Abstract
Objective
To quantify the number of children who experience gaps in insurance coverage and to determine whether vulnerable subgroups of children experience noteworthy lapses in insurance coverage.
Methods
We analyzed nationally representative data from 24 149 children sampled in the 1999–2001 Medical Expenditure Panel Survey linked to the 1997–1999 National Health Interview Survey. Vulnerable subgroups of children included children with chronic conditions, those from ethnic/racial minorities, and those living in poverty. On the basis of cumulative annual monthly insurance coverage status, each child fell into 1 of 3 groups: continuous coverage, uninsured, or gaps in coverage. Using SAS-callable SUDAAN, we conducted multivariate ordinal logistic regression model to quantify the likelihood of having gaps in coverage for vulnerable subgroups of children.
Results
From 1999 to 2001, we found that > 9 million American children annually had gaps in coverage and that 5 to 6 million children annually were uninsured for the entire year. Sixty percent of children experienced gaps of at least 4 months, and > 40% of all publicly and privately insured children had coverage gaps. After accounting for relevant covariates, children with chronic conditions were just as likely as other children to have gaps in coverage or be uninsured; Hispanic children were most likely to have insurance gaps or be uninsured; and children from poor and near-poor families were 4 to 5 times more likely to have lapsed coverage than children from high-income families. Poverty and maternal education were the strongest factors associated with lapsed coverage.
Conclusions
Unstable health insurance is an underrecognized problem for children, including those with chronic conditions. Because unstable insurance coverage can lead to inadequate health care utilization and poor child health outcomes, strategies to promote stable insurance coverage merit serious consideration.
Keywords: chronic conditions, health insurance, medically under-served, health insurance coverage gaps, ethnic disparity
ABBREVIATIONS: TANF, Temporary Assistance to Needy Families; MEPS, Medical Expenditure Panel Survey; HC, Household Component; MPC, Medical Provider Component; IC, Insurance Component; NHIS, National Health Interview Survey
Creating a stable insurance coverage system for American children has been one of the most persistent and intractable challenges in health policy. Previous studies have documented that uninsured children are less likely to use medical services, less likely to use preventive services, and less likely to have a usual source of care.1–6 Cross-sectional studies of uninsured children likely capture some children who experience short-term gaps in coverage as well as those who are ineligible for any coverage within the current system. Unlike ineligible children, it is likely that children with short-term gaps in coverage are eligible for insurance but not enrolled, and there may be opportunities to simplify the current system of enrollment and renewal to prevent these lapses in coverage. Because gaps in coverage can disrupt patient–provider relationships and affect appropriate utilization for children during critical periods of growth and development,7,8 maintaining stable coverage is an important priority. Many childhood and adolescent problems, such as developmental delays, risk-taking behaviors, and nutritional concerns, require regular supervision for early identification and optimal treatment.9–11 For children with chronic conditions, such as asthma or diabetes, continuous coverage is critical to ensure compliance with care regimens.12,13
Despite recent efforts to expand and simplify insurance enrollment procedures, ~8.2 million children, or 12% of all children, were without health insurance coverage at some point in 2003.14 For children in low-income families, the separation of eligibility and enrollment in Medicaid from public cash assistance (known as Temporary Assistance to Needy Families [TANF]) in 1996 was followed by declines in Medicaid enrollment likely as a result of confusion about eligibility and enrollment.15–18 Subsequent outreach and education efforts have led to modest increases in Medicaid enrollment,19,20 yet retention remains a persistent problem. Data from the early 1990s showed that one third to one quarter of children were disenrolled from the program in any given year, and most of these children were uninsured for 4 to 6 months.7,21–23 It is not known whether the separation of TANF eligibility from Medicaid eligibility and the enactment of the State Child Health Insurance Program has affected the number of children who experience gaps in health care coverage in recent years. Although there is clear evidence that children from racial/ethnic minorities and those who live in poverty are more likely to be uninsured than their peers,1,2,24 it is not known whether they are also more likely to experience gaps in insurance coverage. It is also not known whether children from other vulnerable subgroups, such as those with chronic illness, experience considerable gaps in coverage.
In this study, we analyzed data from the 1999–2001 Medical Expenditure Panel Survey (MEPS) linked to the National Health Interview Survey to quantify the number of children with gaps in coverage at the national level and to determine whether vulnerable subgroups of children experience noteworthy lapses in insurance coverage. Given the recent policy changes related to TANF and Medicaid eligibility and previous studies showing that TANF recipients are less likely to be uninsured, we also explored the association between TANF status and the likelihood of experiencing gaps in coverage.
