of these four MAbs are summarized in Table 1.
TABLE 1.
Properties of the four MAbs selected for study in the passive protection studies
| MAb | Specificity | Isotype | Neutralization activitya
|
|
|---|---|---|---|---|
| Nipah virus | Hendra virus | |||
| Nip GIP 1.7 | G | IgG1 | 0.27 | |
| Nip 3B10 | G | IgG1 | 0.9 | |
| Nip GIP 35 | F | IgG1 | 14 | 5.6 |
| Nip GIP 3 | F | IgG2a | 20 | 1.6 |
Neutralizing titers are expressed as the amount of IgG MAbs (in nanograms) required to completely neutralize 25 PFU of NiV.
Passive protection with NiV anti-G or anti-F MAbs.
To assess the potential prophylactic activity of the anti-F or anti-G MAbs against NiV infection, groups of eight animals, 7- to 8 week-old golden hamsters (Mesocricetus auratus), were inoculated with 200 μl of one of the selected MAbs 24 h prior to and 1 h after an intraperitoneal lethal challenge of NiV (100 LD50). The quantities of MAbs given at each injection were 112 μg of Nip GIP 1.7, 100 μg of Nip 3B10, 180 μg of Nip GIP 35, and 520 μg of Nip GIP 3. MAbs were also inoculated into uninfected hamsters to check for toxicity and measure the half-lives of the antibodies.
The hamsters were checked daily for up to 65 days. The results (Table 2) show that passive administration of anti-G or anti-F MAbs protected all hamsters from death except for two hamsters receiving the anti-F MAb Nip GIP 3 that died on day 31. Control hamsters not receiving MAbs died 8 days after infection with the exception of one that died, later, on day 17.
TABLE 2.
Passive protection studies in hamsters (eight animals per group) by anti-NiV MAbs injected 24 h prior to and 1 h after a lethal challenge of NiV
| MAb | Quantity of MAb administered (μg) | % of surviving animals | Mean time of death (days) |
|---|---|---|---|
| None (control) | 0 | 9.5 | |
| Anti-NiV.G | |||
| Nip GIP 1.7 | 112 | 100 | |
| Nip 3B10 | 100 | 100 | |
| Anti-NiV.F | |||
| Nip GIP 35 | 180 | 100 | |
| Nip GIP 3 | 520 | 75 | 31 |
After infection, animals were monitored for a number of parameters, and some were sacrificed 4 or 5 days after infection to measure the level of virus replication in the different organs. The control hamsters receiving no MAbs underwent a weight loss of 10 to 20% 2 days before their death and a reduction of temperature just before their death (24 h or less). In contrast, no weight loss or temperature variation occurred in the protected hamsters.
Two animals in each group were sacrificed, one at day 4 and the other at day 5 after infection, to study by RT-PCR analysis the presence of NiV RNA in organs. No viral RNA was detected in the different organs of MAb-protected animals, except in urine samples of hamsters that received anti-G MAbs (animals sampled at day 4 after infection [data not shown]). In contrast, NiV RNA was detected in spleen, kidney, lung, and urine samples of control animals 4 days after infection and additionally in heart, liver, and brain samples 1 day later (data not shown). Moribund hamsters from the nonprotected control group at day 7 were euthanized and autopsied when severe signs of disease appeared. Their organs were analyzed for the presence of virus RNA. NiV RNA was found in all organs tested.
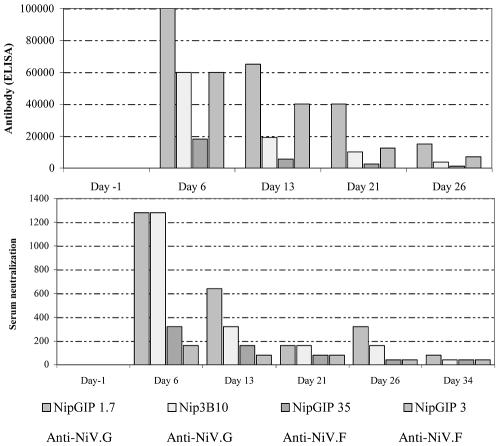
Sera taken from the hamsters during the course of the study were examined for anti-NiV antibodies by both neutralization assay and ELISA. The levels of serum anti-NiV antibodies, whether measured by neutralization assay or by ELISA using virus-infected cells, decreased with time (Fig. 1). The half-lives of the MAbs were calculated to be 10 to 13 days. Further, ELISAs using NiV NP as substrate (data not shown) failed to detect NiV antibodies during the course of the challenge with NiV, thus confirming that in the presence of the passively administered MAbs, the virus did not induce an immune response.
