Abstract
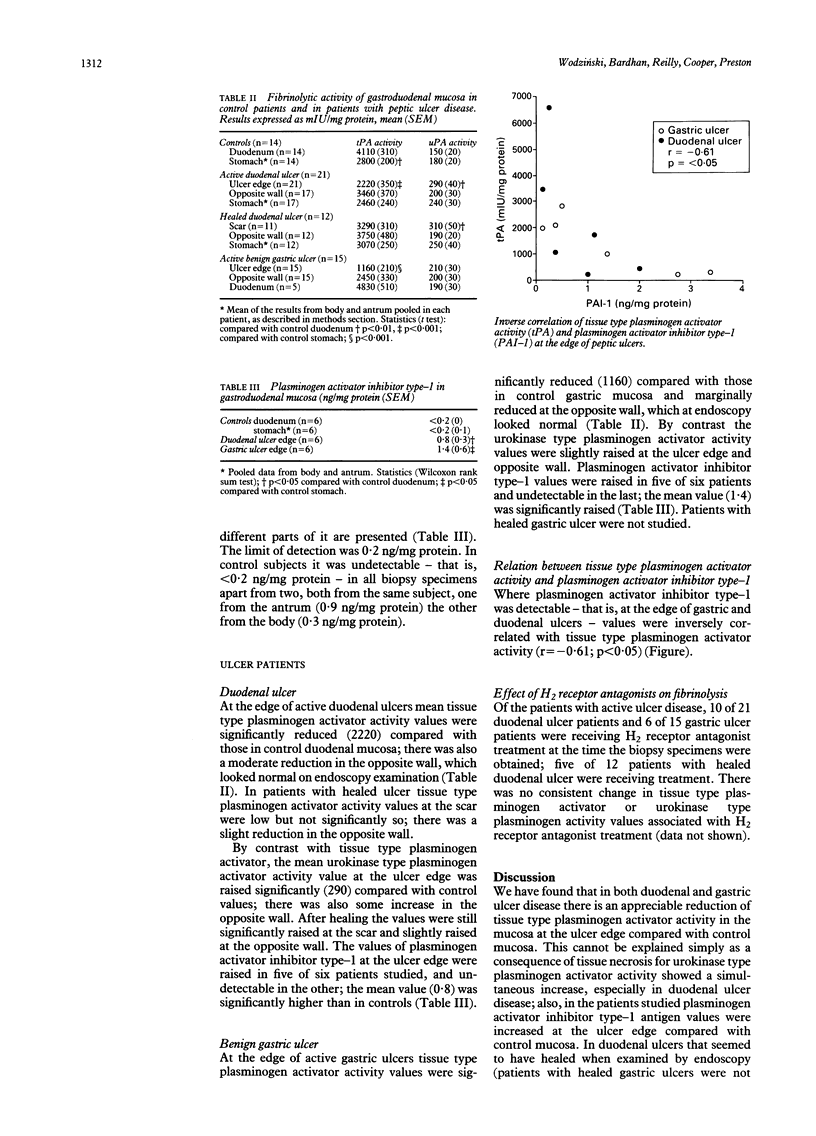
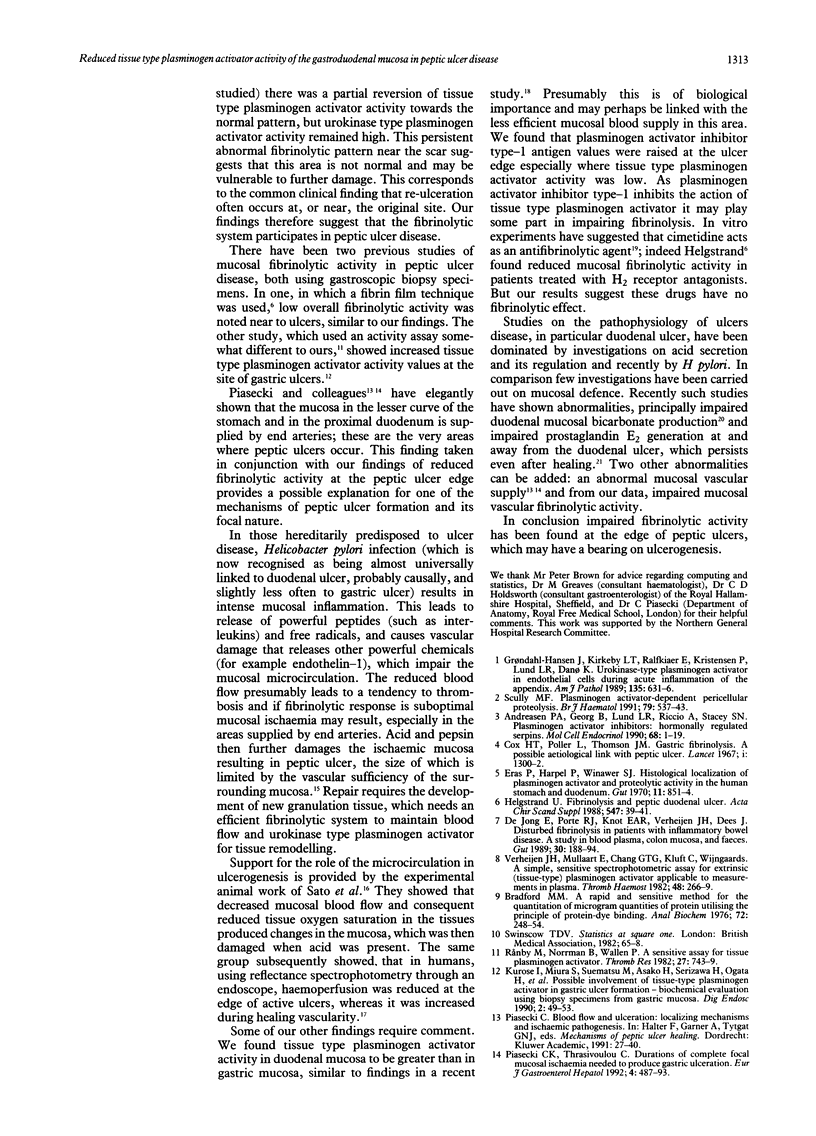
The gastroduodenal mucosa has a rich blood supply. An active fibrinolytic system is presumably required to maintain vascular patency, and impairment may result in reduced blood flow, focal tissue necrosis, and peptic ulcerogenesis. Tissue type and urokinase type plasminogen activator activity (expressed as mIU/mg protein) and plasminogen activator inhibitor type-1 antigen were assayed in homogenates of gastric and duodenal biopsy specimens taken from patients with: normal endoscopy (controls) (n = 14); active duodenal ulcer (n = 21); healed duodenal ulcer (n = 12); and active benign gastric ulcer (n = 15). In controls mean duodenal tissue type plasminogen activator activity was 4110 and urokinase type plasminogen activator activity 150; gastric tissue type plasminogen activator was 2760 and urokinase type plasminogen activator 170; plasminogen activator inhibitor type-1 was generally undetectable. At the edge of active duodenal ulcers tissue type plasminogen activator was considerably reduced, 2220 (p < 0.001) whereas urokinase type plasminogen activator was raised, 290 (p < 0.01). At the edge of active benign gastric ulcers tissue type plasminogen activator was substantially reduced, 1160 (p < 0.001) but urokinase type plasminogen activator was unchanged. At the scar of healed duodenal ulcers tissue type plasminogen activator was slightly reduced, 3290, but urokinase type plasminogen activator was increased, 308 (p < 0.05). H2 receptor antagonist treatment had little effect on tissue type or urokinase type plasminogen activator activity. Plasminogen activator inhibitor type-1 was increased at the edge of active ulcers (p < 0.05) especially when tissue type plasminogen activity was low (r = -0.61, p < 0.05). These findings are consistent with the hypothesis that impaired fibrinolytic activity may be implicated in peptic ulcerogenesis.
