Abstract
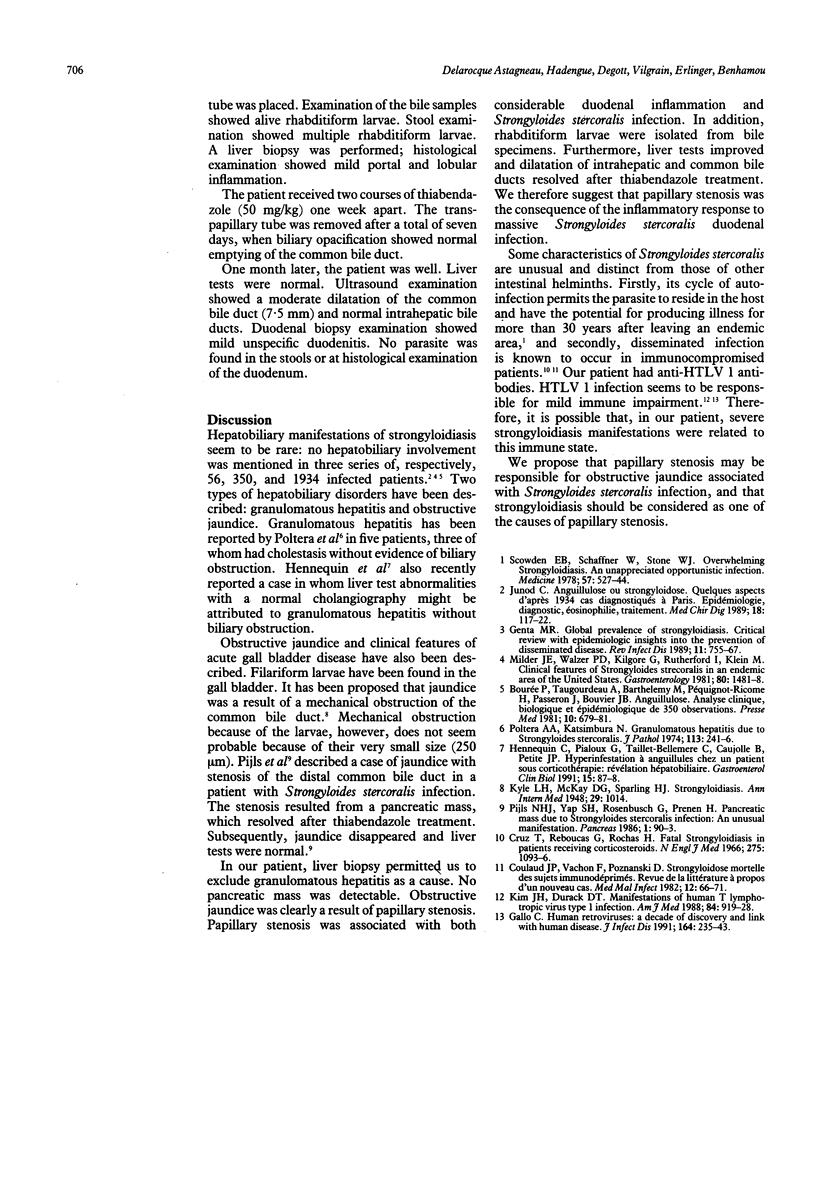
Hepatobiliary manifestations of strongyloidiasis are rare. A case is described of biliary obstruction associated with the presence of Strongyloides stercoralis in the duodenal mucosa and 250 microns rhabditiform larvae in bile. Biliary obstruction resulted from papillary stenosis, which resolved after treatment with thiabendazole. It is proposed that papillary stenosis may be responsible for obstructive jaundice associated with Strongyloides stercoralis infection, and that strongyloidiasis should be added to the causes of papillary stenosis.