FIG. 1.
Anti-G (Nip GIP 1.7 and Nip 3B10) and anti-F (Nip GIP 35 and Nip GIP 3) NiV MAbs were passively administered to hamsters that were subsequently challenged with 100 LD50 of NiV. The anti-NiV serum antibody levels of the animals were measured by ELISA and neutralization assay.
Administration of large quantities of anti-NiV G (anti-NiV.G) or anti-NiV.F MAbs, 24 h before and 1 h after the infection, protected hamsters against a lethal challenge of NiV. The protection induced in this case seems to be sterilizing, as neither neutralizing nor ELISA detectable antibodies were found once the MAbs had been eliminated.
Titration of the protective levels of the anti-G and anti-F MAbs in vivo.
In order to determine the relative protection efficiencies of the different MAbs, dilutions of the anti-G (Nip GIP 1.7) and anti-F (Nip GIP 35) MAbs were administered to hamsters (four animals per group) by the same protocol as in the first experiment, i.e., 24 h prior to and 1 hour after lethal challenge with NiV (100 LD50). Our studies showed that 1.12 μg of Nip GIP 1.7 was sufficient to completely protect the animals from disease, whereas only two out of four animals were protected with 1.8 μg of the anti-F Nip GIP 35 MAb (Table 3).
TABLE 3.
Titration of the in vivo protection of anti-NiV MAbsa
| MAb | Quantity of MAb administered (μg) | % of surviving animals | Mean time of death (days) |
|---|---|---|---|
| None (control) | 0 | 7.5 | |
| Nip GIP 1.7 (anti-NiV.G) | 112 | 100 | |
| 1.12 | 100 | ||
| 0.12 | 25 | 10.5 | |
| 0.012 | 25 | 12.5 | |
| 0.0012 | 25 | 9.5 | |
| Nip GIP 35 (anti-NiV.F) | 180 | 100 | |
| 1.8 | 50 | 11.5 | |
| 0.18 | 0 | 7.75 | |
| 0.0.18 | 0 | 6.75 | |
| 0.0018 | 0 | 6.75 |
Hamsters (four animals per group) were given dilutions of MAbs 24 h prior to and 1 h after receiving a lethal challenge of NiV.