METHODS
The MEPS is a national probability survey of the noninstitutionalized civilian population of the United States, conducted by the Agency for Healthcare Research and Quality. The MEPS collects data on the financing and use of medical care and is designed to provide nationally representative estimates of health care use, expenditures, sources of payment, and insurance coverage. The 3 components of the MEPS include the Household Component (HC), the Medical Provider Component (MPC), and the Insurance Component (IC). The MEPS-HC survey uses the National Health Interview Survey (NHIS) as its sampling frame. The NHIS is a multipurpose, nationally representative survey of the noninstitutionalized civilian population of the United States administered by the National Center for Health Statistics and the Centers for Disease Control and Prevention. The MEPS-HC draws on the previous year’s NHIS sample through an overlapping panel design; therefore, 2 calendar years of information are collected from each household through in-person interviews (eg, the 1999 MEPS collects information from the 1998 and 1997 NHIS). The MEPS-HC collects detailed self-reported data in-person using a computer-assisted personal instrument. These data include demographic characteristics, household income, health and functional status, health insurance coverage, and access to care. The MEPS-MPC supplements and validates information on medical care events reported in the MEPS-HC by contacting medical providers identified by respondents. Weighted sequential hot-deck imputation is used to estimate missing data on the basis of responses from similar respondents. The MEPS includes detailed data on insurance coverage that allow for estimates of monthly insurance status and type of insurance coverage (eg, private, Medicaid, Medicare) for each respondent in a given survey year.
We analyzed data from the 24 149 children (younger than 18 years) who were sampled in the 1999–2001 MEPS linked to the 1997–2000 NHIS. Consistent with previous studies and given the limitations of the MEPS and the NHIS,25–28 chronic conditions included asthma, attention-deficit/hyperactivity disorder, arthritis, autism, cerebral palsy, congenital heart disease, cystic fibrosis, diabetes, mental retardation, muscular dystrophy, and sickle cell disease as determined by asking parents, “Has a doctor or other health professional told you that your child has. . .?” As in other studies,29 children were classified into the following racial/ethnic groups: non-Hispanic white, black, Hispanic, Asian, Alaskan/Pacific Islander, and Native American. Because of the small number of children in the Asian, Alaskan/Pacific Islander, and Native American groups, we had inadequate power to conduct analyses for each of these specific subgroups. On the basis of household income in relation to the federal poverty level, children were classified into the following categories: poor (< 100% of federal poverty level), near-poor (between 100% and 200% of the federal poverty level), middle income (200%–400% of the federal poverty level), and high income (< 400% of the federal poverty level). Within the NHIS, child participation in TANF is ascertained by asking adult respondents whether the child had received TANF or related public cash assistance payments during the year before the interview.30 TANF recipients included any child who was reported to have received TANF or related public cash assistance payments; all others were considered nonrecipients. Other covariates included age, gender, and maternal education. The outcome variable was insurance status classified as continuously insured for the entire year (12 months), uninsured for the entire year, or lapses in coverage. Children who were uninsured for at least 1 month in the survey year were considered to have lapses in insurance coverage. For insured children, each month of coverage was classified as private (employer-based insurance) versus public (Medicaid, State Child Health Insurance Program, Medicare, etc).
To obtain nationally representative estimates, we used MEPS person-level weights, provided by Agency for Healthcare Research and Quality, that reflect population distributions and account for the household probability of selection, ratio adjustment to national population estimates at the household level, and adjustment for nonresponse. Estimates of variability were obtained using a Taylor Series estimation approach. Variance estimation strata and primary sampling unit variables were provided with the MEPS-HC data.
We used χ2 tests to compare distributions of categorical covariates (eg, gender, ethnicity, poverty) between children with continuous insurance coverage and lapsed coverage and those who were uninsured. We used t tests to compare differences in mean age between these groups.
Multivariate ordinal logistic regression models were used to examine the independent association of race, poverty, and presence of chronic conditions with the likelihood of insurance coverage (continuous coverage, uninsured, or lapsed) after taking into account differences in age, gender, maternal educational, TANF status, and year of survey. Statistical tests were 2-tailed and were performed on the nationally weighted representative population using SAS-callable SUDAAN. This study was exempted from review by the Institutional Review Board of The Children’s Hospital of Philadelphia.
RESULTS
The 24 149 children who were sampled in the 1999–2001 MEPS are representative of nearly 218 million American children in total, ~72 million children in each year. In each year, ~78% were insured continuously for all 12 months, 8% were uninsured for the entire year, and 14% had lapses in coverage (Table 1 and Fig 1). Whereas ~5 to 6 million children annually were uninsured in each year, > 9 million children had gaps in coverage in each year. Compared with their healthy peers, the > 5 million children annually with chronic conditions such as asthma, diabetes, and sickle cell disease did not experience any significant improvements in coverage. Among children with these conditions, 13.7% experienced gaps in coverage (vs 14.1% of healthy children; P = .12) and 6.9% were uninsured for the entire year (vs 8.2% of healthy children; P = .12). There were no significant changes in any of these trends between 1999 and 2001.
