Abstract
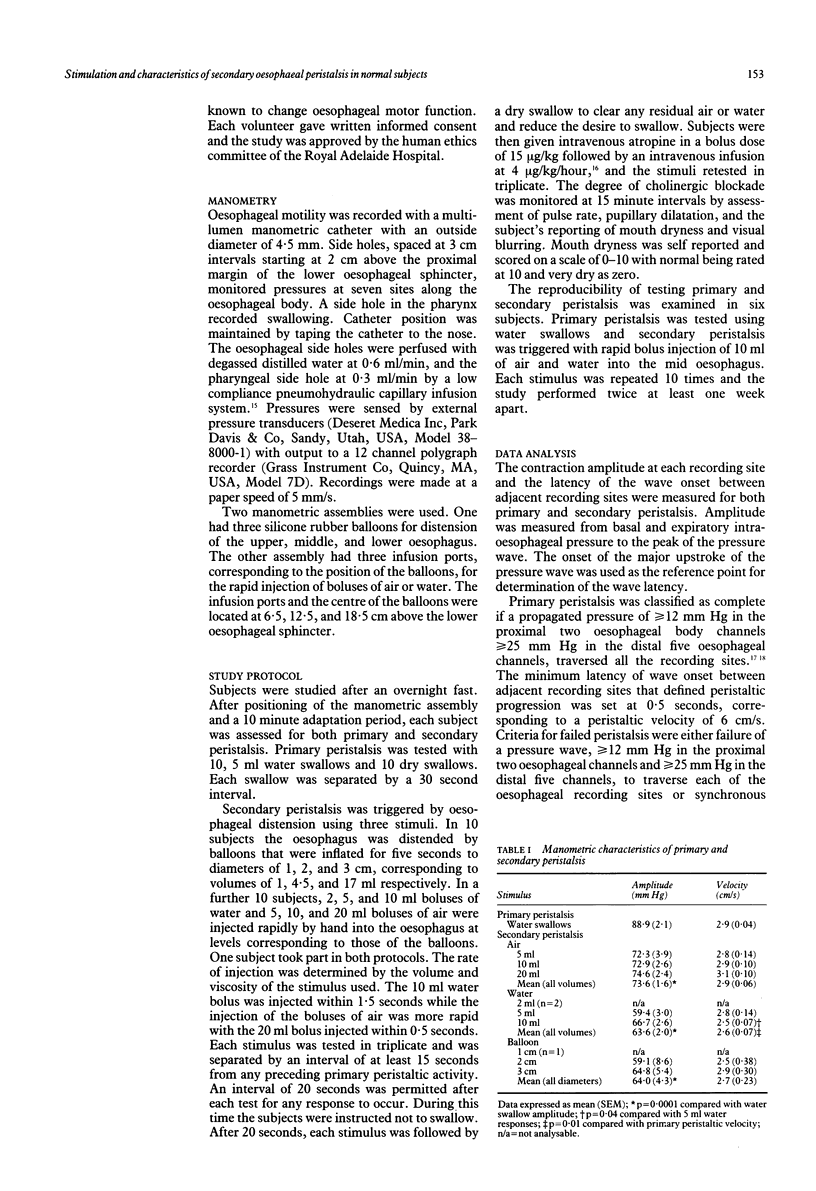
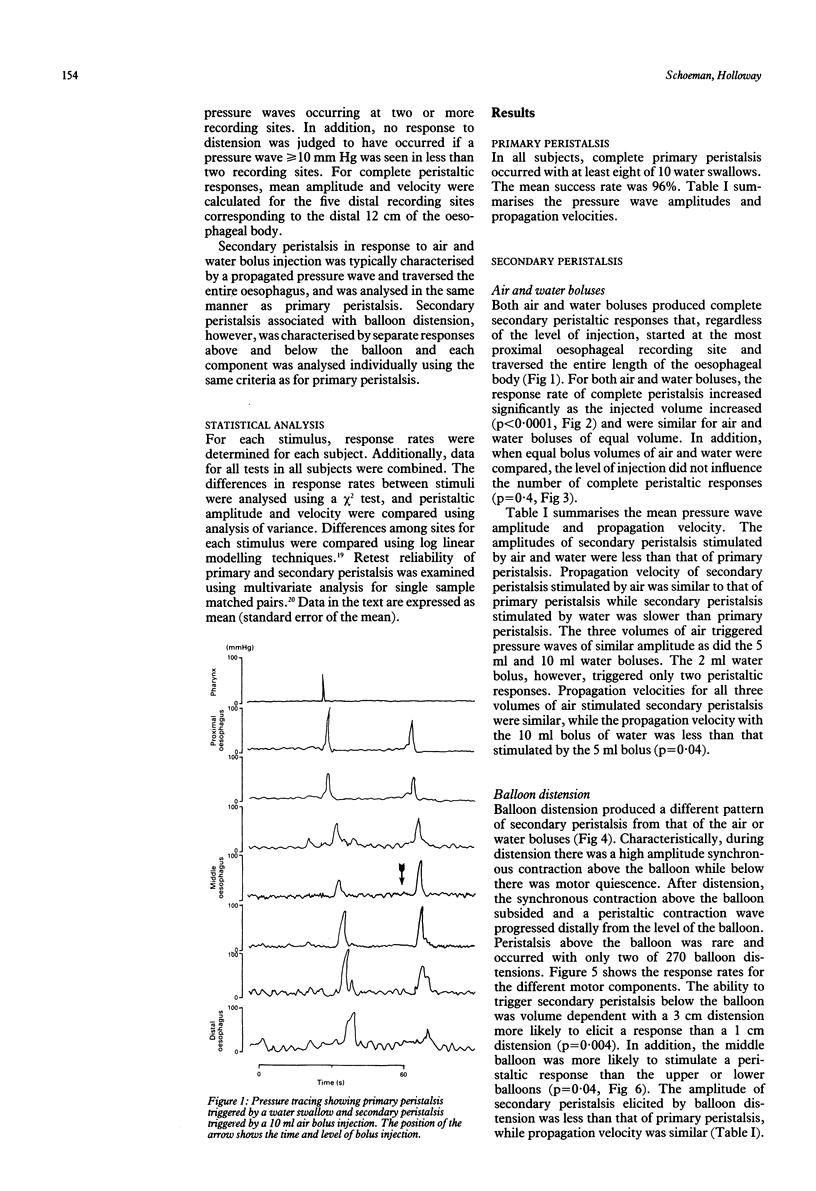
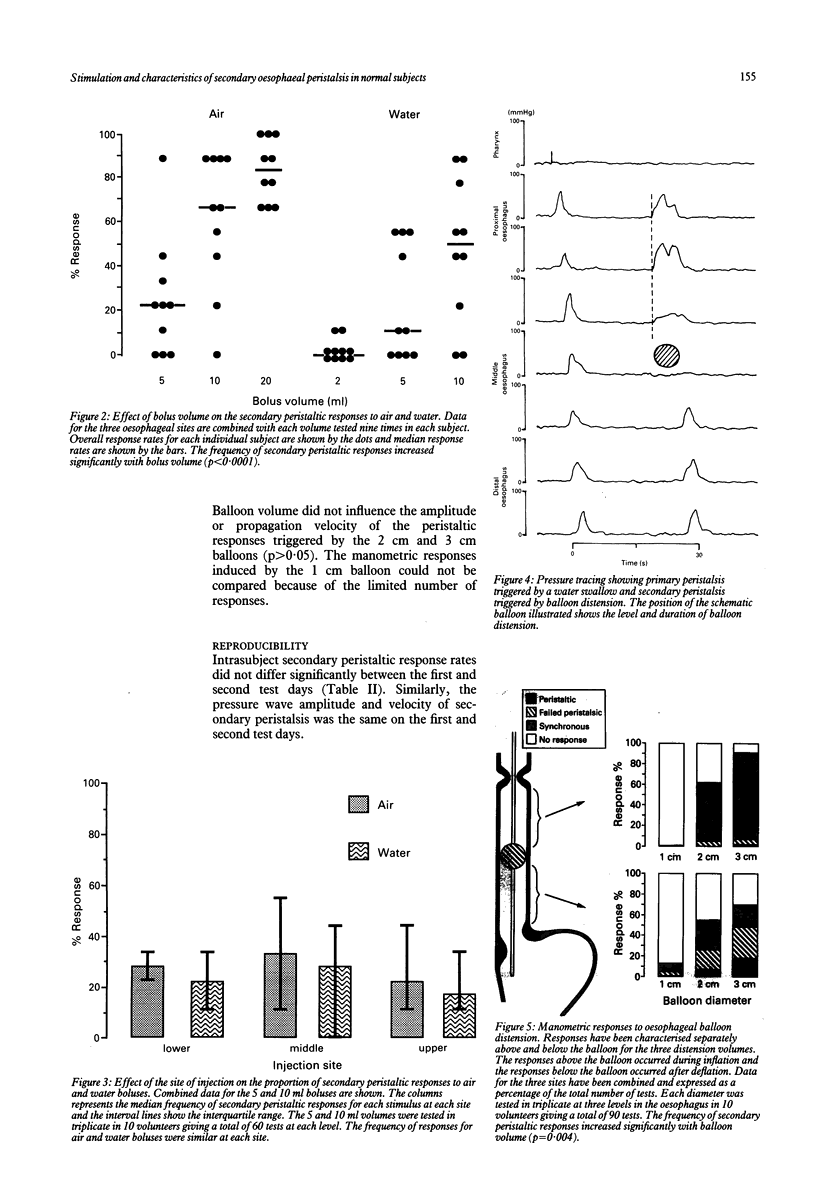
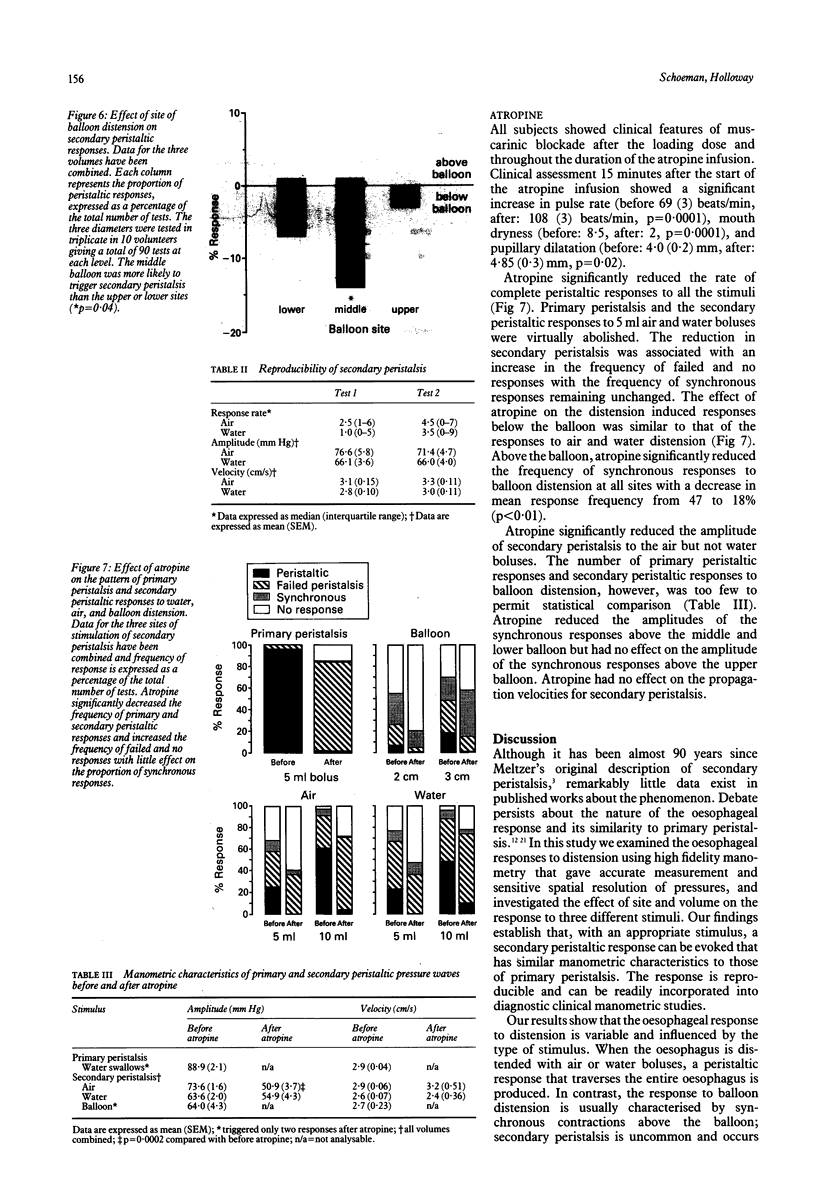
The study evaluates the triggering and characteristics of secondary oesophageal peristalsis in 25 healthy volunteers. Secondary peristalsis was stimulated by rapid intraoesophageal injection of boluses of air and water, and by a five second oesophageal distension with a balloon. Air and water boluses triggered secondary peristalsis that started in the proximal oesophagus regardless of injection site. Response rates were volume dependent with 83% of the 20 ml air boluses triggering secondary peristalsis compared with 2% for the 2 ml water bolus (p < 0.0001). Response rates for air and water were similar for equal bolus volumes and were not influenced by the site of injection. In contrast, balloon distension usually induced a synchronous contraction above the balloon, with secondary peristalsis starting below the balloon after deflation. The peristaltic response rate to balloon distension was also volume dependent and the middle balloon was more effective in triggering secondary peristalsis than either the upper or lower balloons (p < 0.001). Secondary peristaltic amplitude was less than that of primary peristalsis (p < 0.001). Secondary peristaltic velocity with a water bolus was slower (p = 0.001) than that of primary peristalsis. Intravenous atropine significantly reduced secondary peristaltic responses to all