Abstract
Severe asthma, although difficult to define, includes all cases of difficult/therapy-resistant disease of all age groups and bears the largest part of morbidity and mortality from asthma. Acute, severe asthma, status asthmaticus, is the more or less rapid but severe asthmatic exacerbation that may not respond to the usual medical treatment. The narrowing of airways causes ventilation perfusion imbalance, lung hyperinflation, and increased work of breathing that may lead to ventilatory muscle fatigue and life-threatening respiratory failure.
Treatment for acute, severe asthma includes the administration of oxygen, β2-agonists (by continuous or repetitive nebulisation), and systemic corticosteroids. Subcutaneous administration of epinephrine or terbutaline should be considered in patients not responding adequately to continuous nebulisation, in those unable to cooperate, and in intubated patients not responding to inhaled therapy. The exact time to intubate a patient in status asthmaticus is based mainly on clinical judgment, but intubation should not be delayed once it is deemed necessary. Mechanical ventilation in status asthmaticus supports gas-exchange and unloads ventilatory muscles until aggressive medical treatment improves the functional status of the patient. Patients intubated and mechanically ventilated should be appropriately sedated, but paralytic agents should be avoided. Permissive hypercapnia, increase in expiratory time, and promotion of patient-ventilator synchronism are the mainstay in mechanical ventilation of status asthmaticus. Close monitoring of the patient's condition is necessary to obviate complications and to identify the appropriate time for weaning. Finally, after successful treatment and prior to discharge, a careful strategy for prevention of subsequent asthma attacks is imperative.
Keywords: difficult/therapy-resistant asthma, dynamic hyperinflation, fatal asthma, permissive hypercapnia, status asthmaticus
Introduction
Bronchial asthma has a wide clinical spectrum ranging from a mild, intermittent disease to one that is severe, persistent, and difficult to treat, which in some instances can also be fatal [1,2,3,4]. Asthma deaths, although uncommon (one in 2000 asthmatics), have increased over the last decades [2], with more than 5000 deaths reported annually in the USA and 100,000 deaths estimated yearly throughout the world [1,2]. Patients at greater risk for fatal asthma attacks are mainly those with severe, unstable disease, although death can occur to anyone if the asthma attack is intense enough [2,3,4]. Most deaths from asthma are preventable, however, particularly those among young persons. Morbidity in asthma is a considerable problem, and is mainly related to the more severe phenotypes of the disease. The nature of severe, chronic asthma and its optimal management measures remain poorly understood. Patients affected have also the greatest impact on healthcare costs, which have increased rapidly over the last years.
Severity in asthma is difficult to define and its characterization should take into account four components: biological severity (yet to be elucidated in asthma); physiological severity (where the key measures for its definition are pulmonary function tests and assessment of symptom scores); functional severity (that represents the impact of the disease on an individual's ability to perform age-appropriate activities); and burden of illness (viewed in terms of the emotional, social, and financial impact of asthma on the individual, the family and society as a whole) [5].
A large number of terms are used by clinicians when referring to asthmatic patients who have severe disease that is difficult to treat. The National Institute of Health Guidelines for the Diagnosis and Management of Asthma have characterized severe, persistent asthma, in untreated patients, by the presence of several criteria: continual symptoms (also occurring frequently at night) that cause limitations in physical activity; frequent exacerbations; persistent airflow obstruction with forced expired volume in 1 sec (FEV1) and/or peak expiratory flow (PEF) of less than 60% of the predicted value; and PEF diurnal variability greater than 30% [1].
Severe asthma, defined as disease that is unresponsive to current treatment, including systemically administered corticosteroids, is an important subset of asthma and it is estimated that 5–10% of all patients are affected [6]. 'Difficult asthma', defined as the asthmatic phenotype characterized by failure to achieve control despite maximally recommended doses of inhaled steroids prescribed, encompasses a great proportion of patients with severe, persistent asthma [7]. The term 'brittle asthma' describes subgroups of patients with severe, unstable asthma who maintain a wide PEF variability despite high doses of inhaled steroids [8]. The classification of this relatively rare phenotype of asthma into two types has been recently suggested. Type 1 brittle asthma is characterized by a wide, persistent and chaotic PEF variability (>40% diurnal variation for >50% of the time over a period of at least 150 days) despite considerable medical therapy. Type 2 brittle asthma is characterized by sudden acute attacks occurring in less than three hours, without an obvious trigger, on a background of apparent normal airway function or well-controlled asthma [8].
Nocturnal asthma ('early morning dip') is the commonest pattern of instability in asthma and usually denotes suboptimal treatment. Some unstable patients with asthma may present an early morning and an additional evening deterioration pattern in lung function ('double dip'). Premenstrual asthma is a characteristic pattern of instability in asthma where an increase in symptoms and a decrease in PEF are observed two to five days before the menstrual period, with improvement once menstruation begins. Premenstrual exacerbation of asthma, although usually mild and responsive to an increase in antiasthmatic therapy, may also be severe and appear steroid-resistant.
Steroid-resistant asthma refers to those (rare) patients with chronic asthma who are unresponsive to the administration of high dose of steroids (10–14 day course of 20 mg or more, twice daily, of prednisone) [9,10]. Steroid-dependent asthma is defined as asthma that can be controlled only with high doses of oral steroids and may be part of a continuum with steroid-resistant asthma at the other extreme. Aspirin-induced asthma, adult-onset asthma and asthma with 'fixed' obstruction are also patterns of severity in asthma. Recently, the European Respiratory Society Task Force on Difficult/ Therapy-Resistant Asthma adopted such a term to include all the above-described cases of severe, and 'difficult to treat' disease of all age groups [11].
Acute, severe asthma
Asthma exacerbations are acute or subacute episodes of breathlessness, cough, wheezing, and chest tightness, or any combination of these symptoms. Exacerbations are associated with airways obstruction that should be documented and quantified by PEF or FEV1 measurement. Objective measures of airways obstruction in most asthmatics are considered more reliable to indicate the severity of an exacerbation than changes in the severity of symptoms. The intensity of asthma exacerbations may vary from mild to severe. Among patients attending an emergency department, the severity of obstruction in terms of FEV1 is, on average, 30–35% of predicted normal [12].
Status asthmaticus
Acute, severe asthma describes the serious asthmatic attack that places the patient at risk of developing respiratory failure, a condition referred to as status asthmaticus [13,14]. The time course of the asthmatic crisis as well as the severity of airways obstruction may vary broadly [14]. In some patients who present with asthmatic crisis, repeated PEF measurements when available may document subacute worsening of expiratory flow over several days before the appearance of severe symptoms, the so-called 'slow onset asthma exacerbation'. In others, however, lung function may deteriorate severely in less than one hour, the so-called 'sudden onset asthma exacerbation' [14,15]. Slow onset asthma exacerbations are mainly related to faults in management (inadequate treatment, low compliance, inappropriate control, coexisting psychological factors) that should be investigated and corrected in every patient in advance. On the other hand, massive exposure to common allergens, sensitivity to nonsteroidal anti-inflammatory agents, and sensitivity to food allergens and sulphites are mainly considered the triggers in sudden asthma exacerbations. Without prompt and appropriate treatment, status asthmaticus may result in ventilatory failure and death.
Fatal asthma
Two different patterns of fatal asthma have been described (Table 1). The greater number of deaths from asthma (80–85%) occurs in patients with severe and poorly controlled disease who gradually deteriorate over days or weeks, the so-called 'slow onset – late arrival' or type 1 scenario of asthma death [2,3,4,16,17,18]. This pattern of asthma death is generally considered preventable. A variation of this pattern is a history of unstable disease, which is partially responsive to treatment, upon which a major attack is superimposed. In both situations, hypercapnic respiratory failure and mixed acidosis ensues and the patient succumbs to asphyxia, or if mechanical ventilation is applied, to complications such as barotrauma and ventilator-associated pneumonia. Pathologic examination in such cases shows extensive airways plugging by dense and tenacious mucous mixed to inflammatory and epithelial cells, epithelial denudation, mucosal edema, and an intense eosinophilic infiltration of the submucosa. In a small proportion of patients, death from asthma can be sudden and unexpected (sudden asphyxic asthma), without obvious antecedent long-term deterioration of asthma control, the so-called 'sudden onset' or type 2, scenario of asthma death [18,19,20,21]. Affected individuals develop rapidly severe hypercapnic respiratory failure with combined metabolic and respiratory acidosis, and succumb to asphyxia. If treated (medically and/or mechanically ventilated), however, they present a faster rate of improvement than patients with slow-onset asthmatic crisis. Pathologic examination in such cases shows 'empty' airways (no mucous plugs) in some patients, and in almost all patients, a greater proportion of neutrophils than eosinophils infiltrating the submucosa is observed [20,21,22].
Table 1.