TABLE 1.
Characteristics of Children, by Insurance Status: 1999–2001
| Insured Entire Year | Uninsured Entire Year | Gaps in Coverage | |
|---|---|---|---|
| % of sampled children | 77.7 | 8.2 | 14.1 |
| Has chronic condition, %* | 79.4 | 6.9 | 13.7 |
| Age, % | |||
| Preschool (0–5 y) | 76.3 | 6.2 | 17.5 |
| School age (6–11 y) | 77.8 | 7.8 | 14.4 |
| Adolescent (> 12 y) | 78.5 | 10.0 | 11.5 |
| Gender, % male | 51.5 | 53.0 | 49.3 |
| Race/ethnicity, % | |||
| Non-Hispanic white | 82.0 | 5.9 | 12.1 |
| Black | 77.3 | 7.8 | 14.9 |
| Hispanic | 60.6 | 18.6 | 20.9 |
| Other | 81.7 | 4.3 | 14.0 |
| Poverty status, % | |||
| Poor | 66.7 | 11.6 | 21.7 |
| Near poor | 64.0 | 13.8 | 22.2 |
| Middle income | 80.2 | 7.0 | 12.8 |
| High income | 91.2 | 3.6 | 5.3 |
| Receives TANF, %† | 77.5 | 3.8 | 18.7 |
| Poor TANF recipient | 80.3 | 2.0 | 17.7 |
| Near-poor TANF recipient | 72.5 | 6.5 | 21.0 |
| Maternal education, % | |||
| < High school | 62.2 | 13.5 | 24.3 |
| High school graduate | 79.4 | 6.7 | 13.9 |
| > High school | 84.9 | 4.5 | 10.6 |
All percentages are weighted estimates to reflect average annual national population totals.
Chronic conditions include asthma, attention-deficit/hyperactivity disorder, arthritis, autism, cerebral palsy, congenital heart disease, cystic fibrosis, diabetes, mental retardation, and sickle cell disease.
TANF is the public cash assistance program formerly known as Aid to Families With Dependent Children.
Fig 1.
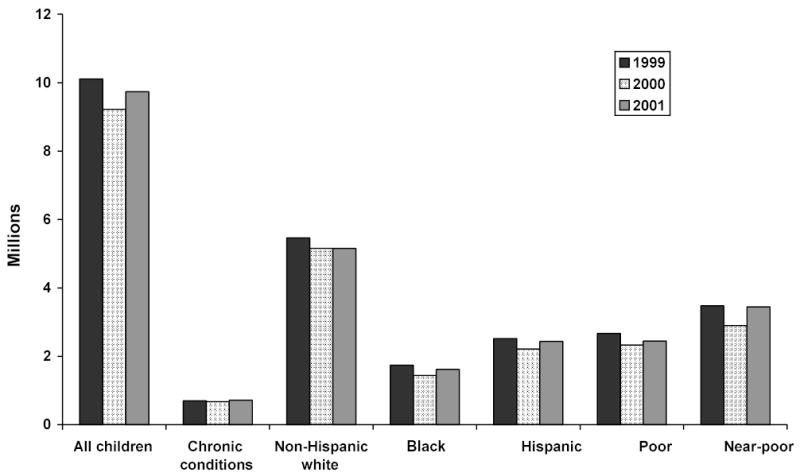
Number of children with gaps in coverage, 1999–2001.
The largest differences in coverage were related to poverty status. Children who were living in poor families were > 4 times as likely as children in high-income families to experience gaps in coverage (21.7% vs 5.3%; P < .01) and > 3 times as likely to be uninsured (11.6% vs 3.6%; P < .01). Children who were living in near-poor families were similarly disadvantaged; they were > 5 times as likely as high-income children to have gaps in coverage (22.2% vs 5.3%; P < .01) and > 3 times as likely to be uninsured (13.8% vs 3.6%; P < .01). Taking children from all income groups as a whole, TANF recipients were less likely than nonrecipients to be uninsured (3.8% vs 8.4%; P < .001) but were more likely to experience gaps in coverage (18.7% vs 13.5%; P < .01). However, because poor and near-poor children composed > 90% of all TANF recipients, there was a significant interaction between TANF status and family income. Among poor children, nonrecipients were almost 7 times more likely than TANF recipients to be uninsured (14.11% vs 2.03%; P < .01) and were 1.3 times more likely to have gaps in coverage (22.5% vs 17.7%; P < .01), whereas the reverse was true among middle- and high-income groups. Similarly, among near-poor children, nonrecipients were more than twice as likely as TANF recipients to be uninsured (14.7% vs 6.5%; P < .01) and were not significantly more or less likely to have gaps in coverage (21.4% vs 21.0; P = .64).
