Abstract
A major limitation of adenovirus (Ad) gene therapy product expression in the liver is subsequent elimination of the hepatocytes expressing the gene therapy product. This elimination is caused by both necrosis and apoptosis related to the innate and cell-mediated immune response to the Ad. Apoptosis of hepatocytes can be induced by the innate immune response by signaling through death domain receptors on hepatocytes including the tumor necrosis factor alpha (TNF-α) receptor (TNFR), Fas, and death domain receptors DR4 and DR5. We have previously shown that blocking signaling through TNFR enhances and prolongs gene therapy product expression in the liver. In the present study, we constructed an Ad that produces a soluble DR5-Fc (AdsDR5), which is capable of neutralizing TNF-related apoptosis-inducing ligand (TRAIL). AdsDR5 prevents TRAIL-mediated apoptosis of CD3-activated T cells and decreases hepatocyte apoptosis after AdCMVLacZ administration and enhances the level and duration of lacZ transgene expression in the liver. In addition to blocking TRAIL and directly inhibiting apoptosis, AdsDR5 decreases production of gamma interferon (IFN-γ) and TNF-α and decreases NK cell activation, all of which limit Ad-mediated transgene expression in the liver. These results indicate that (i) AdsDR5 produces a DR5-Fc capable of neutralizing TRAIL, (ii) AdsDR5 can reduce activation of NK cells and reduce induction of IFN-γ and TNF-α after Ad administration, and (iii) administration of AdsDR5 can enhance Ad gene therapy in the liver.
Gene therapy to the liver is limited in both magnitude and duration by death of liver cells receiving the gene therapy (46, 47). Death domain receptors Fas (11, 25, 26, 38), tumor necrosis factor alpha (TNF-α) receptor (TNFR) (7, 11, 22, 28, 43), and DR4 and DR5 (18, 21, 32, 42, 45) play a prominent role in induction of hepatocyte apoptosis. These receptors are stimulated by Fas ligand (FasL), TNF-α, and TNF-related apoptosis-inducing ligand (TRAIL), respectively. We and others have shown that soluble forms of these receptors for TNF-α and FasL can protect the liver from apoptosis after administration of adenovirus (19, 20, 48, 50, 51).
The conditions under which TRAIL is hepatotoxic are not yet clear (12). Although TRAIL, through ligation of its death domain-containing receptors, can induce either apoptosis by a Fas-associated death domain (FADD)-dependent mechanism or necrosis via a receptor-interactive peptide (RIP)-dependent cascade, under physiological conditions, these death-signaling events are inhibited by as yet unknown survival factors. In various disease states, such as after viral infection, the function of these survival factors may be blocked, unmasking TRAIL hepatotoxicity (2, 18, 45). Understanding the role and mechanism of TRAIL in the induction of adenovirus hepatotoxicity is relevant to both the safety of and long-term expression in adenovirus gene therapy.
TRAIL is constitutively expressed by NK cells in the liver but can be further up-regulated by gamma interferon (IFN-γ) as part of the innate immune response to adenovirus gene therapy. The early innate immune response to adenovirus (10, 44) involves production of IFN-γ primarily by NK cells and production of TNF-α primarily by Kupffer cells (5, 9, 24, 31, 54). Shin et al. (36) have shown that IFN-γ induces up-regulation of TRAIL on a hepatoma cell line and that a DR4-Fc fusion protein can inhibit this apoptosis. Jelachich and Lipton (17) have shown that, after infection with Theiler's murine encephalomyelitis virus, differentiated myelomonocytic cells exhibit up-regulation of TNF-α and TRAIL. These results suggest that regulation of NK cell production of IFN-γ and TRAIL-mediated hepatotoxicity are major factors that determine hepatotoxicity after adenovirus gene therapy.
The importance of TRAIL in regulation of cell death after adenovirus infection is demonstrated by the capability of adenovirus to down-regulate TRAIL receptors. Adenovirus type 5 encodes three proteins, named RID (previously named E3-10.4K/14.5K), E3-14.7K, and E1B-19K, that independently inhibit TRAIL-induced apoptosis of infected human cells. These adenovirus gene products inhibit TRAIL-mediated apoptosis by inducing internalization of TRAIL-R1 (DR4) from the surfaces of cells. Therefore, down-modulation of TRAIL receptors is employed by adenovirus to subvert apoptosis pathways present in hosts (41), further underscoring the importance of TRAIL-mediated apoptosis in the modulation of adenovirus-mediated apoptosis of hepatocytes.
The present experiments examine the effect of blocking TRAIL signaling of DR4 and DR5 by neutralizing TRAIL with an adenovirus capable of producing a soluble DR5 (sDR5), AdsDR5. Pretreatment of mice with AdsDR5 results in increased and prolonged expression of AdCMVLacZ in gene therapy for the liver. This was associated with decreased apoptosis of hepatocytes and decreased liver enzyme aspartate aminotransferase (AST) levels in the blood. Treatment with AdsDR5 results in prolonged and enhanced lacZ gene expression compared to treatment with soluble TNFR (sTNFR) alone. Treatment with both sTNFR1 and AdsDR5 exhibits a synergistic effect on the enhancement of lacZ gene expression. The mechanism of inhibition of apoptosis of liver cells after treatment with AdsDR5 involves both TRAIL-mediated apoptosis and inhibition of other pathways that can mediate adenovirus-induced liver damage. This includes induction of NK cells and stimulation of TNF-α and IFN-γ production. Together, the results indicate that the TRAIL-DR5 interaction after adenovirus gene therapy blocks several pathways of hepatocyte injury and leads to enhanced and prolonged gene therapy product expression in the liver.
MATERIALS AND METHODS
Production of recombinant AdsDR5, AdCMVLacZ, and AdCMVGFP.
The 399-bp sequence coding for the 133 amino acids of the extracellular domain (ED) of DR5 was obtained by PCR and verified by sequence analysis. The DR5-ED was fused with the immunoglobulin G1 Fc coding region to produce sDR5 (6). sDR5 was cloned into the BglII site of pAdTRACKCMV (Fig. 1) (13). The orientation of DR5-Ed in pAdTRACKCMVsDR5 was confirmed by BamHI restriction digestion. To make the recombinant adenovirus AdsDR5, in vitro recombination of pAdTRACKCMVsDR5 with pAdEasy was carried out in BJ5183 cells, after which AdsDR5 was produced as described previously (13). The recombinant adenovirus expressing sDR5 was selected and purified by standard procedures (50). To obtain a large quantity of recombinant AdsDR5, 293 cells were infected and grown for 48 h at 37°C prior to harvest and centrifugation using a tabletop centrifuge at 3,080 × g for 20 min. The infected cells were resuspended in phosphate-buffered saline (PBS) buffer and then lysed with three freeze-thaw cycles. The released virus was purified through two cesium chloride gradients, and then the purified recombinant AdsDR5 was titrated by a plaque assay (51), aliquoted, and stored at −80°C until used. AdCMVLacZ and AdCMVGFP were produced and purified as previously described (50, 51).
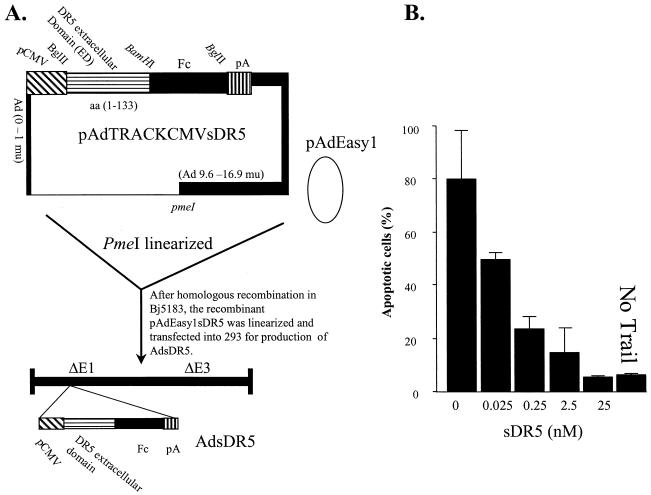
FIG. 1.
