Abstract
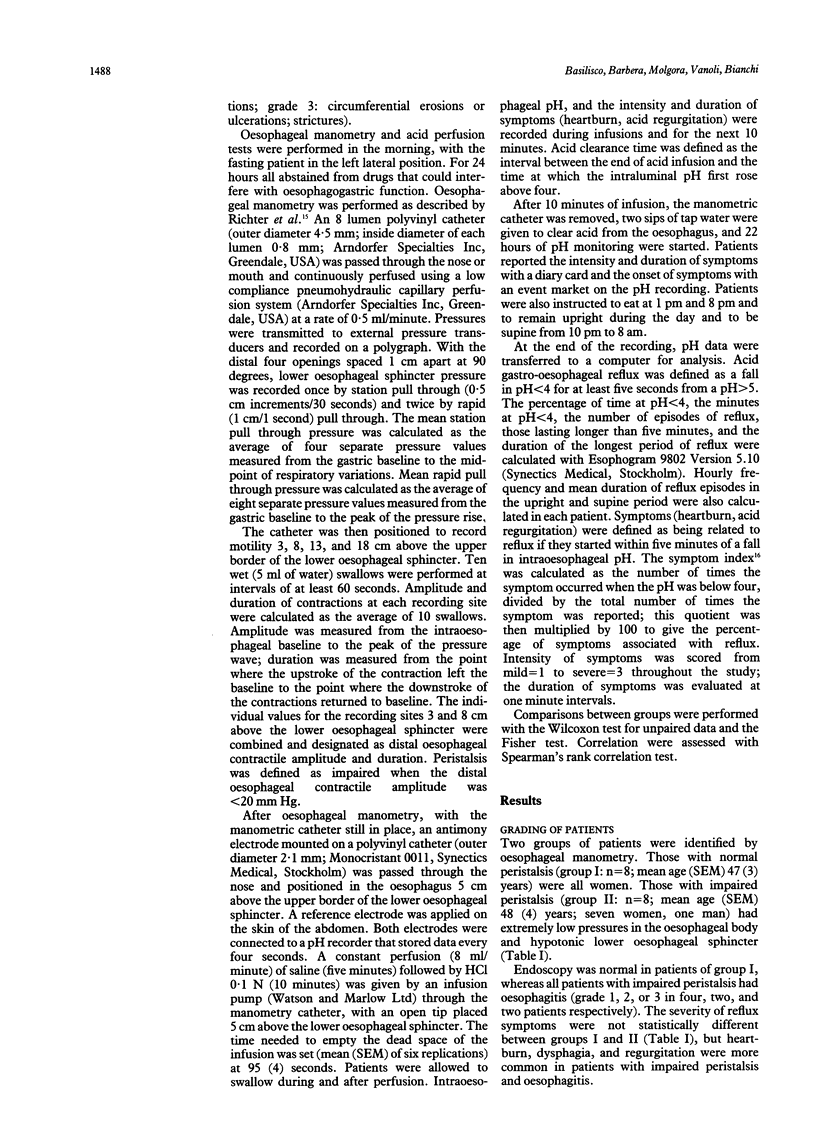
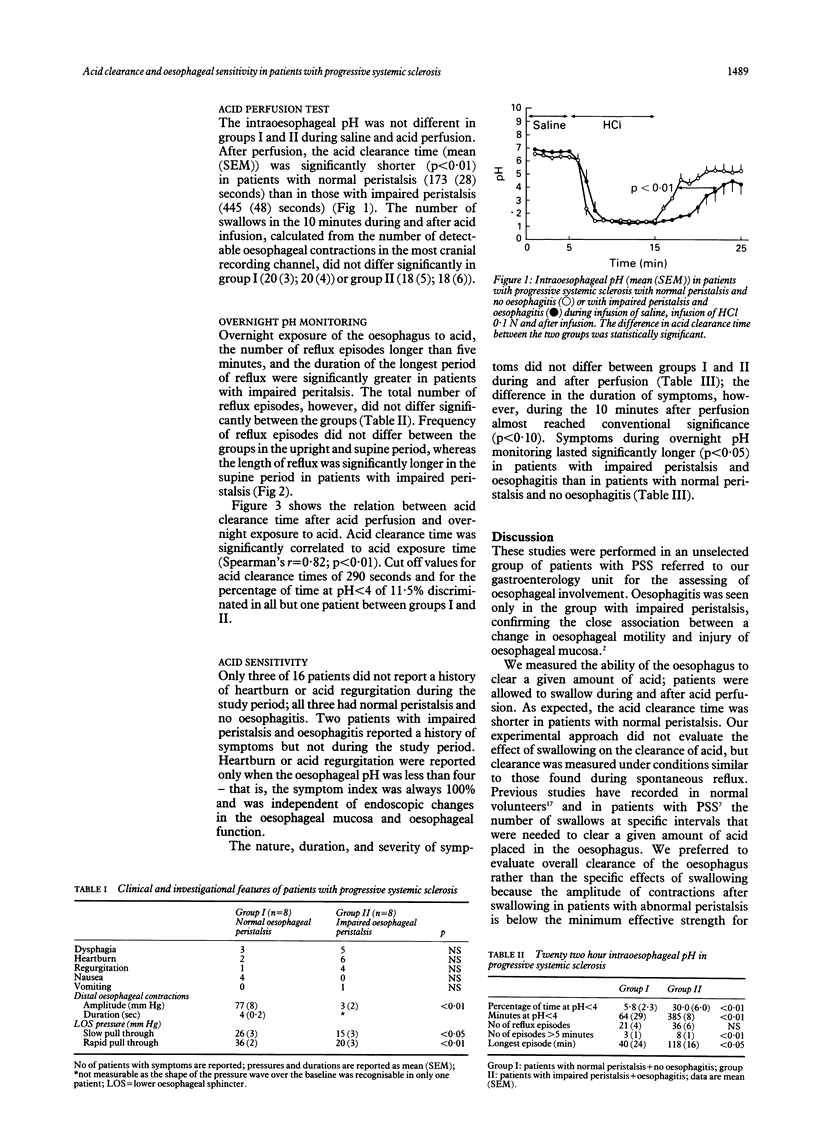
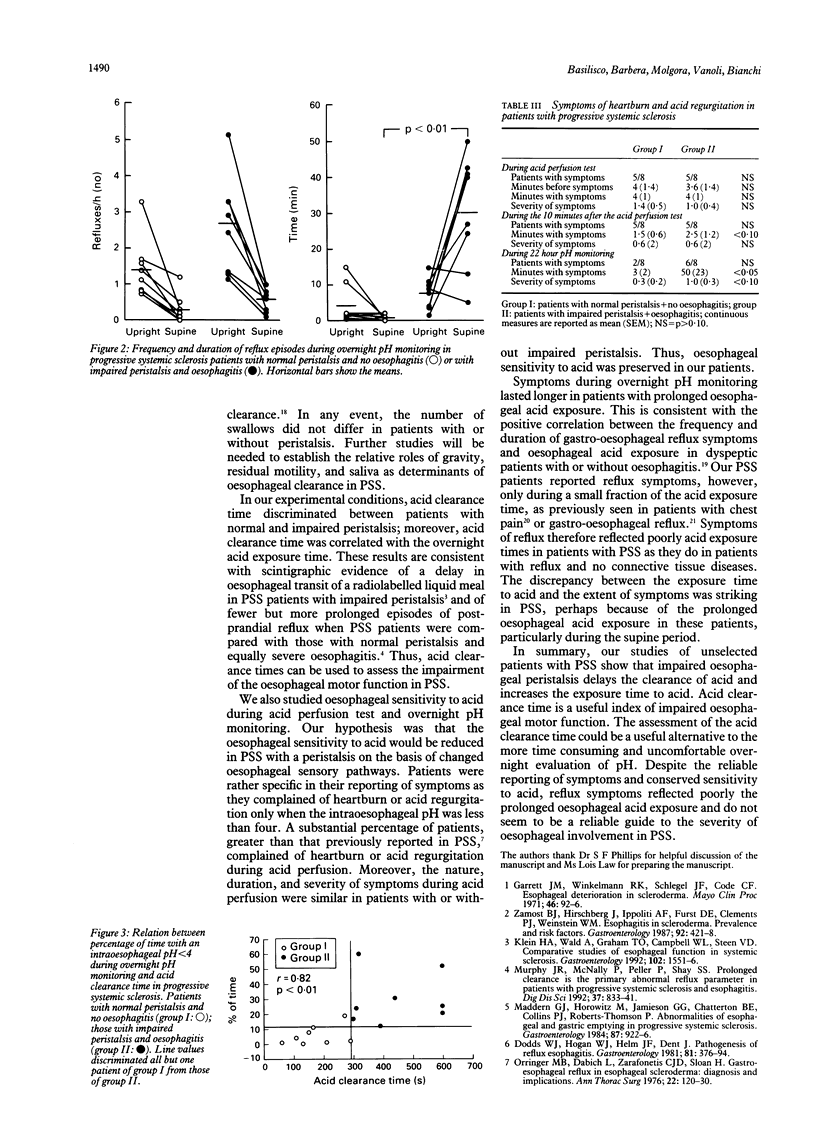
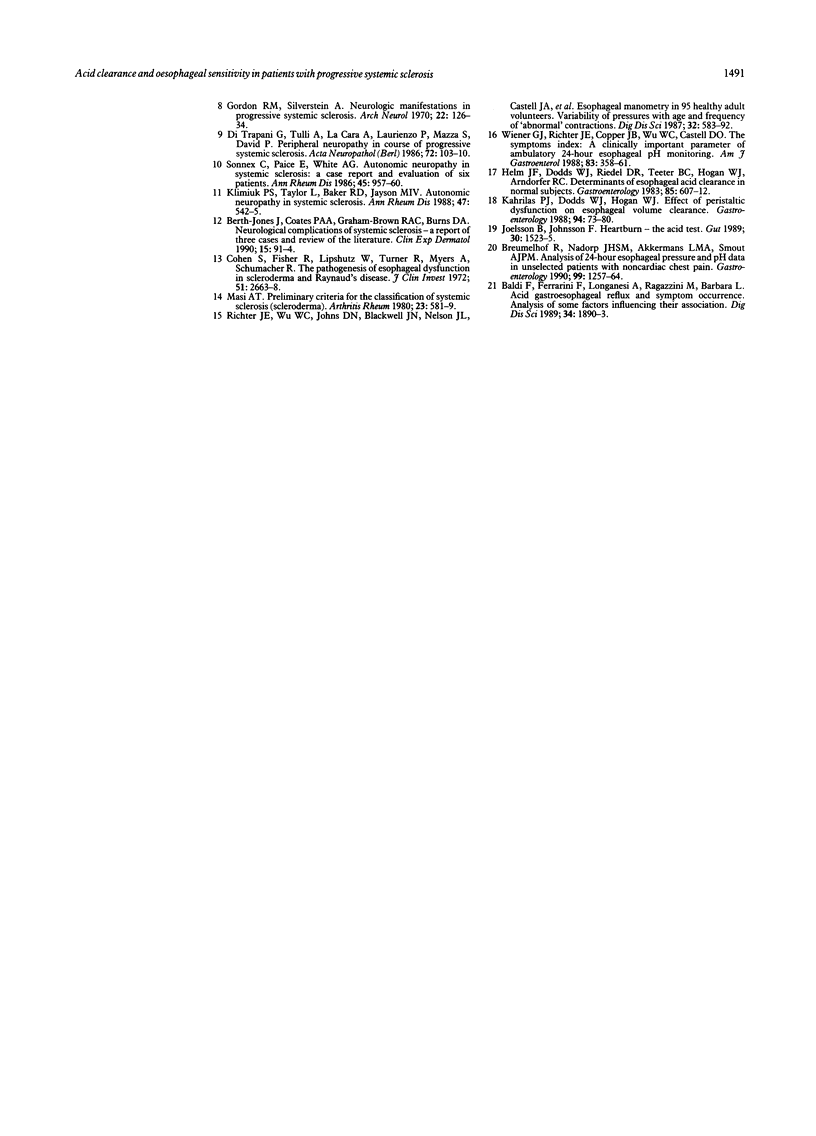
This study examined the hypothesis that impaired oesophageal peristalsis was associated with delayed oesophageal clearance of acid in patients with progressive systemic sclerosis (PSS), some of whom are thought to have impaired oesophageal sensitivity to acid. Sixteen patients with PSS had: (a) oesophageal manometry and endoscopy; (b) acid perfusion of the oesophagus with simultaneous measurement of intraoesophageal pH during perfusion and for the next 10 minutes; (c) 22 hour monitoring of intraoesophageal pH; and (d) an evaluation of reflux symptoms during and after perfusion and during overnight pH monitoring. By oesophageal manometry, eight patients had normal peristalsis and eight patients had impaired peristalsis. Oesophageal endoscopy was unremarkable in patients with normal peristalsis, whereas all patients with impaired peristalsis had oesophagitis. The time needed to clear the oesophagus of perfused acid was shorter (p < 0.01) in patients with normal peristalsis and acid clearance time was significantly correlated (p < 0.01) with acid exposure time during overnight pH monitoring. During and after oesophageal perfusion, the nature, duration, and severity of symptoms did not differ between the groups, but overnight symptoms lasted longer (p < 0.05) in patients with impaired peristalsis. It