Abstract
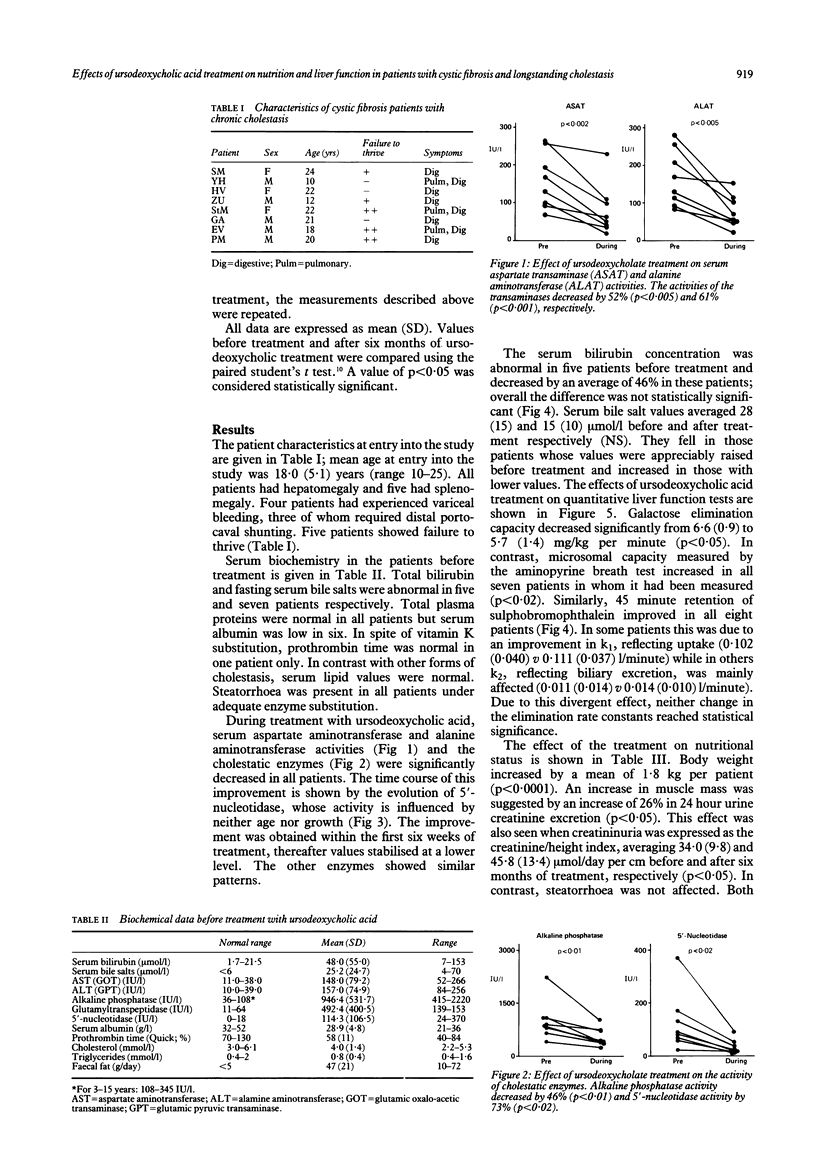
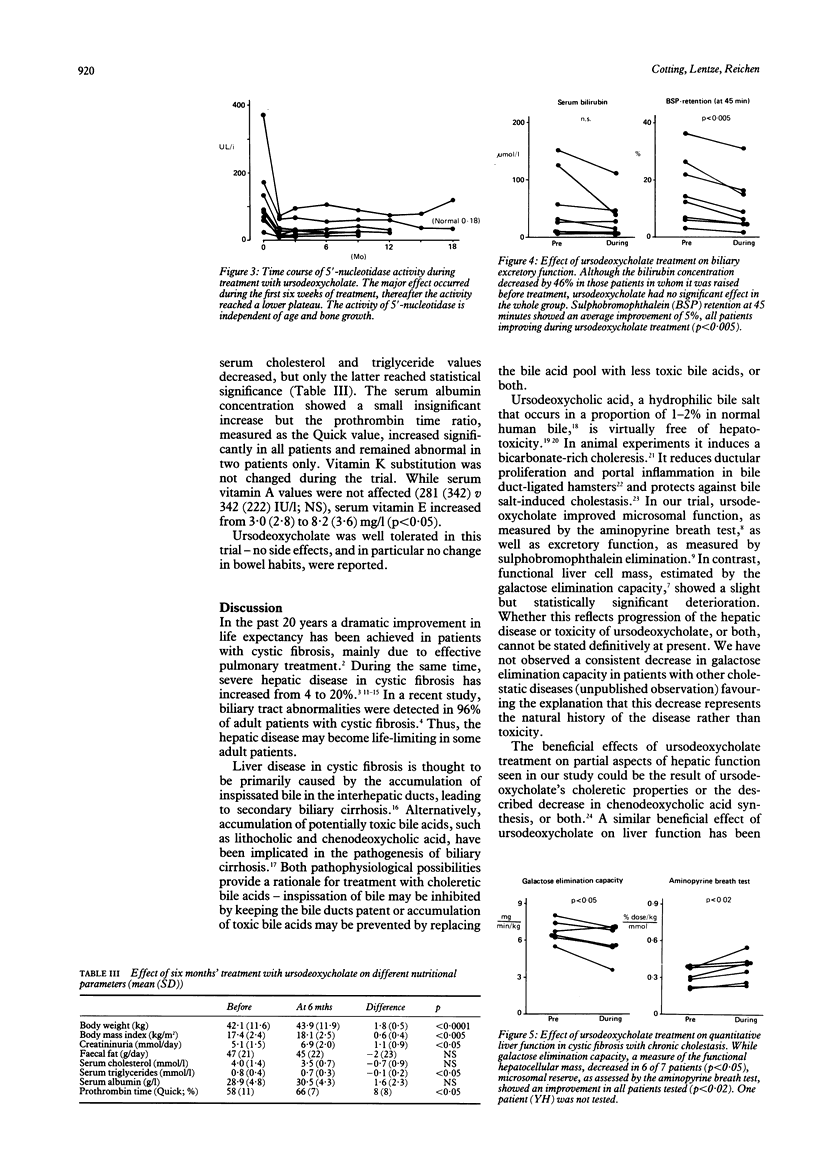
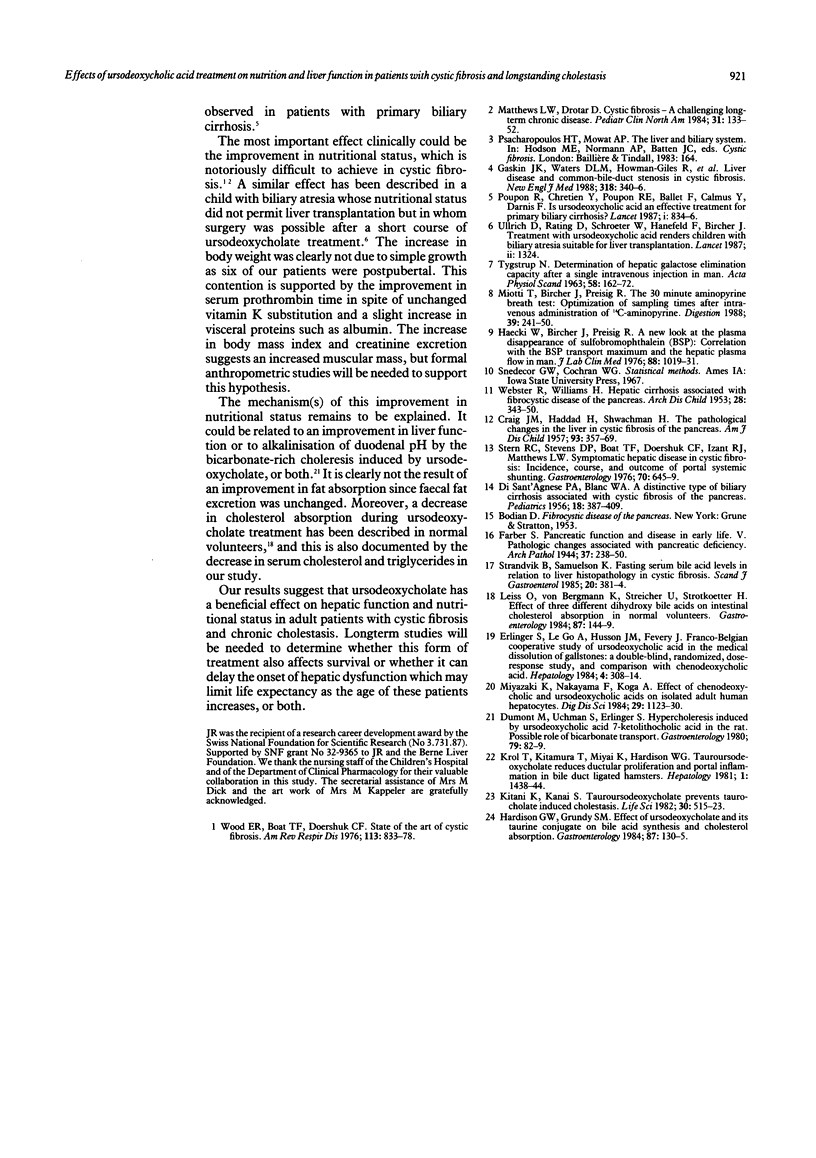
The prevalence of biliary and hepatic diseases is increasing in patients with cystic fibrosis as more of them reach adult life. There is no effective treatment or method of preventing cholestasis in cystic fibrosis, although beneficial effects have been ascribed to the tertiary bile acid, ursodeoxycholate, in other forms of chronic cholestasis. We evaluated prospectively the effects of a six month course of ursodeoxycholate (15-20 mg/kg per day) in eight, mostly adult, patients with cystic fibrosis and chronic cholestasis. Bile acid treatment improved inflammatory activity (average decrease in alanine aminotransferase, 60%, p less than 0.005) and cholestasis (alkaline phosphatase, 47%; p less than 0.01) in all patients. Quantitative liver function, measured by 45 minute sulphobromophthalein retention and by the 14C-aminopyrine breath test, improved in all patients while galactose elimination capacity showed a slight decrease. Patients' nutritional state improved as evidenced by a 1.8 kg weight gain and an increase in muscle mass suggested by a 26% increase in 24 hour urinary creatinine excretion. Steatorrhea was not affected by bile acid treatment. Ursodeoxycholic acid may be beneficial in the treatment of chronic cholestasis in cystic fibrosis by improving liver function and also the patient's nutritional state.
Full text
PDF