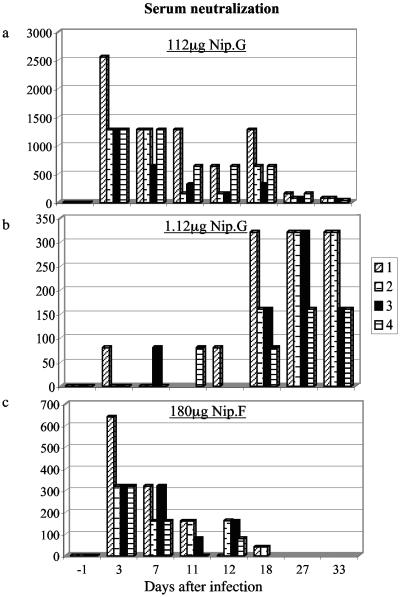
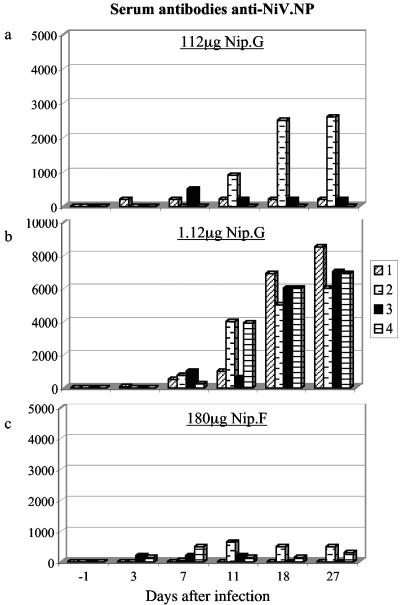
Analysis of the serum neutralizing antibody levels of the hamsters (Fig. 2) showed that those receiving 112 μg of Nip GIP 1.7 or 180 μg of Nip GIP 35 showed a gradual decrease in antibody levels corresponding to the half-life of the MAb. No subsequent increase in neutralizing antibody levels that would therefore correspond to sterilizing immunity was observed. In contrast, animals receiving 1.12 μg of MAb GIP 1.7 (Fig. 2b) had increasing levels of neutralizing antibodies 18 days after the infection, although they were protected against the lethal infection and clinical manifestations. On the basis of these results, it seems that 112 μg of Nip GIP 1.7 and 180 μg of Nip GIP 35 gave a sterilizing immunity, whereas at 1.2 μg or less of Nip GIP 1.7, the MAbs induce a protective immunity but allowed virus replication (Fig. 2). To confirm that this was due to virus replication, the sera were analyzed for NiV.NP antibodies by ELISA (Fig. 3). These results confirmed that virus replication had occurred at the lower MAb concentrations.
FIG. 2.
Passive administration of different protective levels of anti-G (Nip GIP 1.7) or anti-F MAbs in hamsters. The serum antibodies were analyzed in a neutralization assay. Four hamsters were given 112 μg anti-G MAb (a), 1.12 μg anti-G MAb (b), or 180 μg anti-F MAb (c); each bar represents the value for one hamster.
FIG. 3.
Passive administration of different protective levels of anti-G (Nip GIP 1.7) or anti-F MAbs in hamsters. The serum antibodies were analyzed in an ELISA test using NiV NP. Four hamsters were given 112 μg anti-G MAb (a), 1.12 μg anti-G MAb (b), or 180 μg anti-F MAb (c); each bar represents the value for one hamster.
Hamsters were euthanized at the end of the study (36 days), and the different organs were examined for the presence of viral RNA by RT-PCR. In no case was RNA detected, confirming that protection by immunotherapy apparently did not lead to the persistence of the virus (Table 4).
TABLE 4.
Detection of NiV RNA by RT-PCR in different organs of infected hamsters that had received different amounts of anti-G or anti-F NiV MAbsa
| Tested organ or sample | Detection of NiV RNA with the following MAb at the indicated day after infectionb
|
||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| No MAb (control)
|
Nip GIP 1.7 (anti-NiV.G MAb)
|
Nip GIP 35 (anti-NiV.F MAb)
|
|||||||||||||||||
| 112 μg | 1.12 μg | 0.112 μg
|
0.0112 μg
|
0.00112 μg
|
180 μg
|
1.8 μg
|
0.18 μg
|
0.018 μg
|
0.0018 μg
|
||||||||||
| D6 | D7 | D36 | D36 | D11 | D36 | D11 | D36 | D7 | D36 | D36 | D11 | D36 | D7 | D8 | D7 | D13 | D6 | D8 | |
| Organs | |||||||||||||||||||
| Brain | + | + | − | − | + | − | + | − | + | − | − | + | − | + | + | + | + | + | + |
| Heart | + | + | − | − | − | − | − | − | + | − | − | + | − | + | + | + | + | + | + |
| Liver | + | + | − | − | − | − | + | − | + | − | − | + | − | + | + | + | + | + | + |
| Lung | + | + | − | − | − | − | + | − | + | − | − | + | − | + | + | + | + | + | + |
| Spleen | + | + | − | − | − | − | + | − | + | − | − | + | − | + | + | + | + | + | + |
| Kidney | + | + | − | − | + | − | + | − | + | − | − | + | − | + | + | + | + | + | + |
| Urine samples | + | + | − | − | − | − | − | − | + | − | − | + | − | + | + | + | + | + | + |
Hamsters protected by the MAbs were tested 36 days after infection, whereas the organs of the moribund animals were taken just prior to death.
