Abstract
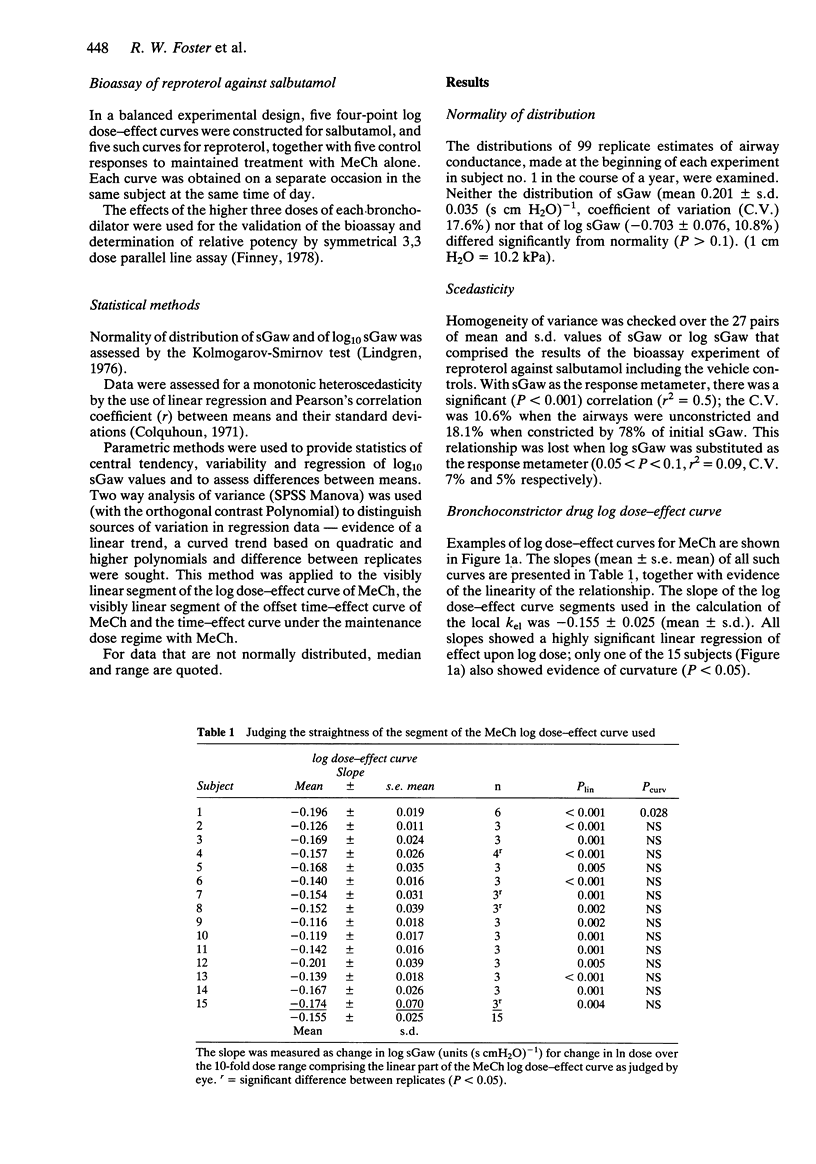
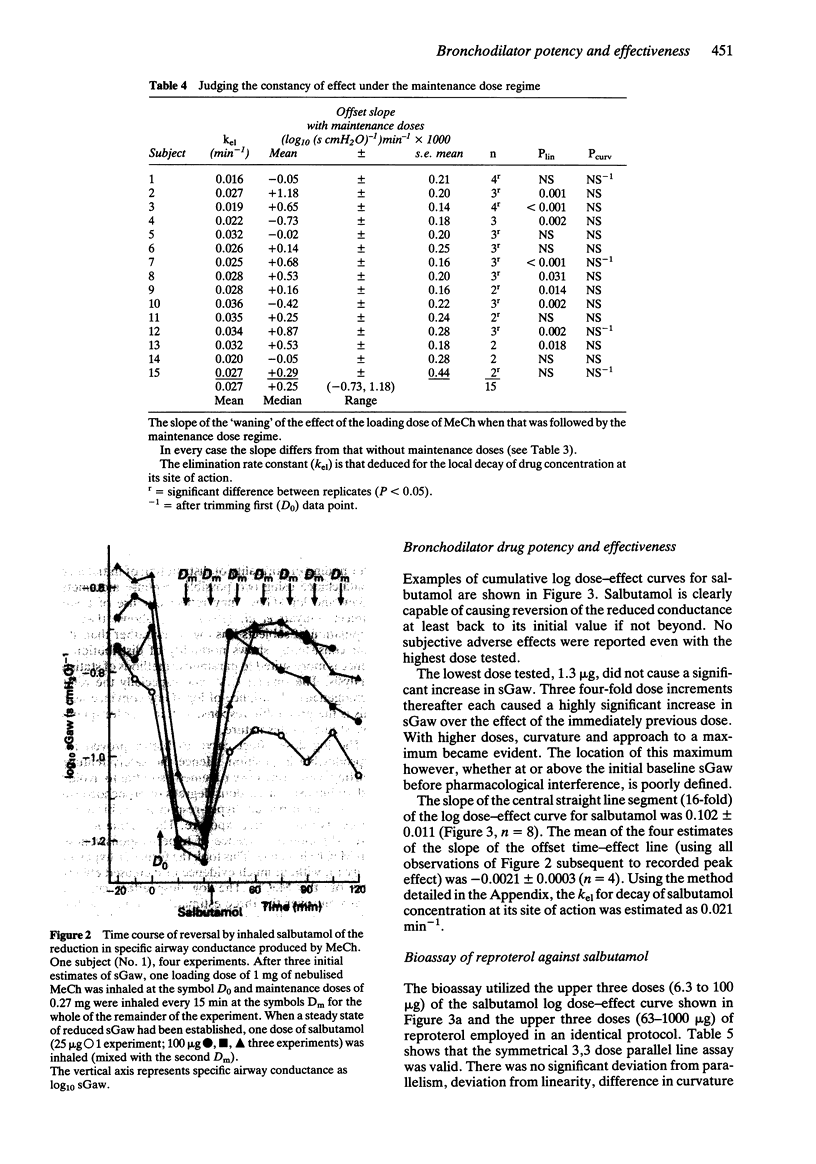
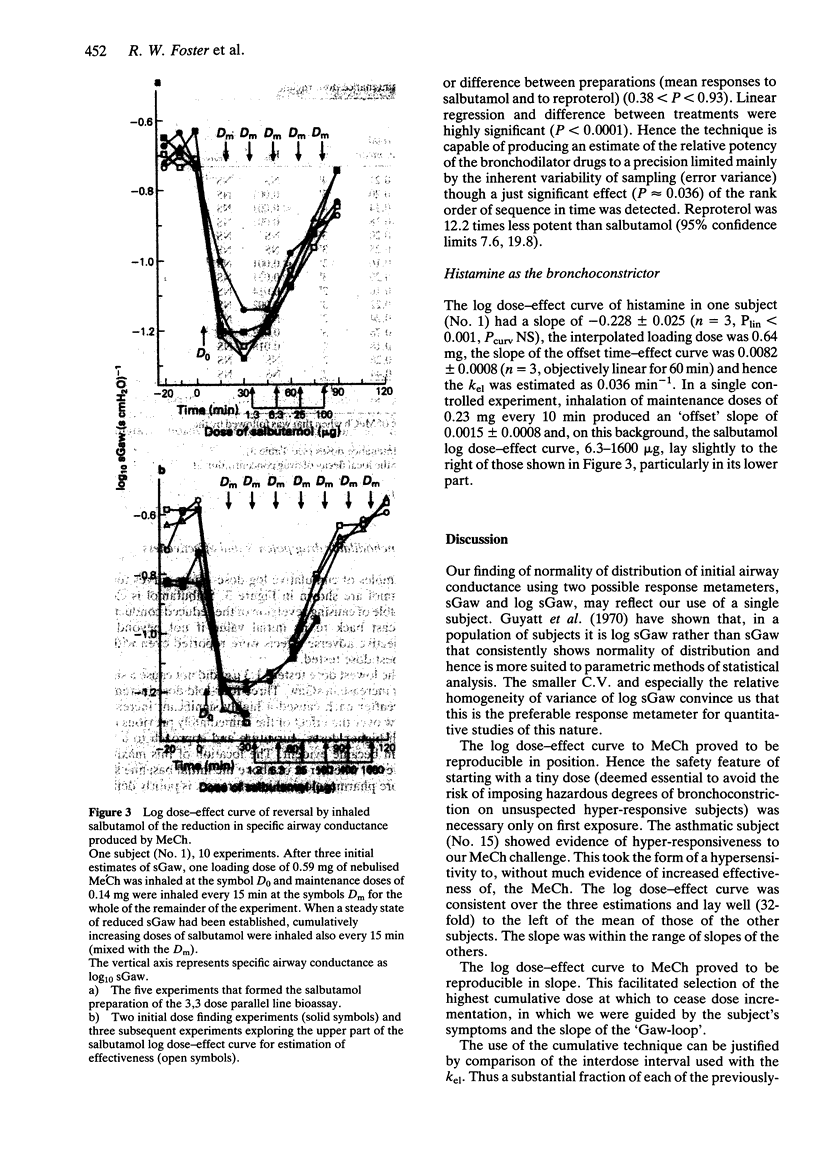
1. Bioassay of inhaled bronchodilator drugs for potency and effectiveness in normal human subjects is rendered difficult and imprecise because bronchomotor tone is low. When attempting to determine log dose-effect relationships for inhaled, nebulised bronchodilator drugs and measuring increased specific airways conductance (sGaw), the coefficient of variation of each mean response is likely to be so large that an intermediate response is not significantly different from either the maximum or no response. 2. A method is described by which inhaled, nebulised bronchodilator drugs can be bioassayed for potency and effectiveness with high precision. The method involves the use of inhaled, nebulised bronchoconstrictor agents (methacholine or histamine) to provide a highly reproducible, near-constant, background reduction in airway conductance in normal human subjects. The activity of bronchodilators is assessed against this background reduction in airway conductance. 