Abstract
Background
Abdominal aortic aneurysms (AAAs) are frequently familial. The aim of this study was to compare the prevalence of AAA among the siblings of AAA patients to that in the spouses’ siblings.
Methods
The siblings of 375 AAA patients and the siblings of the spouses of the AAA patients were included in this study and offered ultrasonography screening for AAA. Participants were asked to complete a questionnaire to collect demographic and general health information. Statistical analysis was carried out using Fisher’s exact test. Odds ratios and 95% confidence intervals were also calculated.
Results
Abdominal ultrasonography examination was carried out for 309 individuals. The results indicated that 11 of 98 (11.2%) brothers of AAA patients, 4 of 147 (2.7%) sisters, and none of the 64 siblings of the spouses of the AAA patients were found to have an AAA. Combining the information from the ultrasonography screening and medical records on already known cases of AAA in these families, altogether 29.0% (44/152) of the brothers of AAA patients, 11.1% (20/181) of the sisters of AAA patients, and 2.3% (2/88) of the siblings of the spouses had an AAA.
Conclusion
There was a significant difference between the siblings of the AAA patients and those of the spouses both in the frequency of AAA detected by ultrasonography screening and in the overall prevalence of AAA. The overall prevalence of AAA in the siblings of AAA patients was about 8 times that observed among the siblings of their spouses (19.2% vs. 2.3%). These findings confirmed previous reports on high prevalence of AAA among siblings of AAA patients and emphasized the importance of an ultrasonography screening program for siblings of AAA patients.
An estimated 1–2% of the population harbor abdominal aortic aneurysms (AAAs).1 The mortality of a ruptured AAA is as high as 80–90% and rupture of an AAA accounts for a significant fraction of deaths, especially among older men.2 In contrast, the mortality for elective open surgery, prior to rupture, is only 2–6%.3, 4 Early diagnosis of AAA prior to rupture is, therefore, important for patients’ survival.
AAAs are frequently familial.5–7 Approximately 15% of patients with AAA and without any recognizable connective tissue disorder, such as the Ehlers-Danlos syndrome or the Marfan syndrome, have a positive family history for AAA.see 7
We carried out an ultrasonography screening study on the siblings of AAA patients, and used the spouses’ siblings as controls. The aims of the study were 1) to determine the prevalence of AAA among the siblings of known AAA patients in a well characterized population (Nova Scotia); and 2) to compare the observed life-time prevalence of AAA among siblings of AAA patients to that in the spouses' siblings with the assumption that they shared similar environmental exposures and cultural habits and were, therefore, well-matched controls for the study.
PATIENTS AND METHODS
A definition of AAA by Johnston et al8 (a diameter of infrarenal aorta ≥3 cm) was used. This definition has been used by other investigators.9, 10 Of the 375 AAA patients (male; n=292, 77.7%), 254 individuals had been operated on at the Dalhousie University Hospitals in Halifax, Canada, between 1992 and 2003 either as elective repair (n=187) or emergency operations (n=67). The remaining 125 AAA patients were not operated on due to their general health status or because the size of the aneurysm was less than 5 cm. We will use the term proband for each of these 375 AAA patients, since each of them was the first affected person in their families who came to our attention. We started to recruit AAA patients for the study in 1999, and enrolled retrospectively 315 AAA patients who were operated on or diagnosed with AAA between 1992 and 1999 and agreed to participate in the study. The patient information from this time period was in an AAA database. Patients to be contacted by phone were selected randomly from this database. In addition, we had an on-going prospective recruitment during 1999 to 2003 and altogether, 60 AAA patients from this time period agreed to participate in the study. The average age of the 375 AAA patients was 72.1±7.2 years. Ninety percent of the AAA patients were Caucasian (n=335). Pedigrees of the 375 AAA probands were constructed and consent for contacting the family members was obtained. Both the AAA probands and the spouses were interviewed whenever possible to gather information for constructing the pedigrees. The study was restricted to individuals who were 50 years or older. The first-degree relatives and spouses of the AAA patients as well as the first-degree relatives of the spouses were contacted by personnel specifically trained for this study, and invited to participate in the study. Written informed consent was obtained from the participants who agreed to ultrasonography examination of the abdominal aorta. If an ultrasonography examination or an equivalent examination such as computerized tomography (CT) scan had been completed within the past six months, a copy of the report was requested and no additional ultrasonography examination was done.
Participants were asked to complete a questionnaire about their general health information (smoking history, past medical history for hypertension, hypercholesterolemia, angina, peripheral vascular disease and diabetes) as well as gender, race and age.
