Abstract
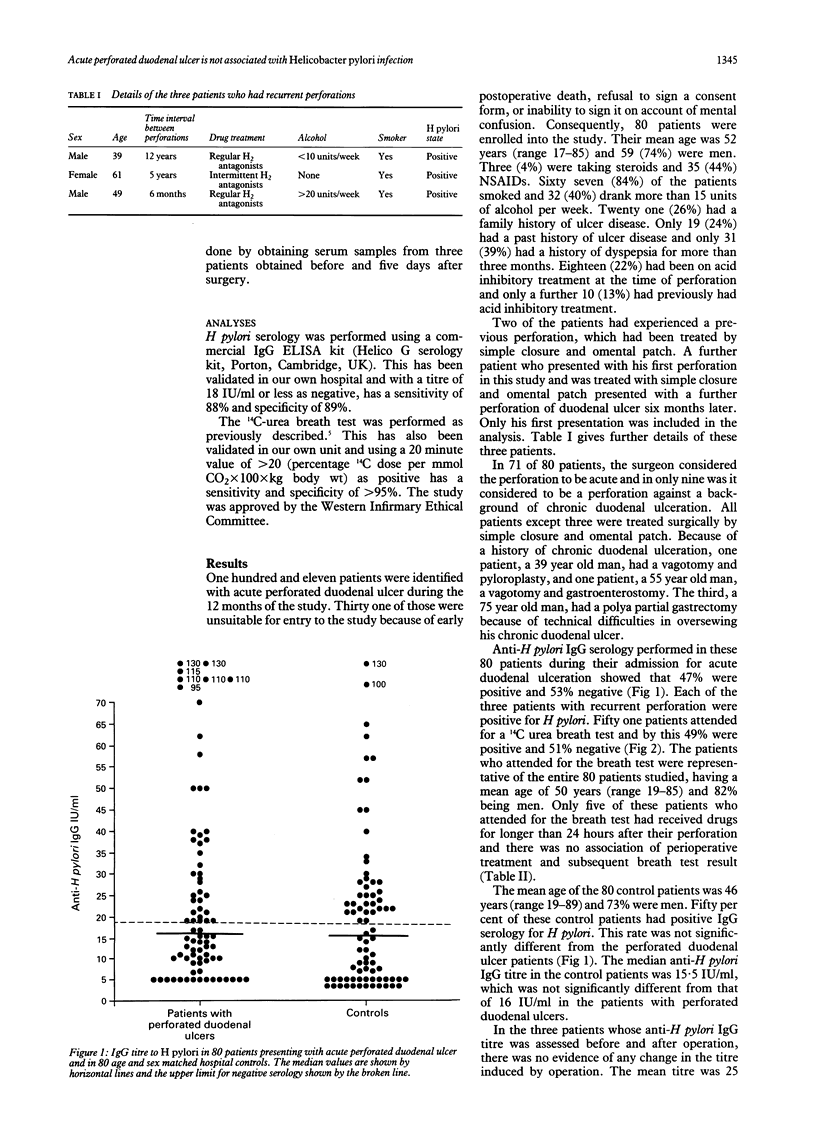
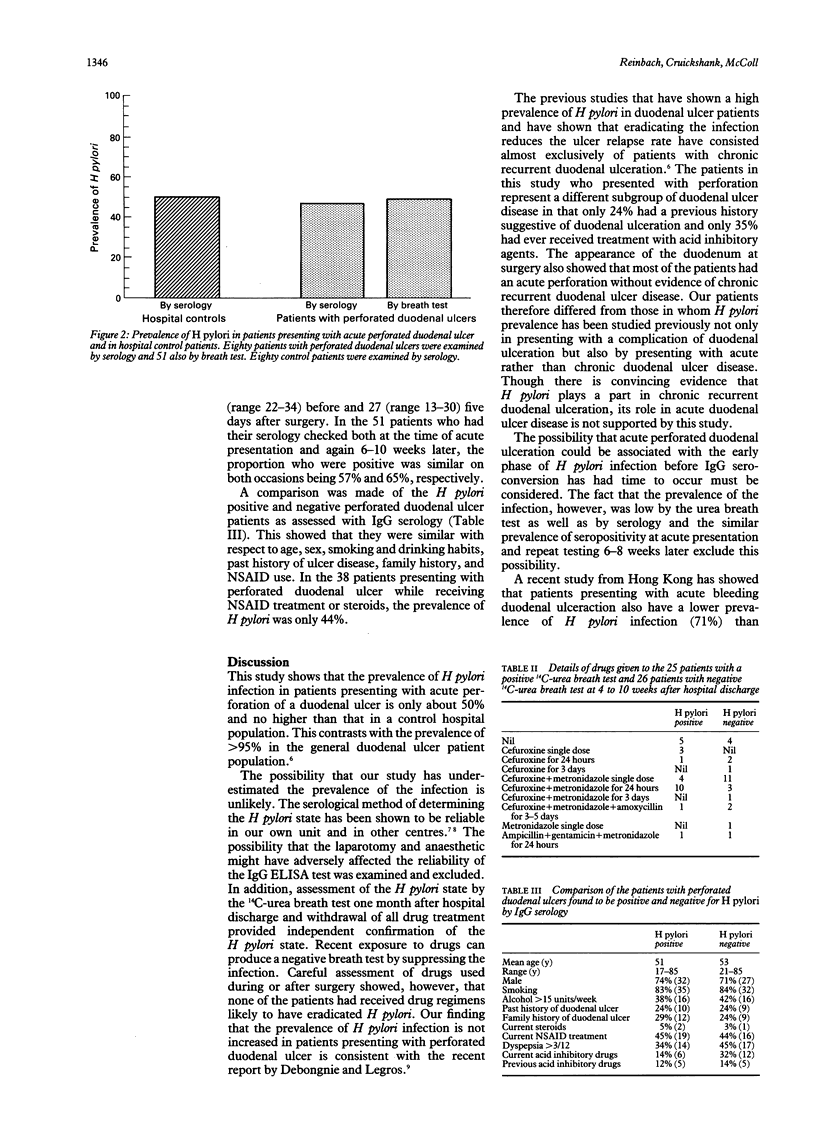
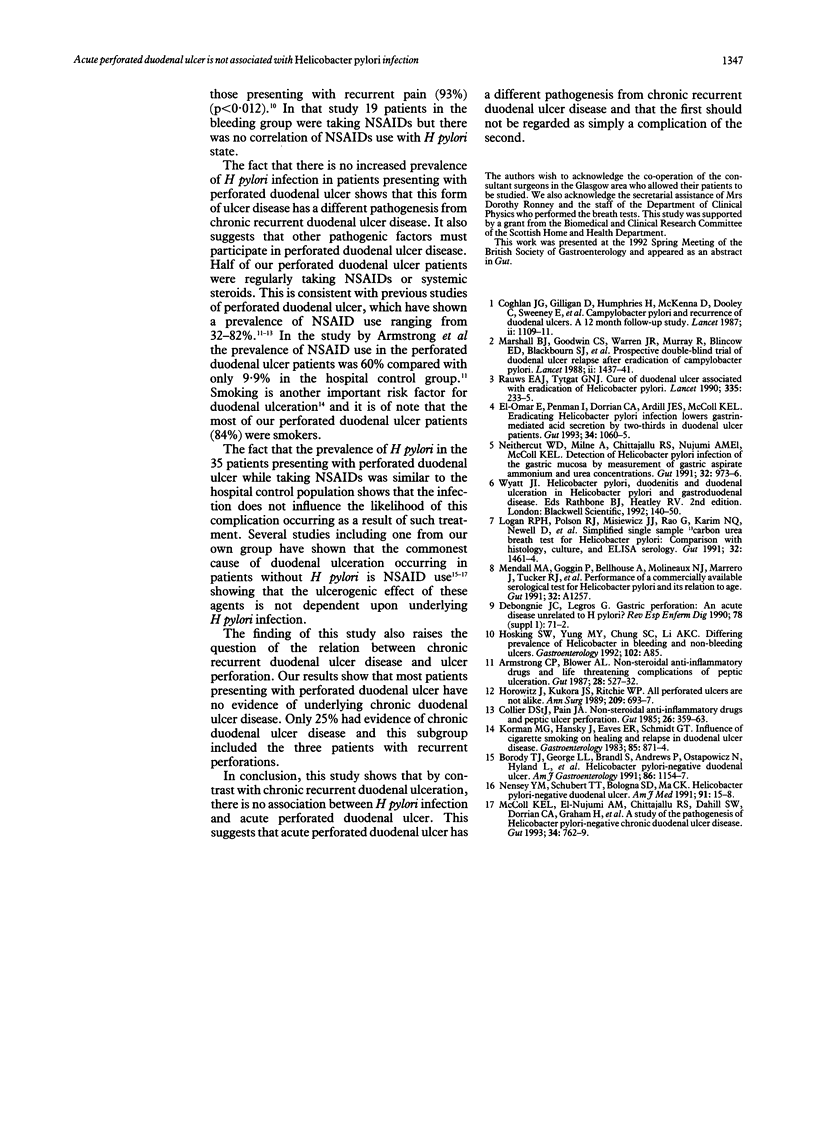
Most patients with chronic duodenal ulcer disease have Helicobacter pylori infection and eradicating it considerably reduces the relapse rate. The prevalence of H pylori in 80 patients (mean age = 52 years, range 17-85) presenting with acute perforated duodenal ulcer was examined and compared with age and sex matched hospital control patients. H pylori state was assessed by serum anti-H pylori IgG (Helico-G kit, Porton) using a titre of 18 or less as negative with a specificity of 89% and sensitivity of 88%. Only 47% of the perforated duodenal ulcer patients were positive for H pylori and this was similar to the value of 50% in the controls. In 51 of the perforated duodenal ulcer patients 14C-urea breath tests were also performed 4-10 weeks after surgery and this confirmed that only 49% were positive for H pylori. None of these patients had received perioperative drugs that might have eradicated the infection. The H pylori positive and H pylori negative perforated duodenal ulcer patients were similar with respect to age (53, 51), smoking (84%, 83%), and consumption of more than 15 units of alcohol per week (42%, 38%). Duodenal ulcer disease had been diagnosed before acute perforation in only 24% of those with H pylori and also 24% of those without the infection. Regular non-steroidal anti-inflammatory drug (NSAID) use was common in both those with (44%) and without (45%) H pylori. In conclusion, the lack of association of acute perforated duodenal ulcer and H pylori infection suggests that perforated duodenal ulcer has a different pathogenesis from chronic duodenal ulcer disease, and that the first should not be regarded simply as a complication of the second.