Different patterns of fatal asthma
| Scenario of asthma death | ||
| Variable | Type 1 | Type 2 |
| Time course | Subacute worsening (days). 'Slow onset – late arrival' | Acute deterioration (hours). 'Sudden asphyxic asthma' |
| Frequency | ≅ 80–85% | ≅ 15–20% |
| Airways | Extensive mucous plugging | More or less 'empty' bronchi |
| Inflammation | Eosinophils | Neutrophils |
| Response to treatment | Slow | Faster |
| Prevention | Possible | (?) |
Risk factors
Patients at high risk of asthma death require special attention and, in particular, intensive education, monitoring and care. Risk factors for death from asthma are [1]:
1. Past history of sudden severe exacerbations.
2. Prior intubation for asthma.
3. Prior admission for asthma to an intensive care unit.
4. Two or more hospitalizations for asthma in the past year.
5. Three or more emergency care visits for asthma in the past year.
6. Hospitalization or an emergency care visit for asthma within the past month.
7. Use of >2 canisters per month of inhaled short-acting β2-agonist.
8. Current use of systemic corticosteroids or recent withdrawal from systemic corticosteroids.
9. Difficulty perceiving airflow obstruction or its severity.
10. Comorbidity, as from cardiovascular diseases or chronic obstructive pulmonary disease.
11. Serious psychiatric disease or psychosocial problems.
12. Low socioeconomic status and urban residence.
13. Illicit drug use
14. Sensitivity to alternaria.
Pathophysiology
Asthma is an inflammatory disease of the airways that appears to involve a broad range of cellular- and cytokine-mediated mechanisms of tissue injury [1]. In asthmatic subjects who die suddenly of an asthma attack, the peripheral airways frequently exhibit occlusion of the bronchial lumen by inspissated secretions, thickened smooth muscles, and bronchial wall inflammatory infiltration and edema [22,23]. These changes observed in the asthmatic airways support the hypothesis that peripheral airways occlusion forms the pathologic basis of the gas exchange abnormalities observed in acute, severe asthma. In such patients, widespread occlusion of the airways leads to the development of extensive areas of alveolar units in which ventilation (V) is severely reduced but perfusion (Q) is maintained (i.e. areas with very low V/Q ratios, frequently lower than 0.1) [24].
Hypoxemia, hypercapnia and lactic acidosis
Intrapulmonary shunt appears to be practically absent in the majority of patients because of the collateral ventilation, the effectiveness of the hypoxic pulmonary vasoconstriction, and the fact that the airway obstruction can never be functionally complete [24]. Hypoxemia is therefore common in every asthmatic crisis of some severity; mild hypoxia is easily corrected with the administration of relatively low concentrations of supplemental oxygen [25]. More severe hypoxemia and the need for higher concentrations of supplemental oxygen may relate to some contribution of shunt physiology.
Analysis of arterial blood gases is important in the management of patients with acute, severe asthma, but it is not predictive of outcome. In the early stages of acute, severe asthma, analysis of arterial blood gases usually reveals mild hypoxemia, hypocapnia and respiratory alkalosis. If the deterioration in the patient's clinical status lasts for a few days there may be some compensatory renal bicarbonate secretion, which manifests as a non-anion-gap metabolic acidosis. As the severity of airflow obstruction increases, arterial carbon dioxide (PaCO2) first normalizes and subsequently increases because of patient's exhaustion, inadequate alveolar ventilation and/or an increase in physiologic death space.
Hypercapnia is not usually observed for FEV1 values higher than 25% of predicted normal, but in general, there is no correlation between airflow rates and gas exchange markers. Furthermore, paradoxical deterioration of gas exchange, while flow rates improve after the administration of β-adrenergic agonists is not uncommon.
Respiratory acidosis is always present in hypercapnic patients who rapidly deteriorate and in severe, advanced-stage disease, metabolic (lactic) acidosis may coexist. The pathogenesis of lactic acidosis in the acutely severe asthmatic patient remains to be fully elucidated. There are several mechanisms that are probably involved [13]: the use of high-dose parenteral β-adrenergic agonists; the highly increased work of breathing resulting in anaerobic metabolism of the ventilatory muscles and overproduction of lactic acid; the eventually coexisting profound tissue hypoxia; the presence of intracellular alkalosis; and the decreased lactate clearance by the liver because of hypoperfusion.
During an asthma attack, all indices of expiratory flow, including FEV1, FEV1/FVC (forced vital capacity), PEF, maximal expiratory flows at 75%, 50%, and 25% of vital capacity (MEF75, MEF50, and MEF25 respectively) and maximal expiratory flow between 25% and 75% of the FVC (MEF25–75) are reduced significantly. The abnormally high airway resistance observed (5–15 times normal) is directly related to the shortening of airway smooth muscle, edema, inflammation, and excessive luminal secretions, and leads to a dramatic increase in flow-related resistive work of breathing. Although the increased resistive work significantly contributes to patient functional status, however, the elastic work also increases significantly, and enhances respiratory muscle fatigue and ventilatory failure [26,27].
Dynamic hyperinflation
In asthmatic crisis, remarkably high volumes of functional residual capacity (FRC), total lung capacity and residual volume can be observed, and tidal breathing occurs near predicted total lung capacity. Lung hyperinflation that develops as a result of acute airflow obstruction, however, can also be beneficial since it improves gas exchange. The increase in lung volume tends to increase airway caliber and consequently reduce the resistive work of breathing. This is accomplished, however, at the expense of increased mechanical load and elastic work of breathing.
Lung hyperinflation in acute, severe asthma, is primarily related to the fact that the highly increased airway expiratory resistance, the high ventilatory demands, the short expiratory time, and the increased post-inspiratory activity of the inspiratory muscles (all present at variable degrees in patients in status asthmaticus) do not permit the respiratory system to reach static equilibrium volume at the end of expiration (Fig. 1). Inspiration, therefore, begins at a volume in which the respiratory system exhibits a positive recoil pressure. This pressure is called intrinsic positive-end expiratory pressure (PEEPI) or auto-PEEP. This phenomenon is called dynamic hyperinflation and is directly proportional to minute ventilation (VE) and to the degree of airflow obstruction.
Figure 1.
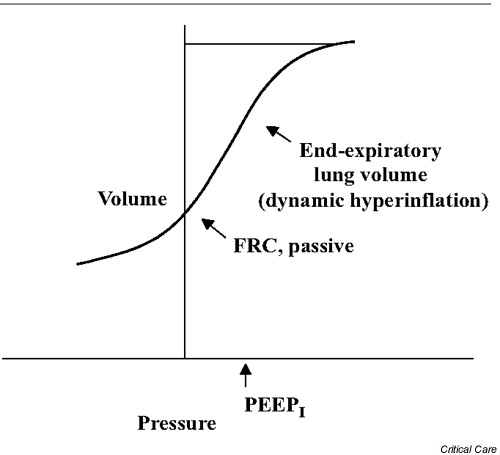
Relationship of volume and pressure in the respiratory system. Dynamic hyperinflation adds an elastic load to inspiratory muscles: to initiate inspiratory flow the inspiratory muscles must first overcomeintrinsic positive end-expiratory pressure (PEEPI). Dynamic hyperinflation shifts tidal breathing to a less compliant part of the respiratory system pressure-volume curve leading to an increased pressure-volume work of breathing. FRC, functional residual capacity.
Dynamic hyperinflation has significant unfavorable effects on lung mechanics. First, dynamic hyperinflation shifts tidal breathing to a less compliant part of the respiratory system pressure-volume curve leading to an increased pressure-volume work of breathing. Second, it flattens the diaphragm and reduces generation of force since muscle contraction results from a mechanically disadvantageous fiber length. Third, dynamic hyperinflation increases dead space, thus increasing the minute volume required to maintain adequate ventilation. Conceivably, asthma increases all three components of respiratory system load, namely resistance, elastance, and minute volume. Finally, in acute severe asthma, the diaphragmatic blood flow may also be reduced. Under these overwhelming conditions, in the case of persistence of the severe asthma attack, ventilatory muscles cannot sustain adequate tidal volumes and respiratory failure ensues.
Effects of asthma on the cardiovascular system
Acute, severe asthma alters profoundly the cardiovascular status and function [28,29]. In expiration, because of the effects of dynamic hyperinflation, the systemic venous return decreases significantly, and again rapidly increases in the next respiratory phase. Rapid right ventricular filling in inspiration, by shifting the interventricular septum toward the left ventricle, may lead to left ventricular diastolic dysfunction and incomplete filling. The large negative intrathoracic pressure generated during inspiration increases left ventricular after-load by impairing systolic emptying. Pulmonary artery pressure may also be increased due to lung hyperinflation, thereby resulting in increased right ventricular afterload. These events in acute, severe asthma may accentuate the normal inspiratory reduction in left ventricular stroke volume and systolic pressure, leading to the appearance of pulsus paradoxus (significant reduction of the arterial systolic pressure in inspiration). A variation greater than 12 mmHg in systolic blood pressure between inspiration and expiration represents a sign of severity in asthmatic crisis. In advanced stages, when ventilatory muscle fatigue ensues, pulsus paradoxus will decrease or disappear as force generation declines. Such status harbingers impeding respiratory arrest.
Clinical and laboratory assessment
Patients with acute, severe asthma appear seriously dyspneic at rest, are unable to talk with sentences or phrases, are agitated and sit upright (Table 2) [1]. Drowsiness or confusion are always ominous signs and denote imminent respiratory arrest. Vital signs in acute, severe asthma are: respiratory rate usually >30 breaths/min; heart rate >120 beats/min; wheezing throughout both the inspiration and the expiration; use of accessory respiratory muscles; evidence of suprasternal retractions; and pulsus paradoxus >12 mmHg.
Table 2.
Clinical and functional assessment of severe asthma exacerbations
| Variable | Severe exacerbation | Imminent respiratory arrest |
| Symptoms | ||
| Dyspnea | At rest | |
| Speech | Single words, not sentences of phrases | |
| Alertness | Agitated | Drowsy or confused |
| Signs | ||
| Respiratory rate | >30 breaths/min | |
| Heart rate | >120 beats/min | Bradycardia |
| Pulsus paradoxus | >25 mmHg | Absence (muscle fatigue) |
| Use of accessory muscles | Evident | Abdominal paradox |
| Wheeze | Present – loud | 'Silent chest' |
| Functional assessment | ||
| PEF | <50% of predicted | |
| PaO2 | <60 mmHg | |
| PaCO2 | >42 mmHg | |
| SaO2 | <90% |
PaCO2, arterial carbon dioxide; PaO2, arterial oxygen; PEF, peak expiratory flow; SaO2, oxygen saturation. Adapted from the National Heart, Lung and Blood Institute report [1].
