Abstract
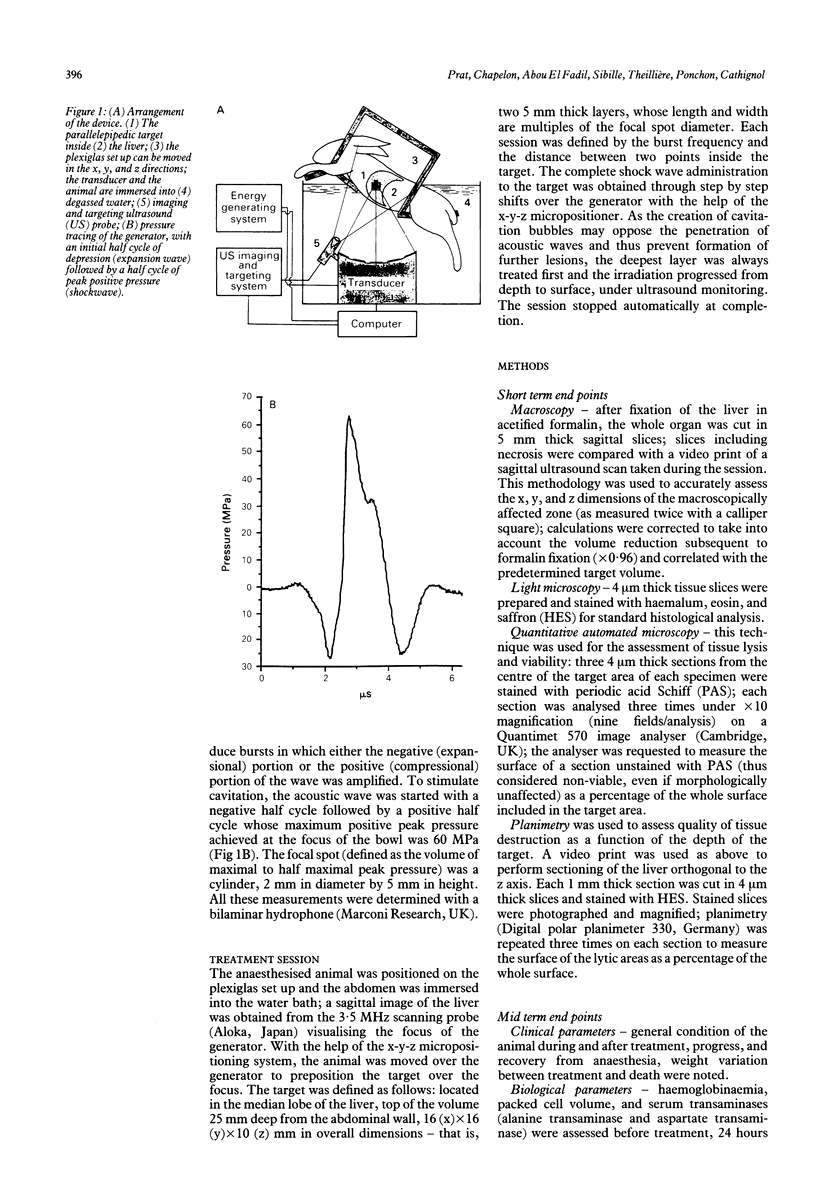
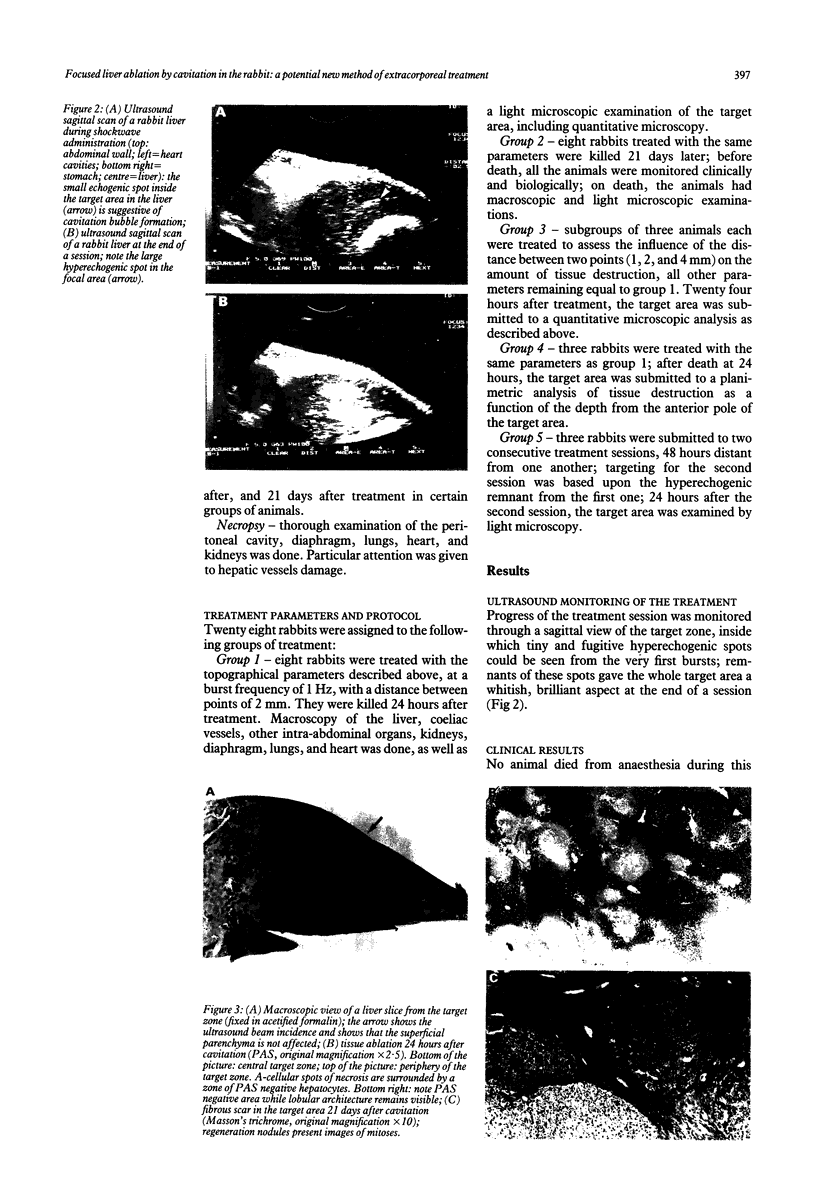
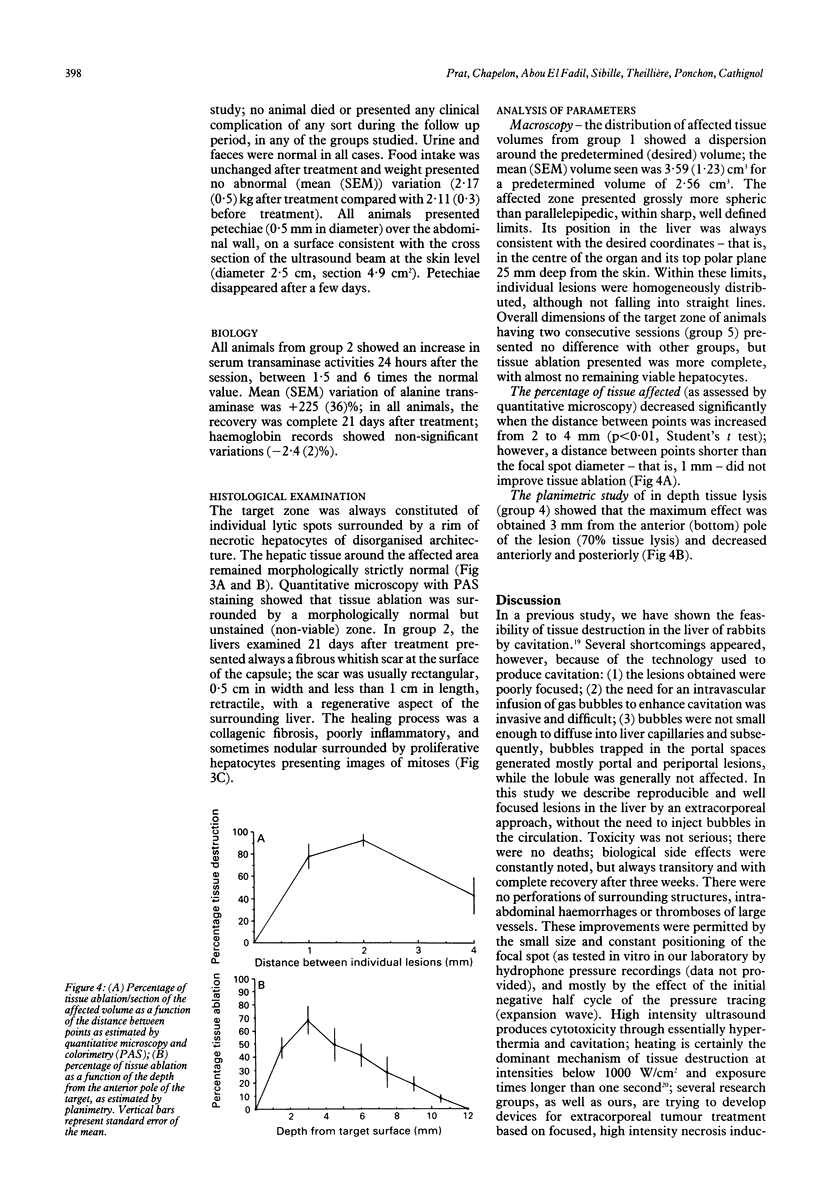
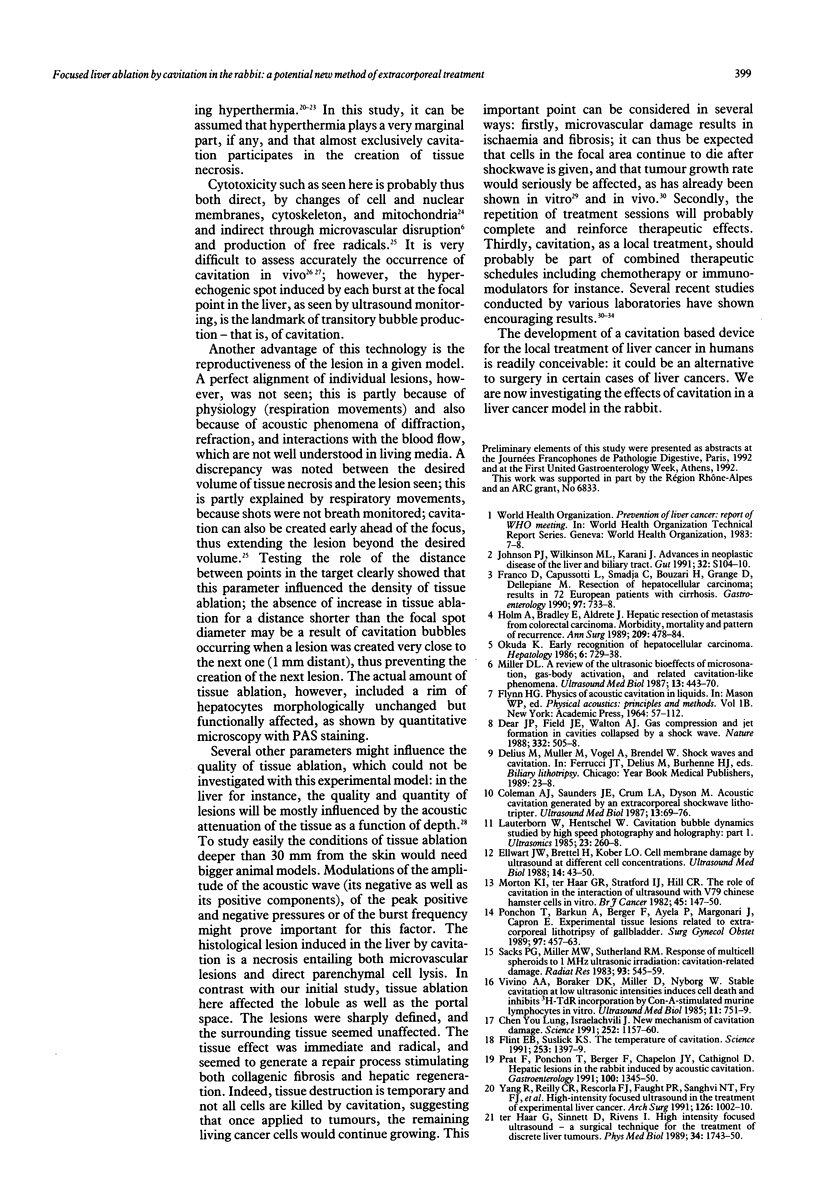
A new device was used to achieve focused tissue ablation by shockwave induced cavitation. The device produced a half cycle of negative pressure followed by a shock wave, thus enhancing cavitation. Twenty eight New Zealand rabbits were treated. Therapeutic ultrasound was targeted at the centre of the liver under ultrasound guidance. The focal volume was scanned with a computer operated x-y-z micropositioner. The number and frequency of bursts as well as the distance between two x-y-z displacements were preselected. The relation of tissue ablation seen to preselected parameters, effects on surrounding tissues, biological side effects, and mode of healing were studied. Macroscopy, planimetry, and quantitative microscopy were used. Focused and homogeneous tissue ablation was achieved within well defined limits. Maximal tissue ablation was seen in the centre of the target. Liver surrounding the target remained unaffected. Lesions were made of a-cellular spots surrounded by disorganised rims of necrotic hepatocytes; 24 hours after treatment, the changes (mean (SEM)) in alanine transaminase and haemoglobin were +225 (36)% and -2.4 (2)% respectively. Serum transaminases, haemoglobinaemia, and packed cell volume were normal 21 days after treatment and the target area was replaced by a fibrous scar. It is concluded that ultrasound cavitation may achieve extracorporeal intrahepatic tissue ablation inside a predetermined target. This technique should now be tested in an animal hepatic tumour model.
