Abstract
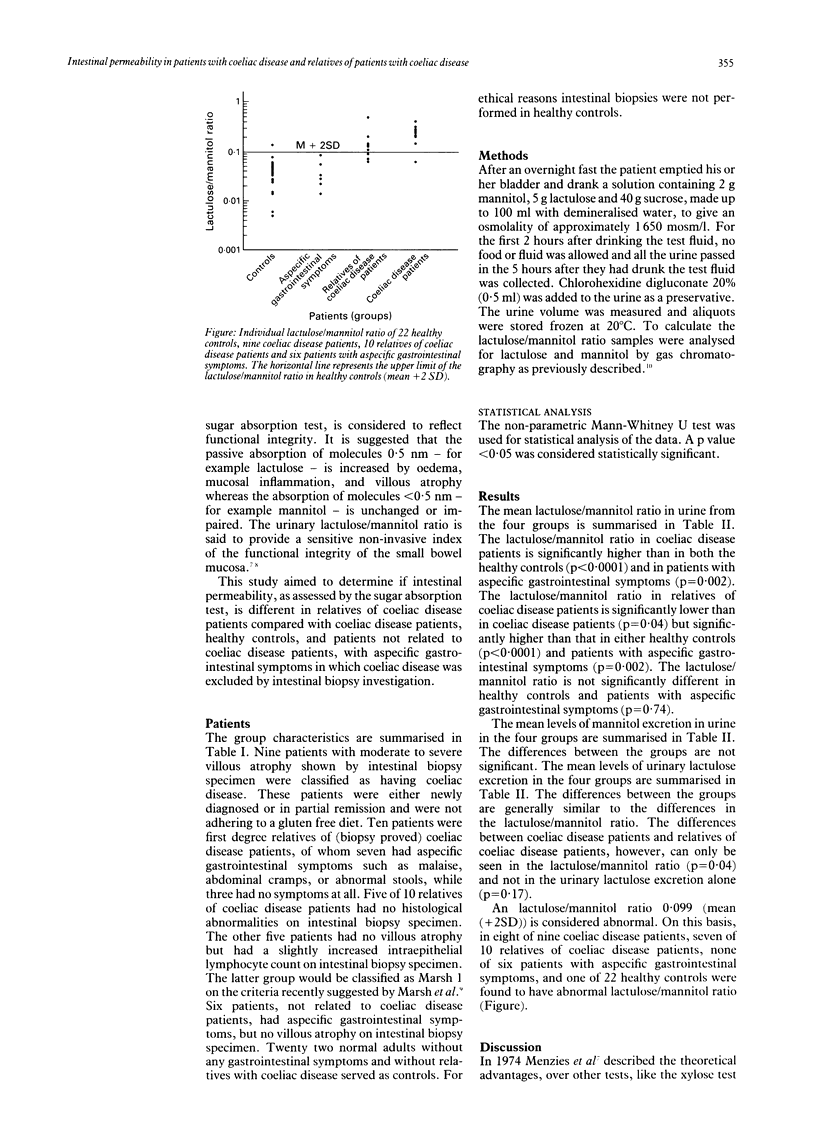
The functional integrity of the small bowel is impaired in coeliac disease. Intestinal permeability, as measured by the sugar absorption test probably reflects this phenomenon. In the sugar absorption test a solution of lactulose and mannitol was given to the fasting patient and the lactulose/mannitol ratio measured in urine collected over a period of five hours. The sugar absorption test was performed in nine patients with coeliac disease with an abnormal jejunum on histological examination, 10 relatives of patients with coeliac disease with aspecific symptoms but no villous atrophy, six patients with aspecific gastrointestinal symptoms but no villous atrophy, and 22 healthy controls to determine whether functional integrity is different in these groups. The lactulose/mannitol ratio (mean (SEM) is significantly higher in both coeliac disease (0.243 (0.034), p < 0.0001)) and relatives of patients with coeliac disease (0.158 (0.040), p < 0.005)) v both healthy controls (0.043 (0.006)) and patients with aspecific gastrointestinal symptoms (0.040 (0.011)). The lactulose/mannitol ratio in relatives of coeliac disease patients was significantly lower than in the coeliac disease patient group (p = 0.04). The lactulose/mannitol ratio was the same in healthy controls and patients with aspecific gastrointestinal symptoms. It is concluded that the sugar absorption test is a sensitive test that distinguishes between patients with coeliac disease and healthy controls. The explanation for the increased permeability in relatives of patients with coeliac disease is uncertain. Increased intestinal permeability may be related to constitutional factors in people susceptible to coeliac disease and may detect latent coeliac disease. The sugar absorption test may therefore be helpful in family studies of coeliac disease.