is concluded that in PSS: (1) Impaired oesophageal motility delayed the clearance of acid and increased the exposure time to acid. (2) Acid clearance time is a useful parameter of impaired oesophageal motor function. The assessment of acid clearance time can be used as an alternative to overnight pH monitoring, to assess the impairment of oesophageal acid clearance. (3) Oesophageal sensitivity to acid was preserved in patients with impaired peristalsis and oesophagitis. (4) Reflux symptoms lasted longer in patients with prolonged oesophageal acid exposure but were still reported for a small fraction of the total acid exposure time. Thus, reflux symptoms reflect poorly prolonged exposure of the oesophagus to acid and are not a reliable guide to acid injury of the oesophagus in PSS.
Full text
PDF
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Baldi F., Ferrarini F., Longanesi A., Ragazzini M., Barbara L. Acid gastroesophageal reflux and symptom occurrence. Analysis of some factors influencing their association. Dig Dis Sci. 1989 Dec;34(12):1890–1893. doi: 10.1007/BF01536707. [DOI] [PubMed] [Google Scholar]
- Berth-Jones J., Coates P. A., Graham-Brown R. A., Burns D. A. Neurological complications of systemic sclerosis--a report of three cases and review of the literature. Clin Exp Dermatol. 1990 Mar;15(2):91–94. doi: 10.1111/j.1365-2230.1990.tb02039.x. [DOI] [PubMed] [Google Scholar]
