Abstract
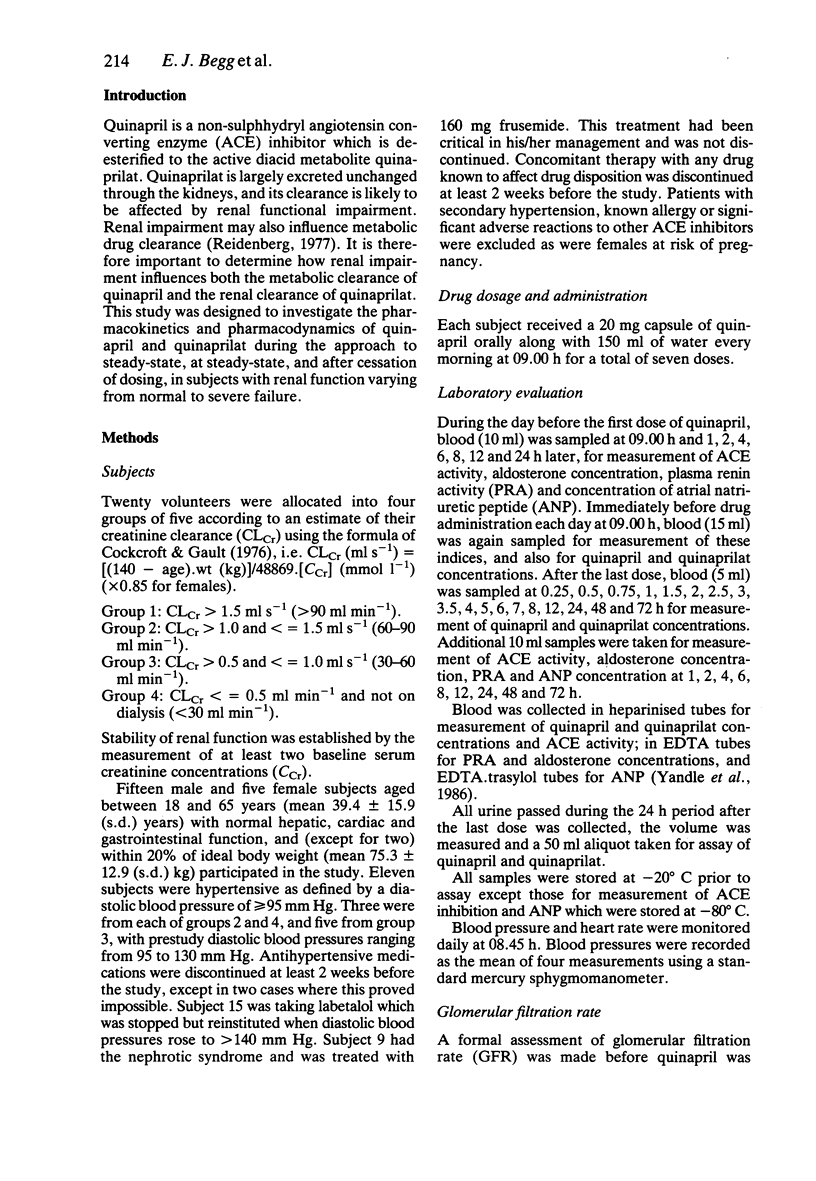
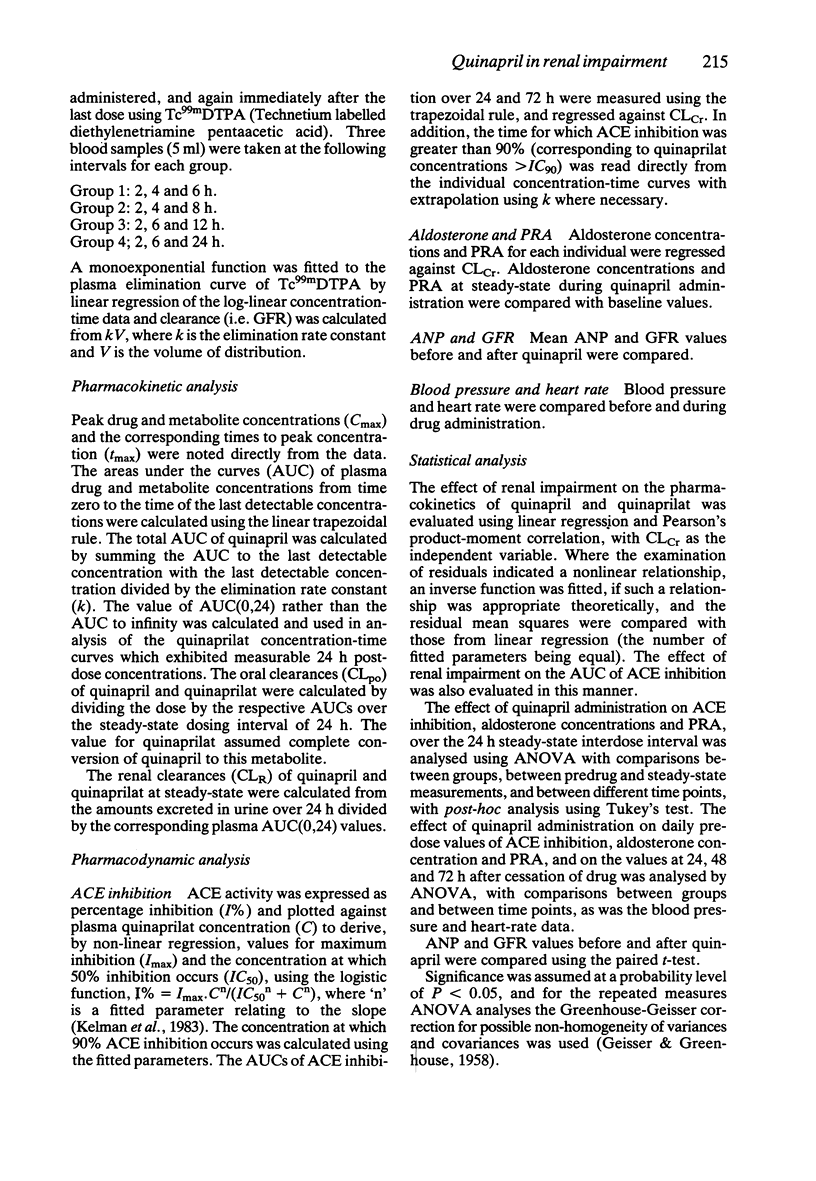
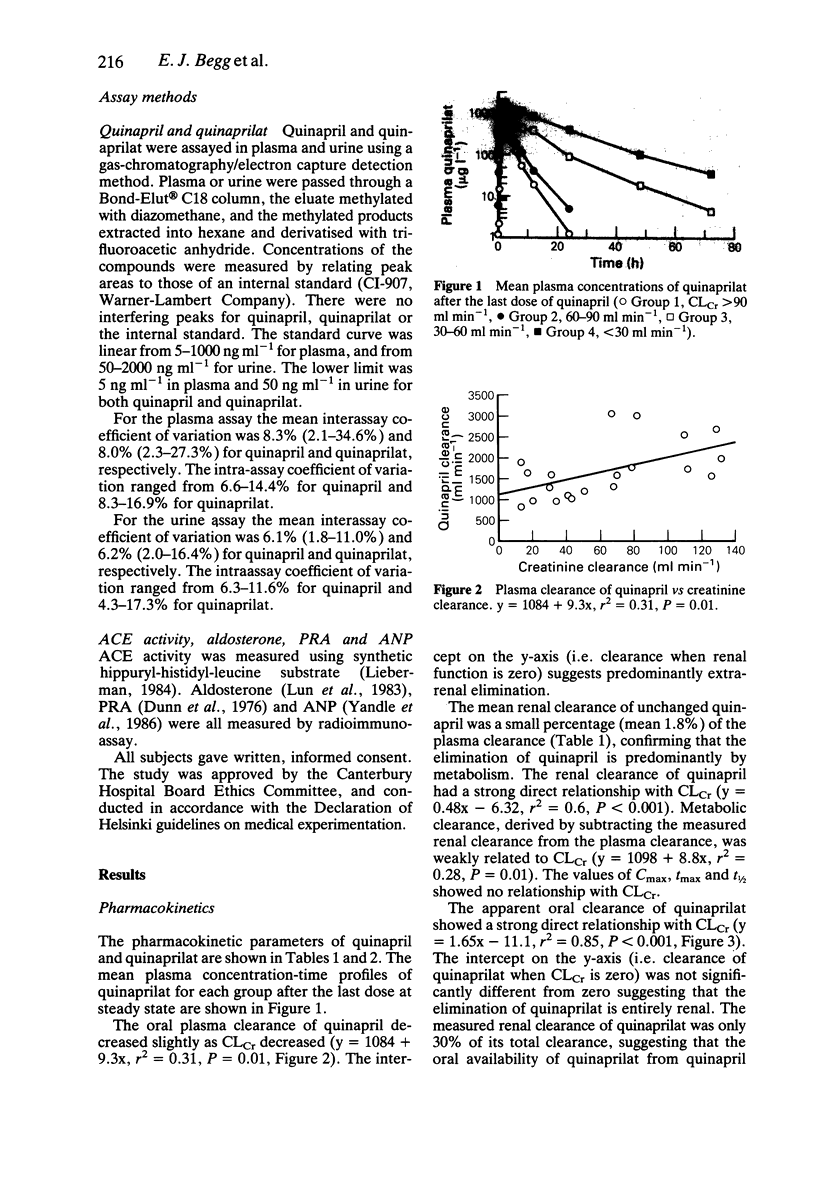
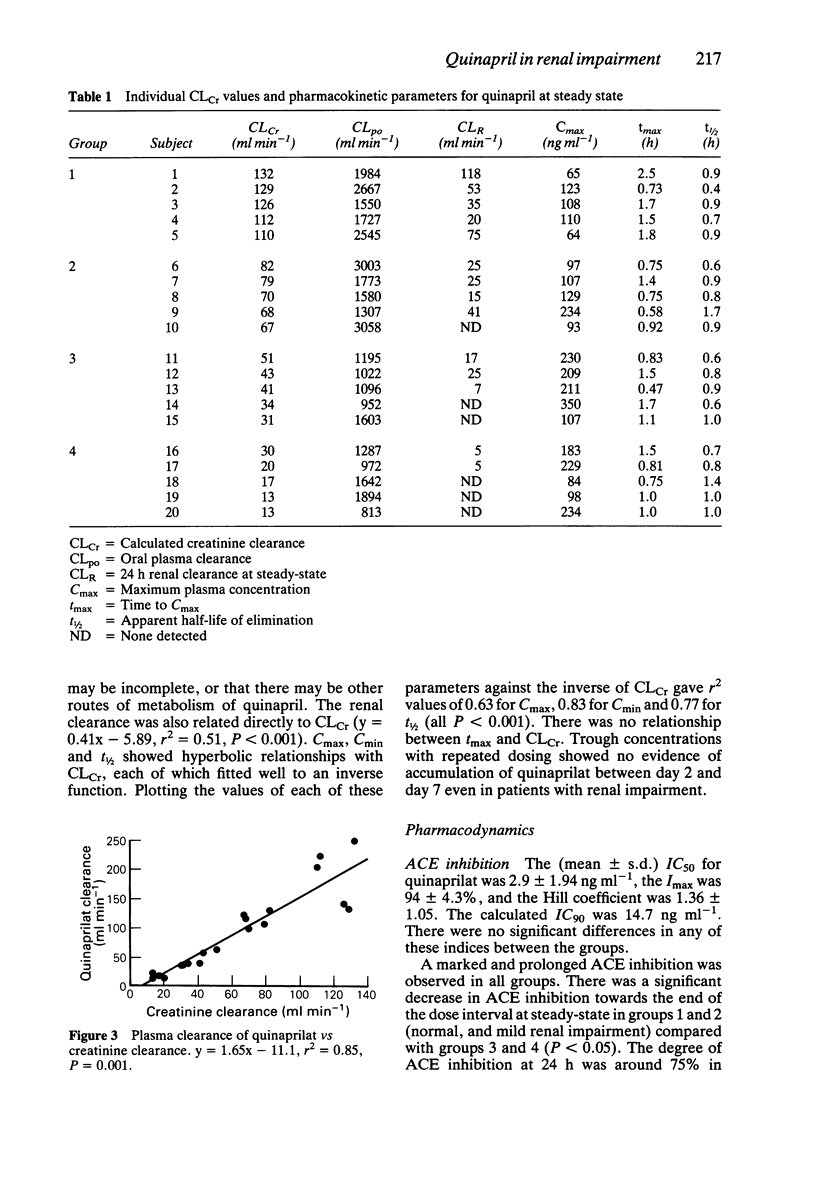
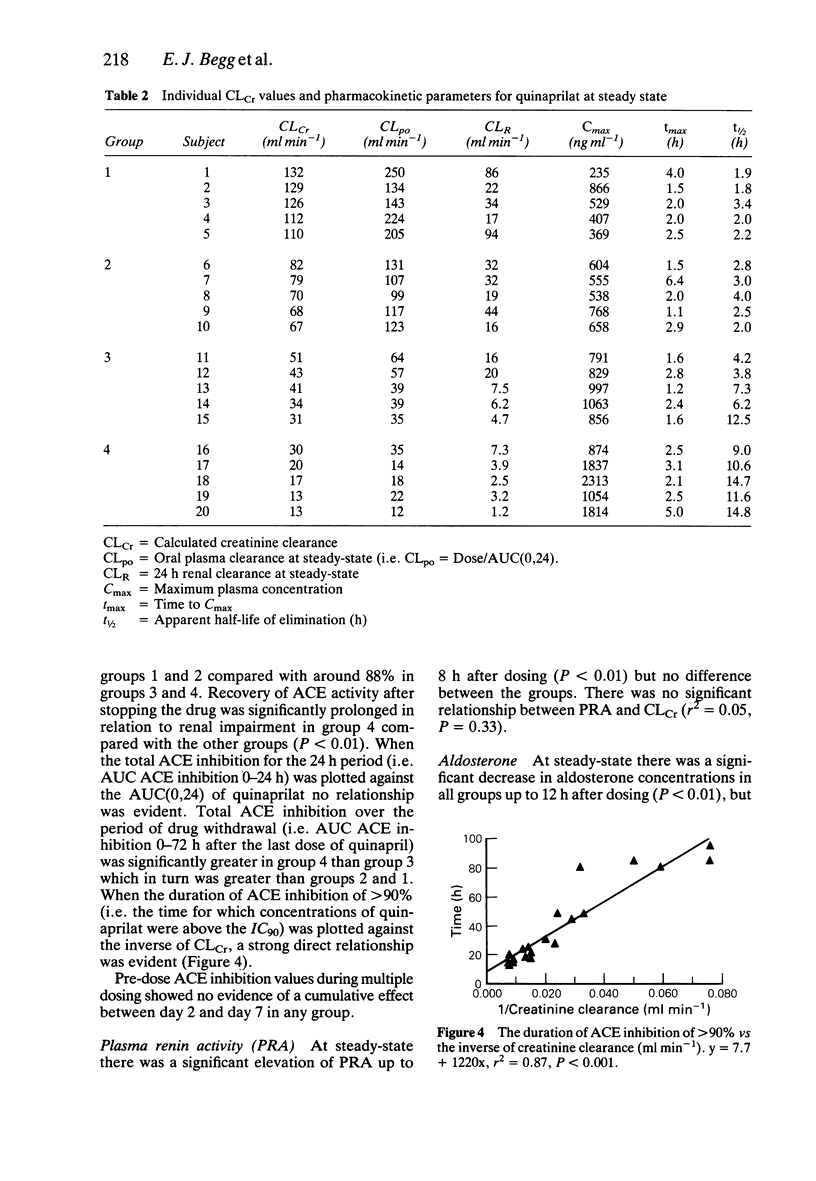
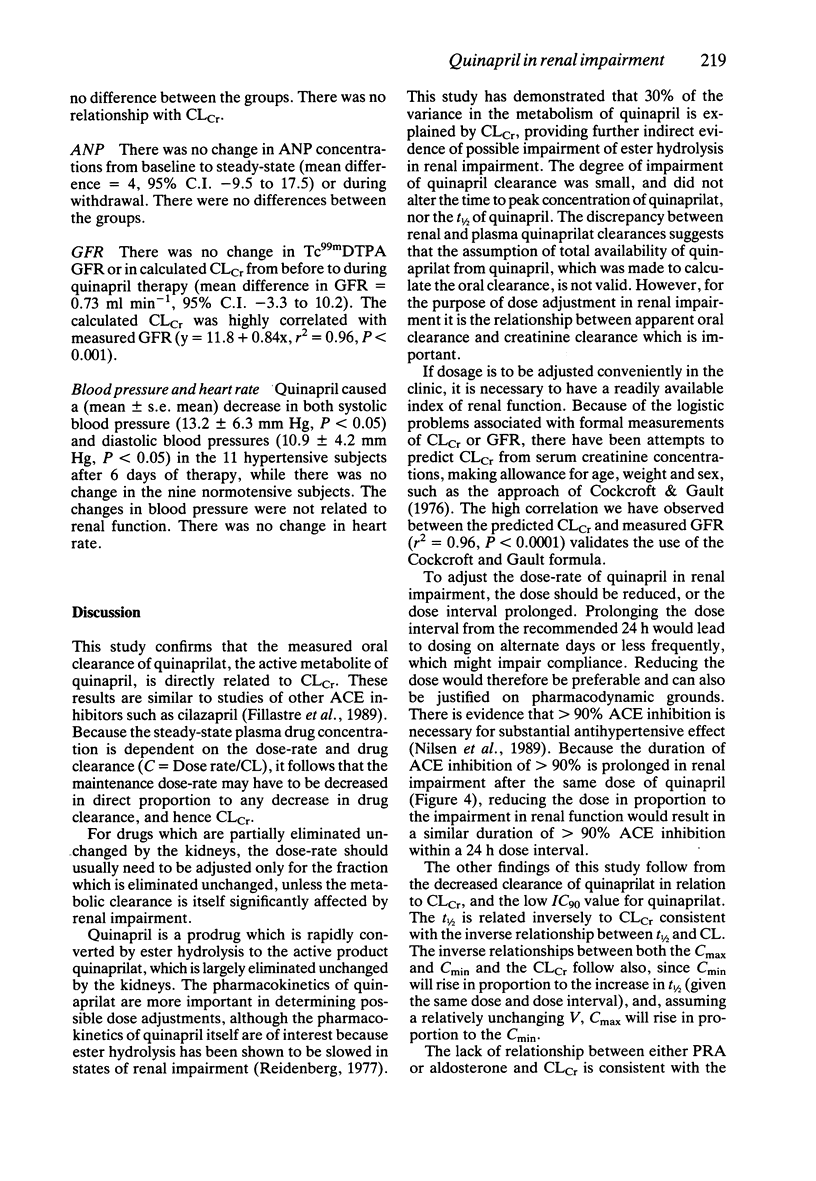
1. The pharmacokinetics and pharmacodynamics of quinapril and its active metabolite quinaprilat were studied in 20 subjects with renal function varying from normal to severe renal failure, during the approach to and at steady-state, and for 72 h after cessation of quinapril 20 mg orally for 7 days. 2. The apparent oral plasma clearance of quinaprilat (dose of quinapril equivalent/AUC of quinaprilat) was directly