Significant differences in coverage were also related to race. Black children were more likely than non-Hispanic white children to have gaps in coverage (14.9% vs 12.1%; P < .01) and to be uninsured (7.8% vs 5.9%; P < .01). Hispanic children were the most disadvantaged in comparison with non-His-panic white children; they were 1.7 times more likely to have gaps in coverage (20.9% vs 12.1%; P < .01) and > 3 times as likely to be uninsured (18.6% vs 5.9%; P < .01).
Substantial differences in coverage were related to maternal educational attainment. Children whose mothers had not completed high school were more than twice as likely as those whose mothers had some college education to experience gaps in coverage (24.3% vs 10.6%; P < .01) and were 3 times as likely to be uninsured (13.5% vs 4.5%; P < .01). We found no significant differences in coverage by gender. Although adolescents were more likely than younger children to lack coverage completely, pre-school children were the most likely to have gaps in coverage (Table 1).
We next examined the monthly distribution of gaps in coverage and type of insurance coverage among children who had gaps (Fig 2). Within this group, ~40% of children experienced a 1- to 3-month gap in insurance coverage, whereas the majority of children, ~5 million in each year from 1999 to 2001, were uninsured for ~4 months. For children with chronic conditions and those from ethnic/racial minorities, similar results were found, with ~60% of children from each of these groups having gaps of 4 months or longer in each year. However, among children with lapsed coverage, high-income children and TANF recipients tended to have shorter gaps in coverage; ~20% of high-income children and one quarter of TANF recipients were uninsured for only 1 month (data not shown). Over the 3-year period from 1999 to 2001, children with lapsed coverage were increasingly likely to have public insurance. In 1999, most children with lapsed coverage were privately insured (48.6% private vs 35.4% public), whereas by 2001, the greatest proportion was publicly insured (39.2% private vs 43.8% public; P < .001 for trend). This erosion of private coverage was found across all income groups.
Fig 2.
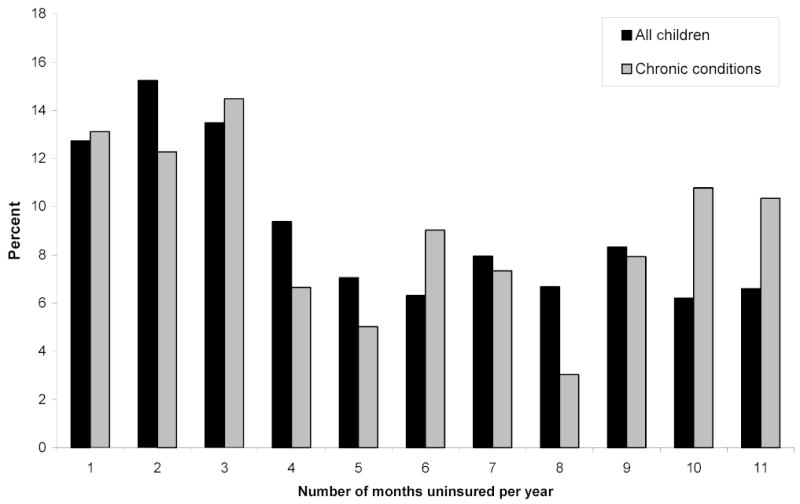
Annual duration of gaps in coverage for children.
The final portion of our analysis used multivariate ordinal logistic regression to identify the independent association of chronic illness, poverty, and race with the likelihood of having lapsed coverage or being uninsured (vs having continuous coverage) after accounting for differences in age, gender, maternal education, TANF status, and year of survey. The attenuated effect sizes in comparison with the findings from Table 1 provide evidence for confounding by race and poverty status. Specifically, the black versus non-Hispanic white difference becomes statistically insignificant, although the Hispanic versus non-Hispanic white difference persists. However, the main findings from our bivariate analysis are unchanged. First, children with chronic conditions are just as likely as other children to have gaps in coverage or to be uninsured. Second, children whose mothers have greater educational attainment are least likely to have lapsed coverage or to be uninsured. Third, although TANF receipt protects children from losing health coverage entirely, TANF recipients are just as likely as nonrecipients to have lapsed coverage. Finally, children from lower income and middle-income families were much more likely to have lapsed coverage than children from higher income families (Table 2).
TABLE 2.