+, NiV RNA detected; −, NiV RNA not detected. D6, day 6 after infection.
Effect of postinfection administration of anti-NiV MAbs on the course of infection.
If immunotherapeutic treatment is to be effective in preventing disease, then it is necessary to know how long after exposure to the disease it is possible to give the treatment. To study this phenomenon, hamsters were infected and either 112 μg of anti-G (Nip GIP 1.7) or 180 μg of anti-F (Nip GIP 35) MAbs was administered to each animal immediately after infection or after 1, 2, 3, or 4 days. The animals were observed for 86 days. The results (Table 5) indicate that anti-G MAbs protected more than 50% of the animals when it was administered after 24 h and that no protection was observed when the MAb was administered later. In contrast, passive administration of anti-F MAbs 1 h after the infection completely protected the animals, and a later administration, at 96 h, protected half of the animals.
TABLE 5.
Protection of hamsters by anti-NiV MAbs after infection with NiVa
| MAb | Time of MAb administration (hours after infection) | % of surviving animals | Mean time of death (days) |
|---|---|---|---|
| None (control) | 0 | 7.5 | |
| Nip GIP 1.7 (anti-NiV.G) | 1 | 75 | 11 |
| 24 | 50 | 15 | |
| 48 | 0 | 20 | |
| 72 | 0 | 12.5 | |
| 96 | 0 | 7.5 | |
| Nip GIP 35 (anti-NiV.F) | 1 | 100 | |
| 24 | 50 | 8 | |
| 48 | 50 | 21 | |
| 72 | 25 | 12.3 | |
| 96 | 50 | 12 |
Hamsters were infected with 100 LD50 and were subsequently given either MAb NIP GIP 1.7 (anti-G) or NIP GIP 35 (anti-F) at 1, 24, 48, 72, or 96 h after infection (four animals per group).
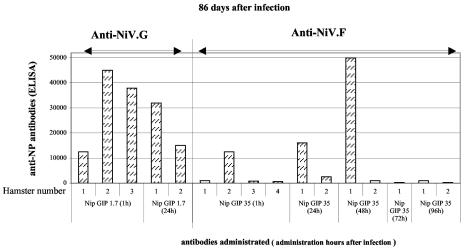
In contrast to the previous studies in which the anti-NiV MAbs were administered 24 h prior to and 1 h after infection, in the present experiment, administration of a single dose of anti-G MAbs 1 h after infection, although protecting the animals from clinical disease did not give a sterilizing immunity, as anti-NP antibodies were detected after challenge (Fig. 4). Under similar conditions, the anti-F MAbs gave a sterilizing immunity in three out of four animals. More than half of the surviving animals that had been given anti-F MAbs given later (1 to 4 days) did not induce anti-NP antibodies.
FIG. 4.
Postinfection treatment of hamsters with anti-NiV MAbs. Serum anti-NiV.NP antibodies measured by ELISA in hamsters receiving anti-G (Nip GIP 1.7) or anti-F (Nip GIP 35) MAbs administered up to 4 days after infection. Serum antibody levels were measured 86 days after infection. Each bar represents the value for one hamster.
DISCUSSION
The strategy of passive immunity was first developed in 1890 in Koch's laboratory (1). Subsequently, the administration of antibodies has been used in both the prevention and treatment of a number of microbial infections, including meningitis (6) and measles (7). However, the development of vaccines led to a decline in the use of antisera as a means of protection. The progress in a number of technologies, such as MAbs, has led to the reassessment of passive immunity as a means to prevent and treat a number of acute infections and cancers. Such a strategy would be appropriate for treating diseases caused by emerging viruses when it may be difficult to put into practice an active vaccination policy.