Pulsus paradoxus can be a valuable sign of asthma severity but its detection should not delay prompt treatment. Paradoxical thoracoabdominal movement and the absence of pulsus paradoxus suggest ventilatory muscle fatigue and, together with the disappearance of wheeze and the transition from tachycardia to bradicardia, represent signs of imminent respiratory arrest. The usual cardiac rhythm in acute, severe asthma is sinus tachycardia, although supraventricular arrhythmias are not uncommon. Less frequently ventricular arrhythmias may be observed in elderly patients.
Electrocardiographic signs of right heart strain such as right axis deviation, clockwise rotation, and evidence of right ventricular hypertrophy may be observed in acute, severe asthma and usually resolve within hours of effective treatment [30].
Physical examination should be especially directed toward the detection of complications of asthma: pneumothorax; pneumomediastinum; subcutaneous emphysema; pneumopericardium; pulmonary interstitial emphysema; pneumoretroperitoneum; tracheoesophageal fistula (in the mechanically ventilated); cardiac arrhythmias, myocardial ischemia or infarction; mucous plugging, atelectasis; pneumonia; sinusitis; coexisting vocal cord dysfunction; theophylline toxicity; electrolyte disturbances (hypokalemia, hypophosphatemia, hypomagnesemia); lactic acidosis; and hyperglycemia.
Complications of acute, severe asthma
Pneumothorax eventually associated with pneumomediastinum, subcutaneous emphysema (Fig. 2), pneumopericardium and tracheoesofageal fistula (in the mechanically ventilated patient) (Fig. 3) are rare but potentially severe complications of acute, severe asthma. Myocardial ischemia should be considered in older patients with coronary artery disease. Mucus plugging and atelectasis are not rare and usually respond to effective treatment. Other complications to consider include theophylline toxicity, lactic acidosis, electrolyte disturbances (hypokalemia, hypophosphatemia, hypomagnesemia), myopathy and ultimately anoxemic brain injury [13].
Figure 2.
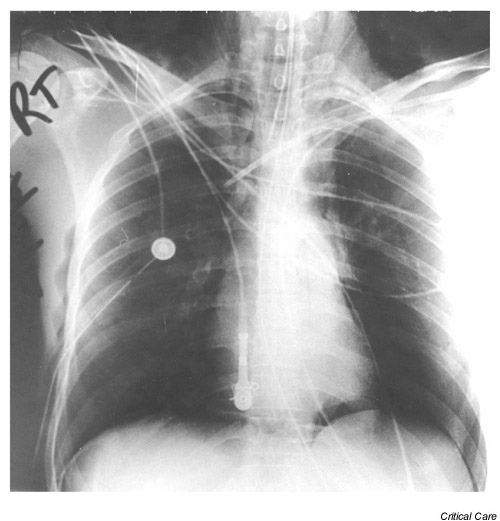
Pneumomediastinum-bilateral pneumothorax in an intubated patient in status asthmaticus. Radiolucent stripes along the soft tissues of the mediastinum, and the continuous diaphragm sign indicate the presence of pneumomediastinum. Bilateral pneumothorax is also seen (deep costophrenic sulcuses and hyperlucent hemidiaphragms bilaterally). Subcutaneous emphysema is also seen on the left of the figure.
Figure 3.
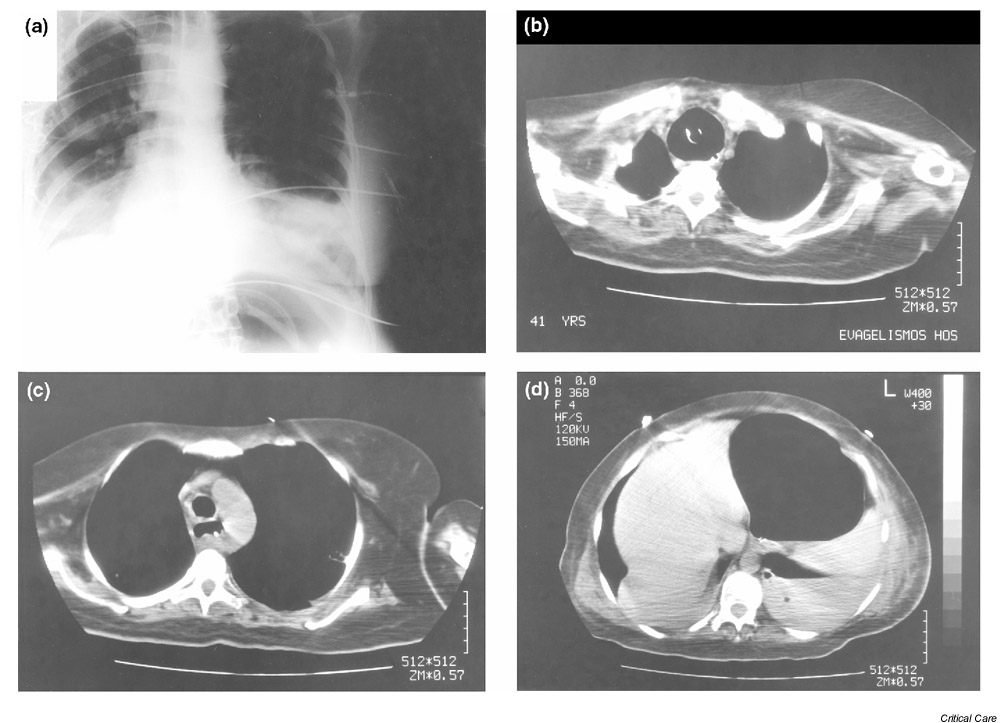
Tracheoesophageal fistula in an intubated patient in status asthmaticus (iatrogenic complication). (a) The chest x-ray shows an abnormal distension of the fundus of the stomach. (b) The overinflated balloon of the endotracheal tube is evident in the computerized tomography of the chest and upper abdomen. The lumen of the endotracheal tube is seen centrally. The nasogastric tube is slightly displaced on the left by the endotracheal balloon and indicates the position of the esophagus. (c) At lower level, the trachea has a normal configuration. The nasogastric tube is again seen, but the esophagus is dilated with air (tracheoesophageal fistula). (d) Extensive dilatation of the fundus of the stomach is seen. The nasogastric junction is indicated by the visualization of the nasogastric tube.
Patient monitoring
Close monitoring by serial measurements of lung function (PEF or FEV1 at bedside) to quantify the severity of airflow obstruction and its response to treatment are of paramount importance. PEF or FEV1 <30–50% of predicted or personal best indicates severe attack. Attention should be paid to measuring lung function in the severely ill patient, however, because the deep inspiration maneuver involved in PEF or FEV1 measurement may precipitate respiratory arrest by worsening bronchospasm [31]. Failure of treatment to improve expiratory flow predicts a more severe course and the need for hospitalization [32].
Blood gas analysis
Although arterial blood gas analysis is useful in the management of patients with acute, severe asthma, it is not predictive of outcome. Arterial blood gas determinations are necessary in the more severe asthmatic crisis, when oxygen saturation is lower than 90%, and in the case of no response or deterioration. In such cases, analysis of blood gases usually reveals severe hypoxemia with arterial oxygen (PaO2) lower than 60 mmHg, hypocapnia and respiratory alkalosis with or without compensatory metabolic acidosis. As the severity of airflow obstruction increases, PaCO2 first normalizes and subsequently increases. The transition from hypocapnia to normocapnia is an important sign of severe clinical deterioration and the appearance of hypercapnia probably indicates the need for mechanical ventilation [13]. Hypercapnia per se is not an indication for intubation, however, and such patients may respond successfully to the application of aggressive medical therapy [1].
Metabolic acidosis denotes impeding respiratory arrest. Repeated measurements of blood gases may be necessary in severe patents to determine clinical deterioration or improvement, and may offer additional information to clinical judgment and PEF measurements.
Chest radiography
Chest radiographs in the majority of patients with acute asthma will be normal [33] but chest radiographic examination is a valuable tool to exclude complications. The cost of the radiographic examination is relatively inexpensive, and the radiation risk is low, therefore, since severe asthmatic attacks may be associated with some complication, it would seem that a chest radiogram would be indicated in all asthmatic attacks of sufficient severity to bring the patient in the emergency department. Chest radiographic examination, however, should never be permitted to delay initiation of treatment.
Blood counts, drug-monitoring, and electrolytes
Complete blood counts may be appropriate in patients with fever and/or purulent sputum. Determination of serum theophylline levels is mandatory in every patient under treatment with theophylline. Finally, it would be prudent to measure electrolytes in patients who have been taking diuretics regularly and in patients with cardiovascular disease because excessive use of β2-agonists may decrease serum levels of potassium, magnesium, and phosphate.
Hospitalization
The immediate prognosis of acute asthma is usually not determined by the intensity of the presenting symptoms or by the severity of the airways obstruction in terms of PEF or FEV1, but rather by the acute response to treatment [32,34]. In general, and for those patients who are not immediate candidates for admission to the intensive care unit, four to six hours of treatment in the emergency department have been considered necessary before deciding on disposition [13,35]. Further studies, however, have shown that the great majority of patients (77%) resolve their symptoms within two hours of presentation, and there is little to be gained by prolonging treatment in the emergency department [34].
There are a number of additional factors that may influence the decision to hospitalize a patient [1]: duration and severity of symptoms; severity of airflow obstruction; course and severity of prior exacerbations; medication use at the time of exacerbation, (access to medical care and medications); adequacy of support and home conditions; and presence of psychiatric illness. Admission to an intensive care unit is mandatory in patients in respiratory arrest, altered mental status and serious concomitant cardiac complications. This should be guaranteed in every patient with severe airflow obstruction who demonstrates a poor response to treatment, or in any patient who deteriorates despite therapy [13]. For less severe patients who continue to have an incomplete response (PEF or FEV1 < 60% predicted) after two hours of continuous nebulization with β2-agonists in the emergency department, admission to the general medical ward is recommended.