Observed life-time prevalence of AAA was calculated by combining the number of already known AAA cases with the number of asymptomatic AAA cases identified in this study using ultrasonography screening.
The study was approved by the Capital Health Research Ethics Board, Nova Scotia, Canada, and the Institutional Review Board of Wayne State University.
Statistical analysis was carried out using Fisher’s exact test. Odds ratios (ORs) and 95% confidence intervals (CIs) were calculated for prevalence of AAA among family members and risk factors such as smoking, hypertension, and hypercholesterolemia.
Only the siblings of the AAA probands and the siblings of the spouses were included in the statistical analyses since the numbers of first-degree relatives other than siblings from the AAA probands’ families and the spouses’ families were small.
RESULTS
Initial interview of the 375 AAA probands indicated that 232 of the probands had a spouse and that there were a total of 2,175 individuals who belonged to one of these two categories: 1) siblings of the AAA probands (n=1,703); or 2) siblings of the spouses (n=472) (Figure 1). Many of them (850; 39.4%), however, were deceased and, therefore, not available for the ultrasonography study. Of the 1,325 living individuals, 904 (68.2%) individuals, 655 siblings of the AAA probands and 249 siblings of the spouses were excluded from the study for the following reasons: 1) resided outside Nova Scotia (n=377; 28.5%), 2) refused to participate in the study (n=142; 10.7%), 3) poor health (n=122; 9.2%), 4) no response to invitations (n=115; 8.7%), 5) no contact information (n=80; 6.0%), 6) under 50 years old (n=46; 3.5%), or 7) other (n=22; 1.7%). As shown in Figure 1, the two sibling groups had similar dropout rates for each of these categories. Altogether 421 individuals (421/1,325, 31.8%) from 187 AAA probands participated in the study (Figure 1): 333 siblings of the AAA probands (333/988, 33.7%), and 88 siblings of the spouses (88/337, 26.1%).
Figure 1.
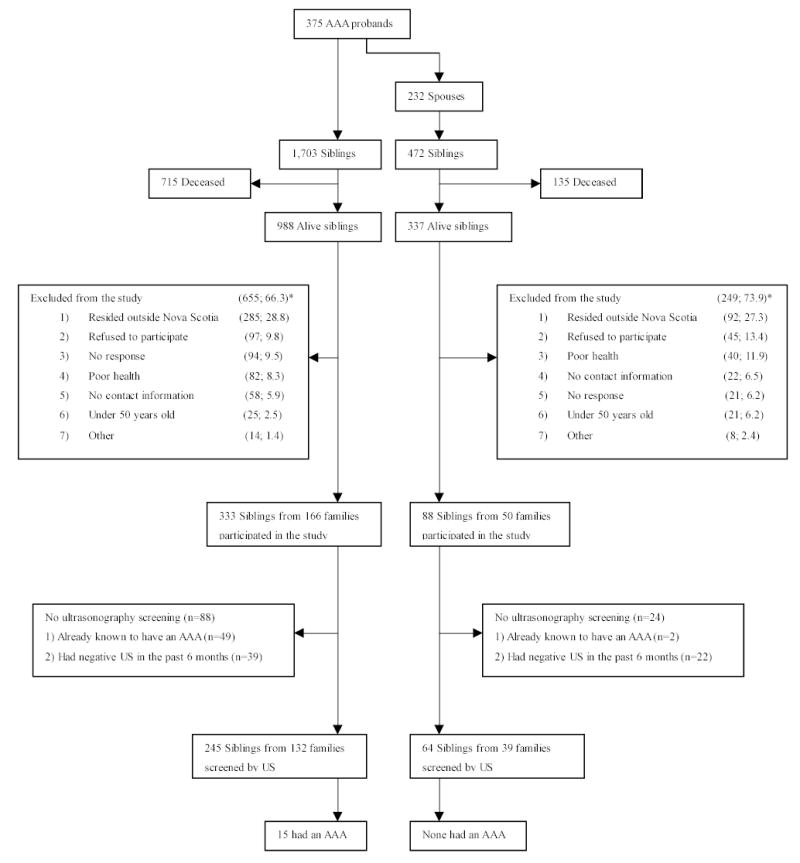
Outline of the Nova Scotia AAA study. The objective of the study was to determine the prevalence of AAA among the first-degree relatives of known AAA patients (referred here as “AAA probands”) in a well-characterized population in Nova Scotia, Canada. Secondly, we examined two comparison groups, the spouses of the AAA probands, and the first-degree relatives of the spouses with the assumption that they shared similar environmental exposures and cultural habits. In the present study we report the findings on the comparison between the two siblings groups, the siblings of the AAA probands and the siblings of the spouses. The spouse group is smaller than the proband group, because 143 AAA probands had no spouses. US, ultrasonography; AAA, abdominal aortic aneurysm.