- Breumelhof R., Nadorp J. H., Akkermans L. M., Smout A. J. Analysis of 24-hour esophageal pressure and pH data in unselected patients with noncardiac chest pain. Gastroenterology. 1990 Nov;99(5):1257–1264. doi: 10.1016/0016-5085(90)91147-x. [DOI] [PubMed] [Google Scholar]
- Cohen S., Fisher R., Lipshutz W., Turner R., Myers A., Schumacher R. The pathogenesis of esophageal dysfunction in scleroderma and Raynaud's disease. J Clin Invest. 1972 Oct;51(10):2663–2668. doi: 10.1172/JCI107084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Di Trapani G., Tulli A., La Cara A., Laurienzo P., Mazza S., David P. Peripheral neuropathy in course of progressive systemic sclerosis. Light and ultrastructural study. Acta Neuropathol. 1986;72(2):103–110. doi: 10.1007/BF00685970. [DOI] [PubMed] [Google Scholar]
- Dodds W. J., Hogan W. J., Helm J. F., Dent J. Pathogenesis of reflux esophagitis. Gastroenterology. 1981 Aug;81(2):376–394. [PubMed] [Google Scholar]
- Garrett J. M., Winkelmann R. K., Schlegel J. F., Code C. F. Esophageal deterioration in scleroderma. Mayo Clin Proc. 1971 Feb;46(2):92–96. [PubMed] [Google Scholar]
- Gordon R. M., Silverstein A. Neurologic manifstations in progressive systemic sclerosis. Arch Neurol. 1970 Feb;22(2):126–134. doi: 10.1001/archneur.1970.00480200032003. [DOI] [PubMed] [Google Scholar]
- Helm J. F., Dodds W. J., Riedel D. R., Teeter B. C., Hogan W. J., Arndorfer R. C. Determinants of esophageal acid clearance in normal subjects. Gastroenterology. 1983 Sep;85(3):607–612. [PubMed] [Google Scholar]