Adjusted Odds Ratios for Insurance Status Among US Children (1999–2001)
| Uninsured Versus Continuous Coverage OR (95% CI) | Gaps Versus Continuous Coverage OR (95% CI) | |
|---|---|---|
| Age | 1.05 (1.04–1.07)* | 0.98 (0.97–0.99)† |
| Gender (male) | 1.05 (0.90–1.22) | 0.93 (0.83–1.04) |
| Has chronic condition‡ | 0.94 (0.73–1.21) | 1.08 (0.90–1.31) |
| Race/ethnicity | ||
| Non-Hispanic white | Reference | Reference |
| Black | 0.82 (0.59–1.14) | 0.83 (0.64–1.07) |
| Hispanic | 2.44 (1.91–3.11)* | 1.44 (1.19–1.73)* |
| Other | 0.72 (0.43–1.20) | 1.18 (0.79–1.78) |
| Poverty | ||
| Poor | 4.21 (2.78–6.37)* | 4.58 (3.40–6.17)* |
| Near poor | 5.19 (3.62–7.43)* | 4.91 (3.76–6.42)* |
| Middle income | 2.30 (1.61–3.29)* | 2.43 (1.86–3.19)* |
| High income | Reference | Reference |
| Receives TANF | 0.24 (0.13–0.45)* | 0.76 (0.53–1.08) |
| Maternal education | ||
| < High school | 1.84 (1.41–2.41)* | 1.58 (1.26–1.97)* |
| High school graduate | 0.95 (0.73–1.23) | 1.31 (1.08–1.58)† |
| > High school | Reference | Reference |
OR indicates odds ratio.
P < .001.
P < .01.
Chronic conditions include asthma, attention-deficit/hyperactivity disorder, arthritis, autism, cerebral palsy, congenital heart disease, cystic fibrosis, diabetes, mental retardation, and sickle cell disease.
DISCUSSION
Our results provide new information about the number of children, especially those from vulnerable subgroups, with lapsed insurance coverage. From 1999 to 2001, we found that, compared with 5 to 6 million children annually who were uninsured for the entire year, ~1.5 times as many children, or > 9 million, had gaps in insurance coverage. Distinguishing between these 2 groups is important because different strategies may be required to address these problems; gaps in coverage may be reduced by simplifying enrollment and renewal procedures, whereas extending coverage to all children requires modifications to current eligibility criteria. Among children with gaps in coverage, we found that > 60% were uninsured for at least 4 months, and this problem affected both publicly and privately insured children. Because gaps in coverage can affect continuity of care for children and adolescents during key periods in which early identification and treatment of common problems is vital to promote long-term well-being,7,8 concerted efforts to address this problem across both sectors are warranted. Our finding that preschool children were most likely to experience gaps compared with other age groups raises additional concerns that critical opportunities to provide well-child care and early intervention services may be missed as a result of coverage gaps. In our analysis of vulnerable subgroups of children, we found that children with chronic conditions are just as likely as other children to have gaps in coverage and be uninsured. Children with these conditions, such as asthma and diabetes, require regular medical care to adjust doses of medication, avoid missing school, and achieve optimal long-term health outcomes.12,26,31,32 In addition to being uninsured, gaps in coverage may be expected to hinder these children from receiving the care necessary to attain these goals.
Not surprising, we found that children with lapsed insurance coverage were most likely to live in families with incomes between 100% and 200% of the federal poverty level, and their mothers were unlikely to have a college education. The association between maternal education and stable health care coverage for children is logical given that women with greater educational attainment are more likely to obtain stable employment with higher incomes and better benefits for themselves and their families. In addition, as others have documented, near-poor working families are at greatest risk for losing health insurance because their incomes are generally too high to qualify for Medicaid and their employers may not offer affordable coverage.33–37 The increasing number of employers who restrict health insurance benefits to a single employee, rather than employees and their families, may contribute to growing instability of health insurance coverage for children who live in low- and middle-income working families.38 Although our finding that TANF recipients were less likely to be uninsured is consistent with previous analyses,18,25 our results documenting that TANF recipients are just as likely to experience gaps in coverage as nonrecipients suggest that there may be administrative procedures that are barriers to retaining coverage and that cut across income groups. This is consistent with our finding that > 40% of publicly and privately insured children ex- perience gaps in coverage. Moreover, the continued rise in private-sector premiums and the growing proportion of part-time workers in the labor force are likely to contribute to the erosion of private coverage across income groups.39–41
To date, although efforts within the private sector have not been well documented, various strategies have been proposed to improve retention procedures for Medicaid-eligible families. Although some children disenroll as a result of increases in family income, others disenroll as a result of administrative “churning” (refers to the suspension of coverage while an application is processed) or failure to complete reenrollment procedures.42 As a result of federal regulations (42 CFR 435.916), states are required to redetermine Medicaid eligibility at least every 12 months with respect to circumstances that may change, such as income.23 However, states may opt to eliminate the face-to-face interview requirement, accept mail-in applications, reduce the complexity of the application form, or simplify verification requirements.23,33 In practice, although making these options available to families certainly can ease the renewal process, other factors (eg, ease of obtaining a mail-in application, ease of completing the application without assistance, how widely it is known that families need not go to a welfare office to apply for Medicaid coverage) can also facilitate or hinder families from renewing. Within the private sector, coverage gaps among children are most likely related to parents’ changing or losing jobs or time periods when they cannot afford to pay the family premium. The current system of COBRA benefits provides coverage for these periods; however, employees must bear the cost of the monthly premium and bear the burden of processing claims retrospectively.43 Additional development of public–private partnerships to subsidize premium costs during these tight budgetary transition periods and eliminating employee claims processing are 2 potential strategies to address this problem.