stimuli. There was also a significant reduction in pressure wave amplitude for air stimulated secondary peristalsis while those for the water responses were similar. Secondary peristaltic velocity with air and water boluses was not changed by atropine. The reproducibility of testing secondary peristalsis was examined six volunteers and did not show any significant differences on separate test days in response rate and peristaltic amplitude or velocity. It is concluded that in normal subjects, secondary peristalsis can be more reliably triggered by intraoesophageal air or water infusion than balloon distension. Secondary peristaltic amplitude and velocity are stimulus but not site or volume dependent and propagation is partially mediated by cholinergic nerves.
Full text
PDF

Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Arndorfer R. C., Stef J. J., Dodds W. J., Linehan J. H., Hogan W. J. Improved infusion system for intraluminal esophageal manometry. Gastroenterology. 1977 Jul;73(1):23–27. [PubMed] [Google Scholar]
- Blank E. L., Greenwood B., Dodds W. J. Cholinergic control of smooth muscle peristalsis in the cat esophagus. Am J Physiol. 1989 Oct;257(4 Pt 1):G517–G523. doi: 10.1152/ajpgi.1989.257.4.G517. [DOI] [PubMed] [Google Scholar]
- CREAMER B., SCHLEGEL J. Motor responses of the esophagus to distention. J Appl Physiol. 1957 May;10(3):498–504. doi: 10.1152/jappl.1957.10.3.498. [DOI] [PubMed] [Google Scholar]