Full text
PDF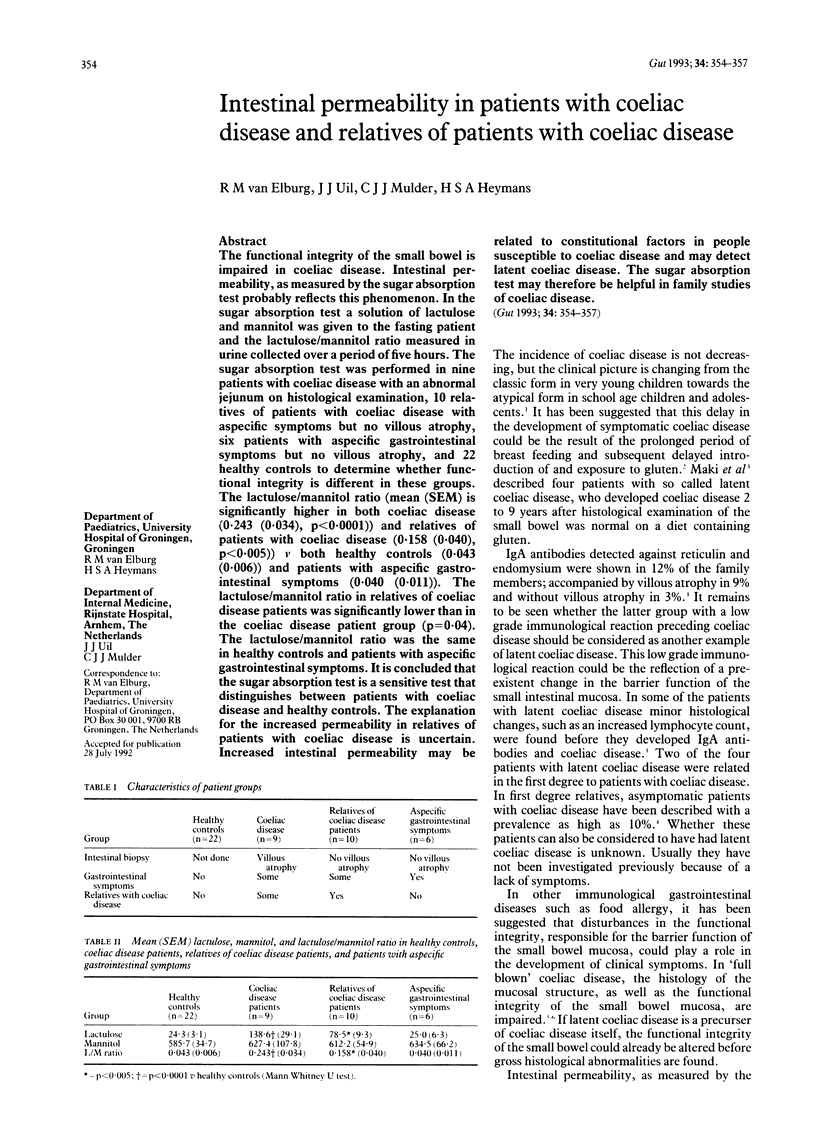


Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Arnason J. A., Gudjónsson H., Freysdóttir J., Jónsdóttir I., Valdimarsson H. Do adults with high gliadin antibody concentrations have subclinical gluten intolerance? Gut. 1992 Feb;33(2):194–197. doi: 10.1136/gut.33.2.194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ceccarelli M., Caiulo V. A., Ughi C. Is childhood coeliac disease underdiagnosed? Eur J Pediatr. 1991 Sep;150(11):821–821. doi: 10.1007/BF02026721. [DOI] [PubMed] [Google Scholar]
- Holmes G. K., Prior P., Lane M. R., Pope D., Allan R. N. Malignancy in coeliac disease--effect of a gluten free diet. Gut. 1989 Mar;30(3):333–338. doi: 10.1136/gut.30.3.333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Howden C. W., Robertson C., Duncan A., Morris A. J., Russell R. I. Comparison of different measurements of intestinal permeability in inflammatory bowel disease. Am J Gastroenterol. 1991 Oct;86(10):1445–1449. [PubMed] [Google Scholar]
- Jansen G., Muskiet F. A., Schierbeek H., Berger R., van der Slik W. Capillary gas chromatographic profiling of urinary, plasma and erythrocyte sugars and polyols as their trimethylsilyl derivatives, preceded by a simple and rapid prepurification method. Clin Chim Acta. 1986 Jun 30;157(3):277–293. doi: 10.1016/0009-8981(86)90303-7. [DOI] [PubMed] [Google Scholar]
- Juby L. D., Rothwell J., Axon A. T. Cellobiose/mannitol sugar test--a sensitive tubeless test for coeliac disease: results on 1010 unselected patients. Gut. 1989 Apr;30(4):476–480. doi: 10.1136/gut.30.4.476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Juby L. D., Rothwell J., Axon A. T. Lactulose/mannitol test: an ideal screen for celiac disease. Gastroenterology. 1989 Jan;96(1):79–85. doi: 10.1016/0016-5085(89)90767-1. [DOI] [PubMed] [Google Scholar]
