Abstract
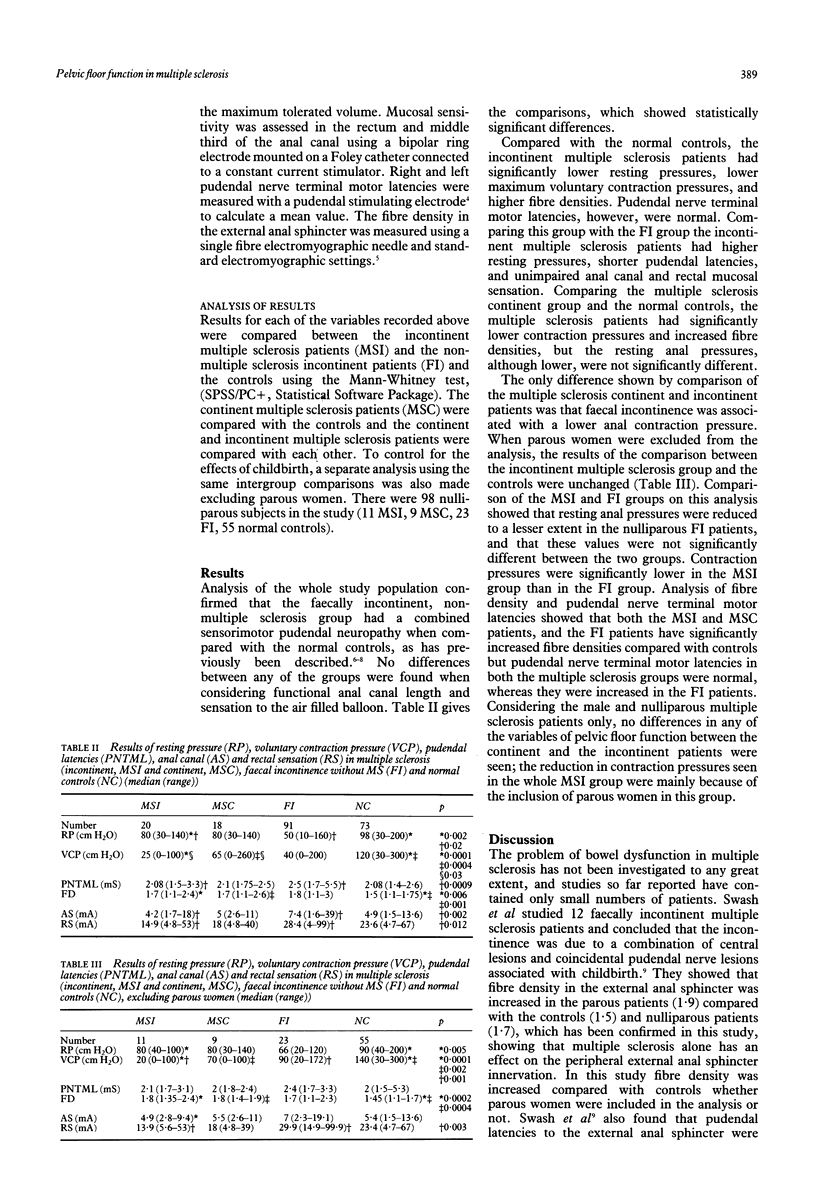
The aim of this study was to define pelvic floor function in patients with multiple sclerosis and bowel dysfunction, either incontinence (MSI) or defecation difficulties without incontinence (MSC). Normal controls and patients with idiopathic neurogenic faecal incontinence without multiple sclerosis (FI, disease controls) were also studied. Thirty eight multiple sclerosis patients (20 incontinent, 18 incontinent) 73 normal controls, and 91 FI patients were studied. The FI group showed the characteristic combined sensorimotor deficit previously described in these patients of low resting and voluntary contraction and pressures, increased sensory threshold to mucosal stimulation, and increased pudendal nerve terminal motor latencies and fibre densities. MSI patients had significantly lower anal resting pressures (80 (30-140) cm H2O, median (range) v 98 (30-200), normal controls, p = 0.002) and both MSC and MSI patients had significantly lower anal maximum voluntary contraction pressures (65 (0-260) cm H2O, MSC and 25 (0-100), MSI v 120 (30-300), normal controls, p = < 0.0004) and higher external anal sphincter fibre densities (1.7 (1.1-2.6), MSC and 1.7 (1.1-2.4), MSI v 1.5 (1.1-1.75), normal controls, p < 0.006) compared with normal controls but pudendal nerve terminal motor latencies were similar and no sensory deficit was found. This contrasted with the idiopathic faecal incontinent patients who, in addition to significantly higher fibre densities (1.8 (1.1-3), p = 0.001) had increased pudendal latencies (2.5 (1.1-5.5) mS v 2.08 (1.4-2.6), p = 0.001) compared with normal controls. The idiopathic faecal incontinent group had significantly lower resting anal pressures (50 (10-160) cm H2O, p=0.02) than the MSI group. Comparison with the incontinent and continent multiple sclerosis groups showed that incontinence was associated with lower voluntary anal contraction pressures (25 (0-100) v 65 (0-260), p=0.03) but that there were no other differences between these two groups. Pelvic floor function is considerably disturbed in multiple sclerosis, showing muscular weakness with preservation of peripheral motor nerve conduction, providing indirect evidence that this is mainly a result of lesions within the central nervous system.
