Abstract
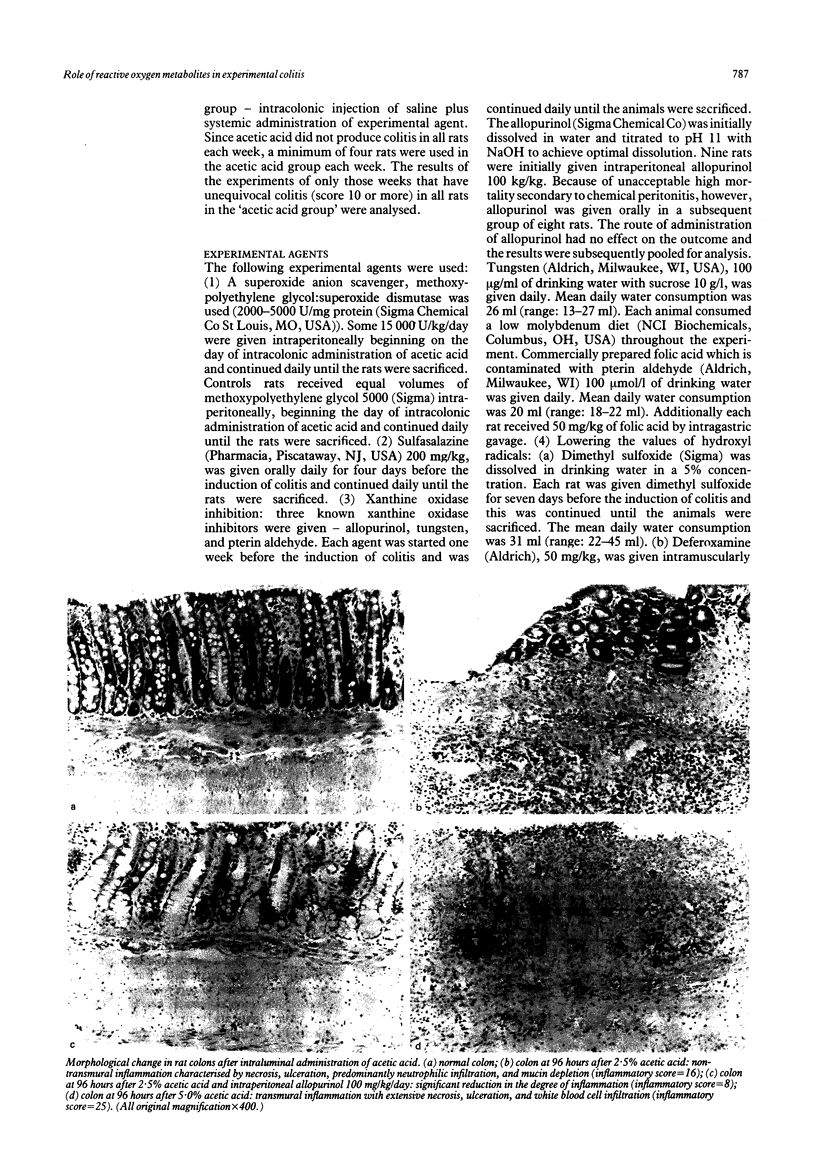
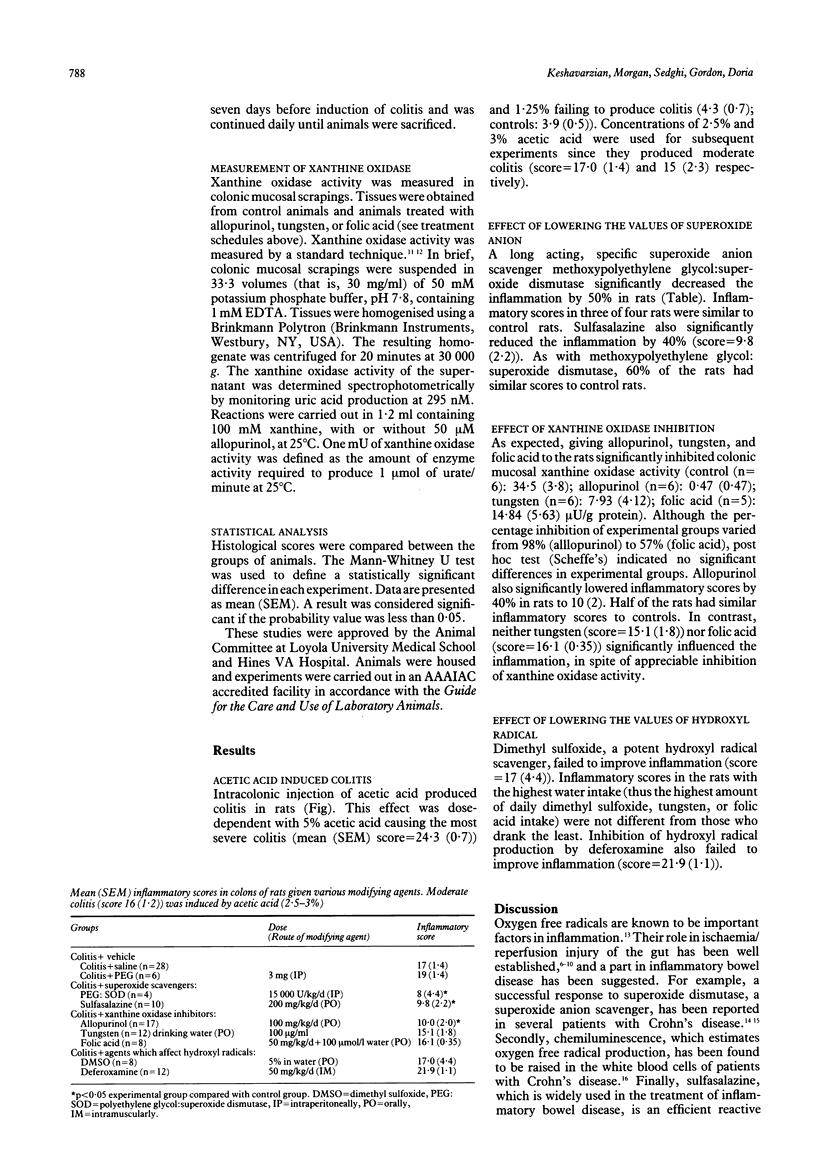
Reactive oxygen metabolites are potent inflammatory mediators that may be involved in tissue injury in inflammatory bowel disease. To evaluate their role in inflammatory bowel disease, we investigated the effects of lowering the activities of reactive oxygen metabolites in experimental colitis induced by intracolonic administration of acetic acid in rats. Intracolonic administration of 5% acetic acid caused severe inflammation (mean (SEM) inflammatory score was 24.3 (0.7) of a maximum score of 32). Acetic acid at 2.5% produced moderate inflammation (score = 17 (1.4) v 4.0 (0.5) in control rats). This lower dose was used for subsequent experiments. Specific superoxide anion scavenger methoxypolyethylene glycol:superoxide dismutase, and reactive oxygen metabolites scavenger, sulfasalazine, significantly decreased the severity of inflammation (scores: 8 (4.4) and 9.8 (2.2) respectively). The xanthine oxidase inhibitors, tungsten and pterin aldehyde, failed to improve inflammation but another xanthine oxidase inhibitor, allopurinol, a compound with known superoxide anion scavenging effect, did limit the inflammation (10(2)). Inhibition of hydroxyl radical production by deferoxamine or lowering hydroxyl radical values by a scavenger, dimethyl sulfoxide, did not affect the severity of inflammation. These data suggest: (1) that reactive oxygen metabolites play an important role in experimental colitis, (2) that the xanthine oxidase pathway is not a major source of reactive oxygen metabolites in colitis, and (3) that tissue injury in experimental colitis is not caused by generation of hydroxyl radicals.