Construction of AdsDR5. (A) The coding sequence for sDR5 was cloned into the BglII site of pAdTRACKCMVsDR5. After linearization with pmeI this fragment underwent in vitro homologous recombination with pAdEasy1, resulting in production of pAdEasy1sDR5. AdsDR5 was produced by transfection of pAdEasysDR5 into 293 cells. aa, amino acids. (B) AdsDR5 prevents TRAIL-mediated apoptosis of the mouse spleen CD-3 activated T cells. Spleen T cells were stimulated with anti-CD3 antibody and 5 U of IL-2/ml for 48 h and then treated with different doses of sDR5, which was purified from AdsDR5-infected 293 cell supernatants with protein G in the presence of TRAIL (1 nM), and apoptosis was determined 24 h later by 7-AAD staining followed by quantification of the apoptotic cells using FACS analysis. The data represent three replicates at each dose. As a control, nontreated T cells were cultured with (lane 1) and without (lane 6) TRAIL.
Spleen T-cell isolation and TRAIL-mediated apoptosis.
Single-cell suspensions from the spleen were prepared with a metal sieve. Erythrocytes were lysed by treatment with NH4Cl lysis buffer (8.29 g of NH4Cl, 1.0 g of KHCO3, and 0.037 g of EDTA/liter). The cells were washed in RPMI 1640 containing 10 mM HEPES and resuspended in RPMI 1640 supplemented with a mixture containing 10% fetal calf serum (FCS; Sigma, St. Louis, Mo.), 1 mM l-glutamine, 5 × 10−5 M 2-mercaptoethanol, 10 mM HEPES, 1 mM sodium pyruvate, 100 μg of penicillin/ml, and 100 U of streptomycin/ml. The T cells were then isolated by using a nylon wood column as described previously (15). The cells were stimulated with a murine anti-CD3 antibody plus 5 U of interleukin-2 (IL-2; Bethesda Research Laboratories, Inc.) for 72 h at 2 × 105 cells/well in 200 μl of RPMI 1640 as described above in a round-bottom 96-well plate (Nunc, Naperville, Ill.). sDR5 was purified from the supernatants of AdsDR5-infected 293 cells with a protein A column (Sigma) and was verified by Western blot analysis as described previously (54). The cells were treated for 18 h with different concentrations of sDR5, ranging from 0.025 to 25 nM, in the presence of a 1 nM concentration of trimeric soluble TRAIL (Alexis Pharmaceuticals, San Diego, Calif.). The T-cell apoptosis induced by TRAIL was determined by 7-aminoactinomycin D (7-AAD) staining as described previously (14) and quantitated by fluorescence-activated cell sorter (FACS) analysis of 7-AAD+ CD3+ cells. The data are represented as the means of three replicates of each dose of sDR5.
Preparation of sDR5.
DR5-Fc (sDR5) was purified from serum-free culture supernatant of AdsDR5-transfected cells. The supernatant was applied to a column of protein G-agarose (Sigma). sDR5 was eluted from the column with acidic elution buffer (100 mM glycine-HCl, pH 2.5) and neutralized with 1 M Tris-HCl, pH 9.0. sDR5 was concentrated to 500 μg/ml with an Amicon Ultrafree filter (Millipore Corporation, Bedford, Mass.), and aliquots were frozen for future use. The concentration of the purified sDR5 was determined by measurement of the absorbance at 280 nM using a spectrophotometer (SMART SPECTTM3000; Bio-Rad Laboratories, Hercules, Calif.), and the binding of the activity of the purified sDR5 to an anti-DR5 antibody (Imgenex, San Diego, Calif.) was determined by enzyme-linked immunosorbent assay (ELISA) as described previously (16).
Mice and treatments.
Eight-week-old BALB/c mice were purchased from Jackson Laboratory (Bar Harbor, Mass.) and housed at the University of Alabama at Birmingham Animal Facility. Mice were first treated with PBS, sTNFR1 (10 μg/mouse) as described previously (54), AdsDR5 (109 PFU/mouse), AdCMVGFP (109 PFU/mouse), and AdsDR5 (109 PFU/mouse) plus sTNFR1 (10 μg/mouse). After pretreatment, the mice were intravenously (i.v.) injected with AdCMVLacZ (109 PFU/mouse). sTNFR1 was administered at days −1, 0, and 1 relative to the time of AdCMVLacZ injection (52). A single dose of AdsDR5 was administered at day −3 relative to injection of AdCMVLacZ. Three mice from each group were sampled for analysis of lacZ gene expression. β-Galactosidase (β-Gal) was evaluated by harvesting the liver at different time points including 3, 7, 21, 30, and 50 days after administration of AdCMVLacZ (109 PFU/mouse; three mice per group). Since AdCMVGFP (109 PFU/mouse) led to a dramatic drop in LacZ expression 7 days after AdCMVLacZ injection, we did not further monitor LacZ expression in this group of mice.
Expression of LacZ in the liver.
Hepatic expression of LacZ in different treatment groups was determined by sacrificing mice at days 3 and 30 and staining with β-Gal as previously described. In brief, the frozen sections were fixed in fresh 4% paraformaldehyde in PBS for 1 h at 4°C, rinsed, and stained with 0.1% X-Gal (5-bromo-4-chloro-3-indolyl-β-d-galactopyranoside), 5 mM K3Fe(CN)6, and 5 mM K4Fe(CN)6 for 24 h at 25°C in a dark room overnight.
β-Gal activity in the liver lysate was measured with the Galacto-light β-Gal detection kit (Tropix Inc., Bedford, Mass.). Briefly, 100 mg of liver was homogenized in 1 ml of lysis solution. The protein concentration of the lysate was determined, and 100 μg of lysate was used for quantitation of β-Gal activity. Recombinant β-Gal (Sigma) was used as a positive control, and liver lysate from nontransfected mice was used as a negative control. The final reaction mixture containing light-emitting substrates was measured with a luminometer (Wallace Instrument Co.), and the results of the β-Gal activity were calculated as counts per milligram of total liver protein per minute.
Analysis of AdCMVLacZ DNA per liver cell.
To determine the amounts of AdCMVLacZ DNA in the liver after the treatments described above, total viral genomic DNA was extracted from livers and subjected to Southern dot blot analysis as previously described. In brief, to determine the vector copy number per cell in the transduced livers of AdCMVLacZ-injected mice, 20 μg of viral genomic DNA extracted from livers was blotted together with copy number standards (pAdeasysDR5) and subjected to Southern blot analysis as described previously (53) with a 3.0-kb lacZ vector sequence-specific probe. The intensity of the dots was quantitated by densitometry (Bio-Rad). The number of DNA particles per 100 cells was determined by multiplying by 100.
Analysis of hepatocyte apoptosis by Hoechst staining.
The liver was sectioned and Hoechst staining was performed as previously described (51). The liver was excised and fixed with 10% buffered formalin prior to being embedded in paraffin. Sections were obtained from the paraffin-embedded tissue samples and stained with hematoxylin and eosin and with Hoechst dye 33342 (Molecular Probes, Inc. Eugene, Oreg.). Hoechst staining was performed as follows: after fixation, the sections were incubated with blocking buffer (5% FCS, 0.1% NaN3 in PBS) for 20 min, incubated with 2 μg of Hoechst 33342/ml in blocking buffer for 7 min, and washed with PBS. Fluorescence was visualized with a standard fluorescence microscope.