There are some limitations to this study. First, MEPS does not provide monthly data on assets or employment status that may affect the ability of families to maintain insurance coverage. We were unable to account for these changes in our analysis. Second, MEPS does not include items to determine whether families have applied for insurance after coverage has been terminated and been denied or whether the application is still pending as part of administrative churning. However, administrative churning usually does not create lapses beyond 2 months.42 Therefore, our finding that > 60% of children with lapsed coverage are uninsured for > 4 months suggests that churning cannot fully explain these coverage gaps. Third, because of limitations in the information collected in the NHIS linked with MEPS, we were unable to include some childhood chronic conditions, such as seizure disorders, in our analysis. This likely led to an underestimation of the prevalence of childhood chronic conditions. Although the National Survey of Children with Special Health Care Needs has begun to provide more comprehensive estimates, this survey was launched in 2000 and data are not yet suitable for trends analysis.44,45 In addition, MEPS data are cross-sectional and future longitudinal studies are necessary to provide evidence of causality. Nevertheless, our findings are the first to present recent data describing the magnitude of this problem for children and, specifically, vulnerable subgroups of children at the national level. Finally, our study does not examine health care utilization or health outcomes among children with lapsed coverage. Previous studies suggested that children with lapsed coverage are likely to have inadequate health care utilization and potentially poor health outcomes,2,3,7 but additional research in this area is required.
In summary, 13% to 14% of American children, even those with chronic conditions that require regular health supervision, experience lapses in coverage annually, and 60% are uninsured for ~4 months. Although children who live in low-income working poor families seem to have the greatest problems with lapsed coverage, the problem affects both publicly and privately insured children. In addition to continued efforts to expand coverage to low-income working poor families, strategies to promote stable insurance coverage for all children, especially those with chronic conditions, merit serious consideration. Key strategies in the public sector may be most effective by focusing on simplifying enrollment and retention procedures, whereas public–private partnerships may be essential to maintaining coverage during budgetary shortfalls experienced by working parents and families.
Acknowledgments
Dr Pati’s research is supported by grants from the National Institute of Child Health and Human Development (K23HD047655-01) and the Anne E. Dyson Foundation.
The authors gratefully acknowledge the comments of Drs Donald F. Schwarz, Wendy Chavkin, and Paul Wise in reviewing this manuscript. This project originated in part from Finding Common Ground, a collaborative research effort between the Mailman School of Public Health at Columbia University and Boston Medical Center.
Footnotes
No conflict of interest declared.