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- BLANC W. A., DI SANT'AGNESE P. A. A distinctive type of biliary cirrhosis of the liver associated with cystic fibrosis of the pancreas; recognition through signs of portal hypertension. Pediatrics. 1956 Sep;18(3):387–409. [PubMed] [Google Scholar]
- CRAIG J. M., HADDAD H., SHWACHMAN H. The pathological changes in the liver in cystic fibrosis of the pancreas. AMA J Dis Child. 1957 Apr;93(4):357–369. doi: 10.1001/archpedi.1957.02060040359002. [DOI] [PubMed] [Google Scholar]
- Dumont M., Erlinger S., Uchman S. Hypercholeresis induced by ursodeoxycholic acid and 7-ketolithocholic acid in the rat: possible role of bicarbonate transport. Gastroenterology. 1980 Jul;79(1):82–89. [PubMed] [Google Scholar]
- Erlinger S., Le Go A., Husson J. M., Fevery J. Franco-Belgian cooperative study of ursodeoxycholic acid in the medical dissolution of gallstones: a double-blind, randomized, dose-response study, and comparison with chenodeoxycholic acid. Hepatology. 1984 Mar-Apr;4(2):308–314. doi: 10.1002/hep.1840040222. [DOI] [PubMed] [Google Scholar]
- Gaskin K. J., Waters D. L., Howman-Giles R., de Silva M., Earl J. W., Martin H. C., Kan A. E., Brown J. M., Dorney S. F. Liver disease and common-bile-duct stenosis in cystic fibrosis. N Engl J Med. 1988 Feb 11;318(6):340–346. doi: 10.1056/NEJM198802113180602. [DOI] [PubMed] [Google Scholar]
- Hardison W. G., Grundy S. M. Effect of ursodeoxycholate and its taurine conjugate on bile acid synthesis and cholesterol absorption. Gastroenterology. 1984 Jul;87(1):130–135. [PubMed] [Google Scholar]