Analysis of levels of AST, IL-6, TNF-α, and IFN-γ in serum.
Blood samples were collected at 24 h before and at different times after treatments, and liver enzyme AST was quantified in the clinical chemistry laboratory of University of Alabama at Birmingham hospital. IL-6, TNF-α, and IFN-γ levels in mouse sera were measured by an ELISA kit (BioSource International, Inc., Camarillo, Calif.).
Analysis of NK cytotoxic activity.
NK target cell YAC-1 was obtained from the American Type Culture Collection (Bethesda, Md.). The cells were cultured in Dulbecco’s modified Eagle medium (DMEM) with 10% FCS. The cytotoxicity of spleen NK cells was analyzed as follows. A single-cell suspension of spleen cells was layered on Ficoll-Paque (Pharmacia LKB, Uppsala, Sweden) and centrifuged at 400 × g for 30 min at 18°C. The lymphocyte layers were then harvested and washed twice with RPMI 1640 and used as effector cells. For the preparation of target cells, YAC-1 was labeled with [51Cr]Na2CrO4 (Amersham, Arlington Heights, Ill.). YAC-1 cells (1.0 × 104) were mixed with various numbers of spleen cells in a total volume of 200 μl of DMEM with 10% FCS. The plates were incubated at 37°C for 4 h, and the experimental radioactivity released (ER) in 100-μl samples of cell-free supernatants was determined. The amounts of radioactivity released in the wells containing YAC-1 cells alone with and without 0.01% Triton X-100 were designated the total release (TR) and the spontaneous release (SR), respectively. The percentage of specific 51Cr release was calculated by [(ER − SR)/(TR − SR)] × 100.
RESULTS
sDR5 protects mouse spleen T cells from TRAIL-mediated apoptosis.
AdsDR5 was constructed as shown in Fig. 1A by using the 133-amino-acid extracellular domain of DR5 (DR5-ED) ligated in frame to the human immunoglobulin G1 Fc. DR5-Fc (sDR5) was cloned into the BglII site of pAdTRACKCMV to produce pAdTRACKCMVsDR5 (Fig. 1). After homologous recombination in vitro with pAdEasy1, the recombinant AdsDR5 adenovirus was produced in 293 cells. To determine if the sDR5 produced by this AdsDR5 could protect mouse T cells against TRAIL-mediated apoptosis, CD3-activated T cells were treated with different doses of affinity-purified sDR5 isolated from the supernatant of AdsDR5-transfected 293 cells and incubated in vitro with recombinant TRAIL (1 nM) for 18 h. T-cell apoptosis was determined by 7-AAD staining followed by FACS analysis. Over 80% of T cells treated with TRAIL in the absence of sDR5 underwent apoptosis (Fig. 1B, left bar). After treatment with sDR5, there was a significant and dose-dependent protection of spleen T cells from TRAIL-mediated apoptosis. Treatment with 25 nM sDR5 reduces TRAIL-mediated T-cell apoptosis to background levels. These results indicate that TRAIL is a potent inducer of apoptosis of activated mouse T cells and that treatment with sDR5 produced from AdsDR5 results in protection against TRAIL-mediated apoptosis.
Prolonged transgene expression after blocking TRAIL-mediated apoptosis.
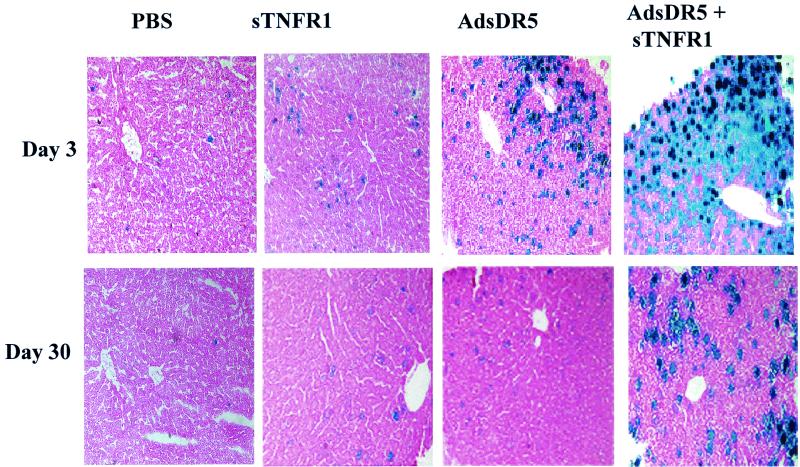
Mice were either untreated or treated with sTNFR1 (10 μg/mouse) on days −1, 0, and 1. Additional groups of mice were pretreated at day −3 with AdsDR5 with and without treatment with sTNFR1 at the same dose and time as described above. At day 0, mice were then injected with AdCMVLacZ (109 PFU/mouse i.v.). LacZ expression was determined by immunohistochemical staining at days 3 and 30. There was low LacZ expression in the liver after PBS treatment at both day 3 and day 30 (Fig. 2). Treatment with sTNFR1 resulted in an enhanced expression of LacZ at both days 3 and 30, consistent with our previous results (54). Pretreatment with AdsDR5 (109 PFU/mouse) at day −3, followed by administration of AdCMVLacZ (109 PFU/mouse) on day 0 resulted in a higher expression of LacZ than treatment with sTNFR1 at both days 3 and 30 (Fig. 2). Combined treatment with AdsDR5 and sTNFR1 prior to administration of AdCMVLacZ resulted in a synergistic enhancement of expression of LacZ at both days 3 and 30. These results indicate that treatment with AdsDR5, which blocks TRAIL-mediated apoptosis of liver cells, increases and prolongs the expression of AdCMVLacZ in gene therapy.
FIG. 2.
Histological analysis of β-Gal in the liver. Mice (three mice/group) were treated with either control PBS, sTNFR1 (10 ng/ml), AdsDR5 (109 PFU/mouse), or both sTNFR1 and AdsDR5 3 days before AdCMVLacZ i.v. injection. Mice were sacrificed on days 3 and 30 after AdCMVLacZ injection and evaluated for β-Gal expression. The figures are representative of five randomly selected areas. Magnification, ×31.
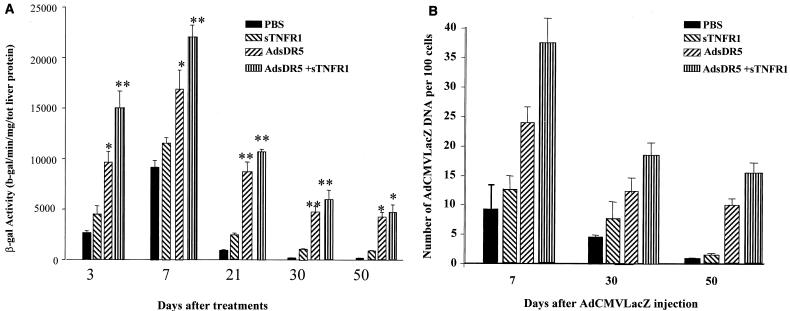
This increased expression of AdCMVLacZ in the liver was also quantified by evaluation of β-Gal activity by calorimetric analysis at days 3, 7, 21, 30, and 50 after these same treatment protocols. At all time points, pretreatment with AdsDR5 resulted in increased expression of β-Gal compared to treatment with sTNFR1 (Fig. 3A). The greatest increase in both magnitude and duration of AdCMVLacZ gene therapy expression was seen after combined treatment with both AdsDR5 and sTNFR1.
FIG. 3.