Management
Early treatment of asthma exacerbations should be the best strategy for management [1,36]. Furthermore, patients at high risk of asthma-related death require special attention, particularly intensive education, monitoring, and care. Patients, their families and their physicians, however, frequently underestimate the severity of asthma. Important elements for the prevention of exacerbations and for early asthma treatment include [1]:
1. A written action plan for home self-management of asthma exacerbations, especially for those patients with severe asthma or a history of previous severe asthma attacks.
2. Provide the patient with the necessary skills to recognize early signs of asthma worsening.
3. Clear instructions for appropriate intensification of therapy in case of deterioration.
4. Prompt communication between patient and clinician about any serious deterioration of asthma control.
Early home management of asthma exacerbations is of paramount importance since it avoids treatment delay and prevents clinical deterioration. The effectiveness of care depends on the abilities of the patients and/or their families, and on the availability of emergency care equipment (peak flow meter, appropriate medications, nebulizer, and eventually, supplemental oxygen).
Pharmacologic management
In the emergency department, a brief history regarding time of onset, cause of exacerbation, severity of symptoms (especially in comparison to previous attacks), prior hospitalizations and/or emergency department visits for asthma, prior intubation or intensive care admission, and complicating illness may be useful for treatment decisions. The primary therapies for acute severe asthma include, the administration of oxygen, inhaled β2-agonists, and systemic corticosteroids. The intensity of pharmacological treatment and patient's surveillance should correspond to the severity of the exacerbation [1].
Oxygen treatment (by nasal cannulae or mask) is recommended for most patients who present with severe exacerbation in order to maintain oxygen saturation >90% (>95% in pregnant women and in patients with coexistent cardiac disease).
Inhaled β2-agonists
Continuous or repetitive nebulisation of short-acting β2-agonists is the most effective means of reversing airflow obstruction and can be given safely. Continuous nebulisation of β2-agonists may be more effective in children and severely obstructed adults [37,38,39]. Salbutamol (albuterol) is the most frequently used agent because of its potency, duration of action (four to six hours) and β2-selectivity. Continuous or repetitive nebulisation of salbutamol should be preferred because duration of activity and effectiveness of β2-agonists are inversely related to the severity of airways obstruction [13]. The usual dose is 2.5 mg of salbutamol (0.5 ml) in 2.5 ml normal saline for each nebulisation (Table 3) [34]. Nebulised β2-agonists should continue until a significant clinical response is achieved or serious side effects appear (severe tachycardia, or arrhythmias). Prior ineffective use of β2-agonists does not preclude their use and does not limittheir efficacy [13]. Inhaled therapy with β2-agonists appears to be equal to, or even better than, their intravenous infusion in treating airways obstruction in patients with severe asthma [13].
Table 3.
Pharmacologic management in the emergency department
| Agent | Dose |
| Salbutamol (albuterol) | 2.5 mg (0.5 ml) in 2.5 ml normal saline by nebulisation continuously, or every 15–20 min until a significant clinical response is achieved or serious side effects appear |
| Epinephrine | 0.3–0.4 ml of a 1:1000 solution subcutaneously every 20 min for 3 doses |
| Terbutaline | Preferable to epinephrine in pregnancy |
| β-agonists | Intravenous administration should be considered in patients who have not responded to inhaled or subcutaneous treatment, in whom respiratory arrest is imminent |
| Corticosteroids | Methylprednisolone 60–125 mg (intravenous) or prednisone 40 mg (oral) |
| Anticholinergics | Ipratropium bromide 0.5 mg by nebulisation every 1–4 hours, combined with salbutamol |
| Methylxanthines | Theophylline 5 mg/kg (intravenous) over 30 min – loading dose in patients not already on theophylline, followed by 0.4 mg/kg/hour intravenous maintenance dose. Serum levels should be checked within 6 hours |
Anticholinergics and methylxanthines
Anticholinergics, such as ipratropium bromide (Table 3), may be considered in the emergency treatment of asthma but there is controversy on their ability to offer additional bronchodilation [40,41]. Methylxanthines, such as theophylline (Table 3), in the emergency department are of debated efficacy and not generally recommended [1,42]. Several authors, however, consider that there is enough data demonstrating that theophylline treatment in the emergency department benefits patients after 24 hours. Its non bronchodilating properties, including its action on the diaphragm and its anti-inflammatory effects, may thus warrant the use of theophylline in the emergency care of acute, severe asthma [43].
Corticosteroid treatment
Systemic corticosteroids (to speed the resolution and reduce relapse) are recommended for most patients in the emergency department, especially those with moderate-to-severe exacerbation and patients who do not respond completely to initial β2-agonist therapy [1,44,45]. The intensification of a patient's corticosteroids therapy, however, should begin much earlier, at the first sign of loss of asthma control. Corticosteroids in the emergency department may also help to reduce mortality from asthma [3]. Since benefits from corticosteroid treatment are not usually seen before six to twelve hours, early administration is necessary. A recent study reports for the first time that large doses of inhaled corticosteroids (18 mg flunisolide in three hours) administered in the emergency department, in addition to β2-agonists, speed the resolution of acute bronchoconstriction [46]. Furthermore, another study recently demonstrated that a single dose of inhaled budesonide (2.4 mg) significantly reduced sputum eosinophils and airway hyperesponsiveness in six hours [47]. These studies appear to also support a role for inhaled steroid treatment in asthma exacerbations, but additional studies are necessary to assess steroid behavior in these conditions [48].
Long-term treatment with inhaled corticosteroids has been shown to reduce hospitalization rates in younger patients with asthma [49] and to reduce the risk of rehospitalization and all-cause mortality in elderly asthmatics [50]. The optimal dose and dosing frequency of systemic corticosteroids in the severe hospitalized asthmatics are not clearly established. One common approach is the intravenous administration of 60–125 mg methylprednisolone every six hours during the initial 24–48 hours of treatment (Table 3), followed by 60–80 mg daily in improving patients, with gradual tapering during the next two weeks [13,51]. In addition to common and well-known side effects of corticosteroid administration (hyperglycemia, hypertension, hypokalemia, psychosis, susceptibility to infections), myopathy should be considered seriously in the intubated and mechanically ventilated patient.
Subcutaneous epinephrine and terbutaline
Subcutaneous administration of epinephrine or terbutaline should be considered, in patients not responding adequately to continuous nebulised salbutamol, and in those patients unable to cooperate (depression of mental status, apnea, coma) [52] It should also be attempted in intubated patients not responding to inhaled therapy. Epinephrine may also be delivered effectively down the endotracheal tube in extreme situations [13]. Subcutaneously, 0.3–0.4 ml (1:1000) of epinephrine can be administered every 20 min for three doses (Table 3). Terbutaline can be administered subcutaneously (0.25 mg) or as intravenous infusion starting at 0.05–0.10 μg/kg per min (Table 3). When administered subcutaneously, however, terbutaline loses its β-selectivity and offers no advantages over epinephrine [53]. Terbutaline administered subcutaneously should be preferred only in pregnancy because it appears safer [13]. Subcutaneous administration of epinephrine or terbutaline should not be avoided or delayed since it is well tolerated even in patients older than 40–50 years with no history of cardiovascular disease (angina or recent myocardial infarction). Intravenous administration of β-agonists (epinephrine, salbutamol) is also an option in extreme situations and should be considered in the treatment of patients who have not responded to inhaled or subcutaneous treatment, and in whom respiratory arrest is imminent, or in patients not adequately ventilated and severely hyperinflated, despite optimal setting of the ventilator.
Other treatments
Antibiotics are not recommended for the treatment of asthma exacerbations and should be reserved for those with evidence of infection (e.g. pneumonia, sinusitis) [1]. Aggressive hydration is not recommended for adults or older children but may be indicated for infants and young children [1]. Chest physical therapy, mucolytics, and sedation are not recommended [1].
Mechanical ventilation
Careful and repeat assessment of patients with severe exacerbations is mandatory [1]. Patients who deteriorate despite aggressive treatment should be intubated. The exact time to intubate is based mainly on clinical judgment, but it should not be delayed once it is deemed necessary.
Current guidelines recommend four actions regarding intubation [1]. First, patients presenting with apnea or coma should be intubated immediately. Patients who present persistent or increasing hypercapnia, exhaustion, depression of the mental status, hemodynamic instability, and refractory hypoxemia are strong candidates for ventilatory support. Second, consultation with or collaborative management by physicians expert in ventilator management is appropriate because mechanical ventilation of patients with severe refractory asthma is complicated and risky. Third, because intubation is difficult in asthma patients, it is best done semi-electively, before respiratory arrest. Finally, intubation should be performed in a controlled setting by a physician with extensive experience in intubation and airway management.
Once the decision to intubate has been made, the goal is to take rapid and complete control of the patient's cardiopulmonary status. The oral route for intubation appears to offer advantages over the nasal route. It allows a larger endotracheal tube that offers less resistance and greater airway clearance possibilities. The nasal route may be preferred in the conscious, breathless, obese patient who may be difficult to ventilate with a bag-valve mask [13], but this requires tubing with a smaller diameter which may be impossible to use in patients with nasal poliposis.
Sedation during ventilation
Effective sedation is necessary to prepare for intubation and to allow synchronism between the patient and the ventilator [13,29]. In addition, sedation improves patient comfort, decreases oxygen consumption and dioxide production, decreases the risk of barotrauma, and facilitates procedures. There appears to be no standard sedation protocol for the asthmatic patient (Table 4). One purposed approach is the intravenous administration of midazolam, 1 mg initially, followed by 1 mg every 2–3 min until the patient allows positioning and inspection of the airway [13].
Table 4.