3. Log specific airway conductance (log sGaw) was chosen as the response metameter on grounds of normality of distribution and relative homoscedasticity. A central straight line segment of the bronchoconstrictor drug dose-effect curve extending over a 10-fold dose multiple could be found easily; the upper end of this segment occurred near 67-75% reduction in sGaw and was reproducible. 4. The effect of a dose bronchoconstrictor drug causing 67-75% reduction in sGaw waned linearly with time at first, over the effect segment corresponding to the linear segment of the drug's log dose-effect curve. The rate constant of local elimination of bronchoconstrictor drug from its site of action, in inhaled dose equivalents, was deduced from the ratio of the slopes of the linear segments of the log dose-effect and time-effect curves. 5. The maintenance dose rate to maintain the peak effect (67-75% reduction in sGaw) of the loading dose was calculated. The repeated administration of maintenance doses at regular short intervals, at this calculated dose rate, created a steady state of bronchoconstriction equal in extent to the effect of the loading dose. This steady state bronchoconstriction occurred without undue discomfort for the subject and was reproducible. 6. Against this background bronchoconstriction, inhaled, nebulised salbutamol produced a rapidly developing and slowly waning increase in sGaw. Reproducible log dose-effect curves for the bronchodilator drugs salbutamol and reproterol allowed measurement of their potency and effectiveness; the potency of reproterol relative to salbutamol was 0.082 with 95% confidence limits of 0.0504 and 0.131. 7. Estimation of the subject's pharmacodynamic and pharmacokinetic parameters for inhaled methacholine from just three dosage individualising sessions provides estimates accurate enough to be of practical value.