(A) Evaluation of β-Gal activity in liver. Mice were treated with PBS, sTNFR1, AdsDR5, or AdsDR5 plus sTNFR1 3 days before the i.v. administration of AdCMVLacZ. Mice were sacrificed at 3, 7, 21, 30, and 50 days after AdCMVLacZ administration, and the β-Gal activity was determined with a spectrophotometer. ∗, P < 0.05; ∗∗, P < 0.01. (B) AdCMVLAcZ-transduced liver cells were eliminated rapidly. Mice were treated as described above. Mice were sacrificed at days 7, 30, and 50 after AdCMVLacZ treatment, and the copy numbers of AdCMVLacZ DNA in liver cells were determined by dot blot hybridization using a [32P]dCTP-labeled LacZ probe. The intensity of the dots was quantitated by densitometry (Bio-Rad). The number of DNA particles per 100 cells was determined by multiplying by 100. Each data point represents the mean ± standard error of the mean of at least three mice per group at each time point.
To distinguish between the ability of cytokines to suppress expression of AdCMVLacZ by the liver cells and the dropout of recombinant AdCMVLacZ viral DNA due to apoptosis of liver cells, viral genomic DNAs were isolated from the livers of mice that were pretreated with PBS, sTNR1, AdsDR5, or combined therapy at different time points after injection of AdCMVLacZ (109 PFU/mouse i.v.) and dot blot hybridization was carried out. At 7, 30, and 50 days after injection of AdCMVLacZ, there was a loss of viral DNA that correlated with the loss of LacZ expression. (Fig. 3B). These results indicate that decreased expression of β-Gal was due to loss of liver cells containing the AdCMVLacZ DNA and not due to down-regulation of the expression of AdCMVLacZ.
AdsDR5 blocks hepatocyte apoptosis after AdCMVLacZ injection.
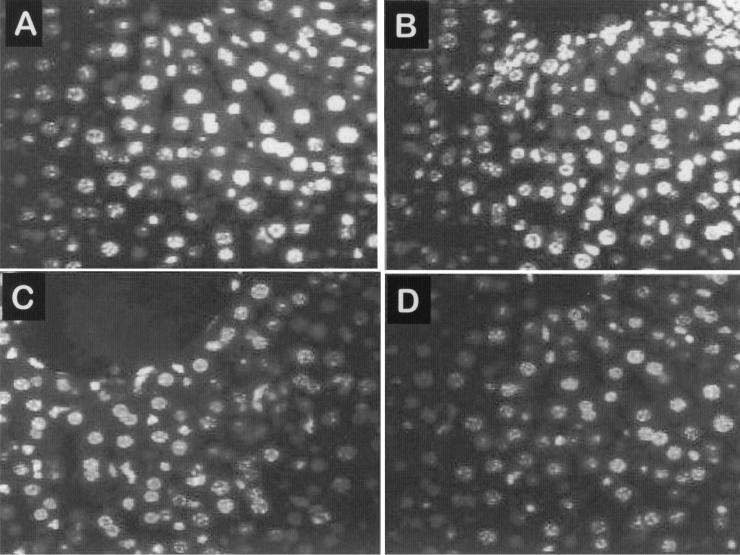
Since loss of LacZ expression by the liver was correlated with the loss of AdCMVLacZ DNA contained by liver cells, we wanted to determine if treatment with AdsDR5 or sTNFR1 or combined treatment followed by injection with AdCMVLacZ inhibited apoptosis of liver cells. Mice were sacrificed at day 7, and the livers were sectioned and stained. The nuclei of hepatocytes were visualized by Hoechst staining. There was high apoptosis of hepatocytes in control PBS-treated mice 7 days after they received 109 PFU of AdCMVLacZ, as indicated by a condensed nuclear pattern and more-intense Hoechst staining (Fig. 4A). There was also high apoptosis in mice treated with sTNFR1 followed by administration of AdCMVLacZ (Fig. 4B). The apoptosis was greatly reduced in mice pretreated with either AdsDR5 or AdsDR5 in combination with sTNFR1 and treated with AdCMVLacZ (Fig. 4C and D). These results indicate that treatment with AdsDR5 protects hepatocytes from AdCMVLacZ-induced apoptosis.
FIG. 4.
Hepatocyte apoptosis after AdCMVLacZ injection. Mice were treated as described for Fig. 3A with either PBS (A), sTNFR1 (B), AdsDR5 (C), or combined AdsDR5 plus sTNFR1 (D) 3 days before i.v. injection of AdCMVLacZ (109 PFU/mouse). Mice were sacrificed at day 7, and the livers were sectioned and stained with Hoechst. The results are representative of five randomly chosen sections of the livers.
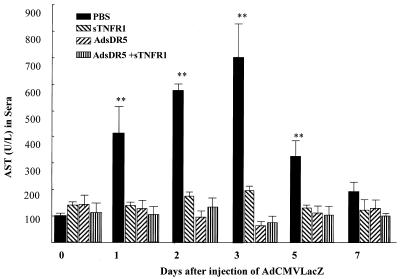
AdsDR5 and sTNFR1 treatment prevents liver enzyme AST release.
Mice were treated, as described above, with either AdsDR5, sTNFR1, or both and then injected on day 0 with 109 PFU of AdCMVLacZ. AST in the serum was determined on days 0, 1, 2, 3, 5, and 7 (Fig. 5). Compared to those on day 0, there was a significant increase in serum AST levels on days 1, 2, 3, and 5 in control mice treated with PBS followed by injection with AdCMVLacZ. There was no significant increase in AST in mice treated with sTNFR1, AdsDR5, or the two combined (Fig. 5). These results indicate that AdsDR5, TNFR1, and combined therapy can prevent AdCMVLacZ-mediated hepatotoxicity.
FIG. 5.
AdsDR5 treatment prevents liver enzyme AST release. Mice were treated as described for Fig. 3A, and the serum AST values were determined at days 0, 1, 2, 3, 5, and 7 after administration of AdCMVLacZ. The results represent the means ± standard errors of the means for at least three mice per group. ∗∗, values that are significantly different from those for the other groups (P < 0.01).
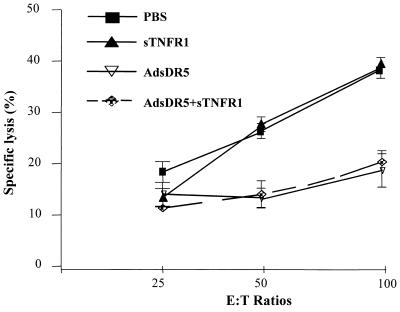
AdsDR5 blocks NK cell activation.
TRAIL has been reported to increase NK cell activity (37, 40, 49). To determine if blocking TRAIL with AdsDR5 could block adenovirus-induced NK cell cytotoxicity, mice were treated as described above with either AdsDR5 or sTNFR1 followed by injection of AdCMVLacZ (109 PFU/mouse i.v.). The mice were sacrificed at day 7, and the spleen lymphocytes were assayed at different effector-to-target cell ratios for the ability to kill 51Cr-labeled major histocompatibility complex class I-negative YAC-1 target cells. There was a significant increase in NK activity after mice were injected with AdCMVLacZ and treated with PBS or sTNFR1 alone (Fig. 6). In contrast, treatment with AdsDR5 followed by treatment with AdCMVLacZ prevented development of NK cell activity. These results indicate that treatment with AdsDR5 can inhibit induction of NK cells in response to AdCMVLacZ.
FIG. 6.
Activation of NK cell activity after administration of AdCMVLacZ. Mice (three to five mice/group) were treated with PBS, sTNFR1, AdsDR5, or AdsDR5 plus sTNFR1 as described for Fig. 3A. At day 7 after administration of AdCMVLacZ (109 PFU/cell) the mice were sacrificed and spleen cells were isolated as described in Materials and Methods. 51Cr-labeled YAC-1 target cells (104) were mixed with different numbers of spleen cells at different effector-to-target cell (E:T) ratios. The specific lysis was determined after incubation at 37°C for 4 h. Each data point represents the mean ± standard error of the mean for at least three mice per group.