related to creatinine clearance (CLCr). The predicted apparent oral clearance of quinaprilat was zero when CLCr was zero, suggesting minimal extrarenal elimination. 3. Peak and trough concentrations of quinaprilat, and its apparent elimination half-life, varied inversely with CLCr. 4. Trough concentrations of quinaprilat showed no accumulation between 2 and 7 days, even in severe renal impairment. 5. There was a weak relationship between the oral plasma clearance of quinapril and CLCr. 6. ACE inhibition was marked and prolonged in all subjects, with 50% inhibition at 2.7 +/- 1.9% ng ml-1 of quinaprilat. The time for which ACE inhibition was greater than 90% was related inversely to CLCr. 7. Aldosterone concentrations and plasma renin activity responded in a predictable way, but with no clear relationship To CLCr. 8. Atrial natriuretic peptide concentrations were not affected by quinapril administration. 9. Glomerular filtration rate, as measured by Tc99mDTPA clearance, was not affected by quinapril administration. 10. Blood pressure at steady-state decreased significantly in the subjects with hypertension. The changes in blood pressure were not related to renal function. 11. These results suggest that the dosage rate of quinapril may have to be altered in renal impairment.(ABSTRACT TRUNCATED AT 250 WORDS)
Full text
PDF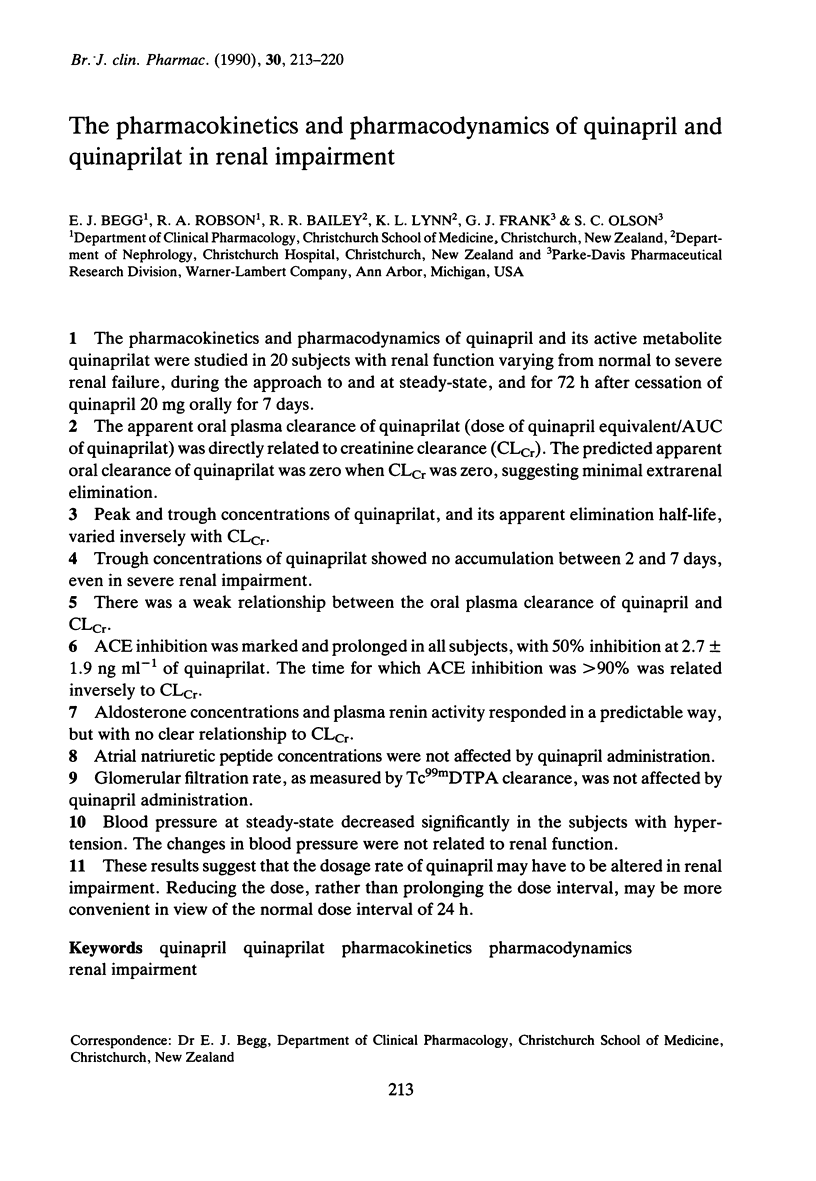

Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Cockcroft D. W., Gault M. H. Prediction of creatinine clearance from serum creatinine. Nephron. 1976;16(1):31–41. doi: 10.1159/000180580. [DOI] [PubMed] [Google Scholar]
- Dunn P. J., Espiner E. A. Outpatient screening tests for primary aldosteronism. Aust N Z J Med. 1976 Apr;6(2):131–135. doi: 10.1111/j.1445-5994.1976.tb03306.x. [DOI] [PubMed] [Google Scholar]
- Fillastre J. P., Moulin B., Godin M., Williams P. E., Brown A. N., Francis R. J., Pinta P., Manfredi R. Pharmacokinetics of cilazapril in patients with renal failure. Br J Clin Pharmacol. 