Full text
PDF
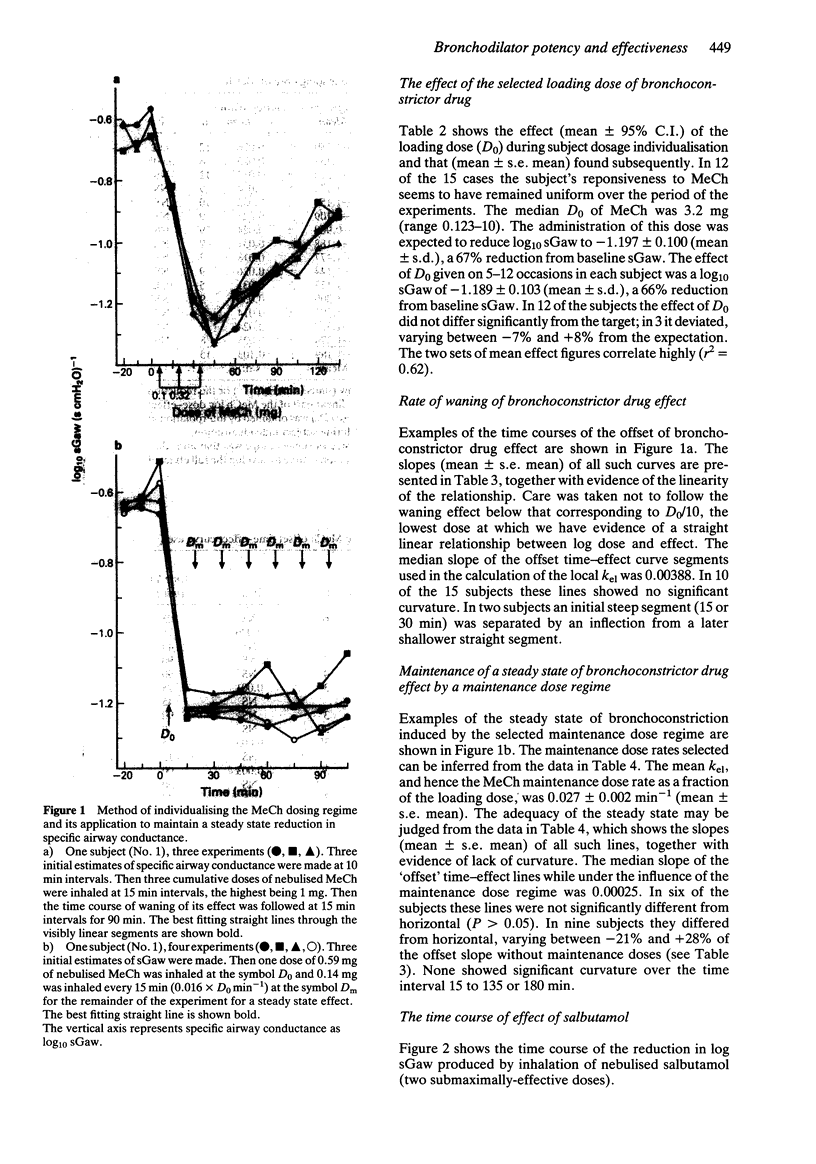
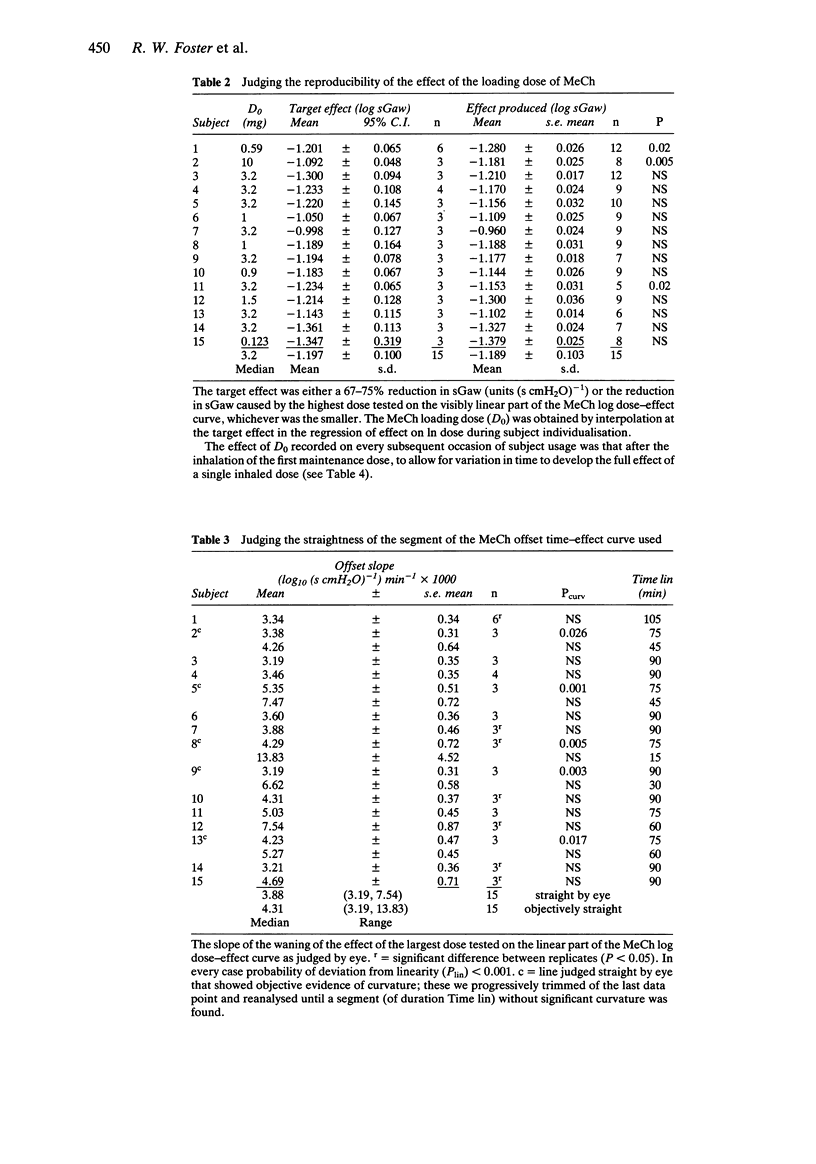
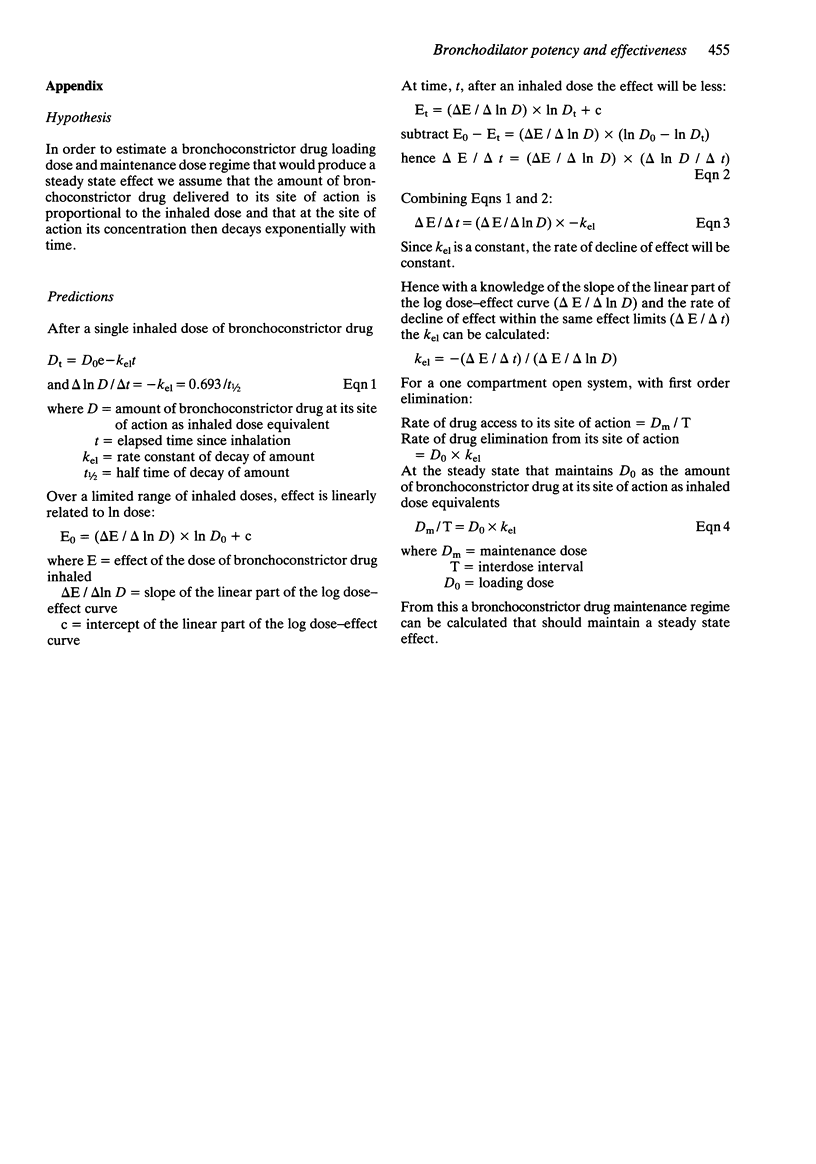
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Barnes P. J., Pride N. B. Dose-response curves to inhaled beta-adrenoceptor agonists in normal and asthmatic subjects. Br J Clin Pharmacol. 1983 Jun;15(6):677–682. doi: 10.1111/j.1365-2125.1983.tb01549.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guyatt A. R., Berry G., Alpers J. H., Bramley A. C., Fletcher C. M. Relationship of airway conductance and its immediate change on smoking to smoking habits and symptoms