Sedatives used in status asthmaticus
| Agents | Dose | Side effects |
| Peri-intubation period | ||
| Midazolam | 1 mg (intravenous) slowly, every 2–3 min until the patient allows positioning and airways inspection | Hypotension, respiratory depression |
| Ketamine | 1–2 mg/kg (intravenous) at a rate of 0.5 mg/kg/min | Sympaticomimetics effects, delirium |
| Propofol | 60–80 mg/min initial intravenous infusion up to 2.0 mg/kg, followed by an infusion of 5–10 mg/kg/hour as needed | Respiratory depression |
| Mechanical ventilation | ||
| Midazolam | 1–10 mg/hour continuous intravenous infusion | |
| Morphine sulfate | 1–5 mg/hour intravenous continuous infusion | Nausea, vomiting, ileus |
| Ketamine | 0.1–0.5 mg/min (intravenous) | |
| Propofol | 1–4.5 mg/kg/hour (intravenous) | Seizures, hyperlipidemia |
Ketamine is an intravenous general anesthetic with sedative, analgesic, anesthetic, and bronchodilating properties that appears useful in the emergency intubation for asthma [54,55,56]. During intubation the intravenous administration of 1–2 mg ketamine/kg at a rate of 0.5 mg/kg/min results in 10–15 min of general anesthesia without significant respiratory depression. Bronchodilation appears within minutes after intravenous administration and lasts 20–30 min after cessation. Because of its sympaticomimetics effects, ketamine is contraindicated in hypertension, cardiovascular disease, high intracranial pressure, and preeclampsia. Additional side effects of ketamine include lowering of the seizure threshold, altered mood, delirium, laryngospasm, and aspiration. Furthermore, since ketamine is metabolized by the liver to norketamine, which also has anesthetic properties and a half-life of about 120 minutes, drug accumulation may occur and lead to prolonged side effects. Paralysis with the short-acting neuro-muscular blocker, succinylcholine, may offer some additional advantages [57].
Propofol is an excellent sedating agent since it has a rapid onset and a rapid resolution of its action [58]. In addition it has bronchodilating properties and since patients can be titrated to anesthetic-depth sedation, it may avoid the need for paralytic agents. Propofol is administered intravenously during the peri-intubation period at a dose of 60–80 mg/min initial infusion, up to 2 mg/kg, followed by an infusion of 5–10 mg/kg/hour as needed, and for sedation for protracted mechanical ventilation 1–4.5 mg/kg/hour [13]. Prolonged propofol administration may be associated with generalized seizures, increase carbon dioxide production, and hypertriglyceridemia [59,60].
Opioids (e.g. morphine sulfate) are not usually recommended for sedation in asthmatics because of their potential to induce hypotension through a combination of direct vasodilation, histamine release, and vagally-mediated bradycardia. Opioids also induce nausea and vomiting, decrease gut motility, and depress ventilatory drive.
The use of neuromuscular-blocking agents (e.g. vecuronium, atracurium, cis-atracurium, pancuronium) lessens the patient–ventilator asynchronism (thus permitting more effective ventilation), lowers the risk for barotrauma, reduces oxygen consumption and dioxide production, and reduces lactate accumulation. The use of paralytics, however, presents a number of disadvantages such as myopathy, excessive airways secretions, histamine release (atracurium), and tachycardia and hypotension (pancuronium). The concomitant use of corticosteroids may increase the risk for postparalytic myopathy [61]. Paralytic agents, when administered, may be given intermittently by bolus or continuous intravenous infusion. If a continuous infusion is used, either a nerve stimulator should be used or the drug should be withheld every four to six hours to avoid drug accumulation and prolonged paralysis. Currently the use of paralytics is usually recommended only in those patients who cannot adequately be controlled with sedation alone.
Effects of intubation
Soon after the intubation of the severe asthmatic patient and the application of positive pressure ventilation, systemic hypotension commonly appears. The determinant factors of systemic hypotension are sedation, hypovolemia, and primarily lung hyperinflation. Dynamic hyperinflation, as previously discussed, occurs when the highly increased airway expiratory resistance prolongs expiratory flow in such a way that the next breath interrupts exhalation of the inspired tidal volume, leading to end-expiratory gas trapping. The mechanisms of intrinsic positive end-expiratory pressure (PEEPI) in acute, severe asthma are as follows:
1. Deceleration of the expiratory flow
High resistance to airflow
Shortened expiratory time
Increased post-inspiratory activity of the inspiratory muscles.
2. Increased expiratory muscle activity.
3. High ventilatory demands.
Additional factors in its pathogenesis are insufficient time during expiration to equilibrate alveolar pressure with atmospheric pressure, persistent inspiratory muscle activity during expiration, and an increased expiratory muscle activity [62,63].
Dynamic hyperinflation is directly proportional to VE and to the degree of airflow obstruction. In the severely obstructed patient, dynamic hyperinflation may further increase in the immediate post intubation period, as a result of the mechanical ventilation, even after the delivering of normal or reduced VE. High levels of dynamic hyperinflation may cause hemodynamic compromise in a somewhat similar way to that caused by the tension pneumothorax. The large intrathoracic pressures that develop due to dynamic hyperinflation increase the right atrial pressure, leading to a decrease in venous return to the right heart. An additional mechanism of decrease in venous return may be related to the positive intrathoracic pressures throughout the respiratory cycle during mechanical ventilation. Sedation, eventually muscle relaxation, and hypovolemia (due to increased water loss or decreased water uptake) reduce the mean systemic blood pressure and cause a further decrease in venous return to the heart. The end result may be sudden cardiovascular collapse, with systemic hypotension and tachycardia. Similar cardiovascular effects also may be observed in patients with tension pneumothorax. In such cases a trial of hypoventilation (delivering of 2–3 breaths/min of 100% oxygen for few minutes) may become necessary to exclude this eventuality. With such setting of the ventilator, in the absence of pneumothorax, the mean intrathoracic pressure will fall, systemic blood pressure will rise, pulse pressure will increase, and pulse rate will fall [13].
Ventilation control
Controlled modes of ventilation are preferred in the immediate post intubation period for different reasons. Patients in status asthmaticus not only have an excessive work of breathing but in addition most of them are intubated and mechanically ventilated when ventilatory muscles are fatigued. Previous studies have shown that at least 24 hours are needed for complete recovery of fatigue. It appears reasonable, therefore, to rest the muscles for some time in the controlled mode of ventilation before switching the ventilator to the assist mode.
Two different modes of controlled setting of the ventilator are widely used. One mode is pressure-controlled ventilation, where the airway pressure can be maintained at a predetermined level independently of any eventual changes of the mechanical properties of the respiratory system. The other method is volume-controlled ventilation, where the ventilator delivers a predetermined tidal volume and the airways pressure becomes the dependent variable. Pressure-controlled ventilation seems more appropriate to maintain airway pressure, especially in status asthmaticus in which airways resistance varies rapidly.
Correction of the hypoxemia is one of the first priorities in setting the ventilator [64]. In non-complicated status asthmaticus, low V/Q ratio is the predominant mechanism and true shunt does not contribute significantly to the hypoxemia. Correction of the hypoxemia is therefore easily obtained by the administration of relatively low concentrations of supplemental oxygen. In the majority of patients, the administration of a fraction of inspired oxygen at the level of 30–50% is sufficient to raise PaO2 above 60 mmHg. Failure of this level of fraction of inspired oxygento increase PaO2 above 60 mmHg indicates some kind of complication (e.g. mucoid impaction atelectasis, pneumonia, or pneumothorax). Complete correction of the respiratory acidosis is not an urgent priority and, since it requires normalization of the PaCO2, which may cause significant deterioration of dynamic hyperinflation, most authors prefer a carefully used buffered therapy for the correction of patient's pH.
The appropriate setting of the ventilator in mechanically ventilated patients is of paramount importance to manage, and to avoid further significant increase of, lung hyperinflation. Several studies have shown that for patients in status asthmaticus, a large part of the morbidity and mortality are related to the mechanical ventilation itself rather to the disease process [64]. In patients on controlled modes, there are three strategies that can decrease dynamic hyperinflation: decrease of VE; increase of expiratory time; and decrease of resistance. Controlled hypoventilation (permissive hypercapnia) is the recommended ventilator strategy to reduce the degree of lung hyperinflation and provide adequate oxygenation and ventilation while minimizing systemic hypotension and barotrauma. [1,65,66,67]. Hypoventilation can be obtained by decreasing either the tidal volume or the respiratory frequency, or both. Hypercapnia is generally well tolerated as long as PaCO2 does not exceed 90 mmHg and acute variations in PaCO2 are avoided. Low values of arterial pH are well tolerated, and slow infusions of sodium bicarbonate appear to be safe in patients with acidosis.
In the immediate post intubation period, and as a result of the mechanical ventilation, especially when patients are ventilated to eucapnia, dynamic hyperinflation may further increase. In order to avoid dangerous levels of dynamic hyperinflation, the ventilator should be set to allow sufficient exhalation time (increasing the expiratory time) while continuing bronchodilator and corticosteroid treatment (decreasing resistance to expiratory flows). The increase in expiratory time can be achieved by increasing inspiratory flows at the expense of increasing peak dynamic pressures, and by the elimination of end-inspiratory pause. The strategy of increasing expiratory time, although less powerful than controlled hypoventilation, decreases dynamic hyperinflation considerably, whereas it improves cardiovascular function and gas exchange [64]. Decreasing resistance to expiratory flows includes pharmacologic treatment to overcome asthma and an effort to decrease the external resistance related to ventilator tubing.
Several studies have shown that setting the ventilator with a level of VE of 8–10 L/min (achieved by a tidal volume of 8–10 ml/kg and respiratory rate of 11–14 breaths/min) combined with an inspiratory flow rate of 80–100 L/min, may be appropriate to avoid dangerous levels of dynamic hyperinflation (Table 5).
