Abstract
Anorectal manometry with balloon distension was performed on 28 patients with diarrhoea predominant irritable bowel syndrome, 27 patients with constipation predominant irritable bowel syndrome and 30 normal controls. In the diarrhoea predominant group balloon volumes required to perceive the sensations of gas, stool, urgency of defecation and discomfort were significantly lower than in controls or constipation predominant patients (p less than 0.001). Diarrhoea predominant patients also had a significantly lower rectal compliance than controls or constipation predominant patients (p less than 0.03) but showed no difference in motor activity induced by distension. When the constipation predominant patients were compared with controls the only significant difference that emerged was in the volume at which discomfort was perceived. No significant differences between constipated subjects and controls were found in the distension induced motor activity. Symptom severity and psychological parameters were also recorded and the diarrhoea predominant patients were found to be more anxious than those with constipation (p = 0.04). It proved possible (by comparison with the control group) to identify three abnormal rectal subtypes in patients with irritable bowel syndrome. These were a sensitive rectum (low sensation thresholds, normal or low rectal pressure), a stiff rectum (normal or low sensation thresholds, high pressure) and an insensitive rectum (high sensation thresholds, normal or high pressure) and their distribution varied considerably depending on bowel habit. Some form of rectal abnormality was identified in 75% of diarrhoea predominant patients compared with 30% of constipation predominant subjects (p = 0.002). A sensitive rectum was a particular feature of diarrhoea predominant patients being observed in 57% of patients compared with only 7% of the constipated group (p less than 0.001).