Our previous studies using polyclonal antibodies against either the NiV G or F glycoproteins showed that hamsters could be protected against a lethal challenge of NiV (9). As the antibody response in these animals greatly increased after challenge, it was assumed that the quantity of antisera did not give a sterilizing immunity. In the present study, we extended our investigations to examine protection by monoclonal antibodies. Antibodies directed to either the G or F glycoprotein and with high in vitro neutralizing activity protected animals from a lethal infection. At the higher MAb levels (112 μg for anti-G and 180 μg for anti-F), sterilizing immunity was achieved, as after challenge the anti-NiV antibody levels of hamsters' sera did not increase and anti-NiV-NP antibodies could not be detected. In contrast, at lower MAb levels where protection from clinical symptoms was still observed, an increase in antibody levels was observed from 18 days after infection. It has been known for some time that polyclonal antibodies can suppress the humoral response to an antigen (16, 20). In our previous studies with measles, we confirmed this observation but noted that even when MAbs were used at extremely high levels, there was no suppression to the humoral response to the measles virus antigen (8). Therefore, the absence of a humoral response in our present studies can be interpreted as obtaining a sterilizing immunity. This was confirmed by the failure to detect virus in different organs using RT-PCR.
Our initial studies in which the MAbs were given prior to infection confirmed the efficiency of treatment using passive immunity. However, in practice it is more likely that personnel would be treated after exposure to an infected source. In our hamster model, in which mortality occurs from the sixth day after infection, we found that the anti-F MAbs were more efficient. Although the anti-G MAbs protected half the animals when given 24 h after the infection, serological analysis showed that virus replication had occurred. In contrast, administration of anti-F MAbs in the same time frame completely suppressed virus replication. Anti-G MAbs block virus attachment to the host cell receptor, whereas anti-F antibodies inhibit fusion. Early studies with simian virus 5 in tissue culture suggested that antibodies to F might be more important than those to the viral attachment protein, because they both neutralize infectivity and prevent cell-to-cell spread of infectivity (14). However, more recent studies have shown that both glycoproteins are involved in the fusion process (23). Thus, the greater efficiency of the F MAb might be due to the intrinsic properties of the antibody, rather than its antigen specificity.
The use of MAbs as a treatment against viral diseases may have the disadvantage of being too specific, as variants of the virus may be outside its spectrum of activity. The G glycoprotein of NiV is potentially the most variable of the two viral glycoproteins with 83.3% homology with the G protein of Hendra virus, whereas the F proteins of the two viruses have 88.1% homology (10, 21). In vitro, our anti-G MAbs do not neutralize Hendra virus, whereas the F MAbs do so. Thus, from the present study, although the anti-G MAb was the most efficient in protection, the anti-F MAb should have a broader application. NiVs recently isolated in Cambodia (19) reacted with the MAbs used in the present study.
In our previous study (9) we showed that immunization with either the Nipah virus G or F glycoprotein prevented a lethal infection in hamsters. We have now extended our studies to show that passive immunoprophylaxis with MAbs directed to either of these viral proteins protects the animals. Thus, the adoption of a prevention or cure policy must be considered. Ribavirin treatment against NiV infections has shown partial activity in recovery of the disease. Efficient treatment may be recommended using combined drug therapy and immunotherapy (3). It is necessary to balance the possibility of vaccinating a susceptible population with a low incidence of infection against employing passive immunotherapy in an outbreak setting.
Acknowledgments
These studies were supported by a grant from Aventis Pharma (Sanofi-Aventis Group) and Bayer Pharma as part of a multiorganism call for proposals. The studies were also supported by INSERM and Institut Pasteur, Paris, France (Valorisation de la Recherche). V.G. was supported by a scholarship from the Direction Générale de l'Armée and the Fondation pour la Recherche Medicale. R.B. is a CNRS scientist.