*(number of individuals; %)
Although 177 of the 232 spouses (18 of spouses were deceased and 32 did not participate for other reasons) participated in the study and 151 of them had an abdominal ultrasonography examination, we excluded them from the statistical arm of the study and present the comparison for the sibling groups only, since most of spouses of the AAA probands were female (81.4%, 144/177).
When family information was gathered, we found out that 49 siblings of the AAA probands and 2 siblings of the spouses were already known to have an AAA (Figure 1). In addition, 39 siblings of the AAA probands and 22 siblings of the spouses had had an abdominal ultrasonography examination or CT scan in the past six months and were found to have an aorta of normal diameter, and were, therefore, not re-screened. These findings indicated that 26.5% [(49+39)/333] of the siblings of the AAA probands and 27.3% [(2+22)/88] of the siblings of the spouses had already had abdominal ultrasonography examination prior to the current study.
From the participants, 245 siblings of 132 AAA probands (73.6%, 245/333) and 64 siblings of 39 spouses (72.7%, 64/88) had an abdominal ultrasonography examination (Figure I). Table I shows the results of the ultrasonography screening for AAA in the two sibling groups. Eleven of the 98 brothers (11.2%) and 4 of the 147 sisters (2.7%) of the AAA probands screened were found to have an AAA. The overall prevalence of AAA in siblings of the 132 AAA probands based on ultrasonography screening was 6.1% (15/245). No AAA was detected in the siblings of the 39 spouses (0/64, 0%). There was a significant difference in the prevalence of AAA detected by ultrasonography screening between the siblings of the AAA probands and the siblings of the spouses (P=.043). When the siblings of the AAA probands were stratified by age over or below 65 years old, the prevalence of AAA among the siblings of the AAA probands over 65 years old was 8.5% (12/141), 16.7% (9/54) in males, and 3.4% (3/87) in females (Table II, online only). On the other hand, the prevalence of AAA among the siblings of the AAA probands below 65 years old was 1.8% (1/57), 0% (0/21) in males, and 2.8% (1/36) in females. There was, however, no significant difference in the prevalence of AAA between the two age groups (P=.054 in males, P=1 in females, and P=.11 in all siblings), probably due to the small sample size.
Table I.
Results of ultrasonography screening for AAA in the study
|
Siblings of AAA probands |
Siblings of spouses |
||||||
|---|---|---|---|---|---|---|---|
| n* | AAA (%) | n* | AAA (%) | P | OR† | CI† | |
| Male | 98 | 11 (11.2) | 26 | 0 (0) | .12 | 6.9 | 0.4–120.6 |
| Female | 147 | 4 (2.7) | 38 | 0 (0) | .58 | 2.4 | 0.1–45.4 |
| Total | 245 | 15 (6.1) | 64 | 0 (0) | .043 | 8.7 | 0.5–146.9 |
AAA , abdominal aortic aneurysm; n, number of individuals examined by abdominal ultrasonography; OR , odds ratio; CI , 95% confidence interval.
245 siblings of the AAA probands were from 132 AAA probands' families and 64 siblings of the spouses were from 39 spouses' families.
Yates' continuity correction was used.
Table II, online only.
Results of ultrasonography screening for AAA stratified by age
|
Siblings of AAA probands |
|||||||
|---|---|---|---|---|---|---|---|
|
below 65 years old |
over 65 years old |
||||||
| n | AAA (%) | n | AAA (%) | P | OR† | CI† | |
| Male | 21 | 0 (0) | 54 | 9 (16.7) | .054 | 8.9 | 0.5–159.6 |
| Female | 36 | 1 (2.8) | 87 | 3 (3.4) | 1 | 1.3 | 0.1–12.4 |
| Total | 57 | 1 (1.8) | 141 | 12 (8.5) | .11 | 5.2 | 0.7–41.0 |
For definitions, see Table I.
Since no AAA was detected by ultrasonography screening among the siblings of the spouses, only the results of the siblings of the AAA probands are shown.
Yates' continuity correction was used.