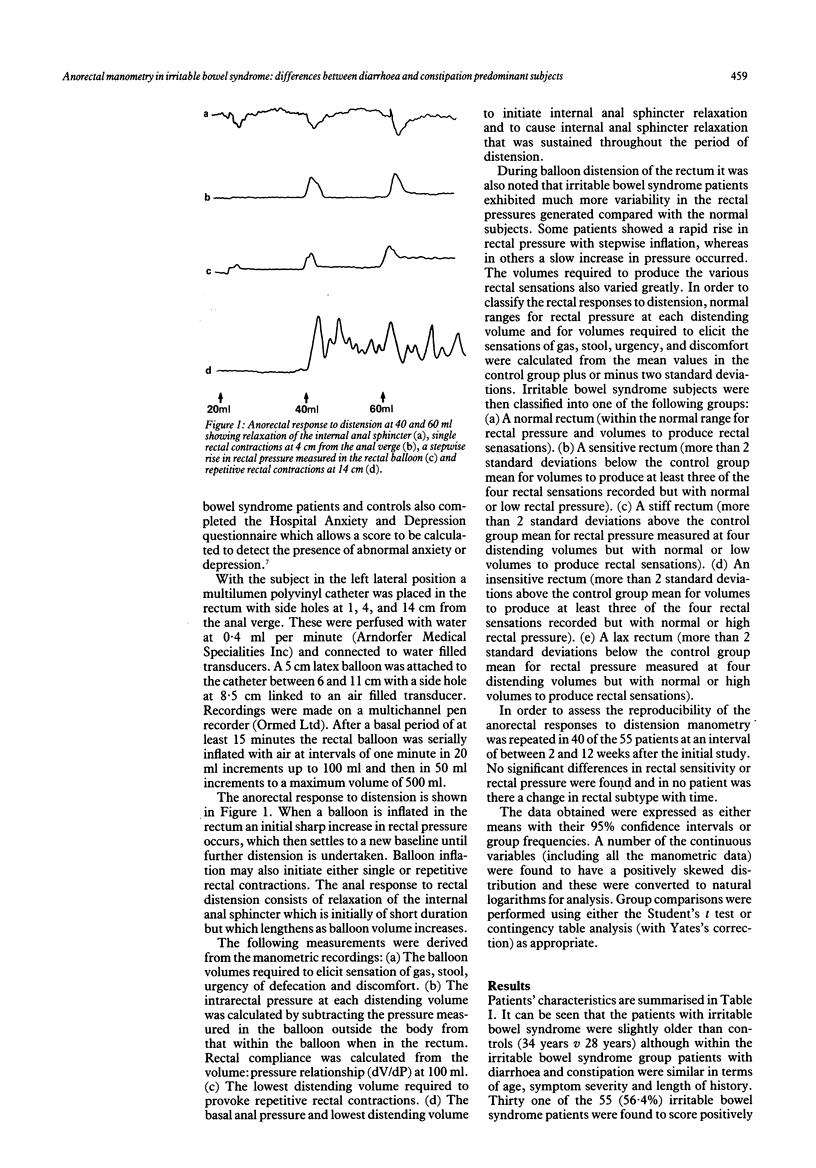
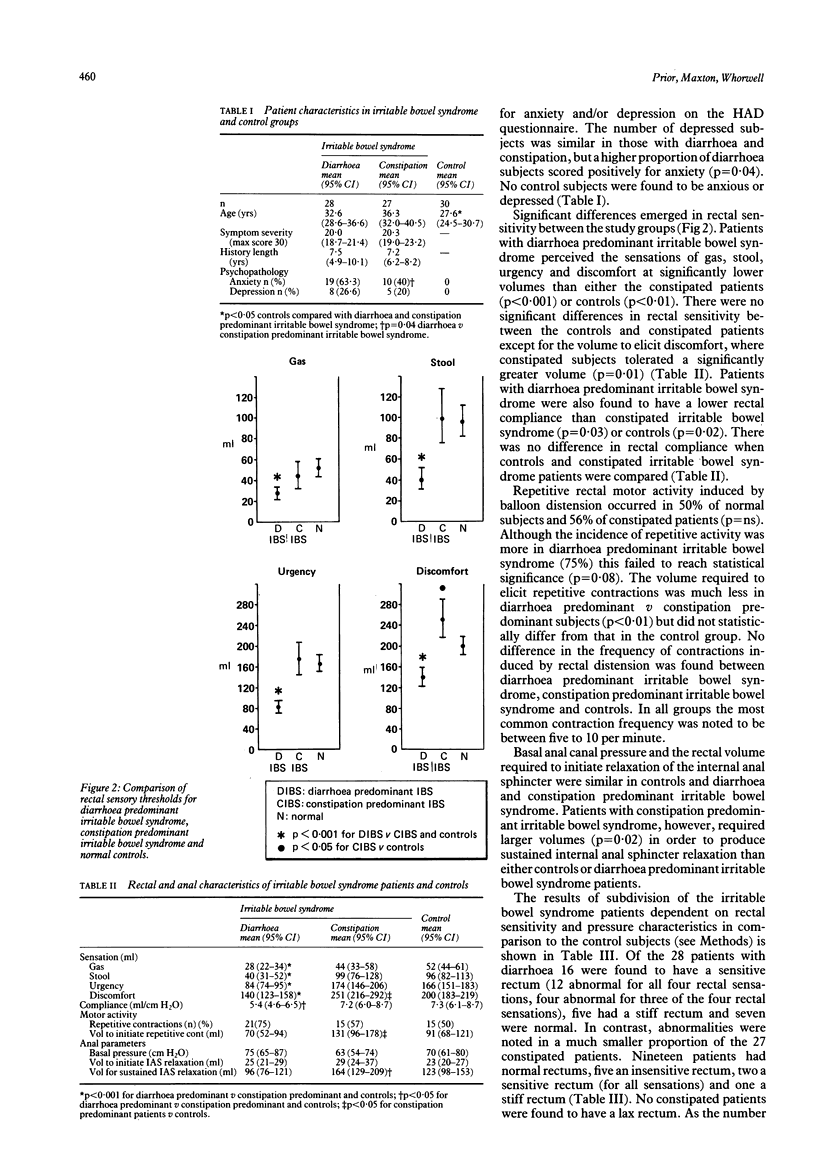
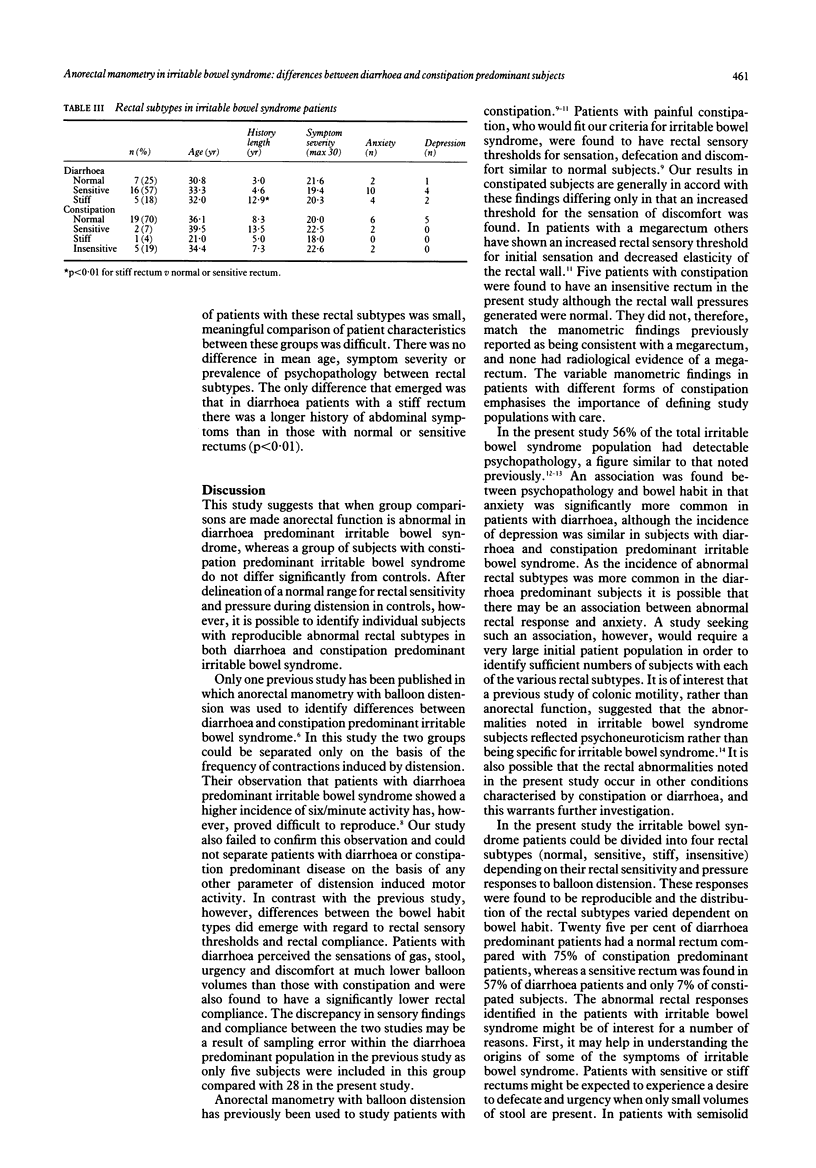
Full text
PDF

Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Bannister J. J., Davison P., Timms J. M., Gibbons C., Read N. W. Effect of stool size and consistency on defecation. Gut. 1987 Oct;28(10):1246–1250. doi: 10.1136/gut.28.10.1246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- CHAUDHARY N. A., TRUELOVE S. C. Human colonic motility: a comparative study of normal subjects, patients with ulcerative colitis, and patients with the irritable colon syndrome. II. The effect of prostigmin. Gastroenterology. 1961 Jan;40:18–26. [PubMed] [Google Scholar]
- Harvey R. F., Read A. E. Effect of cholecystokinin on colonic motility and symptoms in patients with the irritable-bowel syndrome. Lancet. 1973 Jan 6;1(7793):1–3. doi: 10.1016/s0140-6736(73)91219-1. [DOI] [PubMed] [Google Scholar]
- Hislop I. G. Psychological significance of the irritable colon syndrome. Gut. 1971 Jun;12(6):452–457. doi: 10.1136/gut.12.6.452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kellow J. E., Phillips S. F. Altered small bowel motility in irritable bowel syndrome is correlated with symptoms. Gastroenterology. 1987 Jun;92(6):1885–1893. doi: 10.1016/0016-5085(87)90620-2. [DOI] [PubMed] [Google Scholar]
- Kellow J. E., Phillips S. F., Miller L. J., Zinsmeister A. R. Dysmotility of the small intestine in irritable bowel syndrome. Gut. 1988 Sep;29(9):1236–1243. doi: 10.1136/gut.29.9.1236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kullmann G., Fielding J. F. Rectal distensibility in the irritable bowel syndrome. Ir Med J. 1981 May;74(5):140–142. [PubMed] [Google Scholar]
- Kumar D., Wingate D. L. The irritable bowel syndrome: a paroxysmal motor disorder. Lancet. 1985 Nov 2;2(8462):973–977. doi: 10.1016/s0140-6736(85)90525-2. [DOI] [PubMed] [Google Scholar]
