Abstract
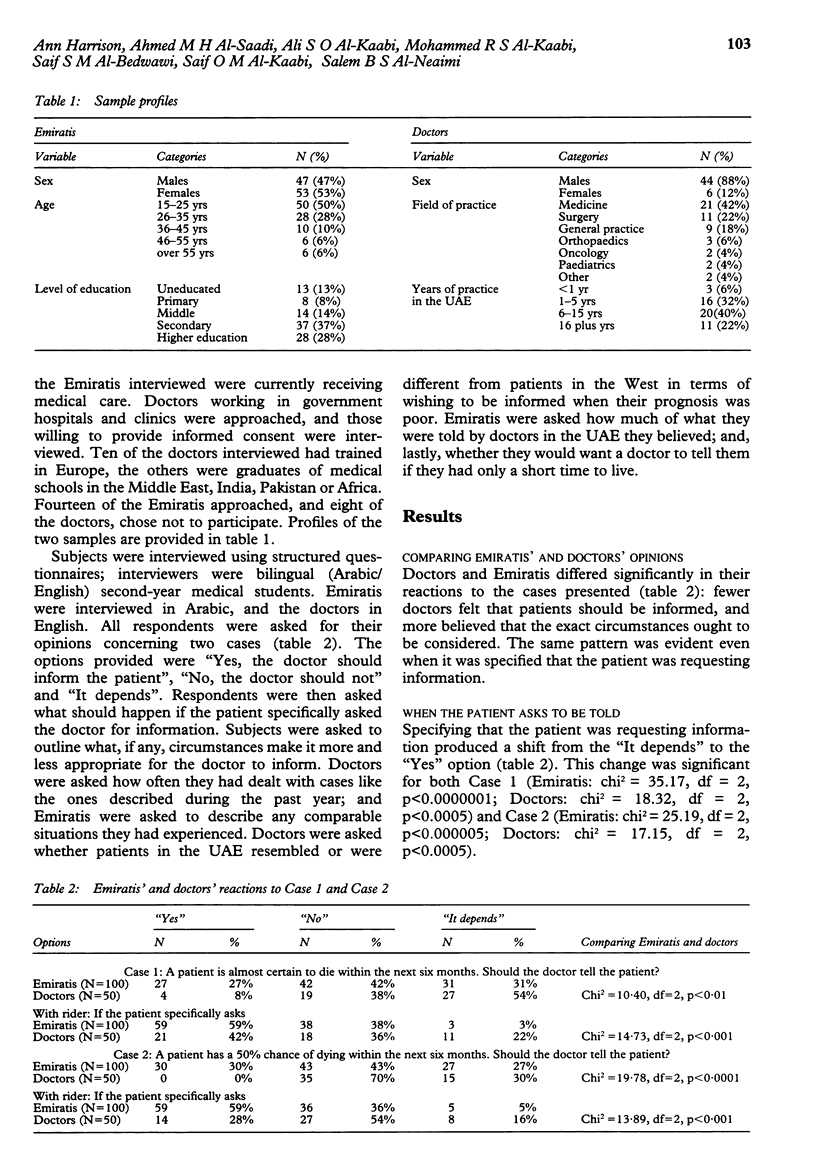
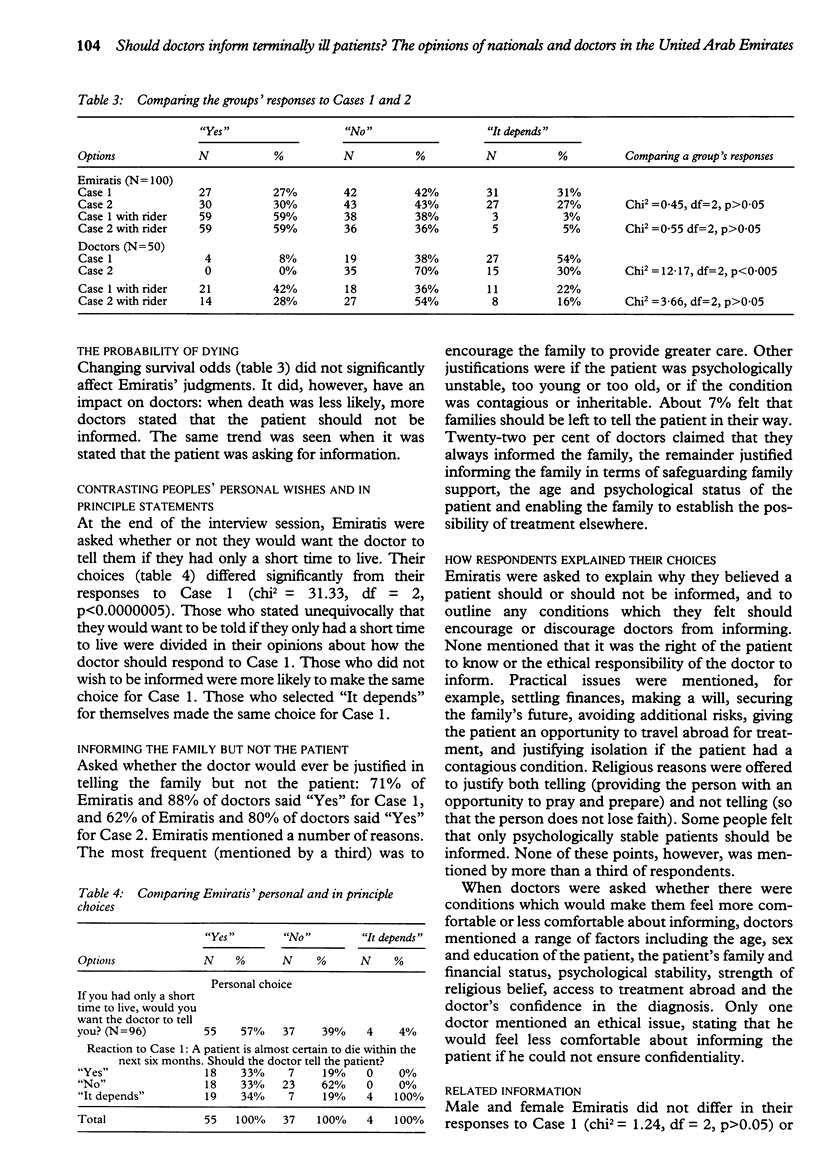
OBJECTIVES: To study the opinions of nationals (Emiratis) and doctors practising in the United Arab Emirates (UAE) with regard to informing terminally ill patients. DESIGN: Structured questionnaires administered during January 1995. SETTING: The UAE, a federation of small, rich, developing Arabian Gulf states. PARTICIPANTS: Convenience samples of 100 Emiratis (minimum age 15 years) and of 50 doctors practising in government hospitals and clinics. RESULTS: Doctors emerged as consistently less in favour of informing than the Emiratis were, whether the patient was described as almost certain to die during the next six months or as having a 50% chance of surviving, and even when it was specified that the patient was requesting information. In the latter situation, a third of doctors maintained that the patient should not be told. Increasing survival odds reduced the number of doctors selecting to inform; but it had no significant impact on Emiratis' choices. When Emiratis were asked whether they would personally want to be informed if they had only a short time to live, less than half responded in the way they had done to the in principle question. CONCLUSIONS: The doctors' responses are of concern because of the lack of reference to ethical principles or dilemmas, the disregard of patients' wishes and dependency on survival odds. The heterogeneity of Emiratis' responses calls into question the usefulness of invoking norms to explain inter-society differences. In the current study, people's in principle choices did not provide a useful guide to how they said they would personally wish to be treated.