Full text
PDF

Images in this article
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Chapelon J. Y., Margonari J., Vernier F., Gorry F., Ecochard R., Gelet A. In vivo effects of high-intensity ultrasound on prostatic adenocarcinoma Dunning R3327. Cancer Res. 1992 Nov 15;52(22):6353–6357. [PubMed] [Google Scholar]
- Coleman A. J., Saunders J. E. A review of the physical properties and biological effects of the high amplitude acoustic field used in extracorporeal lithotripsy. Ultrasonics. 1993;31(2):75–89. doi: 10.1016/0041-624x(93)90037-z. [DOI] [PubMed] [Google Scholar]
- Coleman A. J., Saunders J. E., Crum L. A., Dyson M. Acoustic cavitation generated by an extracorporeal shockwave lithotripter. Ultrasound Med Biol. 1987 Feb;13(2):69–76. doi: 10.1016/0301-5629(87)90076-7. [DOI] [PubMed] [Google Scholar]
- Edmonds P. D., Ross P. Acoustic emission as a measure of exposure of suspended cells in vitro. Ultrasound Med Biol. 1986 Apr;12(4):297–305. doi: 10.1016/0301-5629(86)90339-x. [DOI] [PubMed] [Google Scholar]
- Ellwart J. W., Brettel H., Kober L. O. Cell membrane damage by ultrasound at different cell concentrations. Ultrasound Med Biol. 1988;14(1):43–50. doi: 10.1016/0301-5629(88)90162-7. [DOI] [PubMed] [Google Scholar]
- Flint E. B., Suslick K. S. The temperature of cavitation. Science. 1991 Sep 20;253(5026):1397–1399. doi: 10.1126/science.253.5026.1397. [DOI] [PubMed] [Google Scholar]
- Franco D., Capussotti L., Smadja C., Bouzari H., Meakins J., Kemeny F., Grange D., Dellepiane M. Resection of hepatocellular carcinomas. Results in 72 European patients with cirrhosis. Gastroenterology. 1990 Mar;98(3):733–738. [PubMed] [Google Scholar]
- Frizzell L. A., Linke C. A., Carstensen E. L., Fridd C. W. Thresholds for focal ultrasonic lesions in rabbit kidney, liver, and testicle. IEEE Trans Biomed Eng. 1977 Jul;24(4):393–396. doi: 10.1109/TBME.1977.326151. [DOI] [PubMed] [Google Scholar]
- Fry F. J., Reilly C. R., Dines K. A., Etchison M. R., Trauner E. J. Absorption in liver at the focus of an ultrasonic shock wave field. Ultrasound Med Biol. 1991;17(1):65–69. doi: 10.1016/0301-5629(91)90010-t. [DOI] [PubMed] [Google Scholar]
- Gambihler S., Delius M., Brendel W. Biological effects of shock waves: cell disruption, viability, and proliferation of L1210 cells exposed to shock waves in vitro. Ultrasound Med Biol. 1990;16(6):587–594. doi: 10.1016/0301-5629(90)90024-7. [DOI] [PubMed] [Google Scholar]
- Miller D. L. A review of the ultrasonic bioeffects of microsonation, gas-body activation, and related cavitation-like phenomena. Ultrasound Med Biol. 1987 Aug;13(8):443–470. doi: 10.1016/0301-5629(87)90110-4. [DOI] [PubMed] [Google Scholar]
- Morton K. I., ter Haar G. R., Stratford I. J., Hill C. R. The role of cavitation in the interaction of ultrasound with V79 Chinese hamster cells in vitro. Br J Cancer Suppl. 1982 Mar;5:147–150. [PMC free article] [PubMed] [Google Scholar]