- Corazziari E., Pozzessere C., Dani S., Anzini F., Torsoli A. Intraluminal pH esophageal motility. Gastroenterology. 1978 Aug;75(2):275–277. [PubMed] [Google Scholar]
- DORNHORST A. C., HARRISON K., PIERCE J. W. Observations on the normal oesophagus and cardia. Lancet. 1954 Apr 3;266(6814):695–698. doi: 10.1016/s0140-6736(54)92106-6. [DOI] [PubMed] [Google Scholar]
- Dent J., Dodds W. J., Friedman R. H., Sekiguchi T., Hogan W. J., Arndorfer R. C., Petrie D. J. Mechanism of gastroesophageal reflux in recumbent asymptomatic human subjects. J Clin Invest. 1980 Feb;65(2):256–267. doi: 10.1172/JCI109667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dodds W. J., Dent J., Hogan W. J., Arndorfer R. C. Effect of atropine on esophageal motor function in humans. Am J Physiol. 1981 Apr;240(4):G290–G296. doi: 10.1152/ajpgi.1981.240.4.G290. [DOI] [PubMed] [Google Scholar]
- Dodds W. J., Hogan W. J., Reid D. P., Stewart E. T., Arndorfer R. C. A comparison between primary esophageal peristalsis following wet and dry swallows. J Appl Physiol. 1973 Dec;35(6):851–857. doi: 10.1152/jappl.1973.35.6.851. [DOI] [PubMed] [Google Scholar]
- FLESHLER B., HENDRIX T. R., KRAMER P., INGELFINGER F. J. The characteristics and similarity of primary and secondary peristalis in the esophagus. J Clin Invest. 1959 Jan 1;38(1 Pt 1):110–116. doi: 10.1172/JCI103780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gidda J. S., Buyniski J. P. Swallow-evoked peristalsis in opossum esophagus: role of cholinergic mechanisms. Am J Physiol. 1986 Dec;251(6 Pt 1):G779–G785. doi: 10.1152/ajpgi.1986.251.6.G779. [DOI] [PubMed] [Google Scholar]