1989;27 (Suppl 2):275S–282S. doi: 10.1111/j.1365-2125.1989.tb03492.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kelman A. W., Reid J. L., Millar J. A. Concentration effect modelling with converting enzyme inhibitors in man. Br J Clin Pharmacol. 1983 Apr;15(4):506–507. doi: 10.1111/j.1365-2125.1983.tb01542.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lun S., Espiner E. A., Nicholls M. G., Yandle T. G. A direct radioimmunoassay for aldosterone in plasma. Clin Chem. 1983 Feb;29(2):268–271. [PubMed] [Google Scholar]
- Nilsen O. G., Sellevold O. F., Romfo O. S., Smedsrud A., Grynne B., Williams P. E., Kleinbloesem C. H. Pharmacokinetics and effects on renal function following cilazapril and hydrochlorothiazide alone and in combination in healthy subjects and hypertensive patients. Br J Clin Pharmacol. 1989;27 (Suppl 2):323S–328S. doi: 10.1111/j.1365-2125.1989.tb03499.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reidenberg M. M. The biotransformation of drugs in renal failure. Am J Med. 1977 Apr;62(4):482–485. doi: 10.1016/0002-9343(77)90401-6. [DOI] [PubMed] [Google Scholar]
- Yandle T. G., Espiner E. A., Nicholls M. G., Duff H. Radioimmunoassay and characterization of atrial natriuretic peptide in human plasma. J Clin Endocrinol Metab. 1986 Jul;63(1):72–79. doi: 10.1210/jcem-63-1-72. [DOI] [PubMed] [Google Scholar]