- Lerner A., Lebenthal E. The controversy of the use of anti-gluten antibody (AGA) as a diagnostic tool in celiac disease. J Pediatr Gastroenterol Nutr. 1991 May;12(4):407–409. doi: 10.1097/00005176-199105000-00001. [DOI] [PubMed] [Google Scholar]
- Lifschitz C. H., Shulman R. J. Intestinal permeability tests: are they clinically useful? J Pediatr Gastroenterol Nutr. 1990 Apr;10(3):283–287. doi: 10.1097/00005176-199004000-00002. [DOI] [PubMed] [Google Scholar]
- Marsh M. N. Gluten, major histocompatibility complex, and the small intestine. A molecular and immunobiologic approach to the spectrum of gluten sensitivity ('celiac sprue'). Gastroenterology. 1992 Jan;102(1):330–354. [PubMed] [Google Scholar]
- Mäki M., Holm K. Incidence and prevalence of coeliac disease in Tampere. Coeliac disease is not disappearing. Acta Paediatr Scand. 1990 Oct;79(10):980–982. doi: 10.1111/j.1651-2227.1990.tb11367.x. [DOI] [PubMed] [Google Scholar]
- Mäki M., Holm K., Koskimies S., Hällström O., Visakorpi J. K. Normal small bowel biopsy followed by coeliac disease. Arch Dis Child. 1990 Oct;65(10):1137–1141. doi: 10.1136/adc.65.10.1137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stenhammar L., Fälth-Magnusson K., Jansson G., Magnusson K. E., Sundqvist T. Intestinal permeability to inert sugars and different-sized polyethyleneglycols in children with celiac disease. J Pediatr Gastroenterol Nutr. 1989 Oct;9(3):281–289. doi: 10.1097/00005176-198910000-00004. [DOI] [PubMed] [Google Scholar]
- Ukabam S. O., Cooper B. T. Small intestinal permeability as an indicator of jejunal mucosal recovery in patients with celiac sprue on a gluten-free diet. J Clin Gastroenterol. 1985 Jun;7(3):232–236. doi: 10.1097/00004836-198506000-00009. [DOI] [PubMed] [Google Scholar]