AdsDR5, which blocks TRAIL, prevents production of TNF-α and IFN-γ.
We and others have previously shown that production of TNF-α and IFN-γ limits adenovirus gene therapy product expression and persistence in liver cells (5, 9, 51, 54). The present results indicate that AdsDR5 prolongs gene therapy product expression better than pretreatment with sTNFR1. One source of IFN-γ is NK cells, and macrophages are a potent source of TNF-α. To determine whether production of these cytokines could be reduced by blocking TRAIL, mice were pretreated with either the control, sTNFR1, AdsDR5, or both sTNFR1 and AdsDR5 followed by injection with AdCMVLacZ (109 PFU/mouse i.v.). TNF-α, IFN-γ, and IL-6 levels in sera were determined by ELISA at different times after administration of AdCMVLacZ (Table 1). There was high induction of serum TNF-α and IFN-γ levels within 1 day and greater induction by days 2 and 3 in mice pretreated with control PBS and then treated with AdCMVLacZ. As might be anticipated, the administration of AdCMVGFP 3 days after administration of AdCMVLacZ resulted in higher levels of TNF-α, IFN-γ, and IL-6 at all time points between 6 and 72 h than administration of PBS. Pretreatment with sTNFR1 alone neutralized serum TNF-α production but only partially blocked the elevation of IFN-γ and IL-6. Treatment with AdsDR5 alone, followed by treatment with AdCMVLacZ, suppressed the induction of TNF-α and IFN-γ in the serum and suppressed production of IL-6 compared to levels after challenge with AdCMVGFP. These results indicate that blocking the TRAIL-DR5 interaction with AdsDR5 also blocks AdCMVLacZ-induced TNF-α and IFN-γ and the associated hepatocytoxicity. The decreased production of cytokines after administration of AdsDR5 3 days after AdCMVLacZ is made even more significant by the observation that delivery of a second adenovirus without regulatory effects and anti-inflammatory effects (AdCMVGFP) leads to an increase in proinflammatory cytokines. Thus, treatment with AdsDR5 inhibits direct TRAIL-DR5-mediated apoptosis of liver cells, as well as blocking indirect pathways of hepatocytotoxicity involving both NK cells and induction of TNF-α and IFN-γ production.
TABLE 1.
Serum cytokine levels following i.v. delivery of AdCMVLacZ after five different treatmentsa
| Treatment group | Serum cytokine | Levelb at indicated time (h) after treatment
|
||||||
|---|---|---|---|---|---|---|---|---|
| 0 | 6 | 12 | 24 | 72 | 120 | 168 | ||
| PBS | IL-6 | <10.03 | 12.2 ± 2.4 | 25.4 ± 6.5 | 40.4 ± 9.3 | 51.4 ± 10.2 | 12.0 ± 2.8 | 2.2 ± 1.1 |
| TNF-α | <10 | <10 | 28 ± 5.7 | 36.6 ± 5.4 | 74.2 ± 8.8 | 32.9 ± 11 | 16.9 ± 10.2 | |
| IFN-γ | <10 | <10 | <10 | 18.5 ± 2.8 | 106 ± 4.8 | 98.4 ± 11 | 159.9 ± 15.7 | |
| AdCMVGFP | IL-6 | 8.8 ± 2 | 14 ± 6.4 | 31.1 ± 0.4 | 60.6 ± 11 | 58.2 ± 8.4 | 10.2 ± 6.4 | 1.2 ± 0.7 |
| TNF-α | <10 | 11.0 ± 3.2 | 32.2 ± 4.9 | 58.8 ± 12 | 78.2 ± 14 | 33.2 ± 15 | 19.2 ± 9.2 | |
| IFN-γ | <10 | 21.0 ± 9.3 | 47.2 ± 16 | 68.3 ± 1.3 | 94.2 ± 6.9 | 102.8 ± 11 | 146.3 ± 5.6 | |
| sTNFR1 | IL-6 | <0.03 | 4.7 ± 0.4 | 14.7 ± 0.4 | 34.6 ± 5.4 | 38.4 ± 9.5 | 5.8 ± 6.9 | <0.03 |
| TNF-α | <10 | <10 | <10 | <10 | 15.7 ± 6.9 | <10 | <10 | |
| IFN-γ | <10 | <10 | <10 | 15.4 ± 3.8 | 89.4 ± 12 | 78.4 ± 12 | 106.3 ± 18 | |
| AdsDR5 | IL-6 | <0.03 | <0.03 | 13.4 ± 2.1 | 42.8 ± 2.8 | 36.4 ± 1.6 | 6.1 ± 2.9 | <0.03 |
| TNF-α | <10 | <10 | <10 | 16.4 ± 8.7 | 15.8 ± 5.5 | <10 | <10 | |
| IFN-γ | <10 | <10 | <10 | <10 | 24.3 ± 5.6 | <10 | <10 | |
| AdsDR5 + sTNFR1 | IL-6 | <0.03 | <0.03 | 15.9 ± 6/8 | 36.6 ± 4.9 | 41.2 ± 2.2 | 9.2 ± 1.8 | <0.03 |
| TNF-α | <10 | <10 | <10 | <10 | <10 | <10 | <10 | |
| IFN-γ | <10 | <10 | <10 | <10 | <10 | <10 | <10 | |
Mice were treated with control PBS, AdCMVGFP (109 PFU), sTNFRI (10 μg/mouse), AdsDR5 (109 PFU), or AdsDR5 plus sTNFR1. Three days later, mice were injected with AdCMVLacZ (109 PFU/mouse i.v.) and serum TNF-α, IFN-γ, and IL-6 levels were determined by ELISA at 0, 6, 12, 24, 72, 120, and 168 h after administration of AdCMVLacZ. The results are means ± standard errors of the means for at least three mice per group.\
Units for IL-6 levels are nanograms per milliliter; units for TNF-α and IFN-γ levels are picograms per milliliter.
DISCUSSION
Adenovirus can alter the susceptibility of different cells to TRAIL-mediated apoptosis. Routes et al. (34) have shown that expression of the adenovirus serotype 5 (Ad5) E1A oncogene sensitizes cells to apoptosis by TNF-α and Fas ligand. In contrast, the E3 gene products and, to a lesser extent, E1B-19K inhibit this effect. Benedict et al. (4) and Tollefson et al. (41) have shown that the viral E3 protein, with a molecular weight of 6,700 (6.7K), functions in the specific modulation of the two death receptors for TRAIL. The 6.7K protein is expressed on the cell surface and forms a complex with the 10.4K and 14.5K proteins, and this complex is sufficient to induce down-modulation of TRAIL receptors 1 and 2 from the cell surface and to reverse the sensitivity of infected cells to TRAIL-mediated apoptosis. These results suggest that subversion of this pathway by adenovirus is a natural mechanism of the adenovirus E3 protein to avoid TRAIL-mediated apoptosis of adenovirus-infected cells and that the TRAIL apoptosis pathway plays a key role in elimination of cells that express adenovirus. This is consistent with the present results that pretreatment of mice with AdsDR5, which induces expression of sDR5 capable of neutralizing TRAIL, greatly inhibited liver cell apoptosis and prolonged lacZ gene expression after subsequent administration of AdCMVLacZ.