Table 5.
Initial ventilator settings in status asthmaticus
| Setting | Recommendation |
| Mode | Pressure-controlled ventilation |
| Respiratory rate | 10–15 breaths/min |
| Tidal volume | 6–10 ml/kg |
| Minute ventilation | 8–10 L/min |
| PEEP | 0 cmH2O |
| Inspiratory/Expiratory ratio | ≥ 1:3 |
| Inspiratory flow | ≥ 100 L/min |
| FIO2 | Maintain SaO2 >90% |
| Pplat | <35 cm H2O |
| VEI | <1.4 L |
FIO2, fraction of inspired oxygen; PEEP, positive end-expiratory pressure; Pplat, end-inspiratory plateau pressure; SaO2, oxygen saturation; VEI, end-inspired volume above apneic functional residual capacity.
There are several techniques for the estimation of the level of dynamic hyperinflation. One way is to measure the end-inspired volume above apneic FRC (VEI) [68]. Apneic FRC is determined by measuring the total exhaled volume of gas during 20–40 seconds of apnea in a paralyzed patient. VEI is the sum of the tidal volume and the volume at end exhalation above FRC (Fig. 4). Values of VEI above a threshold value of 20 ml/kg (1.4 L in an average adult) have been shown to predict complications of hypotension and barotrauma [68]. The need for paralysis, however, limits the use of VEI.
Figure 4.
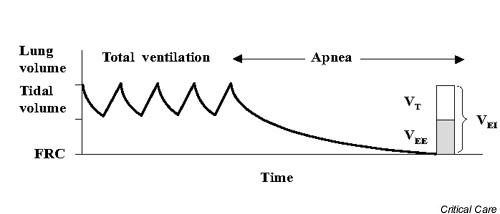
Measurement of the end-inspired volume (VEI) above apneic functional residual capacity (FRC) in order to estimate lung hyperinflation. The total exhaled volume during a period of apnea (20–60 seconds) is measured. VEI is the volume of gas at the end of inspiration above FRC and is the sum of the tidal volume and the volume at end exhalation above FRC (VEE). Published with permission from American Review of Respiratory Disease [68].
In the mechanically ventilated patient other estimates of the degree of dynamic hyperinflation are the determination of the end-inspiratory plateau pressure (Pplat) and the measure of PEEPI [69]. To obtain both measurements patient relaxation, but not paralysis, is necessary. Pplat is an estimate of average end-inspiratory alveolar pressures and is easily determined by stopping flow at end-inspiration (Fig. 5). PEEPI is the lowest average alveolar pressure achieved during the respiratory cycle and is obtained by an end-expiratory hold maneuver (Fig. 6). When evaluating these methods, The American College of Chest Physicians consensus conference on mechanical ventilation concluded that Pplat is the best predictor of hyperinflation in ventilated asthmatic patients and recommended that Pplat must be kept lower than 35 cmH2O [70].
Figure 5.
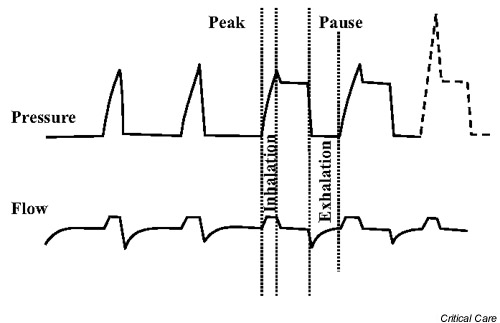
Measurement of end-inspiratory plateau pressure, an estimate of average end-inspiratory alveolar pressures. The peak-to-plateau gradient is easily determined by stopping flow at end-inspiration and can be used as a measure of the severity of inspiratory airway resistance. The plateau pressure is a reflection of the respiratory system pressure change resulting from the delivery of the tidal volume, added to any level of intrinsic positive end-expiratory pressure. The plateau pressure is a useful marker of lung hyperinflation and should be maintained at less than 30 cmH2O. The dotted line indicates a high peak-to-plateau gradient observed in status asthmaticus. Published with permission from Principles of Critical Care [69].
Figure 6.
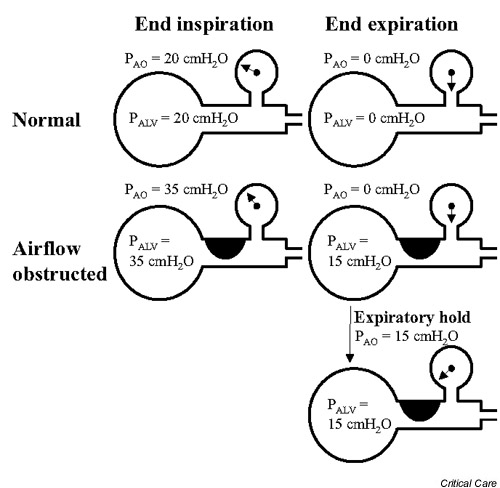
Measurement of intrinsic positive end-expiratory pressure. Intrinsic positive end-expiratory pressure is the lowest average alveolar pressure achieved during the respiratory cycle and is obtained by an end-expiratory hold manoeuvre. In the non-obstructed patient, alveolar pressure (PALV) equals pressure at the airway opening (PAO) both at end inspiration and end expiration. In the severely obstructed patient, PALV may increase because of air trapping, and at end expiration PALV does not equal PAO. If an expiratory hold manoeuvre is performed, PAO will rise, reflecting the degree of lung hyperinflation. Published with permission from Principles of Critical Care [69].
After successful treatment and when the patient's conditions improve, the ventilator should be switched to assisted modes (pressure or volume), and the process of weaning should begin. In order to improve the patient/ventilator synchronism, two issues should be taken into account, the response of ventilator to patient effort, and the response of patient effort to ventilator-delivered breath.
Noninvasive mechanical ventilation
The indications for initiating noninvasive ventilation in acute, severe asthma are not clearly defined, and its use is questioned [62]. Noninvasive mechanical ventilation includes various techniques of increasing alveolar ventilation without an endotracheal airway. The clinical application of noninvasive ventilation includes the use of continuous positive airways pressure (CPAP) alone, referred as 'mask CPAP', and the use of intermittent positive pressure ventilation, with or without CPAP, referred as 'noninvasive (intermittent) positive pressure ventilation' [71].
The application of noninvasive ventilation in acute respiratory failure in patients with chronic obstructive pulmonary disease has proved to be effective and safe [72,73]. Noninvasive ventilation mainly works by improving alveolar ventilation, resting fatigued ventilatory muscles, relieving dyspnea, and improving gas exchange, while it avoids the risks and discomfort of an endotracheal intubation [71]. Since the pathophysiology of acute respiratory failure in asthma is, in many ways, similar to that of acute respiratory failure in chronic obstructive pulmonary disease, an effort has been made to investigate the possible application of noninvasive ventilation in acute, severe asthma [71,74]. From these studies it appears that the application of noninvasive ventilation by properly trained and experienced personnel, added to the standard pharmacological therapy, might be helpful in reducing the intubation rate in a selected group of patients in status asthmaticus. Additional studies are necessary, however, to support use of this technique in patients with acute, severe asthma.
Prognosis of patients in status asthmaticus
Status asthmaticus carries a significant mortality, ranging between 1 and 10% [75,76]. Among patients in status asthmaticus admitted to an intensive care unit, between 10 and 30% required mechanical ventilation [66,77,78]. In recent years the mortality rate of patients in status asthmaticus requiring mechanical ventilation has decreased significantly [62]. This decrease may reflect earlier diagnosis, aggressive medical treatment, and improvements in mechanical ventilation [62]. Death from asthma in mechanically ventilated patients appears to be further decreased after the application of the 'permissive hypercapnia technique'.
Prevention of relapse
Prevention of subsequent asthma attacks is imperative. Patients should be discharged only after they have been provided with the necessary medications (and educated how to use them), instructions in self-assessment (PEF, symptoms score), a follow-up appointment, and instructions for an action plan for managing recurrence of airflow obstruction [1]. Furthermore, an adrenaline kit should be given to patients with a history of sudden asphyxic asthma.
Competing interests
None declared
Abbreviations
CPAP = continuous positive airways pressure; FEV1 = forced expired volume in 1 sec; FRC = functional residual capacity; FVC = forced vital capacity; MEF75, MEF50, and MEF25 = maximal expiratory flows at the 75%, 50%, and 25% of vital capacity; MEF25–75 = maximal expiratory flow between 25% and 75% of the FVC; PaCO2 = arterial carbon dioxide; PaO2 = arterial oxygen; PEEPI = intrinsic positive end-expiratory pressure; PEF = peak expiratory flow; Pplat = end-inspiratory plateau pressure; Q = perfusion; V = ventilation; VE = minute ventilation; VEI = end-inspired volume above apneic FRC.
Acknowledgments
Acknowledgements
The authors are supported by the Thorax Foundation, Athens, Greece.
References
- National Heart, Lung and Blood Institute Guidelines for the Diagnosis and Management of Asthma, Expert Panel Report 2 Bethesda: National Institutes of Health publication number 97–4051. 1997.
- McFadden ER, Jr, Warren EL. Observations on asthma mortality. Ann Intern Med. 1997;127:142–147. doi: 10.7326/0003-4819-127-2-199707150-00009. [DOI] [PubMed] [Google Scholar]
- Benatar SR. Fatal asthma. N Engl J Med. 1986;314:423–429. doi: 10.1056/NEJM198602133140706. [DOI] [PubMed] [Google Scholar]
- McFadden ER., Jr Fatal and near-fatal asthma. N Engl J Med. 1991;324:409–411. doi: 10.1056/NEJM199102073240609. [DOI] [PubMed] [Google Scholar]
- Moore BB, Weiss KB, Sullivan SA. Epidemiology and socioeconomic impact of severe asthma. In Severe Asthma, Pathogenesis and Clinical Management Edited by Szefler SJ, Leung DYM New York: Marcel Dekker Inc; 1996. pp. 1–34. [Lung Biology in Health and Disease, vol 86.]