Full text
PDF

Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Bielefeldt K., Enck P., Erckenbrecht J. F. Sensory and motor function in the maintenance of anal continence. Dis Colon Rectum. 1990 Aug;33(8):674–678. doi: 10.1007/BF02150743. [DOI] [PubMed] [Google Scholar]
- Caruana B. J., Wald A., Hinds J. P., Eidelman B. H. Anorectal sensory and motor function in neurogenic fecal incontinence. Comparison between multiple sclerosis and diabetes mellitus. Gastroenterology. 1991 Feb;100(2):465–470. doi: 10.1016/0016-5085(91)90217-9. [DOI] [PubMed] [Google Scholar]
- Frenckner B., Euler C. V. Influence of pudendal block on the function of the anal sphincters. Gut. 1975 Jun;16(6):482–489. doi: 10.1136/gut.16.6.482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glick M. E., Meshkinpour H., Haldeman S., Bhatia N. N., Bradley W. E. Colonic dysfunction in multiple sclerosis. Gastroenterology. 1982 Nov;83(5):1002–1007. [PubMed] [Google Scholar]
- Hinds J. P., Eidelman B. H., Wald A. Prevalence of bowel dysfunction in multiple sclerosis. A population survey. Gastroenterology. 1990 Jun;98(6):1538–1542. doi: 10.1016/0016-5085(90)91087-m. [DOI] [PubMed] [Google Scholar]
- Kiff E. S., Swash M. Normal proximal and delayed distal conduction in the pudendal nerves of patients with idiopathic (neurogenic) faecal incontinence. J Neurol Neurosurg Psychiatry. 1984 Aug;47(8):820–823. doi: 10.1136/jnnp.47.8.820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kiff E. S., Swash M. Slowed conduction in the pudendal nerves in idiopathic (neurogenic) faecal incontinence. Br J Surg. 1984 Aug;71(8):614–616. doi: 10.1002/bjs.1800710817. [DOI] [PubMed] [Google Scholar]
- MILLER H., SIMPSON C. A., YEATES W. K. BLADDER DYSFUNCTION IN MULTIPLE SCLEROSIS. Br Med J. 1965 May 15;1(5445):1265–1269. doi: 10.1136/bmj.1.5445.1265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller R., Bartolo D. C., Cervero F., Mortensen N. J. Differences in anal sensation in continent and incontinent patients with perineal descent. Int J Colorectal Dis. 1989;4(1):45–49. doi: 10.1007/BF01648550. [DOI] [PubMed] [Google Scholar]
- Neill M. E., Swash M. Increased motor unit fibre density in the external anal sphincter muscle in ano-rectal incontinence: a single fibre EMG study. J Neurol Neurosurg Psychiatry. 1980 Apr;43(4):343–347. doi: 10.1136/jnnp.43.4.343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Poser C. M., Paty D. W., Scheinberg L., McDonald W. I., Davis F. A., Ebers G. C., Johnson K. P., Sibley W. A., Silberberg D. H., Tourtellotte W. W. New diagnostic criteria for multiple sclerosis: guidelines for research protocols. Ann Neurol. 1983 Mar;13(3):227–231. doi: 10.1002/ana.410130302. [DOI] [PubMed] [Google Scholar]
- Rogers J., Henry M. M., Misiewicz J. J. Combined sensory and motor deficit in primary neuropathic faecal incontinence. Gut. 1988 Jan;29(1):5–9. doi: 10.1136/gut.29.1.5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Speakman C. T., Kamm M. A. The internal and sphincter--new insights into faecal incontinence. Gut. 1991 Apr;32(4):345–346. doi: 10.1136/gut.32.4.345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Swash M., Snooks S. J., Chalmers D. H. Parity as a factor in incontinence in multiple sclerosis. Arch Neurol. 1987 May;44(5):504–508. doi: 10.1001/archneur.1987.00520170034018. [DOI] [PubMed] [Google Scholar]
- Weber J., Grise P., Roquebert M., Hellot M. F., Mihout B., Samson M., Beuret-Blanquart F., Pasquis P., Denis P. Radiopaque markers transit and anorectal manometry in 16 patients with multiple sclerosis and urinary bladder dysfunction. Dis Colon Rectum. 1987 Feb;30(2):95–100. doi: 10.1007/BF02554940. [DOI] [PubMed] [Google Scholar]