Detailed demographic and clinical data were collected using a questionnaire from 177 siblings of the AAA probands and 48 siblings of the spouses (Table III). Age, number of males and ever smokers, as well as the presence of hypertension, hypercholesterolemia, heart attack, peripheral vascular disease and diabetes among the siblings of AAA probands were similar to those among the siblings of the spouses. Relative risks of AAA among smokers in the siblings of the AAA probands were: OR=4.7 in males, OR=4.3 in females, and OR=7.3 in all (Table IV, online only).
Table III.
Comparison of the risk factor profiles between siblings of AAA probands and those of the spouses
|
Siblings of AAA patients (n=177)* |
Siblings of spouses (n=48)* |
||||
|---|---|---|---|---|---|
| n (%) | n (%) | P | OR | CI | |
| Male | 80 (45.2) | 22 (45.8) | 1 | 1.0 | 0.5–1.8 |
| Age (±1 SD) (y) | 69.4±8.4 | 68.6±7.6 | .55 | ||
| Ethnicity (Caucasian) | 150 (84.7) | 46 (95.8) | .051 | 0.2 | 0.1–1.1 |
| Hypertension | 73 (41.2) | 20 (41.7) | 1 | 1.0 | 0.5–1.9 |
| Hypercholesterolemia | 85 (48.0) | 20 (41.7) | .51 | 1.3 | 0.7–2.5 |
| Heart attack | 22 (12.4) | 4 (8.3) | .61 | 1.6 | 0.5–4.8 |
| Peripheral vascular disease | 16 (9.0) | 4 (8.3) | 1 | 1.1 | 0.3–3.4 |
| Diabetes | 26 (14.7) | 4 (8.3) | .34 | 1.9 | 0.6–5.7 |
| †Ever smoker | 123 (69.7) | 31 (64.6) | .60 | 1.2 | 0.6–2.4 |
For definitions, see Table I.
Risk factor information was available from 177 (53.1%) of the 333 siblings of the AAA probands and 48 (53.3%) of the 88 siblings of the spouses who participated in the study.
Smoking was defined as ever smoker and included current smoker and past smoker.
Table IV, online only.
Relative risk of AAA among smokers in the siblings of the AAA probands
Table V shows the observed life-time prevalence of AAA in the two sibling groups when taking into account all the previously known cases of AAA and the new AAA cases identified in the ultrasonography screening. Thirty percent (44/152) of the brothers and 11.1% (20/181) of the sisters of the AAA patients had an AAA. The observed life-time prevalence of AAA in the siblings of the 166 AAA probands was 19.2% (64/333). Five percent (2/42) of the brothers of the spouses had an AAA but none of the sisters (0/46). The observed life-time prevalence of AAA in the siblings of the 50 spouses was 2.3% (2/88). There was a significant difference in the observed life-time prevalence of AAA between the siblings of the 166 AAA probands and the siblings of the 50 spouses (male, P=.001; female, P=.01; all siblings, P=<.0001).
Table V.
Comparison of observed life-time prevalences of AAA among siblings of AAA probands to spouses' siblings
|
Siblings of AAA patients |
Siblings of spouses |
||||||
|---|---|---|---|---|---|---|---|
| n* | AAA† (%) | n* | AAA† (%) | P | OR‡ | CI‡ | |
| Male | 152 | 44 (29.0) | 42 | 2 (4.8) | .001 | 8.1 | 1.9–35.2 |
| Female | 181 | 20 (11.1) | 46 | 0 (0) | .01 | 11.7 | 0.7–197.4 |
| Total | 333 | 64 (19.2) | 88 | 2 (2.3) | <.0001 | 10.2 | 2.5–42.7 |
For definitions, see Table I.
The 333 siblings of the AAA probands were from 166 AAA probands' families and 88 siblings of the spouses were from 50 spouses' families.
All known AAA cases in the study groups were included by combining the number of already known AAA cases with the number of asymptomatic AAA cases identified in this study using ultrasonography examinations (see Table I).
Yates' continuity correction was used.
DISCUSSION
AAAs are a complex multifactorial disease with genetic and environmental risk factors. Two segregation studies provided formal statistical proof that a genetic model explains the familial aggregation of AAA and suggested the presence of a major gene effect.11, 12 Recently, we reported on a collection of 233 families with at least two individuals affected with AAA.5 We also reported results on an unbiased, comprehensive genome-wide approach, namely DNA linkage study for familial AAA using sex and family history as covariates, and identified linkage to chromosomes 19q13 and 4q31,13 suggesting that these regions of the human genome harbor genetic risk factors for AAA.