Full text
PDF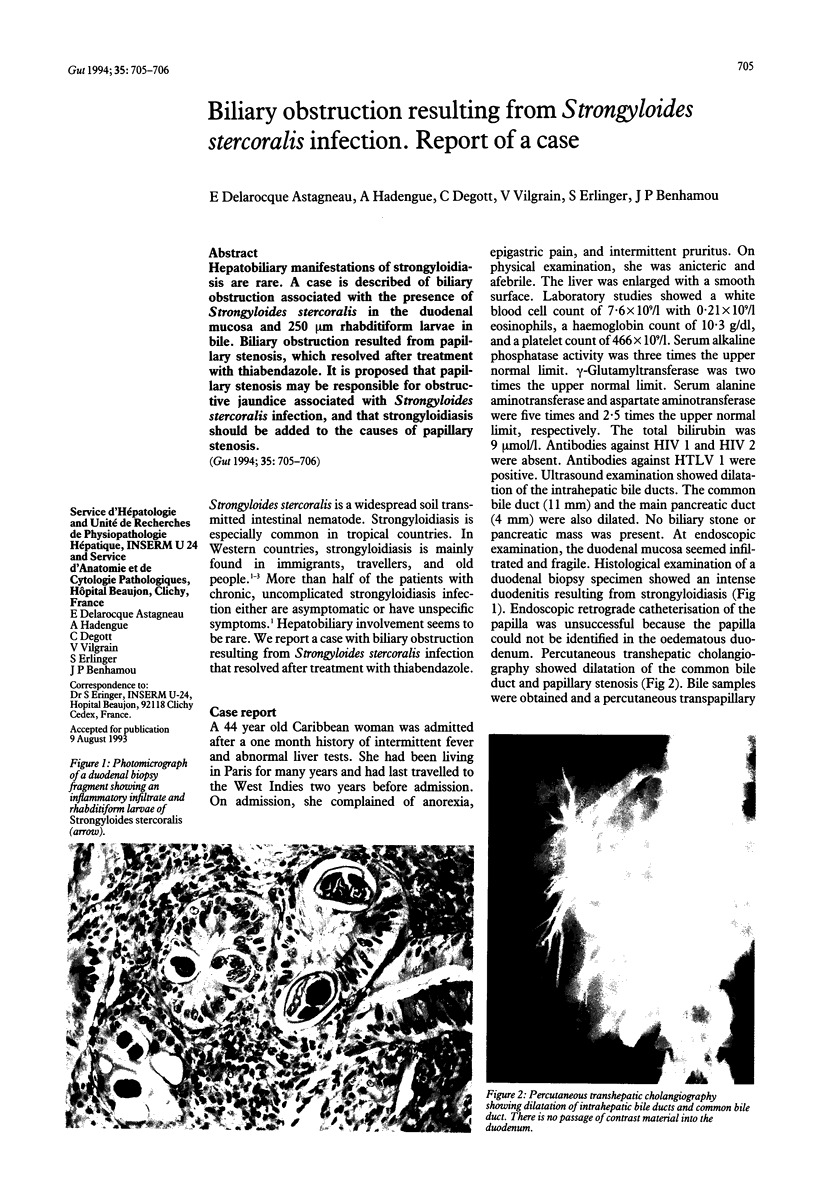
Images in this article
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Bourée P., Taugourdeau A., Barthelémy M., Pequignot-Ricome H., Passeron J., Bouvier J. B. Anguillulose: analyse clinique, biologique et épidémiologique de 350 observations. Nouv Presse Med. 1981 Feb 28;10(9):679–681. [PubMed] [Google Scholar]
- Cruz T., Reboucas G., Rocha H. Fatal strongyloidiasis in patients receiving corticosteroids. N Engl J Med. 1966 Nov 17;275(20):1093–1096. doi: 10.1056/NEJM196611172752003. [DOI] [PubMed] [Google Scholar]
- Gallo R. C. Human retroviruses: a decade of discovery and link with human disease. J Infect Dis. 1991 Aug;164(2):235–243. doi: 10.1093/infdis/164.2.235. [DOI] [PubMed] [Google Scholar]
- Genta R. M. Global prevalence of strongyloidiasis: critical review with epidemiologic insights into the prevention of disseminated disease. Rev Infect Dis. 1989 Sep-Oct;11(5):755–767. doi: 10.1093/clinids/11.5.755. [DOI] [PubMed] [Google Scholar]
- Hennequin C., Pialoux G., Taillet-Bellemere C., Caujolle B., Petite J. P. Hyperinfestation à anguillules chez un patient sous corticothérapie: révélation hépato-biliaire. Gastroenterol Clin Biol. 1991;15(1):87–88. [PubMed] [Google Scholar]
- Kim J. H., Durack D. T. Manifestations of human T-lymphotropic virus type I infection. Am J Med. 1988 May;84(5):919–928. doi: 10.1016/0002-9343(88)90072-1. [DOI] [PubMed] [Google Scholar]
- Milder J. E., Walzer P. D., Kilgore G., Rutherford I., Klein M. Clinical features of Strongyloides stercoralis infection in an endemic area of the United States. Gastroenterology. 1981 Jun;80(6):1481–1488. [PubMed] [Google Scholar]
- Pijls N. H., Yap S. H., Rosenbusch G., Prenen H. Pancreatic mass due to Strongyloides stercoralis infection: an unusual manifestation. Pancreas. 1986;1(1):90–93. doi: 10.1097/00006676-198601000-00016. [DOI] [PubMed] [Google Scholar]
- Poltera A. A., Katsimbura N. Granulomatous hepatitis due to Strongyloides stercoralis. J Pathol. 1974 Aug;113(4):241–246. doi: 10.1002/path.1711130408. [DOI] [PubMed] [Google Scholar]
- Scowden E. B., Schaffner W., Stone W. J. Overwhelming strongyloidiasis: an unappreciated opportunistic infection. Medicine (Baltimore) 1978 Nov;57(6):527–544. [PubMed] [Google Scholar]