- Häcki W., Bircher J., Preisig R. A new look at the plasma disappearance of sulfobromophthalein (BSP): correlation with the BSP transport maximum and the hepatic plasma flow in man. J Lab Clin Med. 1976 Dec;88(6):1019–1031. [PubMed] [Google Scholar]
- Kitani K., Kanai S. Tauroursodeoxycholate prevents taurocholate induced cholestasis. Life Sci. 1982 Feb 7;30(6):515–523. doi: 10.1016/0024-3205(82)90264-8. [DOI] [PubMed] [Google Scholar]
- Leiss O., von Bergmann K., Streicher U., Strotkoetter H. Effect of three different dihydroxy bile acids on intestinal cholesterol absorption in normal volunteers. Gastroenterology. 1984 Jul;87(1):144–149. [PubMed] [Google Scholar]
- Matthews L. W., Drotar D. Cystic fibrosis--a challenging long-term chronic disease. Pediatr Clin North Am. 1984 Feb;31(1):133–152. doi: 10.1016/s0031-3955(16)34541-2. [DOI] [PubMed] [Google Scholar]
- Miotti T., Bircher J., Preisig R. The 30-minute aminopyrine breath test: optimization of sampling times after intravenous administration of 14C-aminopyrine. Digestion. 1988;39(4):241–250. doi: 10.1159/000199632. [DOI] [PubMed] [Google Scholar]
- Miyazaki K., Nakayama F., Koga A. Effect of chenodeoxycholic and ursodeoxycholic acids on isolated adult human hepatocytes. Dig Dis Sci. 1984 Dec;29(12):1123–1130. doi: 10.1007/BF01317087. [DOI] [PubMed] [Google Scholar]
- Poupon R., Chrétien Y., Poupon R. E., Ballet F., Calmus Y., Darnis F. Is ursodeoxycholic acid an effective treatment for primary biliary cirrhosis? Lancet. 1987 Apr 11;1(8537):834–836. doi: 10.1016/s0140-6736(87)91610-2. [DOI] [PubMed] [Google Scholar]