REFERENCES
- 1.Behring, E. A., and S. Kitasato. 1890. Über das Zustandekommen der Diptherie-Immunität Beithoeren. Deutsch. Med. Woch. 49:1113-1114. [Google Scholar]
- 2.Bengis, R. G., F. A. Leighton, J. R. Fischer, M. Artois, T. Morner, and C. M. Tate. 2004. The role of wildlife in emerging and re-emerging zoonoses. Rev. Sci. Technol. 23:497-511. [PubMed] [Google Scholar]
- 3.Chong, H. T., A. Kamarulzaman, C. T. Tan, K. J. Goh, T. Thayaparan, S. R. Kunjapan, N. K. Chew, K. B. Chua, and S. K. Lam. 2001. Treatment of acute Nipah encephalitis with ribavirin. Ann. Neurol. 49:810-813. [DOI] [PubMed] [Google Scholar]
- 4.Chua, K. B., W. J. Bellini, P. A. Rota, B. H. Harcourt, A. Tamin, S. K. Lam, T. G. Ksiazek, P. E. Rollin, S. R. Zaki, W. Shieh, C. S. Goldsmith, D. J. Gubler, J. T. Roehrig, B. Eaton, A. R. Gould, J. Olson, H. Field, P. Daniels, A. E. Ling, C. J. Peters, L. J. Anderson, and B. W. Mahy. 2000. Nipah virus: a recently emergent deadly paramyxovirus. Science 288:1432-1435. [DOI] [PubMed] [Google Scholar]
- 5.Chua, K. B., C. L. Koh, P. S. Hooi, K. F. Wee, J. H. Khong, B. H. Chua, Y. P. Chan, M. E. Lim, and S. K. Lam. 2002. Isolation of Nipah virus from Malaysian Island flying-foxes. Microbes Infect. 4:145-151. [DOI] [PubMed] [Google Scholar]
- 6.Flexner, S. 1913. The results of the serum treatment in thirteen hundred cases of epidemic meningitis. J. Exp. Med. 17:553-575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gallagher, J. R. 1935. Use of convalescent measles serum to control measles in a preparatory school. Am. J. Public Health 25:595-598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Galletti, R., P. Beauverger, and T. F. Wild. 1995. Passively administered antibody suppresses the induction of measles virus antibodies by vaccinia-measles recombinant viruses. Vaccine 13:197-201. [DOI] [PubMed] [Google Scholar]
- 9.Guillaume, V., H. Contamin, P. Loth, M. C. Georges-Courbot, A. Lefeuvre, P. Marianneau, K. B. Chua, S. K. Lam, R. Buckland, V. Deubel, and T. F. Wild. 2004. Nipah virus: vaccination and passive protection studies in a hamster model. J. Virol. 78:834-840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Harcourt, B. H., A. Tamin, T. G. Ksiazek, P. E. Rollin, L. J. Anderson, W. J. Bellini, and P. A. Rota. 2000. Molecular characterization of Nipah virus, a newly emergent paramyxovirus. Virology 271:334-349. [DOI] [PubMed] [Google Scholar]
- 11.Hooper, P., S. Zaki, P. Daniels, and D. Middleton. 2001. Comparative pathology of the diseases caused by Hendra and Nipah viruses. Microbes Infect. 3:315-322. [DOI] [PubMed] [Google Scholar]
- 12.Hsu, V. P., M. J. Hossain, U. D. Parashar, M. M. Ali, T. G. Ksiazek, I. Kuzmin, M. Niezgoda, C. Rupprecht, J. Bresee, and R. F. Breiman. 2004. Nipah virus encephalitis reemergence, Bangladesh. Emerg. Infect. Dis. 10:2082-2087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Mahy, B. W., and C. C. Brown. 2000. Emerging zoonoses: crossing the species barrier. Rev. Sci. Technol. 19:33-40. [DOI] [PubMed] [Google Scholar]
- 14.Merz, D. C., A. Scheid, and P. W. Choppin. 1981. Immunological studies of the functions of paramyxovirus glycoproteins. Virology 109:94-105. [DOI] [PubMed] [Google Scholar]