References
- 1.Newacheck PW, Hughes DC, Stoddard JJ. Children’s access to primary care: differences by race, income, and insurance status. Pediatrics. 1996;97:26–32. [PubMed] [Google Scholar]
- 2.Newacheck PW, Stoddard JJ, Hughes DC, Pearl M. Health insurance and access to primary care for children. N Engl J Med. 1998;338:513–519. doi: 10.1056/NEJM199802193380806. [DOI] [PubMed] [Google Scholar]
- 3.Newacheck PW, Pearl M, Hughes DC, Halfon N. The role of Medicaid in ensuring children’s access to care. JAMA. 1998;280:1789–1793. doi: 10.1001/jama.280.20.1789. [DOI] [PubMed] [Google Scholar]
- 4.Ortega AN, Stewart DC, Dowshen SA, Katz SH. Perceived access to pediatric primary care by insurance status and race. J Community Health. 2000;25:481–493. doi: 10.1023/a:1005196714900. [DOI] [PubMed] [Google Scholar]
- 5.Weinick RM, Weigers ME, Cohen JW. Children’s health insurance, access to care, and health status: new findings. Health Aff. 1998;17:127–136. doi: 10.1377/hlthaff.17.2.127. [DOI] [PubMed] [Google Scholar]
- 6.Kasper JD, Giovannini TA, Hoffman C. Gaining and losing health insurance: strengthening the evidence for effects on access to care and health outcomes. Med Care Res Rev. 2000;57:298–318. doi: 10.1177/107755870005700302. discussion 319–325. [DOI] [PubMed] [Google Scholar]
- 7.Kogan MD, Alexander GR, Teitelbaum MA, Jack BW, Kotelchuck M, Pappas G. The effect of gaps in health insurance on continuity of a regular source of care among preschool-aged children in the United States. JAMA. 1995;274:1429–1435. [PubMed] [Google Scholar]
- 8.Zlotnick C, Soman LA. The impact of insurance lapse among low-income children. J Urban Health. 2004;81:568–583. doi: 10.1093/jurban/jth141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Barlow SE, Dietz WH, Klish WJ, Trowbridge FL. Medical evaluation of overweight children and adolescents: reports from pediatricians, pediatric nurse practitioners, and registered dietitians. Pediatrics. 2002;110:22–228. [PubMed] [Google Scholar]
- 10.Recommendations for preventative pediatric health care. American Academy of Pediatrics Committee on Practice and Ambulatory Medicine. . Pediatrics. 2000;105:645–646. [Google Scholar]
- 11.Hakim RB, Bye BV. Effectiveness of compliance with pediatric preventive care guidelines among Medicaid beneficiaries. Pediatrics. 2001;108:90–97. doi: 10.1542/peds.108.1.90. [DOI] [PubMed] [Google Scholar]
- 12.Institute of Medicine. Crossing the Quality Chasm: A New Health System for the 21st Century Washington, DC: National Academies Press; 2001 [PubMed]
- 13.Diette GB, Skinner EA, Markson LE, et al. Consistency of care with national guidelines for children with asthma in managed care. J Pediatr. 2001;138:59–64. doi: 10.1067/mpd.2001.109600. [DOI] [PubMed] [Google Scholar]
- 14.DeNavas-Walt C, Proctor BD, Mills RJ. Income, Poverty, and Health Insurance Coverage in the United States: 2003 (US Census Bureau, Current Population Reports, P60-226). Washington, DC: US Government Printing Office; 2004
- 15.Medicaid Enrollment: Amid Declines, State Efforts to Ensure Coverage After Welfare Reform Vary. Washington, DC: US General Accounting Office; 1999
- 16.Losing Health Insurance: The Unintended Consequences of Welfare Reform. Washington, DC: Families USA Foundation; 1999
- 17.Chavkin W, Romero D, Wise PH. State welfare reform policies and declines in health insurance. Am J Public Health. 2000;90:900–908. doi: 10.2105/ajph.90.6.900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Pati S, Romero D, Chavkin W. Changes in use of health insurance and food assistance programs in medically underserved communities in the era of welfare reform: an urban study. Am J Public Health. 2002;92:1441–1445. doi: 10.2105/ajph.92.9.1441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wheatley B. State approaches to expanding family coverage. State Coverage Initiatives Issue Brief. 2000;1:1–6. [PubMed] [Google Scholar]
- 20.Health Insurance Historical Tables. US Census Bureau. Available at: www.census.gov/hhes/hlthins/historic Accessed September 18, 2003
- 21.Irvin C, Peikes D, Trenholm C, Khan N. Discontinuous Coverage in Medicaid and the Implications of 12-Month Continuous Coverage for Children. Cambridge, MA: Mathematica Policy Research, Inc; 2001 (MPR Reference No. 8657–402)
- 22.Carrasquillo O, Himmelstein DU, Woolhandler S, Bor DH. Can Medicaid managed care provide continuity of care to new Medicaid enrollees? An analysis of tenure on Medicaid. Am J Public Health. 1998;88:464–466. doi: 10.2105/ajph.88.3.464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Enrolling and Retaining Low-Income Families and Children in Health Care Coverage. Washington, DC: Center for Medicare and Medicaid Services, US Department of Health and Human Services; 2001 (CMS Pub. No. 11000)
