Abstract
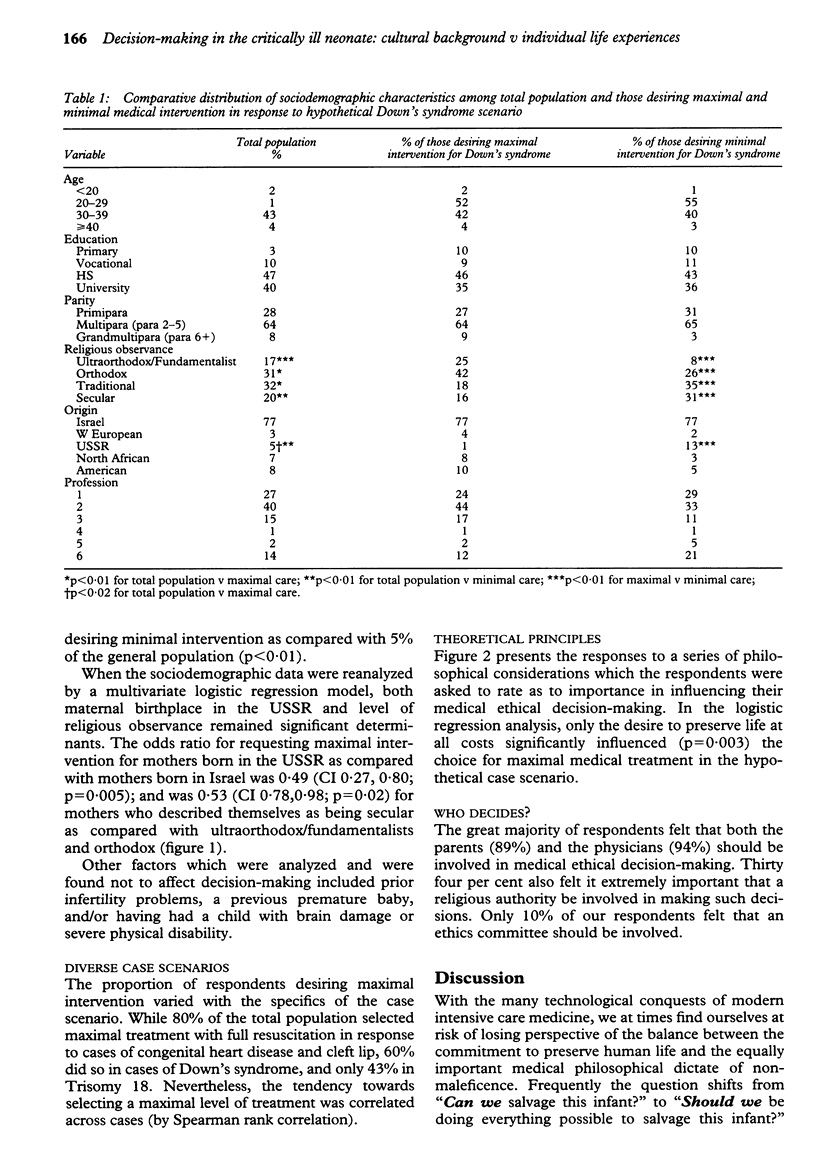
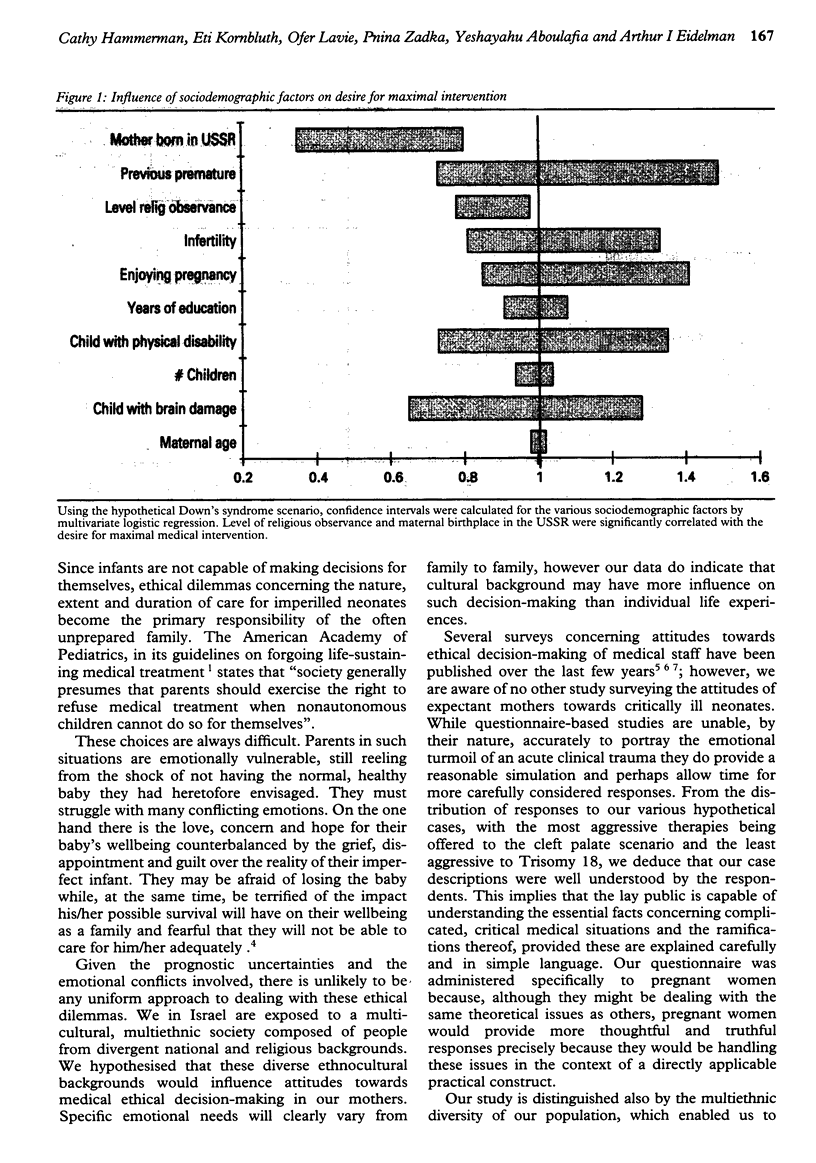
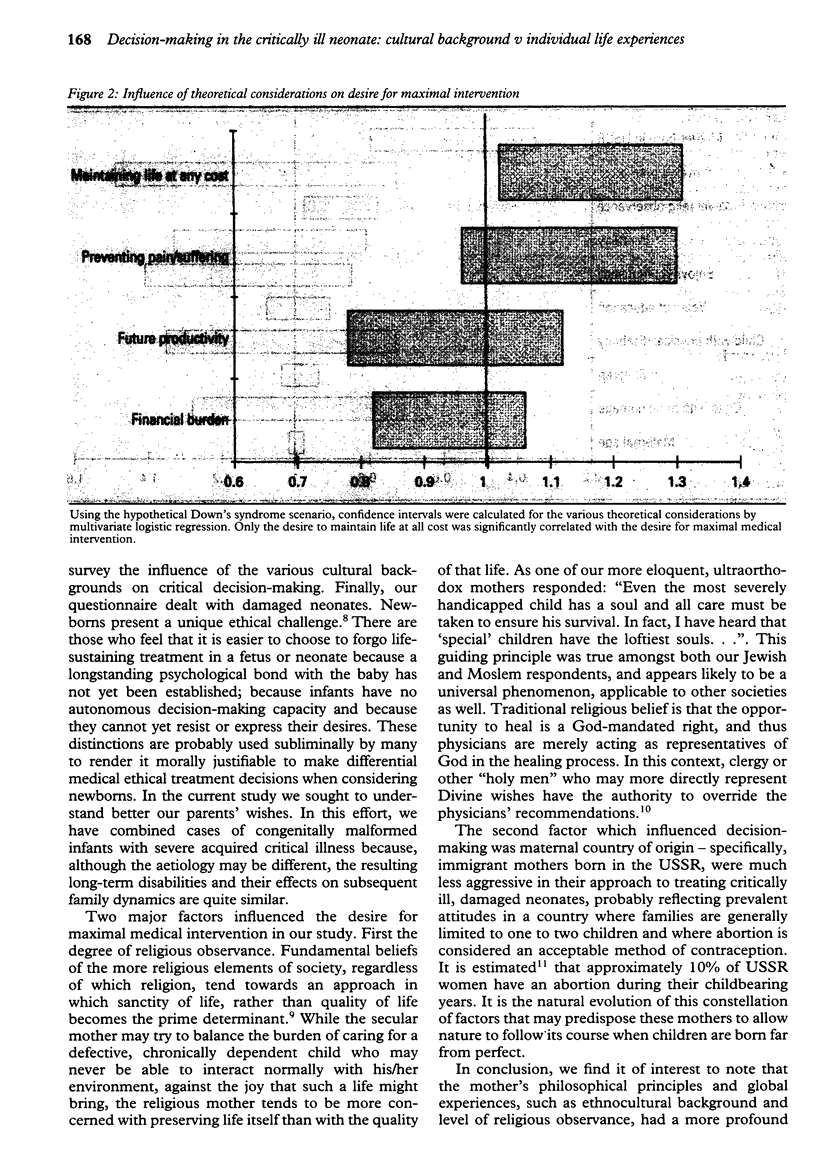
OBJECTIVES: In treating critically ill neonates, situations occasionally arise in which aggressive medical treatment prolongs the inevitable death rather than prolonging life. Decisions as to limitation of neonatal medical intervention remain controversial and the primary responsibility of the generally unprepared family. This research was designed to study response patterns of expectant mothers towards treatment of critically ill and/or malformed infants. DESIGN/SETTING: Attitudes were studied via comprehensive questionnaires divided into three sections: 1-Sociodemographic data and prior personal experience with perinatal problems; 2-Theoretical philosophical principles used in making medical ethical decisions; and 3-Hypothetical case scenarios with choices of treatment options. SUBJECTS AND RESULTS: Six hundred and fifty pregnant women were studied. Maternal birthplace (p = 0.005) and level of