- 15.Middleton, D. J., H. A. Westbury, C. J. Morrissy, B. M. van der Heide, G. M. Russell, M. A. Braun, and A. D. Hyatt. 2002. Experimental Nipah virus infection in pigs and cats. J. Comp. Pathol. 126:124-136. [DOI] [PubMed] [Google Scholar]
- 16.Murphy, B. R., R. A. Olmsted, P. L. Collins, R. M. Chanock, and G. A. Prince. 1988. Passive transfer of respiratory syncytial virus (RSV) antiserum suppresses the immune response to the RSV fusion (F) and large (G) glycoproteins expressed by recombinant vaccinia viruses. J. Virol. 62:3907-3910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Murray, K., P. Selleck, P. Hooper, A. Hyatt, A. Gould, L. Gleeson, H. Westbury, L. Hiley, L. Selvey, B. Rodwell, et al. 1995. A morbillivirus that caused fatal disease in horses and humans. Science 268:94-97. [DOI] [PubMed] [Google Scholar]
- 18.Olson, J. G., C. Rupprecht, P. E. Rollin, U. S. An, M. Niezgoda, T. Clemins, J. Walston, and T. G. Ksiazek. 2002. Antibodies to Nipah-like virus in bats (Pteropus lylei), Cambodia. Emerg. Infect. Dis. 8:987-988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18a.Reed, L. J., and H. Muench. 1938. A simple method of estimating 50 percent end points. Am. J. Hyg. 27:493-497. [Google Scholar]
- 19.Reynes, J. M., D. Counor, S. Ong, C. Faure, V. Seng, S. Molia, J. Walston, M. C. Georges-Courbot, V. Deubel, and J. L. Sarthou. 2005. Nipah virus in Lyle's flying foxes, Cambodia. Emerg. Infect. Dis. 11:1042-1047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Rowley, D. A., F. W. Fitch, F. P. Stuart, H. Kohler, and H. Cosenza. 1973. Specific suppression of immune responses. Science 181:1133-1141. [DOI] [PubMed] [Google Scholar]
- 21.Wang, L., B. H. Harcourt, M. Yu, A. Tamin, P. A. Rota, W. J. Bellini, and B. T. Eaton. 2001. Molecular biology of Hendra and Nipah viruses. Microbes Infect. 3:279-287. [DOI] [PubMed] [Google Scholar]
- 22.Wang, L. F., M. Yu, E. Hansson, L. I. Pritchard, B. Shiell, W. P. Michalski, and B. T. Eaton. 2000. The exceptionally large genome of Hendra virus: support for creation of a new genus within the family Paramyxoviridae. J. Virol. 74:9972-9979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Wild, T. F., E. Malvoisin, and R. Buckland. 1991. Measles virus: both the haemagglutinin and fusion glycoproteins are required for fusion. J. Gen. Virol. 72:439-442. [DOI] [PubMed] [Google Scholar]
- 24.Wong, K. T., W. J. Shieh, S. Kumar, K. Norain, W. Abdullah, J. Guarner, C. S. Goldsmith, K. B. Chua, S. K. Lam, C. T. Tan, K. J. Goh, H. T. Chong, R. Jusoh, P. E. Rollin, T. G. Ksiazek, and S. R. Zaki. 2002. Nipah virus infection: pathology and pathogenesis of an emerging paramyxoviral zoonosis. Am. J. Pathol. 161:2153-2167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Yob, J. M., H. Field, A. M. Rashdi, C. Morrissy, B. van der Heide, P. Rota, A. bin Adzhar, J. White, P. Daniels, A. Jamaluddin, and T. Ksiazek. 2001. Nipah virus infection in bats (order Chiroptera) in peninsular Malaysia. Emerg. Infect. Dis. 7:439-441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Yu, M., E. Hansson, J. P. Langedijk, B. T. Eaton, and L. F. Wang. 1998. The attachment protein of Hendra virus has high structural similarity but limited primary sequence homology compared with viruses in the genus Paramyxovirus. Virology 251:227-233. [DOI] [PubMed] [Google Scholar]