- Helm J. F., Dodds W. J., Pelc L. R., Palmer D. W., Hogan W. J., Teeter B. C. Effect of esophageal emptying and saliva on clearance of acid from the esophagus. N Engl J Med. 1984 Feb 2;310(5):284–288. doi: 10.1056/NEJM198402023100503. [DOI] [PubMed] [Google Scholar]
- Hewson E. G., Ott D. J., Dalton C. B., Chen Y. M., Wu W. C., Richter J. E. Manometry and radiology. Complementary studies in the assessment of esophageal motility disorders. Gastroenterology. 1990 Mar;98(3):626–632. [PubMed] [Google Scholar]
- Hollis J. B., Castell D. O. Effect of dry swallows and wet swallows of different volumes on esophageal peristalsis. J Appl Physiol. 1975 Jun;38(6):1161–1164. doi: 10.1152/jappl.1975.38.6.1161. [DOI] [PubMed] [Google Scholar]
- Janssens J., Valembois P., Hellemans J., Vantrappen G., Pelemans W. Studies on the necessity of a bolus for the progression of secondary peristalsis in the canine esophagus. Gastroenterology. 1974 Aug;67(2):245–251. [PubMed] [Google Scholar]
- Kahrilas P. J., Dodds W. J., Hogan W. J. Effect of peristaltic dysfunction on esophageal volume clearance. Gastroenterology. 1988 Jan;94(1):73–80. doi: 10.1016/0016-5085(88)90612-9. [DOI] [PubMed] [Google Scholar]
- Massey B. T., Dodds W. J., Hogan W. J., Brasseur J. G., Helm J. F. Abnormal esophageal motility. An analysis of concurrent radiographic and manometric findings. Gastroenterology. 1991 Aug;101(2):344–354. [PubMed] [Google Scholar]