Previously reported risk factors for AAA include aging, male gender, hypertension, smoking, family history of AAA, and peripheral arterial disease.14–16 Using the siblings of the spouses as a control group in the current study, we made the assumption that the two groups shared similar environmental exposures and had similar cultural habits, since all participants lived in Nova Scotia, Canada. Also, these two groups were similar in terms of age, sex, and the presence of previously identified risk factors for AAA (Table III).
In this study, the prevalence of AAA in the siblings of the AAA probands detected by ultrasonography screening was 6.1%, 11.2% in the brothers and 2.7% in the sisters (Table I). The high prevalence values of AAA among the siblings are in agreement with previous ultrasonography screening studies (Table VI).9, 17–30 Combining all the published results, 114/666 brothers (17.2%) and 22/523 sisters (4.2%) of AAA patients were detected to harbor an AAA. When we compared the siblings who were below 65 years old to those who were over 65 years old in the families of the AAA probands, there was no significant difference in the prevalence of AAA detected by ultrasonography screening (Table II, online only). This result might, however, be due to a small number of participants.
Table VI.
Ultrasonography screening studies of AAA among first-degree relatives
| Authors | Country | Brothers* (%) | Sisters* (%) | Other†(%) |
|---|---|---|---|---|
| Bengtsson et al. 198917 | Sweden | 10/35 (28.6) | 3/52 (5.8) | |
| Collin & Walton 198918 | UK | 4/16 (25.0) | 0/15 (0) | |
| Webster et al. 199119 | USA | 5/24 (20.8) | 2/30 (6.7) | 7/103 (6.8) |
| Adamson et al. 199220 | UK | 5/25 (20.0) | 3/28 (10.7) | |
| Bengtsson et al. 199221 | Sweden | 9/62 (14.5) | ||
| van der Lugt et al. 199222 | The Netherlands | 16/56 (28.6) | 3/52 (5.8) | |
| Adams et al. 199323 | UK | 4/23 (17.4) | 1/28 (3.6) | 6/23 (26.1) |
| Moher et al. 199424 | Canada | 9/48 (18.8) | ||
| Fitzgerald et al. 199525 | Ireland | 13/60 (21.7) | 2/65 (3.1) | |
| Larcos et al. 199526 | Australia | 0/52 (0) | ||
| Baird et al. 19959 | Canada | 7/26 (26.9) | 3/28 (10.7) | |
| Jaakkola et al. 199627 | Finland | 4/45 (8.9) | 1/78 (1.3) | |
| van der Graaf et al. 199828 | The Netherlands | 26/210 (12.4) | ||
| Salo et al. 199929 | Finland | 11/238 (4.6) | ||
| Rossaak et al. 200130 | New Zealand | 4/49 (8.2) | ||
| Current study‡ | Canada | 11/98 (11.2) | 4/147 (2.7) | 0/31 (0) |
| Total | 114/666 (17.2) | 22/523 (4.2) | 37/558 (6.6) |
Number of individuals identified with AAA/number of individuals examined by ultrasonography. The numbers listed in this table include only AAAs detected by ultrasonography screening.
Other refers to relatives other than sisters and brothers of the AAA patient, or the categories of relatives were not specified.
When combining the ultrasonography results to information about already known cases of AAA in each family, the observed life-time prevalence of AAA in the siblings of the AAA probands was 19.2%, 29.0% in the brothers and 11.1% in the sisters, and 8 times that observed in the siblings of the spouses (2.3%), 6 times that in the males (29.0% vs. 4.8%) and 11.1% vs. 0% in the females (Table IV). All comparisons showed significant difference (male, P=.001; female, P=.01; all siblings, P=<.0001). The high observed prevalence of AAA in the siblings of the AAA patients in the current study (19.2%) is in agreement with previous studies based on interviews (6.1–35.7%).see7 The prevalence of AAA in the siblings of the spouses is similar to the prevalence found in control groups or in general populations in previous studies.2, see 7
Several prospective randomized ultrasonography screening studies for AAA have been carried out and they have demonstrated cost-effectiveness of population-based ultrasonography screening programs for AAA and a decrease in the number of aneurysm-related deaths.31–38 Several recommendations have been made including a recent consensus statement, in which Kent et al39 recommended ultrasonography screening for AAA for all individuals over 60 years of age and for those over 50 years of age with family history for AAA and the recommendation by the US Preventive Service Task Force to screen for AAA in men aged 65 to 75 years who have ever smoked.40 In our study, the prevalence of AAA in the siblings of the AAA probands detected by ultrasonography screening (6.1%, 15/245) was significantly higher than that in the siblings of the spouses (0%, 0/64; P=.043). Our results support the proposal39 of using family history for AAA as one of the screening criteria for AAA. Larger studies are, however, required to determine, if those individuals with a positive family history should be screened already at younger age.
