Abstract
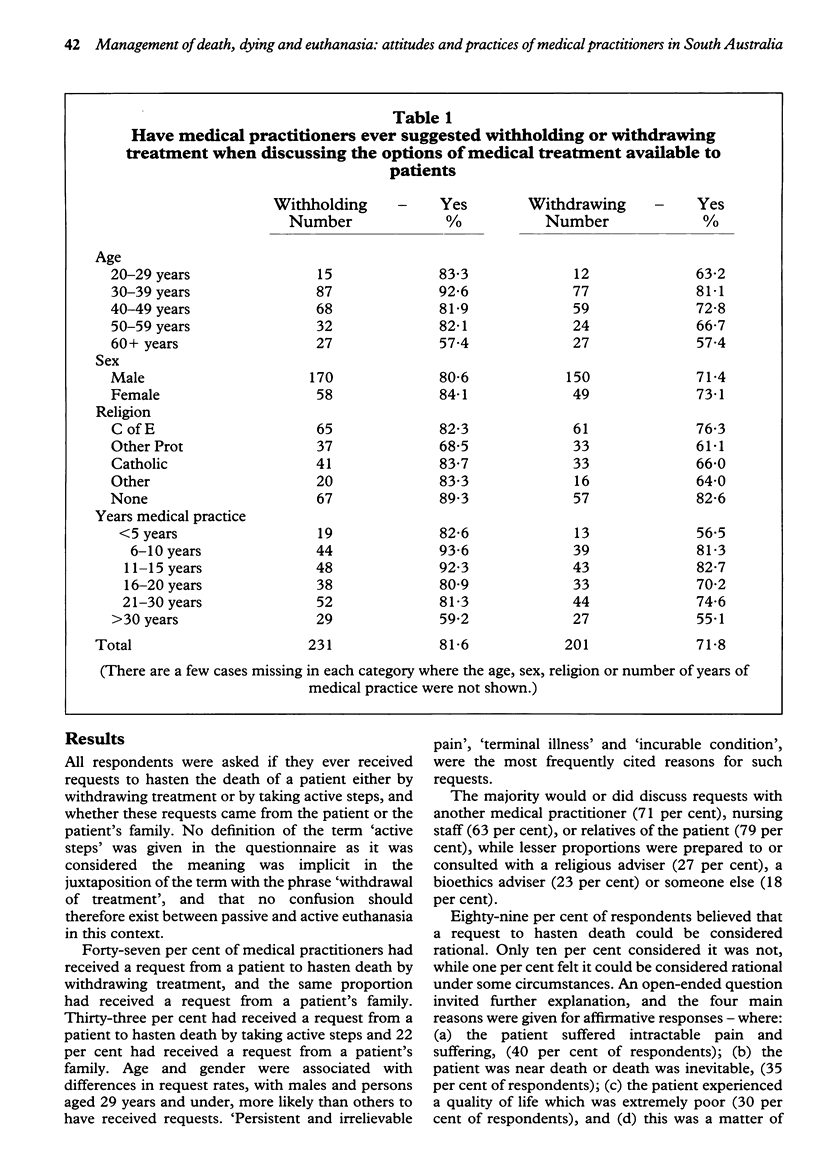
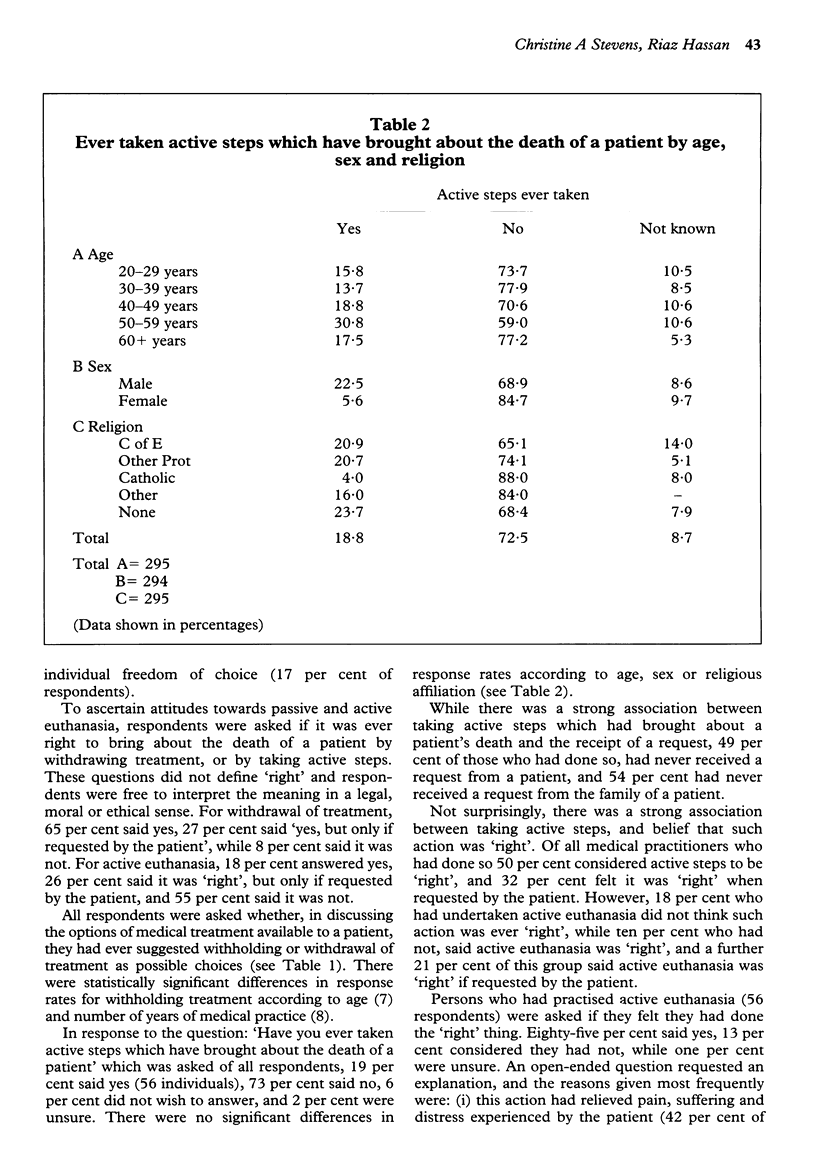
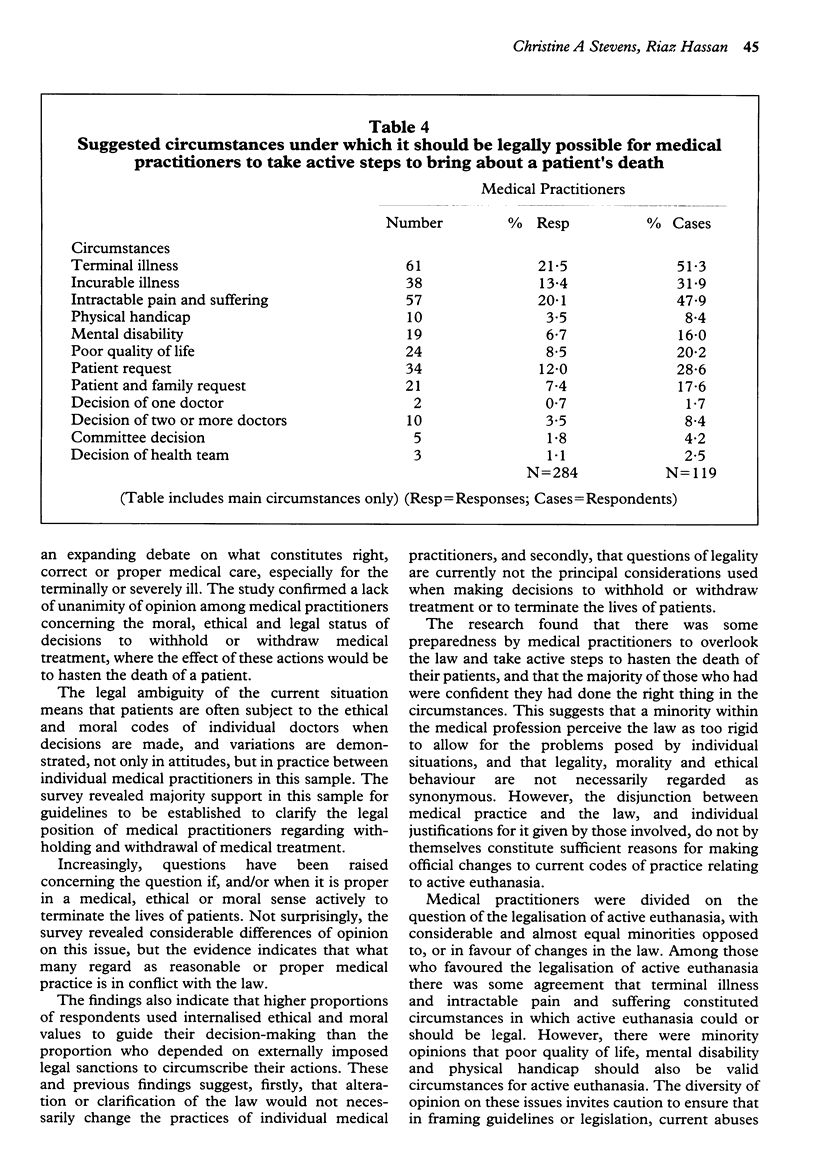
This article presents the first results of a study of the decisions made by health professionals in South Australia concerning the management of death, dying, and euthanasia, and focuses on the findings concerning the attitudes and practices of medical practitioners. Mail-back, self-administered questionnaires were posted in August 1991 to a ten per cent sample of 494 medical practitioners in South Australia randomly selected from the list published by the Medical Board of South Australia. A total response rate of 68 per cent was obtained, 60 per cent of which (298) were usable returns. It was found that forty-seven per cent had received requests from patients to hasten their deaths. Nineteen per cent had taken active steps which had brought about the death of a patient. Sixty-eight per cent thought that guidelines for withholding and withdrawal of treatment should be established. Forty-five per cent were in favour of legalisation of active euthanasia under certain circumstances.