religious observance (p = 0.02) were strongly associated with the desire for maximally aggressive medical intervention in the hypothetical case scenario. Specific personal experiences such as infertility problems, previous children with serious mental or physical problems were not correlated with the selection of different treatment choices. Of the theoretical principles studied, only the desire to preserve life at all costs was significantly associated with the choice for maximal medical treatment (p = 0.003). CONCLUSIONS: Maternal ethnocultural background and philosophical principles more profoundly influenced medical ethical decision-making than did specific personal life experiences.
Full text
PDF
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Byrne P. J., Tyebkhan J. M., Laing L. M. Ethical decision-making and neonatal resuscitation. Semin Perinatol. 1994 Feb;18(1):36–41. [PubMed] [Google Scholar]
- Eidelman A. I. Caring for newborns: three world views. In Israel, families look to two messengers of God. Hastings Cent Rep. 1986 Aug;16(4):18–19. [PubMed] [Google Scholar]
- Harlap S., Davies A. M., Grover N. B., Prywes R. The Jerusalem perinatal study: the first decade 1964--73. Isr J Med Sci. 1977 Nov;13(11):1073–1091. [PubMed] [Google Scholar]
- Jakobovits I. Jewish medical ethics--a brief overview. J Med Ethics. 1983 Jun;9(2):109–112. doi: 10.1136/jme.9.2.109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rostain A. L., Bhutani V. K. Ethical dilemmas of neonatal--perinatal surgery. Clin Perinatol. 1989 Mar;16(1):275–302. [PubMed] [Google Scholar]
- Segal S. Ethical issues presented by children with congenital anomalies. Semin Perinatol. 1992 Dec;16(6):369–373. [PubMed] [Google Scholar]
- Steinberg A. Meningomyelocele in the neonate: medical and ethical considerations. J Perinatol. 1991 Mar;11(1):51–56. [PubMed] [Google Scholar]
- Todres I. D., Guillemin J., Grodin M. A., Batten D. Life-saving therapy for newborns: a questionnaire survey in the state of Massachusetts. Pediatrics. 1988 May;81(5):643–649. [PubMed] [Google Scholar]