Male gender is a strong risk factor for AAA.14, 15, 36 In this study, the prevalence of AAA in the brothers of the AAA probands was almost 3 times that in the sisters (brothers 29.0% vs. sisters 11.1%). Similar trend was observed in the group of the siblings of the spouses (brothers 4.8% vs. sisters 0%). Smoking is also a well-known risk factor for AAA14, 15, a finding which was confirmed in the current study (Table IV).
The biggest limitation of our study was the high dropout of eligible participants, although the dropouts were distributed equally between the AAA families and the families of the spouses. Another limitation of the study was that the total number of living siblings of the spouses (n=337) was much smaller than that of the siblings of the AAA probands (n=988). This was partly due to the fact that 38% (143/375) of the AAA probands had no spouses. The average size of the living sibship (=probands+sisters+brothers) participating in the study was 3.0 [(333+166)/166] for the AAA proband families and 2.8 [(88+50)/50] for the spouse families, suggesting that there was no systematic bias in the recruitment of the spouses’ siblings. In addition, it is possible that the siblings of the AAA probands were more motivated to participate in the ultrasonography screening, since they had an affected sibling and might feel that they could benefit from knowing if they also had an AAA. Yet another limitation was the fact that the risk factor information was self-reported by the participants without verification using medical records. Our study demonstrated the difficulties in family studies of late-age-at-onset deadly diseases, since approximately 40% of the siblings were no longer alive at the time of recruitment.
In conclusion, this is the first study that compared the prevalence of AAA among the siblings of AAA patients to that in the spouses’ siblings and demonstrated a high prevalence of familial AAA. There was a significant difference between the siblings of the AAA patients and the siblings of the spouses both in the prevalence of AAA detected by ultrasonography and the observed life-time prevalence of AAA. These findings emphasize the importance of ultrasonography screening for AAA among the siblings of AAA patients.
Footnotes
Financial support: Supported in part by the National Heart, Lung, and Blood Institute, National Institutes of Health (grant HL064310).
Present address: Department of Vascular Surgery, KAISER PERMANENTE®, CA (C.W.C)
References
- 1.Kochanek KD, Smith BL. Deaths: preliminary data for 2002. Natl Vital Stat Rep. 2004;52:1–47. [PubMed] [Google Scholar]
- 2.Wilmink AB, Quick CR. Epidemiology and potential for prevention of abdominal aortic aneurysm. Br J Surg. 1998;85:155–162. doi: 10.1046/j.1365-2168.1998.00714.x. [DOI] [PubMed] [Google Scholar]
- 3.Heller JA, Weinberg A, Arons R, et al. Two decades of abdominal aortic aneurysm repair: have we made any progress? J Vasc Surg. 2000;32:1091–1100. doi: 10.1067/mva.2000.111691. [DOI] [PubMed] [Google Scholar]
- 4.Bengtsson H, Bergqvist D. Ruptured abdominal aortic aneurysm: a population-based study. J Vasc Surg. 1993;18:74–80. doi: 10.1067/mva.1993.42107. [DOI] [PubMed] [Google Scholar]
- 5.Kuivaniemi H, Shibamura H, Arthur C, et al. Familial abdominal aortic aneurysms: collection of 233 multiplex families. J Vasc Surg. 2003;37:340–345. doi: 10.1067/mva.2003.71. [DOI] [PubMed] [Google Scholar]
- 6.Kuivaniemi H, Tromp G. Search for the aneurysm susceptibility genes. In: keen R, Dobrin PB, eds. Development of aneurysms Georgetown: Landies Bioscience; 2000:219–233.
- 7.Kuivaniemi H, Shibamura H. Candidate Genes for Abdominal aortic Aneurysms. In: Liotta D, Del Rio M, Cooley D, eds. Diseases of the Aorta Buenos Aires, Argentina: Liotta Foundation Medical; 2003:89–100.