A second mechanism by which pretreatment with AdsDR5 may inhibit liver cell apoptosis after AdCMVLacZ treatment is by inhibition of NK cell activation and production of cytokines including IFN-γ. Several investigators (1, 8, 28, 35, 39) have shown that NK cells are a relatively rare cell population in peripheral lymphoid organs but are abundant in the liver. An initial response to viral infection primarily involves the innate arm of the immune response resulting in killing of infected cells by NK cells. Once the virus has invaded the cell, however, a second host defense-mediated response, which involves the induction of IFNs, is triggered. Several investigators (3, 37) have shown that IFN-γ induces a number of intracellular genes that directly prevent virus replication or genes that facilitate apoptosis, including TRAIL. Liu et al. (23) have shown that, after adenovirus administration, liver NK cells cause hepatocyte apoptosis associated with an increase in liver enzymes in the serum. The findings in this paper are novel since they suggest that TRAIL is a mediator in a positive-amplification loop that results in further stimulation of NK cells and production of IFN-γ. Such a positive-feedback loop involving TRAIL has been previously proposed by Oshima et al. (29). We propose that TRAIL production, similar to production of other cytokines, including IL-12 and IL-18, is stimulated by adenovirus gene therapy and that TRAIL serves as an important regulator of a positive-feedback loop for further NK cell activation and cytokine production by other cells in the liver. Interruption of this positive-feedback loop by preadministration of AdsDR5 nearly completely inhibits NK cell activation and production of hepatotoxic cytokines, including TNF-α and IFN-γ. Reduction of all of these factors leads to greatly prolonged gene therapy expression.
We and other investigators have shown that AdCMVLacZ treatment leads to induction of TNF-α, which has been proposed to be produced by Kupffer cells in the liver (27). Consistent with our previous report (54) administration of sTNFRI neutralizes AdCMVLacZ-induced TNF-α and prolongs gene therapy. However, blockade of TRAIL interactions with its receptor by pretreatment with AdsDR5 also reduced TNF-α and IFN-γ production, suggesting that AdCMVLacZ-induced TRAIL production in the liver is a highly significant event that influences the production of multiple cytokines, including IFN-γ and TNF-α, that limits gene therapy expression. Administration of AdCMVGFP 3 days after administration of AdCMVLacZ resulted in higher levels of TNF-α, IFN-γ, and IL-6 at all time points between 6 and 72 h than administration of PBS, indicating that administration of AdsDR5 also inhibited IL-6 more than a second administration of a control adenovirus.
Although pretreatment with AdsDR5 inhibits hepatotoxicity, as determined by measurement of AST, and apoptosis of hepatocytes, as determined by Hoechst staining, other mechanisms that regulate the level of lacZ gene expression in the liver were investigated. Several investigators have reported that certain cytokines including IFN-γ and TNF-α can down-regulate CMV promoter activity and affect lacZ gene therapy (30, 33). To distinguish between the effects of cytokines on promoter activation and vector chromosome dropout, dot blot hybridization of the lacZ gene in liver cells was examined at 7, 30, and 50 days after AdCMVLacZ injection. The results indicate that the major decrease in lacZ gene expression was due to vector chromosome dropout, which would result from hepatocyte cell death, and that decreased expression was not due to inhibitory effects of cytokines on CMV promoter activity.
Very low serum sDR5 levels were present after administration of AdsDR5 (109 PFU/mouse) i.v. Serum sDR5 levels as determined by an ELISA were 172 ± 27 and 89 ± 11 pg/ml on days 6 and 10, respectively, after injection of AdsDR5. Since the AdsDR5 was administered 3 days prior to injection of AdCMVLacZ, these levels correspond to days 3 and 7 after AdCMVLacZ injection, respectively. Serum sDR5 levels are not detectable at earlier or later time points. These results indicate that low serum sDR5 levels are associated with the inhibition of the acute effects of the administration of AdCMVLacZ. It is likely that intrahepatic levels of sDR5 may be higher than serum levels, and this may account for the strong inhibition of production of TNF-α and IFN-γ and hepatocellular damage after administration of AdCMVLacZ.
In summary, pretreatment with AdsDR5 results in relatively low serum sDR5 levels capable of blocking TRAIL interactions with its receptor in the liver. This leads to prolonged expression after subsequent administration of AdCMVLacZ, which was associated with decreased hepatocellular damage and decreased hepatocyte apoptosis. The decreased apoptosis was likely due to both direct inhibition of TRAIL-mediated apoptosis of hepatocytes and inhibition of a novel positive-feedback amplification loop by TRAIL. Inhibition of this novel positive-amplification feedback loop of TRAIL results in decreased NK cell activation and decreased production of IFN-γ and TNF-α, which greatly reduce hepatocellular damage after administration of AdCMVLacZ. Experiments to determine the effect of these treatments on the T-cell and B-cell antibody response to adenovirus are under way.
Acknowledgments
We thank T. Rogers and M. Spell of the FACS Core Facility at UAB for operating the FACS. We also thank Deidre Downs for critical review of the manuscript and Linda Flurry for excellent secretary work.
H.-C. Hsu is a recipient of a grant from the Center for Aging at the University of Alabama at Birmingham. H.-G. Zhang is a recipient of an Arthritis Foundation Investigator Award. This work was supported by NIH grants R01 AG 11653, N01 AR 6-2224, and RO1 AI 42900 and a Birmingham VAMC Merit Review Grant to J.D.M. and H.-G.Z.
REFERENCES
- 1.Abo, T., T. Kawamura, and H. Watanabe. 2000. Physiological responses of extrathymic T cells in the liver. Immunol. Rev. 174:135-149. [DOI] [PubMed] [Google Scholar]
- 2.Ashkenazi, A., and V. M. Dixit. 1999. Apoptosis control by death and decoy receptors. Curr. Opin. Cell Biol. 11:255-260. [DOI] [PubMed] [Google Scholar]
- 3.Barber, G. N. 2000. The interferons and cell death: guardians of the cell or accomplices of apoptosis? Semin. Cancer Biol. 10:103-111. [DOI] [PubMed] [Google Scholar]
- 4.Benedict, C. A., P. S. Norris, T. I. Prigozy, J. L. Bodmer, J. A. Mahr, C. T. Garnett, F. Martinon, J. Tschopp, L. R. Gooding, and C. F. Ware. 2001. Three adenovirus E3 proteins cooperate to evade apoptosis by tumor necrosis factor-related apoptosis-inducing ligand receptor-1 and -2. J. Biol. Chem. 276:3270-3278. [DOI] [PubMed] [Google Scholar]