of chronic bronchitis. Am Rev Respir Dis. 1970 Jan;101(1):44–54. doi: 10.1164/arrd.1970.101.1.44. [DOI] [PubMed] [Google Scholar]
- Harvey J. E., Tattersfield A. E. Airway response to salbutamol: effect of regular salbutamol inhalations in normal, atopic, and asthmatic subjects. Thorax. 1982 Apr;37(4):280–287. doi: 10.1136/thx.37.4.280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Higgs C. M., Laszlo G. The duration of protection from exercise-induced asthma by inhaled salbutamol, and a comparison with inhaled reproterol. Br J Dis Chest. 1983 Jul;77(3):262–269. [PubMed] [Google Scholar]
- Holgate S. T., Baldwin C. J., Tattersfield A. E. beta-adrenergic agonist resistance in normal human airways. Lancet. 1977 Aug 20;2(8034):375–377. doi: 10.1016/s0140-6736(77)90304-x. [DOI] [PubMed] [Google Scholar]
- Smith A. P., Orehek J., Charpin J. Bronchodilator drug tests in normal subjects [proceedings]. Br J Dis Chest. 1977 Oct;71(4):234–236. [PubMed] [Google Scholar]
- Tattersfield A. E., Keeping I. M. Assessing change in airway calibre--measurement of airway resistance. Br J Clin Pharmacol. 1979 Oct;8(4):307–319. doi: 10.1111/j.1365-2125.1979.tb04711.x. [DOI] [PMC free article] [PubMed] [Google Scholar]


