Abstract
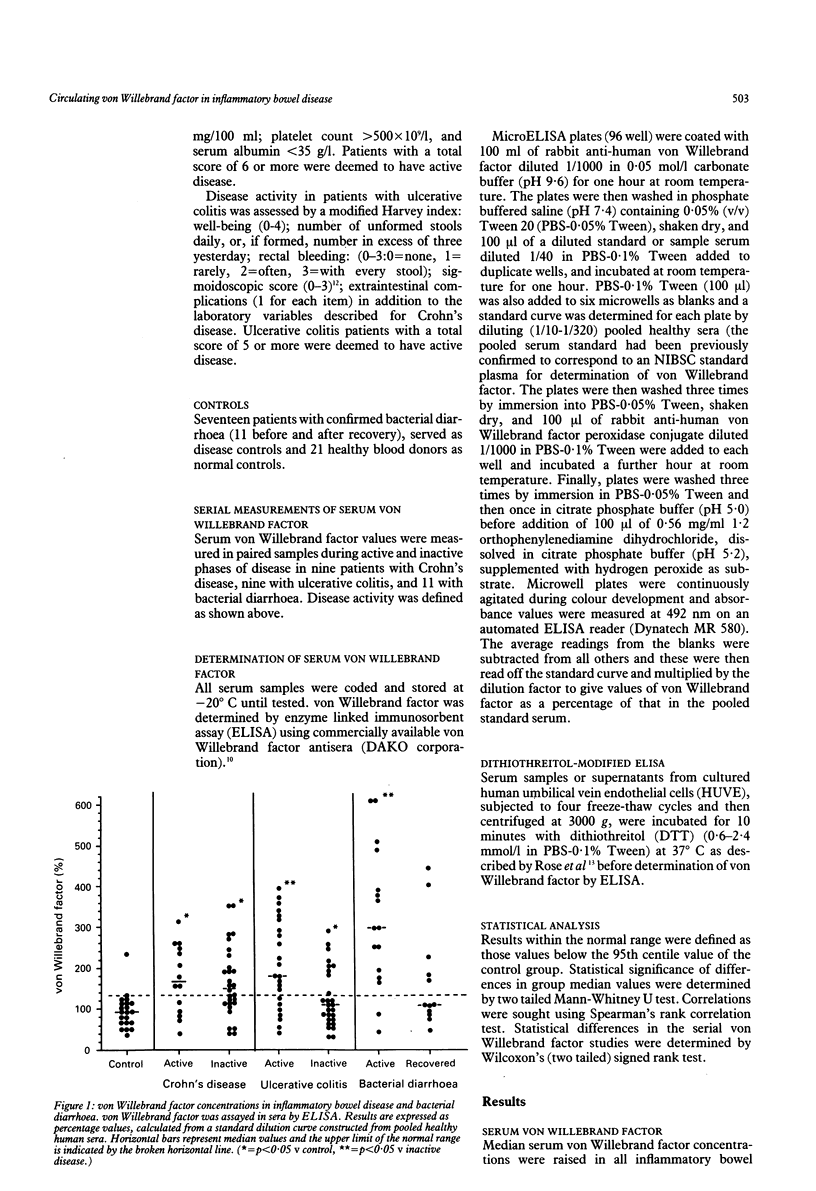
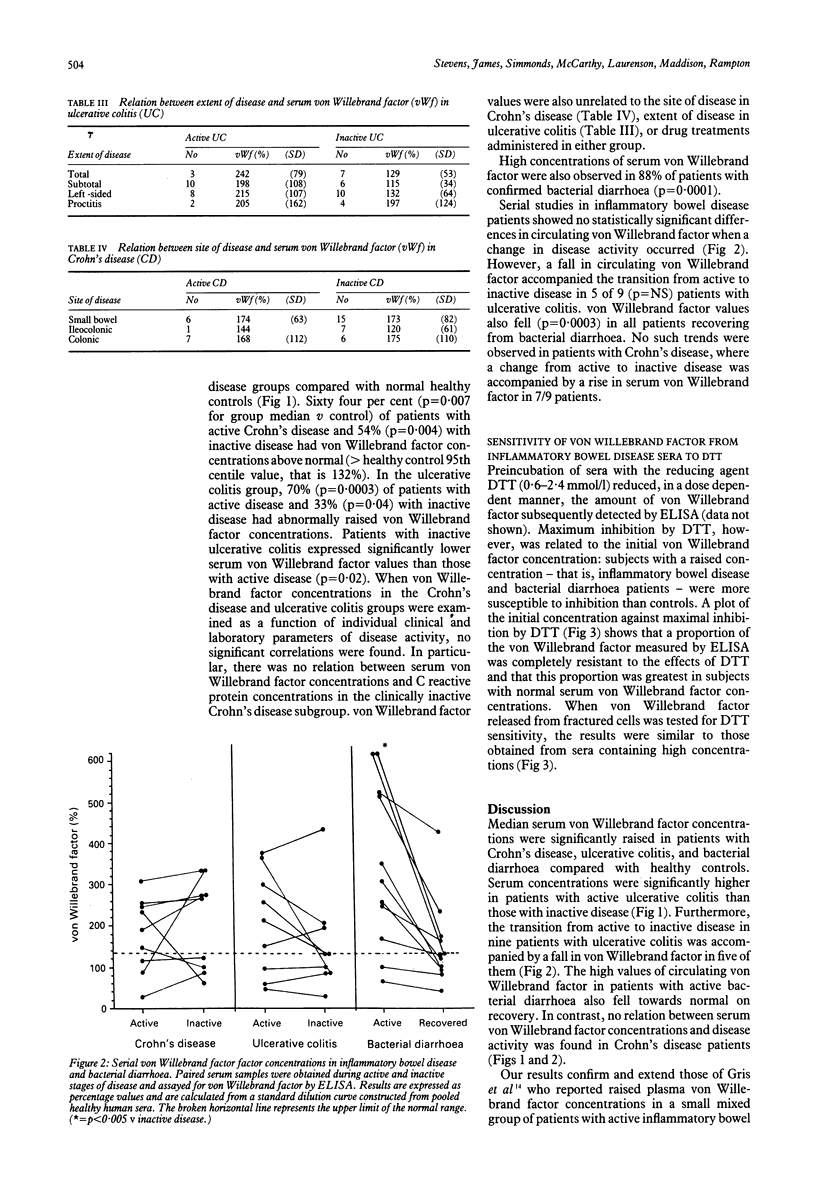
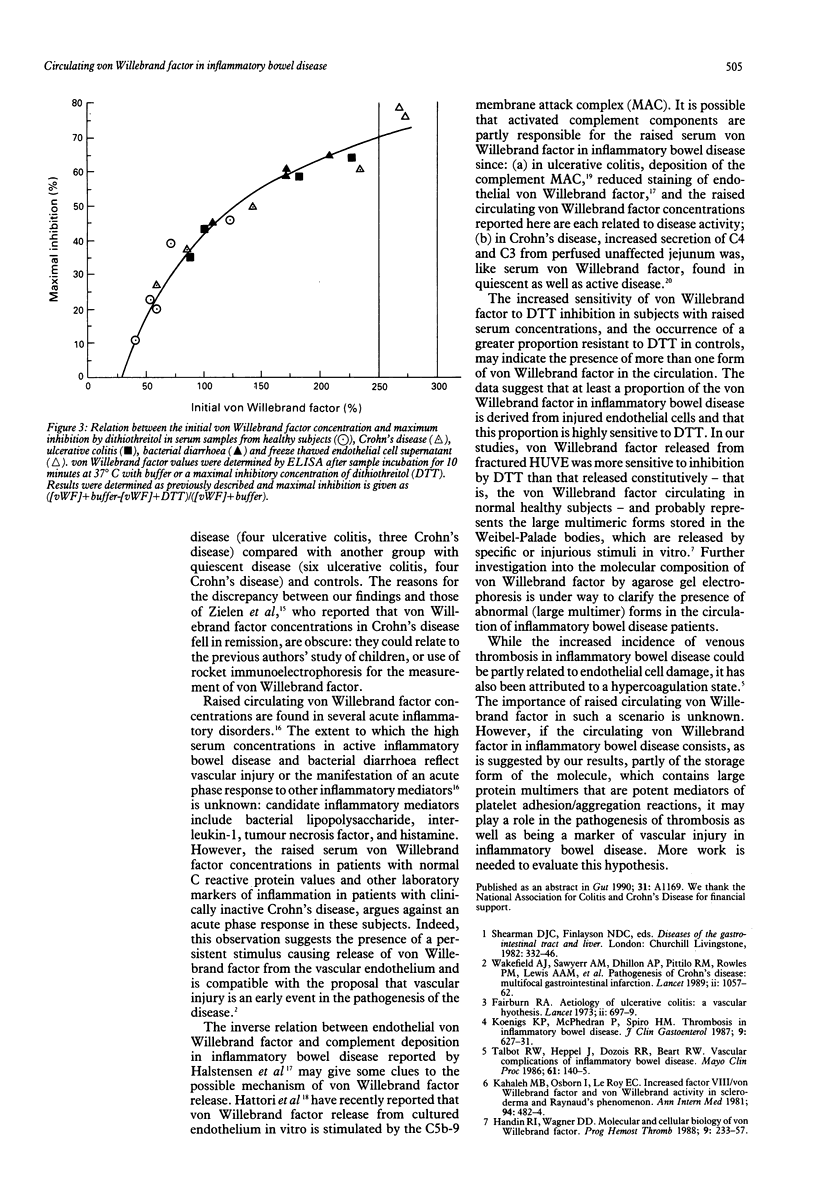
Raised circulating von Willebrand factor is a recognised marker of vascular injury. To evaluate the role of vascular injury in the pathogenesis of inflammatory bowel disease, serum von Willebrand factor in Crohn's disease, ulcerative colitis, confirmed bacterial diarrhoea, and healthy subjects was measured. von Willebrand factor values were raised in 9/14 patients (p = 0.007) with active Crohn's disease, 15/28 (p = 0.0004) with inactive Crohn's disease, 16/23 (p = 0.0003) with active ulcerative colitis, 9/27 (p = 0.04) with inactive ulcerative colitis, and 15/17 (p = 0.0001) patients with bacterial diarrhoea. Serum von Willebrand factor was unrelated to disease activity in Crohn's disease but was significantly raised in active (p = 0.02) compared with inactive ulcerative colitis. In contrast to controls, the detection of von Willebrand factor from inflammatory bowel disease sera and that from fractured endothelial cells was significantly inhibited by the reducing agent, dithiothreitol, suggesting the presence of an additional dithiothreitol sensitive form of the molecule derived from injured endothelial cells in inflammatory bowel disease. That serum von Willebrand factor is raised in quiescent as well as active Crohn's disease is compatible with the proposal that vascular injury is a fundamental abnormality in this disorder. The raised von Willebrand factor values in active inflammatory bowel disease and bacterial diarrhoea could be caused by either vascular injury, occurring secondary to bowel inflammation, or to an acute phase response resulting from endothelial cell stimulation by mediators released during the inflammatory process. Raised circulating von Willebrand factor could contribute to the increased risk of thrombosis associated with active inflammatory bowel disease.