- 24.Aday LA, Lee ES, Spears B, Chung CW, Youssef A, Bloom B. Health insurance and utilization of medical care for children with special health care needs. Med Care. 1993;31:1013–1026. doi: 10.1097/00005650-199311000-00004. [DOI] [PubMed] [Google Scholar]
- 25.Wise PH, Wampler NS, Chavkin W, Romero D. Chronic illness among poor children enrolled in the Temporary Assistance for Needy Families program. Am J Public Health. 2002;92:1458–1461. doi: 10.2105/ajph.92.9.1458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.McPherson M, Honberg L. Identification of children with special health care needs: a cornerstone to achieving healthy people 2010. Ambul Pediatr. 2002;2:22–23. doi: 10.1367/1539-4409(2002)002<0022:iocwsh>2.0.co;2. [DOI] [PubMed] [Google Scholar]
- 27.Perrin EC, Newacheck P, Pless IB, et al. Issues involved in the definition and classification of chronic health conditions. Pediatrics. 1993;91:787–793. [PubMed] [Google Scholar]
- 28.Szilagyi PG, Shenkman E, Brach C, et al. Children with special health care needs enrolled in the State Children’s Health Insurance Program (SCHIP): patient characteristics and health care needs. Pediatrics. 2003;112(6 suppl) Available at: www.pediatrics.org/cgi/content/full/112/6/SE1/e508. [PubMed] [Google Scholar]
- 29.Newacheck PW, Park MJ, Brindis CD, Biehl M, Irwin CE., Jr Trends in private and public health insurance for adolescents. JAMA. 2004;291:1231–1237. doi: 10.1001/jama.291.10.1231. [DOI] [PubMed] [Google Scholar]
- 30.NHIS Survey Description, 2001 National Health Interview Survey Public Use Data Release. Hyattsville, MD: Division of Health Interview Statistics, National Center for Health Statistics; 2003
- 31.Epstein SG, Walker DK. Applying the lessons learned in identifying children with special health care needs: next steps to assure quality care. Ambul Pediatr. 2002;2:26–28. doi: 10.1367/1539-4409(2002)002<0026:atllii>2.0.co;2. [DOI] [PubMed] [Google Scholar]
- 32.Szilagyi PG. Care of children with special health care needs. Future Child. 2003;13:137–151. [PubMed] [Google Scholar]
- 33.Maloy KA, Kenney KA, Darnell J, Cyprien S. Can Medicaid Work for low-income Working Families? Washington, DC: Kaiser Commission on Medicaid and the Uninsured; 2002
- 34.Kenney GM, Haley J. Why Aren’t More Uninsured Children Enrolled in Medicaid or SCHIP? Washington, DC: Urban Institute; 2001 (Assessing the New Federalism Policy Brief No. B-35)
- 35.Byck GR. A comparison of the socioeconomic and health status characteristics of uninsured, State Children’s Health Insurance program-eligible children in the United States with those of other groups of insured children: implications for policy. Pediatrics. 2000;106:14–21. doi: 10.1542/peds.106.1.14. [DOI] [PubMed] [Google Scholar]
- 36.Guendelman S, Wyn R, Tsai YW. Children of working low-income families in California: does parental work benefit children’s insurance status, access, and utilization of primary health care? Health Serv Res. 2000;35:417–441. [PMC free article] [PubMed] [Google Scholar]
- 37.Cunningham PJ, Park MH. Recent trends in children’s health insurance coverage: no gains for low-income children. Issue Brief Cent Study Health Syst Change. 2000;(29):1–6. [PubMed] [Google Scholar]
- 38.Health Care: Are You Better Off Today Than You Were Four Years Ago? Washington, DC: Families USA; 2004 (Publication No. C4-04-100)
- 39.Krantz R, Di Natale M, Krolik TJ. The U.S. labor market in 2003: signs of improvement by year’s end. Month Labor Rev. 2004 March;:3–29. [Google Scholar]
- 40.Heffler S, Smith S, Keehan S, Clemens MK, Zezza M, Truffer C. Health spending projections through 2013. Health Aff. 2004;(Suppl Web Exclusives):W4-79–93. doi: 10.1377/hlthaff.w4.79. [DOI] [PubMed] [Google Scholar]
- 41.Levit K, Smith C, Cowan C, Sensenig A, Catlin A. Health Accounts Team. Health spending rebound continues in 2002. Health Aff. 2004;23:147–159. doi: 10.1377/hlthaff.23.1.147. [DOI] [PubMed] [Google Scholar]
- 42.Ellwood MR, Lewis K. On and Off Medicaid: Enrollment Patterns for California and Florida in 1995. Washington, DC: The Urban Institute; 1999 (Occasional Paper Number 27)
- 43.Frequently asked questions about COBRA continuation health coverage. US Department of Labor. Available at: www.dol.gov/ebsa/faqs/faq_consumer_cobra.html Accessed January 28, 2005
- 44.Blumberg SJ, Olson L, Frankel M, et al. Design and operation of the National Survey of Children with Special Health Care Needs, 2001. Vital Health Stat 1. 2003;(41):1–136. [PubMed] [Google Scholar]
- 45.Olson LM, Tang SS, Newachak PW. Children in the United States with discontinuous health insurance coverage. N Engl J Med. 2005;353:382–391. doi: 10.1056/NEJMsa043878. [DOI] [PubMed] [Google Scholar]