Full text
PDF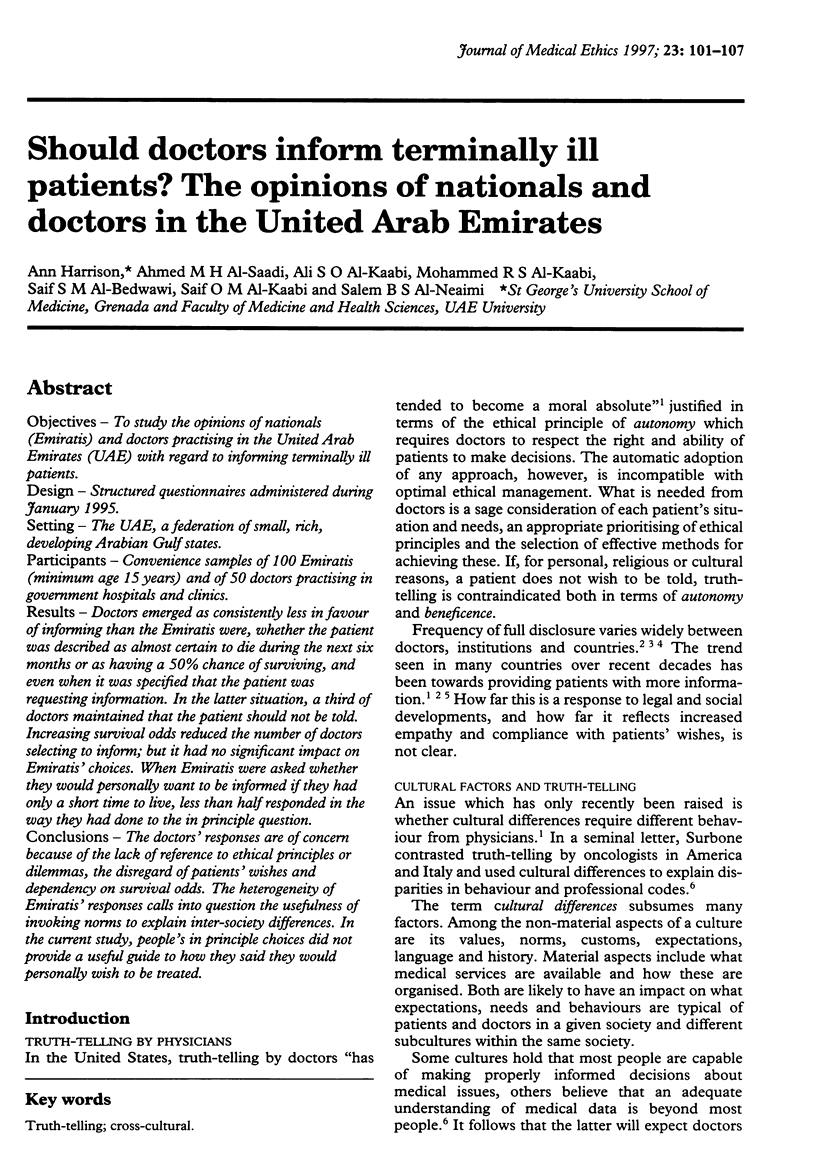
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Dalla-Vorgia P., Katsouyanni K., Garanis T. N., Touloumi G., Drogari P., Koutselinis A. Attitudes of a Mediterranean population to the truth-telling issue. J Med Ethics. 1992 Jun;18(2):67–74. doi: 10.1136/jme.18.2.67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liberati A., Mosconi P., Meyerowitz B. Truth telling: a cultural or individual choice? JAMA. 1993 Feb 24;269(8):989–989. [PubMed] [Google Scholar]
- McNeil B. J., Pauker S. G., Sox H. C., Jr, Tversky A. On the elicitation of preferences for alternative therapies. N Engl J Med. 1982 May 27;306(21):1259–1262. doi: 10.1056/NEJM198205273062103. [DOI] [PubMed] [Google Scholar]
- Newall D. J., Gadd E. M., Priestman T. J. Presentation of information to cancer patients: a comparison of two centres in the UK and USA. Br J Med Psychol. 1987 Jun;60(Pt 2):127–131. doi: 10.1111/j.2044-8341.1987.tb02722.x. [DOI] [PubMed] [Google Scholar]
- Pellegrino E. D. Is truth telling to the patient a cultural artifact? JAMA. 1992 Oct 7;268(13):1734–1735. [PubMed] [Google Scholar]
- Thomsen O. O., Wulff H. R., Martin A., Singer P. A. What do gastroenterologists in Europe tell cancer patients? Lancet. 1993 Feb 20;341(8843):473–476. doi: 10.1016/0140-6736(93)90218-6. [DOI] [PubMed] [Google Scholar]