Full text
PDF


Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Andreasen P. A., Georg B., Lund L. R., Riccio A., Stacey S. N. Plasminogen activator inhibitors: hormonally regulated serpins. Mol Cell Endocrinol. 1990 Jan 2;68(1):1–19. doi: 10.1016/0303-7207(90)90164-4. [DOI] [PubMed] [Google Scholar]
- Bradford M. M. A rapid and sensitive method for the quantitation of microgram quantities of protein utilizing the principle of protein-dye binding. Anal Biochem. 1976 May 7;72:248–254. doi: 10.1016/0003-2697(76)90527-3. [DOI] [PubMed] [Google Scholar]
- Chakrabarti R., Thompson S. G. Cimetidine and fibrinolysis. Lancet. 1979 Nov 3;2(8149):962–962. doi: 10.1016/s0140-6736(79)92660-6. [DOI] [PubMed] [Google Scholar]
- Cox H. T., Poller L., Thomson J. M. Gastric fibrinolysis. A possible aetiological link with peptic ulcer. Lancet. 1967 Jun 17;1(7503):1300–1302. doi: 10.1016/s0140-6736(67)91594-2. [DOI] [PubMed] [Google Scholar]
- Eras P., Harpel P., Winawer S. J. Histological localization of plasminogen activator and proteolytic activity in the human stomach and duodenum. Gut. 1970 Oct;11(10):851–854. doi: 10.1136/gut.11.10.851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grøndahl-Hansen J., Kirkeby L. T., Ralfkiaer E., Kristensen P., Lund L. R., Danø K. Urokinase-type plasminogen activator in endothelial cells during acute inflammation of the appendix. Am J Pathol. 1989 Oct;135(4):631–636. [PMC free article] [PubMed] [Google Scholar]
- Helgstrand U. Fibrinolysis and peptic ulcer. Acta Chir Scand Suppl. 1988;547:39–41. [PubMed] [Google Scholar]
- Isenberg J. I., Selling J. A., Hogan D. L., Koss M. A. Impaired proximal duodenal mucosal bicarbonate secretion in patients with duodenal ulcer. N Engl J Med. 1987 Feb 12;316(7):374–379. doi: 10.1056/NEJM198702123160704. [DOI] [PubMed] [Google Scholar]
- Pugh S., Williams S. E., Lewin M. R., Ishaque M., Barton T. P., Bose K., Bardhan K. D., Clark C. G. Duodenal and antral mucosal prostaglandin E2 synthesis in a study of normal subjects and all stages of duodenal ulcer disease treated by H2 receptor antagonists. Gut. 1989 Feb;30(2):161–165. doi: 10.1136/gut.30.2.161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rånby M., Norrman B., Wallén P. A sensitive assay for tissue plasminogen activator. Thromb Res. 1982 Sep 15;27(6):743–749. doi: 10.1016/0049-3848(82)90012-3. [DOI] [PubMed] [Google Scholar]
- Sato N., Kawano S., Kamada T., Takeda M. Hemodynamics of the gastric mucosa and gastric ulceration in rats and in patients with gastric ulcer. Dig Dis Sci. 1986 Feb;31(2 Suppl):35S–41S. doi: 10.1007/BF01309321. [DOI] [PubMed] [Google Scholar]
- Scully M. F. Plasminogen activator-dependent pericellular proteolysis. Br J Haematol. 1991 Dec;79(4):537–543. doi: 10.1111/j.1365-2141.1991.tb08078.x. [DOI] [PubMed] [Google Scholar]
- Sier C. F., Verspaget H. W., Griffioen G., Ganesh S., Vloedgraven H. J., Lamers C. B. Plasminogen activators in normal tissue and carcinomas of the human oesophagus and stomach. Gut. 1993 Jan;34(1):80–85. doi: 10.1136/gut.34.1.80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Verheijen J. H., Mullaart E., Chang G. T., Kluft C., Wijngaards G. A simple, sensitive spectrophotometric assay for extrinsic (tissue-type) plasminogen activator applicable to measurements in plasma. Thromb Haemost. 1982 Dec 27;48(3):266–269. [PubMed] [Google Scholar]
- Wormsley K. G. Aetiology of ulcers. Baillieres Clin Gastroenterol. 1988 Jul;2(3):555–571. doi: 10.1016/s0950-3528(88)80005-8. [DOI] [PubMed] [Google Scholar]
- de Jong E., Porte R. J., Knot E. A., Verheijen J. H., Dees J. Disturbed fibrinolysis in patients with inflammatory bowel disease. A study in blood plasma, colon mucosa, and faeces. Gut. 1989 Feb;30(2):188–194. doi: 10.1136/gut.30.2.188. [DOI] [PMC free article] [PubMed] [Google Scholar]