- Lanfranchi G. A., Bazzocchi G., Brignola C., Campieri M., Labò G. Different patterns of intestinal transit time and anorectal motility in painful and painless chronic constipation. Gut. 1984 Dec;25(12):1352–1357. doi: 10.1136/gut.25.12.1352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Latimer P., Sarna S., Campbell D., Latimer M., Waterfall W., Daniel E. E. Colonic motor and myoelectrical activity: a comparative study of normal subjects, psychoneurotic patients, and patients with irritable bowel syndrome. Gastroenterology. 1981 May;80(5 Pt 1):893–901. [PubMed] [Google Scholar]
- Read N. W., Timms J. M., Barfield L. J., Donnelly T. C., Bannister J. J. Impairment of defecation in young women with severe constipation. Gastroenterology. 1986 Jan;90(1):53–60. doi: 10.1016/0016-5085(86)90074-0. [DOI] [PubMed] [Google Scholar]
- Ritchie J. Pain from distension of the pelvic colon by inflating a balloon in the irritable colon syndrome. Gut. 1973 Feb;14(2):125–132. doi: 10.1136/gut.14.2.125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sullivan M. A., Cohen S., Snape W. J., Jr Colonic myoelectrical activity in irritable-bowel syndrome. Effect of eating and anticholinergics. N Engl J Med. 1978 Apr 20;298(16):878–883. doi: 10.1056/NEJM197804202981604. [DOI] [PubMed] [Google Scholar]
- Verduron A., Devroede G., Bouchoucha M., Arhan P., Schang J. C., Poisson J., Hémond M., Hébert M. Megarectum. Dig Dis Sci. 1988 Sep;33(9):1164–1174. doi: 10.1007/BF01535795. [DOI] [PubMed] [Google Scholar]
- Whitehead W. E., Engel B. T., Schuster M. M. Irritable bowel syndrome: physiological and psychological differences between diarrhea-predominant and constipation-predominant patients. Dig Dis Sci. 1980 Jun;25(6):404–413. doi: 10.1007/BF01395503. [DOI] [PubMed] [Google Scholar]
- Zigmond A. S., Snaith R. P. The hospital anxiety and depression scale. Acta Psychiatr Scand. 1983 Jun;67(6):361–370. doi: 10.1111/j.1600-0447.1983.tb09716.x. [DOI] [PubMed] [Google Scholar]