- 5.Benihoud, K., I. Saggio, P. Opolon, B. Salone, F. Amiot, E. Connault, C. Chianale, F. Dautry, P. Yeh, and M. Perricaudet. 1998. Efficient, repeated adenovirus-mediated gene transfer in mice lacking both tumor necrosis factor alpha and lymphotoxin alpha. J. Virol. 72:9514-9525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cheng, J., T. Zhou, C. Liu, J. P. Shapiro, M. J. Brauer, M. C. Kiefer, P. J. Barr, and J. D. Mountz. 1994. Protection from Fas-mediated apoptosis by a soluble form of the Fas molecule. Science 263:1759-1762. [DOI] [PubMed] [Google Scholar]
- 7.Clement, M. V., and I. Stamenkovic. 1994. Fas and tumor necrosis factor receptor-mediated cell death: similarities and distinctions. J. Exp. Med. 180:557-567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Crispe, I. N., T. Dao, K. Klugewitz, W. Z. Mehal, and D. P. Metz. 2000. The liver as a site of T-cell apoptosis: graveyard, or killing field? Immunol. Rev. 174:47-62. [DOI] [PubMed] [Google Scholar]
- 9.Elkon, K. B., C. C. Liu, J. G. Gall, J. Trevejo, M. W. Marino, K. A. Abrahamsen, X. Song, J. L. Zhou, L. J. Old, R. G. Crystal, and E. Falck-Pedersen. 1997. Tumor necrosis factor alpha plays a central role in immune-mediated clearance of adenoviral vectors. Proc. Natl. Acad. Sci. USA 94:9814-9819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Fearon, D. T., and R. M. Locksley. 1996. The instructive role of innate immunity in the acquired immune response. Science 272:50-53. [DOI] [PubMed] [Google Scholar]
- 11.Galle, P. R., W. J. Hofmann, H. Walczak, H. Schaller, G. Otto, W. Stremmel, P. H. Krammer, and L. Runkel. 1995. Involvement of the CD95 (APO-1/Fas) receptor and ligand in liver damage. J. Exp. Med. 182:1223-1230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gores, G. J., and S. H. Kaufmann. 2001. Is TRAIL hepatotoxic? Hepatology 34:3-6. [DOI] [PubMed] [Google Scholar]
- 13.He, T. C., S. Zhou, L. T. da Costa, J. Yu, K. W. Kinzler, and B. Vogelstein. 1998. A simplified system for generating recombinant adenoviruses. Proc. Natl. Acad. Sci. USA 95:2509-2514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hsu, H. C., L. D. Shultz, X. Su, J. Shi, P. A. Yang, M. J. Relyea, H. G. Zhang, and J. D. Mountz. 2001. Mutation of the hematopoietic cell phosphatase (Hcph) gene is associated with resistance to gamma-irradiation-induced apoptosis in Src homology protein tyrosine phosphatase (SHP)-1-deficient “motheaten” mutant mice. J. Immunol. 166:772-780. [DOI] [PubMed] [Google Scholar]
- 15.Hsu, H. C., T. Zhou, J. Shi, P. A. Yang, D. Liu, H. G. Zhang, H. Bluethmann, and, J. D. Mountz. 2001. Aged mice exhibit in vivo defective peripheral clonal deletion of D(b)/H-Y reactive CD8+ T cells. Mech. Ageing Dev. 122:305-326. [DOI] [PubMed] [Google Scholar]
- 16.Ichikawa, K., W. Liu, L. Zhao, Z. Wang, D. Liu, T. Ohtsuka, H. Zhang, J. D. Mountz, W. J. Koopman, R. P. Kimberly, and, T. Zhou. 2001. Tumoricidal activity of a novel anti-human DR5 monoclonal antibody without hepatocyte cytotoxicity. Nat. Med. 7:954-960. [DOI] [PubMed] [Google Scholar]
- 17.Jelachich, M. L., and H. L. Lipton. 2001. Theiler's murine encephalomyelitis virus induces apoptosis in gamma interferon-activated M1 differentiated myelomonocytic cells through a mechanism involving tumor necrosis factor alpha (TNF-α) and TNF-α-related apoptosis-inducing ligand. J. Virol. 75:5930-5938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Jo, M., T. H. Kim, D. W. Seol, J. E. Esplen, K. Dorko, T. R. Billiar, and S. C. Strom. 2000. Apoptosis induced in normal human hepatocytes by tumor necrosis factor-related apoptosis-inducing ligand. Nat. Med. 6:564-567. [DOI] [PubMed] [Google Scholar]
- 19.Kolls, J., K. Peppel, M. Silva, and B. Beutler. 1994. Prolonged and effective blockade of tumor necrosis factor activity through adenovirus-mediated gene transfer. Proc. Natl. Acad. Sci. USA 91:215-219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kolls, J. K., D. Lei, S. Nelson, W. R. Summer, S. Greenberg, and B. Beutler. 1995. Adenovirus-mediated blockade of tumor necrosis factor in mice protects against endotoxic shock yet impairs pulmonary host defense. J. Infect. Dis. 171:570-575. [DOI] [PubMed] [Google Scholar]
- 21.Lawrence, D., Z. Shahrokh, S. Marsters, K. Achilles, D. Shih, B. Mounho, K. Hillan, K. Totpal, L. DeForge, P. Schow, J. Hooley, S. Sherwood, R. Pai, S. Leung, L. Khan, B. Gliniak, J. Bussiere, C. A. Smith, S. S. Strom, S. Kelley, J. A. Fox, D. Thomas, and, A. Ashkenazi. 2001. Differential hepatocyte toxicity of recombinant Apo2L/TRAIL versions. Nat. Med. 7:383-385. [DOI] [PubMed] [Google Scholar]
- 22.Leist, M., F. Gantner, S. Jilg, and A. Wendel. 1995. Activation of the 55 kDa TNF receptor is necessary and sufficient for TNF-induced liver failure, hepatocyte apoptosis, and nitrite release. J. Immunol. 154:1307-1316. [PubMed] [Google Scholar]
- 23.Liu, Z. X., S. Govindarajan, S. Okamoto, and G. Dennert. 2000. NK cells cause liver injury and facilitate the induction of T cell-mediated immunity to a viral liver infection. J. Immunol. 164:6480-6486. [DOI] [PubMed] [Google Scholar]
- 24.Minter, R. M., J. E. Rectenwald, K. Fukuzuka, C. L. Tannahill, D. La Face, V. Tsai, I. Ahmed, E. Hutchins, R. Moyer, E. M. Copeland III, and L. L. Moldawer. 2000. TNF-alpha receptor signaling and IL-10 gene therapy regulate the innate and humoral immune responses to recombinant adenovirus in the lung. J. Immunol. 164:443-451. [DOI] [PubMed] [Google Scholar]
- 25.Ni, R., Y. Tomita, K. Matsuda, A. Ichihara, K. Ishimura, J. Ogasawara, and S. Nagata. 1994. Fas-mediated apoptosis in primary cultured mouse hepatocytes. Exp. Cell Res. 215:332-337. [DOI] [PubMed] [Google Scholar]
- 26.Ogasawara, J., R. Watanabe-Fukunaga, M. Adachi, A. Matsuzawa, T. Kasugai, Y. Kitamura, N. Itoh, T. Suda, and S. Nagata. 1993. Lethal effect of the anti-Fas antibody in mice. Nature 364:806-809. [DOI] [PubMed] [Google Scholar]
- 27.Onda, M., M. Willingham, Q. C. Wang, R. J. Kreitman, Y. Tsutsumi, S. Nagata, and I. Pastan. 2000. Inhibition of TNF-alpha produced by Kupffer cells protects against the nonspecific liver toxicity of immunotoxin anti-Tac(Fv)-PE38, LMB-2. J. Immunol. 165:7150-7156. [DOI] [PubMed] [Google Scholar]
- 28.Orange, J. S., T. P. Salazar-Mather, S. M. Opal, and C. A. Biron. 1997. Mechanisms for virus-induced liver disease: tumor necrosis factor-mediated pathology independent of natural killer and T cells during murine cytomegalovirus infection. J. Virol. 71:9248-9258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Oshima, K., N. Yanase, C. Ibukiyama, A. Yamashina, N. Kayagaki, H. Yagita, and, J. Mizuguchi. 2001. Involvement of TRAIL/TRAIL-R interaction in ifn-alpha-induced apoptosis of Daudi B lymphoma cells. Cytokine 14:193-201. [DOI] [PubMed] [Google Scholar]