- Okuda K. Early recognition of hepatocellular carcinoma. Hepatology. 1986 Jul-Aug;6(4):729–738. doi: 10.1002/hep.1840060432. [DOI] [PubMed] [Google Scholar]
- Prat F., Chapelon J. Y., Chauffert B., Ponchon T., Cathignol D. Cytotoxic effects of acoustic cavitation on HT-29 cells and a rat peritoneal carcinomatosis in vitro. Cancer Res. 1991 Jun 1;51(11):3024–3029. [PubMed] [Google Scholar]
- Prat F., Ponchon T., Berger F., Chapelon J. Y., Gagnon P., Cathignol D. Hepatic lesions in the rabbit induced by acoustic cavitation. Gastroenterology. 1991 May;100(5 Pt 1):1345–1350. [PubMed] [Google Scholar]
- Russo P., Stephenson R. A., Mies C., Huryk R., Heston W. D., Melamed M. R., Fair W. R. High energy shock waves suppress tumor growth in vitro and in vivo. J Urol. 1986 Mar;135(3):626–628. doi: 10.1016/s0022-5347(17)45764-8. [DOI] [PubMed] [Google Scholar]
- Sacks P. G., Miller M. W., Sutherland R. M. Response of multicell spheroids to 1-MHz ultrasonic irradiation: cavitation-related damage. Radiat Res. 1983 Mar;93(3):545–559. [PubMed] [Google Scholar]
- Steinbach P., Hofstädter F., Nicolai H., Rössler W., Wieland W. In vitro investigations on cellular damage induced by high energy shock waves. Ultrasound Med Biol. 1992;18(8):691–699. doi: 10.1016/0301-5629(92)90120-y. [DOI] [PubMed] [Google Scholar]
- Vivino A. A., Boraker D. K., Miller D., Nyborg W. Stable cavitation at low ultrasonic intensities induces cell death and inhibits 3H-TdR incorporation by Con-A-stimulated murine lymphocytes in vitro. Ultrasound Med Biol. 1985 Sep-Oct;11(5):751–759. doi: 10.1016/0301-5629(85)90109-7. [DOI] [PubMed] [Google Scholar]
- Warlters A., Morris D. L., Cameron-Strange A., Lynch W. Effect of electrohydraulic and extracorporeal shock waves on gastrointestinal cancer cells and their response to cytotoxic agents. Gut. 1992 Jun;33(6):791–793. doi: 10.1136/gut.33.6.791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weiss N., Delius M., Gambihler S., Dirschedl P., Goetz A., Brendel W. Influence of the shock wave application mode on the growth of A-Mel 3 and SSK2 tumors in vivo. Ultrasound Med Biol. 1990;16(6):595–605. doi: 10.1016/0301-5629(90)90025-8. [DOI] [PubMed] [Google Scholar]
- Williams A. R., Delius M., Miller D. L., Schwarze W. Investigation of cavitation in flowing media by lithotripter shock waves both in vitro and in vivo. Ultrasound Med Biol. 1989;15(1):53–60. doi: 10.1016/0301-5629(89)90132-4. [DOI] [PubMed] [Google Scholar]
- Yang R., Reilly C. R., Rescorla F. J., Faught P. R., Sanghvi N. T., Fry F. J., Franklin T. D., Jr, Lumeng L., Grosfeld J. L. High-intensity focused ultrasound in the treatment of experimental liver cancer. Arch Surg. 1991 Aug;126(8):1002–1010. doi: 10.1001/archsurg.1991.01410320088012. [DOI] [PubMed] [Google Scholar]
- ter Haar G., Sinnett D., Rivens I. High intensity focused ultrasound--a surgical technique for the treatment of discrete liver tumours. Phys Med Biol. 1989 Nov;34(11):1743–1750. doi: 10.1088/0031-9155/34/11/021. [DOI] [PubMed] [Google Scholar]