- Joelsson B., Johnsson F. Heartburn--the acid test. Gut. 1989 Nov;30(11):1523–1525. doi: 10.1136/gut.30.11.1523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kahrilas P. J., Dodds W. J., Hogan W. J. Effect of peristaltic dysfunction on esophageal volume clearance. Gastroenterology. 1988 Jan;94(1):73–80. doi: 10.1016/0016-5085(88)90612-9. [DOI] [PubMed] [Google Scholar]
- Klein H. A., Wald A., Graham T. O., Campbell W. L., Steen V. D. Comparative studies of esophageal function in systemic sclerosis. Gastroenterology. 1992 May;102(5):1551–1556. doi: 10.1016/0016-5085(92)91713-e. [DOI] [PubMed] [Google Scholar]
- Klimiuk P. S., Taylor L., Baker R. D., Jayson M. I. Autonomic neuropathy in systemic sclerosis. Ann Rheum Dis. 1988 Jul;47(7):542–545. doi: 10.1136/ard.47.7.542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maddern G. J., Horowitz M., Jamieson G. G., Chatterton B. E., Collins P. J., Roberts-Thomson P. Abnormalities of esophageal and gastric emptying in progressive systemic sclerosis. Gastroenterology. 1984 Oct;87(4):922–926. [PubMed] [Google Scholar]
- Murphy J. R., McNally P., Peller P., Shay S. S. Prolonged clearance is the primary abnormal reflux parameter in patients with progressive systemic sclerosis and esophagitis. Dig Dis Sci. 1992 Jun;37(6):833–841. doi: 10.1007/BF01300380. [DOI] [PubMed] [Google Scholar]
- Orringer M. B., Dabich L., Zarafonetis C. J., Sloan H. Gastroesophageal reflux in esophageal scleroderma: diagnosis and implications. Ann Thorac Surg. 1976 Aug;22(2):120–130. doi: 10.1016/s0003-4975(10)63972-0. [DOI] [PubMed] [Google Scholar]