Full text
PDF
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Ahrenstedt O., Knutson L., Nilsson B., Nilsson-Ekdahl K., Odlind B., Hällgren R. Enhanced local production of complement components in the small intestines of patients with Crohn's disease. N Engl J Med. 1990 May 10;322(19):1345–1349. doi: 10.1056/NEJM199005103221903. [DOI] [PubMed] [Google Scholar]
- BARON J. H., CONNELL A. M., LENNARD-JONES J. E. VARIATION BETWEEN OBSERVERS IN DESCRIBING MUCOSAL APPEARANCES IN PROCTOCOLITIS. Br Med J. 1964 Jan 11;1(5375):89–92. doi: 10.1136/bmj.1.5375.89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fairburn R. A. On the aetiology of ulcerative colitis. A vascular hypothesis. Lancet. 1973 Mar 31;1(7805):697–699. doi: 10.1016/s0140-6736(73)91482-7. [DOI] [PubMed] [Google Scholar]
- Gris J. C., Schved J. F., Raffanel C., Dubois A., Aguilar-Martinez P., Arnaud A., Sanchez N., Sarlat C., Balmès J. L. Impaired fibrinolytic capacity in patients with inflammatory bowel disease. Thromb Haemost. 1990 Jun 28;63(3):472–475. [PubMed] [Google Scholar]
- Halstensen T. S., Mollnes T. E., Brandtzaeg P. Persistent complement activation in submucosal blood vessels of active inflammatory bowel disease: immunohistochemical evidence. Gastroenterology. 1989 Jul;97(1):10–19. doi: 10.1016/0016-5085(89)91409-1. [DOI] [PubMed] [Google Scholar]
- Halstensen T. S., Mollnes T. E., Fausa O., Brandtzaeg P. Deposits of terminal complement complex (TCC) in muscularis mucosae and submucosal vessels in ulcerative colitis and Crohn's disease of the colon. Gut. 1989 Mar;30(3):361–366. doi: 10.1136/gut.30.3.361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Handin R. I., Wagner D. D. Molecular and cellular biology of von Willebrand factor. Prog Hemost Thromb. 1989;9:233–259. [PubMed] [Google Scholar]
- Harvey R. F., Bradshaw J. M. A simple index of Crohn's-disease activity. Lancet. 1980 Mar 8;1(8167):514–514. doi: 10.1016/s0140-6736(80)92767-1. [DOI] [PubMed] [Google Scholar]
- Hattori R., Hamilton K. K., McEver R. P., Sims P. J. Complement proteins C5b-9 induce secretion of high molecular weight multimers of endothelial von Willebrand factor and translocation of granule membrane protein GMP-140 to the cell surface. J Biol Chem. 1989 May 25;264(15):9053–9060. [PubMed] [Google Scholar]
- James J. P., Stevens T. R., Hall N. D., Maddison P. J., Goulding N. J., Silman A., Holligan S., Black C. Factor VIII related antigen in connective tissue disease patients and relatives. Br J Rheumatol. 1990 Feb;29(1):6–9. doi: 10.1093/rheumatology/29.1.6. [DOI] [PubMed] [Google Scholar]
- Kahaleh M. B., Osborn I., LeRoy E. C. Increased factor VIII/von Willebrand factor antigen and von Willebrand factor activity in scleroderma and in Raynaud's phenomenon. Ann Intern Med. 1981 Apr;94(4 Pt 1):482–484. doi: 10.7326/0003-4819-94-4-482. [DOI] [PubMed] [Google Scholar]
- Koenigs K. P., McPhedran P., Spiro H. M. Thrombosis in inflammatory bowel disease. J Clin Gastroenterol. 1987 Dec;9(6):627–631. [PubMed] [Google Scholar]
- Morisato D. K., Gralnick H. R. Selective binding of the factor VIII/von Willebrand factor protein to human platelets. Blood. 1980 Jan;55(1):9–15. [PubMed] [Google Scholar]
- Novotny M. J., Turrentine M. A., Johnson G. S., Adams H. R. Experimental endotoxemia increases plasma von Willebrand factor antigen concentrations in dogs with and without free-radical scavenger therapy. Circ Shock. 1987;23(3):205–213. [PubMed] [Google Scholar]
- Rose P. E., Struthers G. S., Robertson M., Kavi J., Chant I., Taylor C. M. Factor VIII von Willebrand protein in haemolytic uraemic syndrome and systemic vasculitides. Lancet. 1990 Mar 3;335(8688):500–502. doi: 10.1016/0140-6736(90)90736-o. [DOI] [PubMed] [Google Scholar]
- Talbot R. W., Heppell J., Dozois R. R., Beart R. W., Jr Vascular complications of inflammatory bowel disease. Mayo Clin Proc. 1986 Feb;61(2):140–145. doi: 10.1016/s0025-6196(12)65200-8. [DOI] [PubMed] [Google Scholar]
- Wakefield A. J., Sawyerr A. M., Dhillon A. P., Pittilo R. M., Rowles P. M., Lewis A. A., Pounder R. E. Pathogenesis of Crohn's disease: multifocal gastrointestinal infarction. Lancet. 1989 Nov 4;2(8671):1057–1062. doi: 10.1016/s0140-6736(89)91078-7. [DOI] [PubMed] [Google Scholar]