- Busse WW, Banks-Schlegel S, Wenzel SE. Pathophysiology of severe asthma. J Allergy Clin Immunol. 2000;106:1033–1042. doi: 10.1067/mai.2000.111307. [DOI] [PubMed] [Google Scholar]
- Barnes PJ, Woolcock AJ. Difficult asthma. Eur Respir J. 1998;12:1208–1218. doi: 10.1183/09031936.98.12051209. [DOI] [PubMed] [Google Scholar]
- Ayres JG, Miles JF, Barnes PJ. Brittle asthma. Thorax. 1998;58:315–321. doi: 10.1136/thx.53.4.315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Woolcock AJ. Steroid resistant asthma: what is the clinical definition? Eur Respir J. 1993;6:743–747. [PubMed] [Google Scholar]
- Kamada AK, Leung DYM, Ikle D, Gelfand EW, Szefler SJ. High-dose systemic glucocorticoid therapy in the treatment of asthma: a case of resistance and patterns of response. J Allergy Clin Immunol. 1992;90:685–687. doi: 10.1016/0091-6749(92)90144-q. [DOI] [PubMed] [Google Scholar]
- European Respiratory Society Task Force on Difficult/Therapy-Resistant Asthma Difficult/therapy-resistant asthma. The need for an integrated approach to define clinical phenotypes, evaluate risk factors, understand pathophysiology and find novel therapies. Eur Respir J. 1999;13:1198–1208. doi: 10.1034/j.1399-3003.1999.13e43.x. [DOI] [PubMed] [Google Scholar]
- McFadden ER., Jr Clinical and physiological correlates in asthma. J Allergy Clin Immunol. 1986;77:1–5. [PubMed] [Google Scholar]
- Corbridge TC, Hall JB. The assessment and management of adults with status asthmaticus. Am J Respir Crit Care Med. 1995;151:1296–1316. doi: 10.1164/ajrccm.151.5.7735578. [DOI] [PubMed] [Google Scholar]
- Fanta CH. Acute, severe asthma. In Asthma Edited by Barnes PJ, Grunstein MM, Leff AR, Woolcock AJ: Philadelphia: Lippincott-Raven; 1997. pp. 1931–1943.
- Kolbe J, Fergusson W, Garrett J. Rapid onset asthma: a severe but uncommon manifestation. Thorax. 1998;53:241–247. doi: 10.1136/thx.53.4.241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- British Thoracic Association Death due to asthma. Br Med J. 1982;285:1251–1255. [PMC free article] [PubMed] [Google Scholar]
- Molfino NA, Nannini LJ, Martelli AN, Slutsky AS. Respiratory arrest in near-fatal asthma. N Engl J Med. 1991;324:285–288. doi: 10.1056/NEJM199101313240502. [DOI] [PubMed] [Google Scholar]
- Strunk RC. Death due to asthma [editorial]. Am J Respir Crit Care Med. 1993;148:550–552. [Google Scholar]
- Roe PF. Sudden death in asthma. Brit J Dis Chest. 1965;59:158–163. doi: 10.1016/s0007-0971(65)80006-7. [DOI] [PubMed] [Google Scholar]
- Wasserfallen J-B, Schaller M-D, Feihl F, Perret CH. Sudden asphyxic asthma: a distinct entity? Am Rev Respir Dis. 1990;142:108–111. doi: 10.1164/ajrccm/142.1.108. [DOI] [PubMed] [Google Scholar]
- Sur S, Crotty TB, Kephart GM, Hyma BA, Colby TV, Reed CE, Hunt LW, Gleich GJ. Sudden-onset fatal asthma. A distinct entity with few eosinophils and relatively more neutrophils in the airway submucosa? Am J Respir Crit Care Med. 1993;148:713–719. doi: 10.1164/ajrccm/148.3.713. [DOI] [PubMed] [Google Scholar]
- Reid LM. The presence or absence of bronchial mucus in fatal asthma. J Allergy Clin Immunol. 1987;80 (suppl):415–419. doi: 10.1016/0091-6749(87)90064-9. [DOI] [PubMed] [Google Scholar]
- Saetta M, Di Stefano A, Rosina C, Thiene G, Fabbri LM. Quantitative structural analysis of peripheral airways and arteries in sudden fatal asthma. Am Rev Respir Dis. 1991;143:138–143. doi: 10.1164/ajrccm/143.1.138. [DOI] [PubMed] [Google Scholar]
- Rodriguez-Roisin R. Acute severe asthma: pathophysiology and pathobiology of gas exchange abnormalities. Eur Respir J. 1997;10:1359–1371. doi: 10.1183/09031936.97.10061359. [DOI] [PubMed] [Google Scholar]
- Rodriguez-Roisin R, Ballaster E, Roca J, Torres A, Wagner PD. Mechanism of hypoxemia in patients with status asthmaticus requiring mechanical ventilation. Am Rev Respir Dis. 1989;139:732–739. doi: 10.1164/ajrccm/139.3.732. [DOI] [PubMed] [Google Scholar]
- Roussos CH, Macklem PT. The respiratory muscles. N Engl J Med. 1982;307:786–797. doi: 10.1056/NEJM198209233071304. [DOI] [PubMed] [Google Scholar]
- Roussos CH, Macklem PT. Diaphragmatic fatigue in man. J Appl Physiol: Respirat Environ Exercise Physiol. 1977;43(2):189–197. doi: 10.1152/jappl.1977.43.2.189. [DOI] [PubMed] [Google Scholar]
- Manthous CA. Management of severe exacerbations of asthma. Am J Med. 1995;99:298–308. doi: 10.1016/s0002-9343(99)80163-6. [DOI] [PubMed] [Google Scholar]
- Levy BD, Kitch B, Fanta CH. Medical and ventilatory management of status asthmaticus. Intensive Care Med. 1998;24:105–117. doi: 10.1007/s001340050530. [DOI] [PubMed] [Google Scholar]
- Grossman J. The occurrence of arrhythmias in hospitalized asthma patients. J Allergy Clin Immunol. 1976;57:310–317. doi: 10.1016/0091-6749(76)90087-7. [DOI] [PubMed] [Google Scholar]
- Lemarchand P, Labrune S, Herer B, Huchon GJ. Cardiorespiratory arrest following peak expiratory flow measurement during attack of asthma. Chest. 1991;100:1168–1169. doi: 10.1378/chest.100.4.1168. [DOI] [PubMed] [Google Scholar]
- Rodrigo G, Rodrigo C. Assessment of the patient with acute asthma in the emergency department: a factor analytic study. Chest. 1993;104:1325–1328. doi: 10.1378/chest.104.5.1325. [DOI] [PubMed] [Google Scholar]
- White CS, Cole RP, Lubetsky HW, Austin JHM. Acute asthma: admission chest radiography in hospitalized adult patients. Chest. 1991;100:14–16. doi: 10.1378/chest.100.1.14. [DOI] [PubMed] [Google Scholar]
- Mc Fadden ER, Elsanadi N, Dixon L, Takacs M, Deal EC, Boyd KK, Idemoto BK, Bruseman LA, Panuskal , Hammons T, Smith B, Carcuso F, McFadden CB, Shoemaker L, Warrey EL, Hefal R, Strauss L, Gilbert IA. Protocol therapy for acute asthma: therapeutics benefits and cost savings. Am J Med. 1995;99:651–661. doi: 10.1016/s0002-9343(99)80253-8. [DOI] [PubMed] [Google Scholar]
- Kelsen SG, Kelsen DP, Fleegler BF, Jones RC, Rodman T. Emergency room assessment and treatment of patients with acute asthma. Am J Med. 1978;64:622–628. doi: 10.1016/0002-9343(78)90582-x. [DOI] [PubMed] [Google Scholar]
- Petty TL. Treat status asthmaticus three days before it occurs. J Intensive Care Med. 1989;4:135–136. [Google Scholar]
- Lin RY, Sauter D, Newman T, Sirteaf J, Walters J, Tavakoi M. Continuous versus intermittent albuterol nebulization in the treatment of acute asthma. Ann Emerg Med. 1993;22:1847–1853. doi: 10.1016/s0196-0644(05)80412-3. [DOI] [PubMed] [Google Scholar]
- Rudnitsky GS, Eberlein RS, Schoffstall JM, Mazur JE, Spivey WH. Comparison of intermittent and continuously nebulized albuterol for treatment of asthma in an urban emergency department. Ann Emerg Med. 1993;22:1842–1846. doi: 10.1016/s0196-0644(05)80411-1. [DOI] [PubMed] [Google Scholar]
- Papo MC, Frank J, Thompson AE. A prospective, randomized study of continuous versus intermittent nebulized albuterol for severe status asthmaticus in children. Crit Care Med. 1993;21:1479–1486. doi: 10.1097/00003246-199310000-00015. [DOI] [PubMed] [Google Scholar]
- Karpel JP, Schacter EN, Fanta C, Levey D, Spiro P, Aldrich R, Menjoge SS, Witek TJ. A comparison of ipratropium and albuterol vs. albuterol alone for the treatment of acute asthma. Chest. 1996;110:611–616. doi: 10.1378/chest.110.3.611. [DOI] [PubMed] [Google Scholar]
- O'Driscoll BR, Kaira S, Wilson M, Pickering CA, Carroll KB, Woodcock AA. Nebulised salbutamol with and without ipratropium bromide in acute airflow obstruction. Lancet. 1993;341:324–327. [Google Scholar]