- Preliminary criteria for the classification of systemic sclerosis (scleroderma). Subcommittee for scleroderma criteria of the American Rheumatism Association Diagnostic and Therapeutic Criteria Committee. Arthritis Rheum. 1980 May;23(5):581–590. doi: 10.1002/art.1780230510. [DOI] [PubMed] [Google Scholar]
- Richter J. E., Wu W. C., Johns D. N., Blackwell J. N., Nelson J. L., 3rd, Castell J. A., Castell D. O. Esophageal manometry in 95 healthy adult volunteers. Variability of pressures with age and frequency of "abnormal" contractions. Dig Dis Sci. 1987 Jun;32(6):583–592. doi: 10.1007/BF01296157. [DOI] [PubMed] [Google Scholar]
- Sonnex C., Paice E., White A. G. Autonomic neuropathy in systemic sclerosis: a case report and evaluation of six patients. Ann Rheum Dis. 1986 Nov;45(11):957–960. doi: 10.1136/ard.45.11.957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wiener G. J., Richter J. E., Copper J. B., Wu W. C., Castell D. O. The symptom index: a clinically important parameter of ambulatory 24-hour esophageal pH monitoring. Am J Gastroenterol. 1988 Apr;83(4):358–361. [PubMed] [Google Scholar]
- Zamost B. J., Hirschberg J., Ippoliti A. F., Furst D. E., Clements P. J., Weinstein W. M. Esophagitis in scleroderma. Prevalence and risk factors. Gastroenterology. 1987 Feb;92(2):421–428. doi: 10.1016/0016-5085(87)90137-5. [DOI] [PubMed] [Google Scholar]