Full text
PDF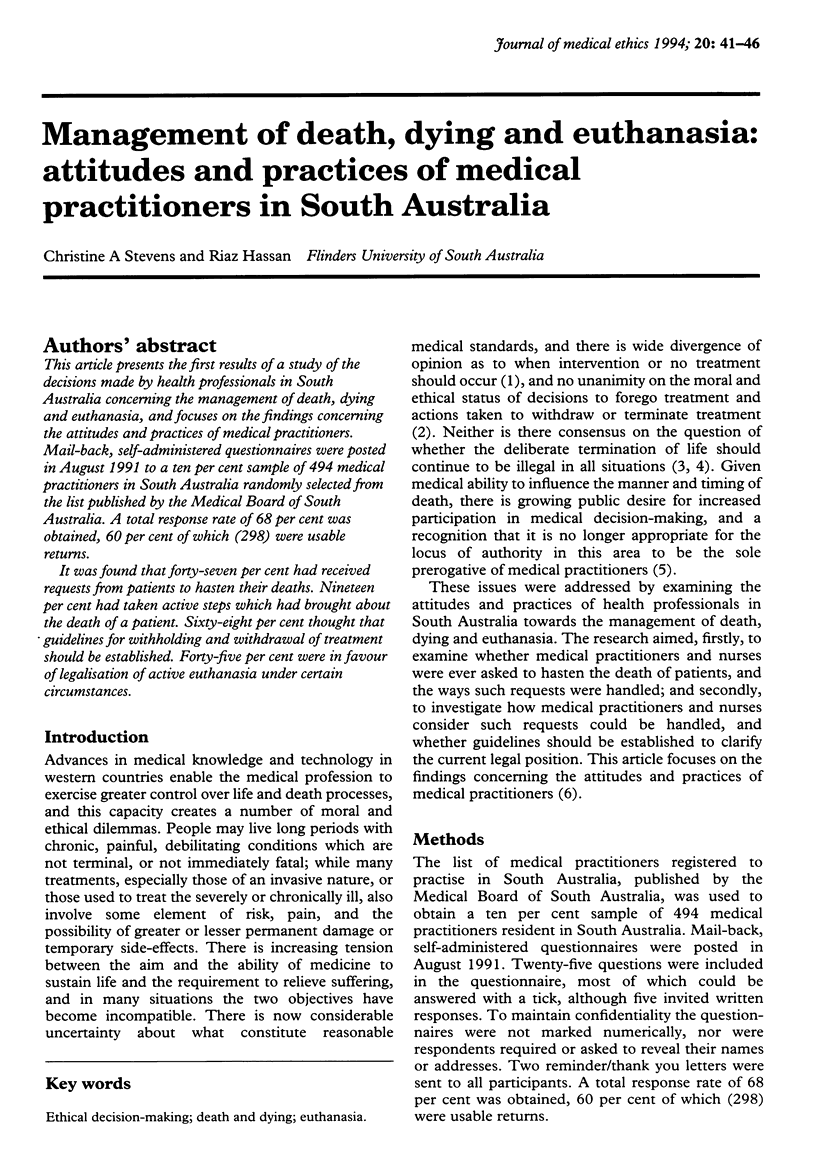
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Davies J. Raping and making love are different concepts: so are killing and voluntary euthanasia. J Med Ethics. 1988 Sep;14(3):148–149. doi: 10.1136/jme.14.3.148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gillon R. Euthanasia, withholding life-prolonging treatment, and moral differences between killing and letting die. J Med Ethics. 1988 Sep;14(3):115–117. doi: 10.1136/jme.14.3.115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Loewy E. H. Involving patients in do not resuscitate (DNR) decisions: an old issue raising its ugly head. J Med Ethics. 1991 Sep;17(3):156–160. doi: 10.1136/jme.17.3.156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parker M. Moral intuition, good deaths and ordinary medical practitioners. J Med Ethics. 1990 Mar;16(1):28–34. doi: 10.1136/jme.16.1.28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pollard B. J. Withdrawing life-sustaining treatment from severely brain-damaged persons. Med J Aust. 1991 Apr 15;154(8):559–561. doi: 10.5694/j.1326-5377.1991.tb119456.x. [DOI] [PubMed] [Google Scholar]
- Wanzer S. H., Federman D. D., Adelstein S. J., Cassel C. K., Cassem E. H., Cranford R. E., Hook E. W., Lo B., Moertel C. G., Safar P. The physician's responsibility toward hopelessly ill patients. A second look. N Engl J Med. 1989 Mar 30;320(13):844–849. doi: 10.1056/NEJM198903303201306. [DOI] [PubMed] [Google Scholar]