- 30.Paillard, F. 1997. Promoter attenuation in gene therapy: causes and remedies. Hum. Gene Ther. 8:2009-2010. [PubMed] [Google Scholar]
- 31.Peng, Y., E. Falck-Pedersen, and K. B. Elkon. 2001. Variation in adenovirus transgene expression between BALB/c and C57BL/6 mice is associated with differences in interleukin-12 and gamma interferon production and NK cell activation. J. Virol. 75:4540-4550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Pitti, R. M., S. A. Marsters, S. Ruppert, C. J. Donahue, A. Moore, and A. Ashkenazi. 1996. Induction of apoptosis by Apo-2 ligand, a new member of the tumor necrosis factor cytokine family. J. Biol. Chem. 271:12687-12690. [DOI] [PubMed] [Google Scholar]
- 33.Qin, L., Y. Ding, D. R. Pahud, E. Chang, M. J. Imperiale, and J. S. Bromberg. 1997. Promoter attenuation in gene therapy: interferon-gamma and tumor necrosis factor-alpha inhibit transgene expression. Hum. Gene Ther. 8:2019-2029. [DOI] [PubMed] [Google Scholar]
- 34.Routes, J. M., S. Ryan, A. Clase, T. Miura, A. Kuhl, T. A. Potter, and, J. L. Cook. 2000. Adenovirus E1A oncogene expression in tumor cells enhances killing by TNF-related apoptosis-inducing ligand (TRAIL). J. Immunol. 165:4522-4527. [DOI] [PubMed] [Google Scholar]
- 35.Salazar-Mather, T. P., T. A. Hamilton, and C. A. Biron. 2000. A chemokine-to-cytokine-to-chemokine cascade critical in antiviral defense. J. Clin. Investig. 105:985-993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Shin, E. C., J. M. Ahn, C. H. Kim, Y. Choi, Y. S. Ahn, H. Kim, S. J. Kim, and J. H. Park. 2001. IFN-gamma induces cell death in human hepatoma cells through a TRAIL/death receptor-mediated apoptotic pathway. Int. J. Cancer 93:262-268. [DOI] [PubMed] [Google Scholar]
- 37.Smyth, M. J., E. Cretney, K. Takeda, R. H. Wiltrout, L. M. Sedger, N. Kayagaki, H. Yagita, and, K. Okumura. 2001. Tumor necrosis factor-related apoptosis-inducing ligand (TRAIL) contributes to interferon gamma-dependent natural killer cell protection from tumor metastasis. J. Exp. Med. 193:661-670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Suda, T., T. Takahashi, P. Golstein, and S. Nagata. 1993. Molecular cloning and expression of the Fas ligand, a novel member of the tumor necrosis factor family. Cell 75:1169-1178. [DOI] [PubMed] [Google Scholar]
- 39.Takahashi, M., K. Ogasawara, K. Takeda, W. Hashimoto, H. Sakihara, K. Kumagai, R. Anzai, M. Satoh, and S. Seki. 1996. LPS induces NK1.1+ alpha beta T cells with potent cytotoxicity in the liver of mice via production of IL-12 from Kupffer cells. J. Immunol. 156:2436-2442. [PubMed] [Google Scholar]
- 40.Takeda, K., Y. Hayakawa, M. J. Smyth, N. Kayagaki, N. Yamaguchi, S. Kakuta, Y. Iwakura, H. Yagita, and, K. Okumura. 2001. Involvement of tumor necrosis factor-related apoptosis-inducing ligand in surveillance of tumor metastasis by liver natural killer cells. Nat. Med. 7:94-100. [DOI] [PubMed] [Google Scholar]
- 41.Tollefson, A. E., K. Toth, K. Doronin, M. Kuppuswamy, O. A. Doronina, D. L. Lichtenstein, T. W. Hermiston, C. A. Smith, and W. S. Wold. 2001. Inhibition of TRAIL-induced apoptosis and forced internalization of TRAIL receptor 1 by adenovirus proteins. J. Virol. 75:8875-8887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Wiley, S. R., K. Schooley, P. J. Smolak, W. S. Din, C. P. Huang, J. K. Nicholl, G. R. Sutherland, T. D. Smith, C. Rauch, C. A. Smith, et al. 1995. Identification and characterization of a new member of the TNF family that induces apoptosis. Immunity 3:673-682. [DOI] [PubMed] [Google Scholar]
- 43.Wong, G. H., and D. V. Goeddel. 1994. Fas antigen and p55 TNF receptor signal apoptosis through distinct pathways. J. Immunol. 152:1751-1755. [PubMed] [Google Scholar]
- 44.Worgall, S., G. Wolff, E. Falck-Pedersen, and R. G. Crystal. 1997. Innate immune mechanisms dominate elimination of adenoviral vectors following in vivo administration. Hum. Gene Ther. 8:37-44. [DOI] [PubMed] [Google Scholar]
- 45.Yamanaka, T., K. Shiraki, K. Sugimoto, T. Ito, K. Fujikawa, M. Ito, K. Takase, M. Moriyama, T. Nakano, and A. Suzuki 2000. Chemotherapeutic agents augment TRAIL-induced apoptosis in human hepatocellular carcinoma cell lines. Hepatology 32:482-490. [DOI] [PubMed] [Google Scholar]
- 46.Yang, Y., and J. M. Wilson. 1995. Clearance of adenovirus-infected hepatocytes by MHC class I-restricted CD4+ CTLs in vivo. J. Immunol. 155:2564-2570. [PubMed] [Google Scholar]
- 47.Yang, Y., Z. Xiang, H. C. Ertl, and J. M. Wilson. 1995. Upregulation of class I major histocompatibility complex antigens by interferon gamma is necessary for T-cell-mediated elimination of recombinant adenovirus-infected hepatocytes in vivo. Proc. Natl. Acad. Sci. USA 92:7257-7261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Yasu, Y. M., H.-G. Zhang, H.-C. Hsu, P. Yang, D. Liu, K. Zinn, C. K. Edwards III, J. M. Mountz, T. Zhou, and J. D. Mountz. Soluble Fas gene therapy protects the liver from Fas-mediated apoptosis but not TNFα induced lethality. Death Differ., in press.
- 49.Zamai, L., M. Ahmad, I. M. Bennett, L. Azzoni, E. S. Alnemri, and B. Perussia. 1998. Natural killer (NK) cell-mediated cytotoxicity: differential use of TRAIL and Fas ligand by immature and mature primary human NK cells. J. Exp. Med. 188:2375-2380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Zhang, H. G., G. Bilbao, T. Zhou, J. L. Contreras, J. Gomez-Navarro, M. Feng, I. Saito, J. D. Mountz, and D. T. Curiel. 1998. Application of a Fas ligand encoding a recombinant adenovirus vector for prolongation of transgene expression. J. Virol. 72:2483-2490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Zhang, H. G., D. Liu, Y. Heike, P. Yang, Z. Wang, X. Wang, D. T. Curiel, T. Zhou, and J. D. Mountz. 1998. Induction of specific T-cell tolerance by adenovirus-transfected, Fas ligand-producing antigen presenting cells. Nat. Biotechnol. 16:1045-1049. [DOI] [PubMed] [Google Scholar]
- 52.Zhang, H. G., X. Su, D. Liu, W. Liu, P. Yang, Z. Wang, C. K. Edwards, H. Bluethmann, J. D. Mountz, and T. Zhou. 1999. Induction of specific T cell tolerance by Fas ligand-expressing antigen-presenting cells. J. Immunol. 162:1423-1430. [PubMed] [Google Scholar]
- 53.Zhang, H. G., J. Xie, P. Yang, Y. Wang, L. Xu, D. Liu, H. C. Hsu, T. Zhou, C. K. Edwards, and J. D. Mountz. 2000. Adeno-associated virus production of soluble tumor necrosis factor receptor neutralizes tumor necrosis factor alpha and reduces arthritis. Hum. Gene Ther. 11:2431-2442. [DOI] [PubMed] [Google Scholar]
- 54.Zhang, H. G., T. Zhou, P. Yang, C. K. Edwards III, D. T. Curiel, and J. D. Mountz. 1998. Inhibition of tumor necrosis factor alpha decreases inflammation and prolongs adenovirus gene expression in lung and liver. Hum. Gene Ther. 9:1875-1884. [DOI] [PubMed] [Google Scholar]