- 8.Johnston KW, Rutherford RB, Tilson MD, et al. Suggested standards for reporting on arterial aneurysms. Subcommittee on Reporting Standards for Arterial Aneurysms, Ad Hoc Committee on Reporting Standards, Society for Vascular Surgery and North American Chapter, International Society for Cardiovascular Surgery. J Vasc Surg. 1991;13:452–458. doi: 10.1067/mva.1991.26737. [DOI] [PubMed] [Google Scholar]
- 9.Baird PA, Sadovnick AD, Yee IM, et al. Sibling risks of abdominal aortic aneurysm. Lancet. 1995;346:601–604. doi: 10.1016/s0140-6736(95)91436-6. [DOI] [PubMed] [Google Scholar]
- 10.Lederle FA, Johnson GR, Wilson SE. Abdominal aortic aneurysm in women. J Vasc Surg. 2001;34:122–126. doi: 10.1067/mva.2001.115275. [DOI] [PubMed] [Google Scholar]
- 11.Majumder PP, St Jean PL, Ferrell RE, et al. On the inheritance of abdominal aortic aneurysm. Am J Hum Genet. 1991;48:164–170. [PMC free article] [PubMed] [Google Scholar]
- 12.Verloes A, Sakalihasan N, Koulischer L, et al. Aneurysms of the abdominal aorta: familial and genetic aspects in three hundred thirteen pedigrees. J Vasc Surg. 1995;21:646–655. doi: 10.1016/s0741-5214(95)70196-6. [DOI] [PubMed] [Google Scholar]
- 13.Shibamura H, Olson JM, van Vlijmen-Van Keulen C, et al. Genome scan for familial abdominal aortic aneurysm using sex and family history as covariates suggests genetic heterogeneity and identifies linkage to chromosome 19q13. Circulation. 2004;109:2103–2108. doi: 10.1161/01.CIR.0000127857.77161.A1. [DOI] [PubMed] [Google Scholar]
- 14.Lederle FA, Johnson GR, Wilson SE, et al. The aneurysm detection and management study screening program: validation cohort and final results. Aneurysm Detection and Management Veterans Affairs Cooperative Study Investigators. Arch Intern Med. 2000;160:1425–1430. doi: 10.1001/archinte.160.10.1425. [DOI] [PubMed] [Google Scholar]
- 15.Lederle FA, Johnson GR, Wilson SE, et al. Prevalence and associations of abdominal aortic aneurysm detected through screening. Aneurysm Detection and Management (ADAM) Veterans Affairs Cooperative Study Group. Ann Intern Med. 1997;126:441–449. doi: 10.7326/0003-4819-126-6-199703150-00004. [DOI] [PubMed] [Google Scholar]
- 16.Alcorn HG, Wolfson SK, Jr, Sutton-Tyrrell K, et al. Risk factors for abdominal aortic aneurysms in older adults enrolled in The Cardiovascular Health Study. Arterioscler Thromb Vasc Biol. 1996;16:963–970. doi: 10.1161/01.atv.16.8.963. [DOI] [PubMed] [Google Scholar]
- 17.Bengtsson H, Norrgard O, Angquist KA, et al. Ultrasonographic screening of the abdominal aorta among siblings of patients with abdominal aortic aneurysms. Br J Surg. 1989;76:589–591. doi: 10.1002/bjs.1800760620. [DOI] [PubMed] [Google Scholar]
- 18.Collin J, Walton J. Is abdominal aortic aneurysm familial? BMJ. 1989;299:493. doi: 10.1136/bmj.299.6697.493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Webster MW, St Jean PL, Steed DL, et al. Abdominal aortic aneurysm: results of a family study. J Vasc Surg. 1991;13:366–372. doi: 10.1067/mva.1991.26359. [DOI] [PubMed] [Google Scholar]
- 20.Adamson J, Powell JT, Greenhalgh RM. Selection for screening for familial aortic aneurysms. Br J Surg. 1992;79:897–898. doi: 10.1002/bjs.1800790914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bengtsson H, Sonesson B, Lanne T, et al. Prevalence of abdominal aortic aneurysm in the offspring of patients dying from aneurysm rupture. Br J Surg. 1992;79:1142–1143. doi: 10.1002/bjs.1800791108. [DOI] [PubMed] [Google Scholar]
- 22.van der Lugt A, Kranendonk SE, Baars AM. [Screening for familial occurrence of abdominal aortic aneurysm] Ned Tijdschr Geneeskd. 1992;136:1910–1913. [PubMed] [Google Scholar]
- 23.Adams DC, Tulloh BR, Galloway SW, et al. Familial abdominal aortic aneurysm: prevalence and implications for screening. Eur J Vasc Surg. 1993;7:709–712. doi: 10.1016/s0950-821x(05)80721-2. [DOI] [PubMed] [Google Scholar]