Full text
PDF
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Armstrong C. P., Blower A. L. Non-steroidal anti-inflammatory drugs and life threatening complications of peptic ulceration. Gut. 1987 May;28(5):527–532. doi: 10.1136/gut.28.5.527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borody T. J., George L. L., Brandl S., Andrews P., Ostapowicz N., Hyland L., Devine M. Helicobacter pylori-negative duodenal ulcer. Am J Gastroenterol. 1991 Sep;86(9):1154–1157. [PubMed] [Google Scholar]
- Coghlan J. G., Gilligan D., Humphries H., McKenna D., Dooley C., Sweeney E., Keane C., O'Morain C. Campylobacter pylori and recurrence of duodenal ulcers--a 12-month follow-up study. Lancet. 1987 Nov 14;2(8568):1109–1111. doi: 10.1016/s0140-6736(87)91545-5. [DOI] [PubMed] [Google Scholar]
- Collier D. S., Pain J. A. Non-steroidal anti-inflammatory drugs and peptic ulcer perforation. Gut. 1985 Apr;26(4):359–363. doi: 10.1136/gut.26.4.359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Horowitz J., Kukora J. S., Ritchie W. P., Jr All perforated ulcers are not alike. Ann Surg. 1989 Jun;209(6):693–697. doi: 10.1097/00000658-198906000-00006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Korman M. G., Hansky J., Eaves E. R., Schmidt G. T. Influence of cigarette smoking on healing and relapse in duodenal ulcer disease. Gastroenterology. 1983 Oct;85(4):871–874. [PubMed] [Google Scholar]
- Logan R. P., Polson R. J., Misiewicz J. J., Rao G., Karim N. Q., Newell D., Johnson P., Wadsworth J., Walker M. M., Baron J. H. Simplified single sample 13Carbon urea breath test for Helicobacter pylori: comparison with histology, culture, and ELISA serology. Gut. 1991 Dec;32(12):1461–1464. doi: 10.1136/gut.32.12.1461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lozano Polo J. L., Echevarría Vierna S., Casafont Morencos F., Ledesma Castaño F., Pons Romero F. Células natural killer (NK) e interleucina 2 (IL-2) en la enfermedad de Crohn. Rev Esp Enferm Dig. 1990 Aug;78(2):71–75. [PubMed] [Google Scholar]
- Marshall B. J., Goodwin C. S., Warren J. R., Murray R., Blincow E. D., Blackbourn S. J., Phillips M., Waters T. E., Sanderson C. R. Prospective double-blind trial of duodenal ulcer relapse after eradication of Campylobacter pylori. Lancet. 1988 Dec 24;2(8626-8627):1437–1442. doi: 10.1016/s0140-6736(88)90929-4. [DOI] [PubMed] [Google Scholar]
- McColl K. E., el-Nujumi A. M., Chittajallu R. S., Dahill S. W., Dorrian C. A., el-Omar E., Penman I., Fitzsimons E. J., Drain J., Graham H. A study of the pathogenesis of Helicobacter pylori negative chronic duodenal ulceration. Gut. 1993 Jun;34(6):762–768. doi: 10.1136/gut.34.6.762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Neithercut W. D., Milne A., Chittajallu R. S., el Nujumi A. M., McColl K. E. Detection of Helicobacter pylori infection of the gastric mucosa by measurement of gastric aspirate ammonium and urea concentrations. Gut. 1991 Sep;32(9):973–976. doi: 10.1136/gut.32.9.973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nensey Y. M., Schubert T. T., Bologna S. D., Ma C. K. Helicobacter pylori-negative duodenal ulcer. Am J Med. 1991 Jul;91(1):15–18. doi: 10.1016/0002-9343(91)90067-8. [DOI] [PubMed] [Google Scholar]
- el-Omar E., Penman I., Dorrian C. A., Ardill J. E., McColl K. E. Eradicating Helicobacter pylori infection lowers gastrin mediated acid secretion by two thirds in patients with duodenal ulcer. Gut. 1993 Aug;34(8):1060–1065. doi: 10.1136/gut.34.8.1060. [DOI] [PMC free article] [PubMed] [Google Scholar]