- Rodrigo C, Rodrigo G. Treatment of acute asthma. Lack of therapeutic benefit and increase of toxicity from aminophylline given in addition to high doses of salbutamol delivered by metered-dose inhaler with a spacer. Chest. 1994;106:1071–1076. doi: 10.1378/chest.106.4.1071. [DOI] [PubMed] [Google Scholar]
- Aubier M, De Troyer A, Sampson M, Macklem P, Roussos C. Aminophylline improves diaphragmatic contractility. N Engl J Med. 1981;305:249–252. doi: 10.1056/NEJM198107303050503. [DOI] [PubMed] [Google Scholar]
- Chapman KR, Verbeek PR, White JG, Rebuck AS. Effect of a short course of prednisone in the prevention of early relapse after the emergency room treatment of acute asthma. N Engl J Med. 1991;324:788–794. doi: 10.1056/NEJM199103213241202. [DOI] [PubMed] [Google Scholar]
- Rowe BH, Keller JL, Oxman AD. Effectiveness of steroid therapy in acute exacerbations of asthma: a meta analysis. Am J Emerg Med. 1992;10:301–310. doi: 10.1016/0735-6757(92)90007-k. [DOI] [PubMed] [Google Scholar]
- Rodrigo G, Rodrigo C. Inhaled flunisolide for acute severe asthma. Am J Respir Crit Care Med. 1998;157:698–703. doi: 10.1164/ajrccm.157.3.9704022. [DOI] [PubMed] [Google Scholar]
- Gibson PG, Saltos N, Fakes K. Acute anti-inflammatory effects of inhaled budesonide in asthma. Am J Respir Crit Care Med. 2001;163:32–36. doi: 10.1164/ajrccm.163.1.9807061. [DOI] [PubMed] [Google Scholar]
- McFadden ER., Jr Inhaled glucocorticoids and acute asthma. Therapeutic breakthrough or nonspecific effect? Am J Respir Crit Care Med. 1998;157:677–678. doi: 10.1164/ajrccm.157.3.ed01-98. [DOI] [PubMed] [Google Scholar]
- Blais L, Ernst P, Boivin JF, Suissa S. Inhaled corticosteroids and the prevention of readmission to hospital for asthma. Am J Respir Crit Care Med. 1998;158:126–132. doi: 10.1164/ajrccm.158.1.9707107. [DOI] [PubMed] [Google Scholar]
- Sin DD, Tu JV. Inhaled corticosteroid therapy reduces the risk of rehospitalization and all-cause mortality in elderly asthmatics. Eur Respir J. 2001;17:380–385. doi: 10.1183/09031936.01.17303800. [DOI] [PubMed] [Google Scholar]
- McFadden ER., Jr Dosages of corticosteroids in asthma. Am Rev Respir Dis. 1993;147:1306–1310. doi: 10.1164/ajrccm/147.5.1306. [DOI] [PubMed] [Google Scholar]
- Appel D, Karpel JP, Sherman M. Epinephrine improves expiratory airflow rates in patients with asthma who do not respond to inhaled metaproterenol sulfate. J Allergy Clin Immunol. 1989;84:90–98. doi: 10.1016/0091-6749(89)90182-6. [DOI] [PubMed] [Google Scholar]
- Amory DW, Burnham SC, Cheney FW. Comparison of the cardiopulmonary effects of subcutaneously administered epinephrine and terbutaline in patients with reversible airway obstruction. Chest. 67:279–286. doi: 10.1378/chest.67.3.279. [DOI] [PubMed] [Google Scholar]
- Corseen G, Guitierez J, Reves JG, Huber FC. Ketamine in the anesthetic management of asthmatic patients. Anesth Analg. 1972;8:87–92. [PubMed] [Google Scholar]
- Huber FC, Guitierez J, Corseen G. Ketamine: its effects on airways resistance in man. South Med J. 1972;65:1176–1180. doi: 10.1097/00007611-197210000-00003. [DOI] [PubMed] [Google Scholar]
- Sarma V. Use of ketamine in acute severe asthma. Acta Anaesthesiol Scand. 1992;36:106–107. doi: 10.1111/j.1399-6576.1992.tb03432.x. [DOI] [PubMed] [Google Scholar]
- L'Hommedieu CS, Arens JJ. The use of ketamine for the emergency intubation of patients with status asthmaticus. Ann Emerg Med. 1987;16:568–571. doi: 10.1016/s0196-0644(87)80688-1. [DOI] [PubMed] [Google Scholar]
- Clarckson K, Power CK, O'Connell F, Pathmakanthan S, Burke CM. A comparative evaluation of propofol and midazolam as sedative agents in fiberoptic bronchoscopy. Chest. 1993;104:1029–1031. doi: 10.1378/chest.104.4.1029. [DOI] [PubMed] [Google Scholar]
- Collier C, Kelly K. Propofol and convulsions, the evidence mounts. Anaesth Intensive Care. 1991;19:573–575. doi: 10.1177/0310057X9101900416. [DOI] [PubMed] [Google Scholar]
- Gottardis M, Khunl-Brady KS, Koller W, Sigl G, Hackl JM. Effect of prolonged sedation with propofol on serum triglyceride and cholesterol concentrations. Br J Anaest. 1989;62:393–396. doi: 10.1093/bja/62.4.393. [DOI] [PubMed] [Google Scholar]
- Leatherman JW, Fluegel WL, David WS, Davies SF, Iber C. Muscle weakness in mechanically ventilated patients with severe asthma. Am J Respir Crit Care Med. 1996;153:1686–1690. doi: 10.1164/ajrccm.153.5.8630621. [DOI] [PubMed] [Google Scholar]
- Alex CG, Tobin MJ. Ventilation of asthmatic patients. In Asthma Edited by Barnes PJ, Grunstein MM, Leff AR, Woolcock AJ Philadelphia: Lippincott-Raven; 1997. pp. 1977–2003.
- Zakynthinos SG, Vassilakopoulos T, Zakynthinos E, Roussos CH. Accurate measurement of intrinsic positive end-expiratory pressure: how to detect and correct for expioratory muscle activity. Eur Respir J. 1997;10:522–529. [PubMed] [Google Scholar]
- Georgopoulos D, Kondili E, Prinianakis G. How to set the ventilator in asthma. Monaldi Arch Chest Dis. 2000;55:74–83. [PubMed] [Google Scholar]
- Menitove SM, Goldring RM. Combined ventilator and bicarbonate strategy in the management of status asthmaticus. Am J Med. 1983;74:898–901. doi: 10.1016/0002-9343(83)91082-3. [DOI] [PubMed] [Google Scholar]
- Darioli R, Perret C. Mechanical controlled hypoventilation in status asthmaticus. Am Rev Respir Dis. 1984;129:385–387. doi: 10.1164/arrd.1984.129.3.385. [DOI] [PubMed] [Google Scholar]
- Tuxen DV. Permissive hypercapnic ventilation. Am J Respir Crit Care Med. 1994;150:870–874. doi: 10.1164/ajrccm.150.3.8087364. [DOI] [PubMed] [Google Scholar]
- Tuxen DV. Detrimental effects of positive end-expiratory pressure during controlled mechanical ventilation of patients with severe airflow obstruction. Am Rev Respir Dis. 1989;140:5–9. doi: 10.1164/ajrccm/140.1.5. [DOI] [PubMed] [Google Scholar]
- Corbridge TC, Hall JB. Status asthmaticus. In Principles of Critical Care Edited by Hall JB, Schmidt GA, Wood LD McGraw Hill; 1998. pp. 579–595.
- Slutsky AS. Mechanical ventilation. Chest. 1993;104:1833–1859. doi: 10.1378/chest.104.6.1833. [DOI] [PubMed] [Google Scholar]
- Meduri GU, Cook TR, Turner RE, Cohen M, Leeper KV. Noninvasive positive pressure ventilation in status asthmaticus. Chest. 1996;110:767–774. doi: 10.1378/chest.110.3.767. [DOI] [PubMed] [Google Scholar]
- Bott J, Carroll MP, Conway JH, Keilty SE, Ward EM, Brown AM, Paul EA, Elliott MW, Godfrey RC, Wedzicha JA, Moxham J. Randomized controlled trial of nasal ventilation in acute ventilatory failure due to chronic obstructive airways disease. Lancet. 1993;341:1555–1558. doi: 10.1016/0140-6736(93)90696-e. [DOI] [PubMed] [Google Scholar]
- Brochard L, Mancebo J, Wysocki M, Lofaso F, Conti G, Rauss A, Simoneau G, Benito S, Gasparetto A, Lemaire F, Isabey D, Hare A. Noninvasive ventilation for acute exacerbations of chronic obstructive pulmonary disease. N Engl J Med. 1995;333:817–822. doi: 10.1056/NEJM199509283331301. [DOI] [PubMed] [Google Scholar]
- Fernandez MM, Villagra A, Blanch L, Fernandez R. Non-invasive mechanical ventilation in status asthmaticus. Intensive Care Med. 2001;27:486–492. doi: 10.1007/s001340100853. [DOI] [PubMed] [Google Scholar]
- Scoggin CH, Sahn SA, Petty TL. Status asthmaticus: a nine-year experience. J Am Med Assoc. 1977;238:1158–1162. [PubMed] [Google Scholar]
- Williams MH. Life-threatening asthma. Arch Int Med. 1980;140:1604–1605. [PubMed] [Google Scholar]
- Dworkin G, Kattan M. Mechanical ventilation for status asthmaticus in children. J Pediatr. 1989;114:545–549. doi: 10.1016/s0022-3476(89)80691-2. [DOI] [PubMed] [Google Scholar]
- Braman SS, Kaemmerlen JT. Intensive care of status asthmaticus: a 10-year experience. J Am Med Assoc. 1990;264:366–368. [PubMed] [Google Scholar]