- 24.Moher D, Cole CW, Hill GB. Definition and management of abdominal aortic aneurysms: results from a Canadian survey. Can J Surg. 1994;37:29–32. [PubMed] [Google Scholar]
- 25.Fitzgerald P, Ramsbottom D, Burke P, et al. Abdominal aortic aneurysm in the Irish population: a familial screening study. Br J Surg. 1995;82:483–486. doi: 10.1002/bjs.1800820418. [DOI] [PubMed] [Google Scholar]
- 26.Larcos G, Gruenewald SM, Fletcher JP. Ultrasound screening of families with abdominal aortic aneurysm. Australas Radiol. 1995;39:254–256. doi: 10.1111/j.1440-1673.1995.tb00287.x. [DOI] [PubMed] [Google Scholar]
- 27.Jaakkola P, Kuivaniemi H, Partanen K, et al. Familial abdominal aortic aneurysms: screening of 71 families. Eur J Surg. 1996;162:611–617. [PubMed] [Google Scholar]
- 28.van der Graaf Y, Akkersdijk GJ, Hak E, et al. Results of aortic screening in the brothers of patients who had elective aortic aneurysm repair. Br J Surg. 1998;85:778–780. doi: 10.1046/j.1365-2168.1998.00652.x. [DOI] [PubMed] [Google Scholar]
- 29.Salo JA, Soisalon-Soininen S, Bondestam S, et al. Familial occurrence of abdominal aortic aneurysm. Ann Intern Med. 1999;130:637–642. doi: 10.7326/0003-4819-130-8-199904200-00003. [DOI] [PubMed] [Google Scholar]
- 30.Rossaak JI, Hill TM, Jones GT, et al. Familial abdominal aortic aneurysms in the Otago region of New Zealand. Cardiovasc Surg. 2001;9:241–248. doi: 10.1016/s0967-2109(00)00140-x. [DOI] [PubMed] [Google Scholar]
- 31.Ashton HA, Buxton MJ, Day NE, et al. The Multicentre Aneurysm Screening Study (MASS) into the effect of abdominal aortic aneurysm screening on mortality in men: a randomised controlled trial. Lancet. 2002;360:1531–1539. doi: 10.1016/s0140-6736(02)11522-4. [DOI] [PubMed] [Google Scholar]
- 32.Wilmink TB, Quick CR, Hubbard CS, et al. The influence of screening on the incidence of ruptured abdominal aortic aneurysms. J Vasc Surg. 1999;30:203–208. doi: 10.1016/s0741-5214(99)70129-1. [DOI] [PubMed] [Google Scholar]
- 33.Lindholt JS, Juul S, Fasting H, et al. Hospital costs and benefits of screening for abdominal aortic aneurysms. Results from a randomised population screening trial. Eur J Vasc Endovasc Surg. 2002;23:55–60. doi: 10.1053/ejvs.2001.1534. [DOI] [PubMed] [Google Scholar]
- 34.Heather BP, Poskitt KR, Earnshaw JJ, et al. Population screening reduces mortality rate from aortic aneurysm in men. Br J Surg. 2000;87:750–753. doi: 10.1046/j.1365-2168.2000.01476.x. [DOI] [PubMed] [Google Scholar]
- 35.Earnshaw JJ, Shaw E, Whyman MR, et al. Screening for abdominal aortic aneurysms in men. BMJ. 2004;328:1122–1124. doi: 10.1136/bmj.328.7448.1122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Cole CW, Hill GB, Millar WJ, et al. Selective screening for abdominal aortic aneurysm. Chronic Dis Can. 1996;17:51–55. [PubMed] [Google Scholar]
- 37.Norman PE, Jamrozik K, Lawrence-Brown MM, et al. Population based randomised controlled trial on impact of screening on mortality from abdominal aortic aneurysm. BMJ. 2004;329:1259. doi: 10.1136/bmj.38272.478438.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Scott RA, Wilson NM, Ashton HA, et al. Influence of screening on the incidence of ruptured abdominal aortic aneurysm: 5-year results of a randomized controlled study. Br J Surg. 1995;82:1066–1070. doi: 10.1002/bjs.1800820821. [DOI] [PubMed] [Google Scholar]
- 39.Kent KC, Zwolak RM, Jaff MR, et al. Screening for abdominal aortic aneurysm: a consensus statement. J Vasc Surg. 2004;39:267–269. doi: 10.1016/j.jvs.2003.08.019. [DOI] [PubMed] [Google Scholar]
- 40.U. S. Preventive Service Task Force. Screening for abdominal aortic aneurysm: recommendation statement. Ann Intern Med. 2005;142:198–202. doi: 10.7326/0003-4819-142-3-200502010-00011. [DOI] [PubMed] [Google Scholar]