Full text
PDF

Images in this article
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Aruoma O. I., Wasil M., Halliwell B., Hoey B. M., Butler J. The scavenging of oxidants by sulphasalazine and its metabolites. A possible contribution to their anti-inflammatory effects? Biochem Pharmacol. 1987 Nov 1;36(21):3739–3742. doi: 10.1016/0006-2952(87)90028-1. [DOI] [PubMed] [Google Scholar]
- Auscher C., Amory N., van der Kemp P., Delbarre F. Xanthine oxidase activity in human intestines. Histochemical and radiochemical study. Adv Exp Med Biol. 1979;122B:197–201. doi: 10.1007/978-1-4684-8559-2_33. [DOI] [PubMed] [Google Scholar]
- Crissinger K. D., Grisham M. B., Granger D. N. Developmental biology of oxidant-producing enzymes and antioxidants in the piglet intestine. Pediatr Res. 1989 Jun;25(6):612–616. doi: 10.1203/00006450-198906000-00012. [DOI] [PubMed] [Google Scholar]
- Emerit J., Loeper J., Chomette G. Superoxide dismutase in the treatment of post-radiotherapeutic necrosis and of Crohn's disease. Bull Eur Physiopathol Respir. 1981;17 (Suppl):287–287. [PubMed] [Google Scholar]
- Granger D. N., McCord J. M., Parks D. A., Hollwarth M. E. Xanthine oxidase inhibitors attenuate ischemia-induced vascular permeability changes in the cat intestine. Gastroenterology. 1986 Jan;90(1):80–84. doi: 10.1016/0016-5085(86)90078-8. [DOI] [PubMed] [Google Scholar]
- Granger D. N., Rutili G., McCord J. M. Superoxide radicals in feline intestinal ischemia. Gastroenterology. 1981 Jul;81(1):22–29. [PubMed] [Google Scholar]
- Johnson J. L., Rajagopalan K. V., Cohen H. J. Molecular basis of the biological function of molybdenum. Effect of tungsten on xanthine oxidase and sulfite oxidase in the rat. J Biol Chem. 1974 Feb 10;249(3):859–866. [PubMed] [Google Scholar]
- Kirsner J. B., Shorter R. G. Recent developments in nonspecific inflammatory bowel disease (second of two parts). N Engl J Med. 1982 Apr 8;306(14):837–848. doi: 10.1056/NEJM198204083061404. [DOI] [PubMed] [Google Scholar]
- Lewis A. S., Murphy L., McCalla C., Fleary M., Purcell S. Inhibition of mammalian xanthine oxidase by folate compounds and amethopterin. J Biol Chem. 1984 Jan 10;259(1):12–15. [PubMed] [Google Scholar]
- MacPherson B., Pfeiffer C. J. Experimental colitis. Digestion. 1976;14(5-6):424–452. doi: 10.1159/000197966. [DOI] [PubMed] [Google Scholar]
- Niwa Y., Somiya K., Michelson A. M., Puget K. Effect of liposomal-encapsulated superoxide dismutase on active oxygen-related human disorders. A preliminary study. Free Radic Res Commun. 1985;1(2):137–153. doi: 10.3109/10715768509056547. [DOI] [PubMed] [Google Scholar]
- Parks D. A., Bulkley G. B., Granger D. N. Role of oxygen-derived free radicals in digestive tract diseases. Surgery. 1983 Sep;94(3):415–422. [PubMed] [Google Scholar]
- Perry M. A., Wadhwa S., Parks D. A., Pickard W., Granger D. N. Role of oxygen radicals in ischemia-induced lesions in the cat stomach. Gastroenterology. 1986 Feb;90(2):362–367. doi: 10.1016/0016-5085(86)90933-9. [DOI] [PubMed] [Google Scholar]
- Sharon P., Ligumsky M., Rachmilewitz D., Zor U. Role of prostaglandins in ulcerative colitis. Enhanced production during active disease and inhibition by sulfasalazine. Gastroenterology. 1978 Oct;75(4):638–640. [PubMed] [Google Scholar]
- Sharon P., Stenson W. F. Enhanced synthesis of leukotriene B4 by colonic mucosa in inflammatory bowel disease. Gastroenterology. 1984 Mar;86(3):453–460. [PubMed] [Google Scholar]
- Sharon P., Stenson W. F. Metabolism of arachidonic acid in acetic acid colitis in rats. Similarity to human inflammatory bowel disease. Gastroenterology. 1985 Jan;88(1 Pt 1):55–63. doi: 10.1016/s0016-5085(85)80132-3. [DOI] [PubMed] [Google Scholar]
- Smith S. M., Grisham M. B., Manci E. A., Granger D. N., Kvietys P. R. Gastric mucosal injury in the rat. Role of iron and xanthine oxidase. Gastroenterology. 1987 Apr;92(4):950–956. doi: 10.1016/0016-5085(87)90969-3. [DOI] [PubMed] [Google Scholar]
- Topham R. W., Walker M. C., Calisch M. P. Liver xanthine dehydrogenase and iron mobilization. Biochem Biophys Res Commun. 1982 Dec 31;109(4):1240–1246. doi: 10.1016/0006-291x(82)91910-6. [DOI] [PubMed] [Google Scholar]
- Weiss S. J. Tissue destruction by neutrophils. N Engl J Med. 1989 Feb 9;320(6):365–376. doi: 10.1056/NEJM198902093200606. [DOI] [PubMed] [Google Scholar]