- Paterson W. G., Rattan S., Goyal R. K. Esophageal responses to transient and sustained esophageal distension. Am J Physiol. 1988 Nov;255(5 Pt 1):G587–G595. doi: 10.1152/ajpgi.1988.255.5.G587. [DOI] [PubMed] [Google Scholar]
- Richter J. E., Wu W. C., Johns D. N., Blackwell J. N., Nelson J. L., 3rd, Castell J. A., Castell D. O. Esophageal manometry in 95 healthy adult volunteers. Variability of pressures with age and frequency of "abnormal" contractions. Dig Dis Sci. 1987 Jun;32(6):583–592. doi: 10.1007/BF01296157. [DOI] [PubMed] [Google Scholar]
- Thompson D. G., Andreollo N. A., McIntyre A. S., Earlam R. J. Studies of the oesophageal clearance responses to intraluminal acid. Gut. 1988 Jul;29(7):881–885. doi: 10.1136/gut.29.7.881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vanek A. W., Diamant N. E. Responses of the human esophagus to paired swallows. Gastroenterology. 1987 Mar;92(3):643–650. doi: 10.1016/0016-5085(87)90012-6. [DOI] [PubMed] [Google Scholar]
- Williams D., Thompson D. G., Marples M., Heggie L., O'Hanrahan T., Mani V., Bancewicz J. Identification of an abnormal esophageal clearance response to intraluminal distention in patients with esophagitis. Gastroenterology. 1992 Sep;103(3):943–953. doi: 10.1016/0016-5085(92)90028-w. [DOI] [PubMed] [Google Scholar]
- Winship D. H., Zboralske F. F. The esophageal propulsive force: esophageal response to acute obstruction. J Clin Invest. 1967 Sep;46(9):1391–1401. doi: 10.1172/JCI105631. [DOI] [PMC free article] [PubMed] [Google Scholar]