- Stern R. C., Stevens D. P., Boat T. F., Doershuk C. F., Izant R. J., Jr, Matthews L. W. Symptomatic hepatic disease in cystic fibrosis: incidence, course, and outcome of portal systemic hunting. Gastroenterology. 1976 May;70(5 PT1):645–649. [PubMed] [Google Scholar]
- Strandvik B., Samuelson K. Fasting serum bile acid levels in relation to liver histopathology in cystic fibrosis. Scand J Gastroenterol. 1985 Apr;20(3):381–384. doi: 10.3109/00365528509091668. [DOI] [PubMed] [Google Scholar]
- TYGSTRUP N. Determination of the hepatic galactose elimination capacity after a single intravenous injection in man: the reproducibility and the influence of uneven distribution. Acta Physiol Scand. 1963 Jun-Jul;58:162–172. doi: 10.1111/j.1748-1716.1963.tb02638.x. [DOI] [PubMed] [Google Scholar]
- Ullrich D., Rating D., Schröter W., Hanefeld F., Bircher J. Treatment with ursodeoxycholic acid renders children with biliary atresia suitable for liver transplantation. Lancet. 1987 Dec 5;2(8571):1324–1324. doi: 10.1016/s0140-6736(87)91208-6. [DOI] [PubMed] [Google Scholar]
- WEBSTER R., WILLIAMS H. Hepatic cirrhosis associated with fibrocystic disease of the pancreas; clinical and pathological reports of five patients. Arch Dis Child. 1953 Oct;28(141):343–350. doi: 10.1136/adc.28.141.343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wood R. E., Boat T. F., Doershuk C. F. Cystic fibrosis. Am Rev Respir Dis. 1976 Jun;113(6):833–878. doi: 10.1164/arrd.1976.113.6.833. [DOI] [PubMed] [Google Scholar]


