Abstract
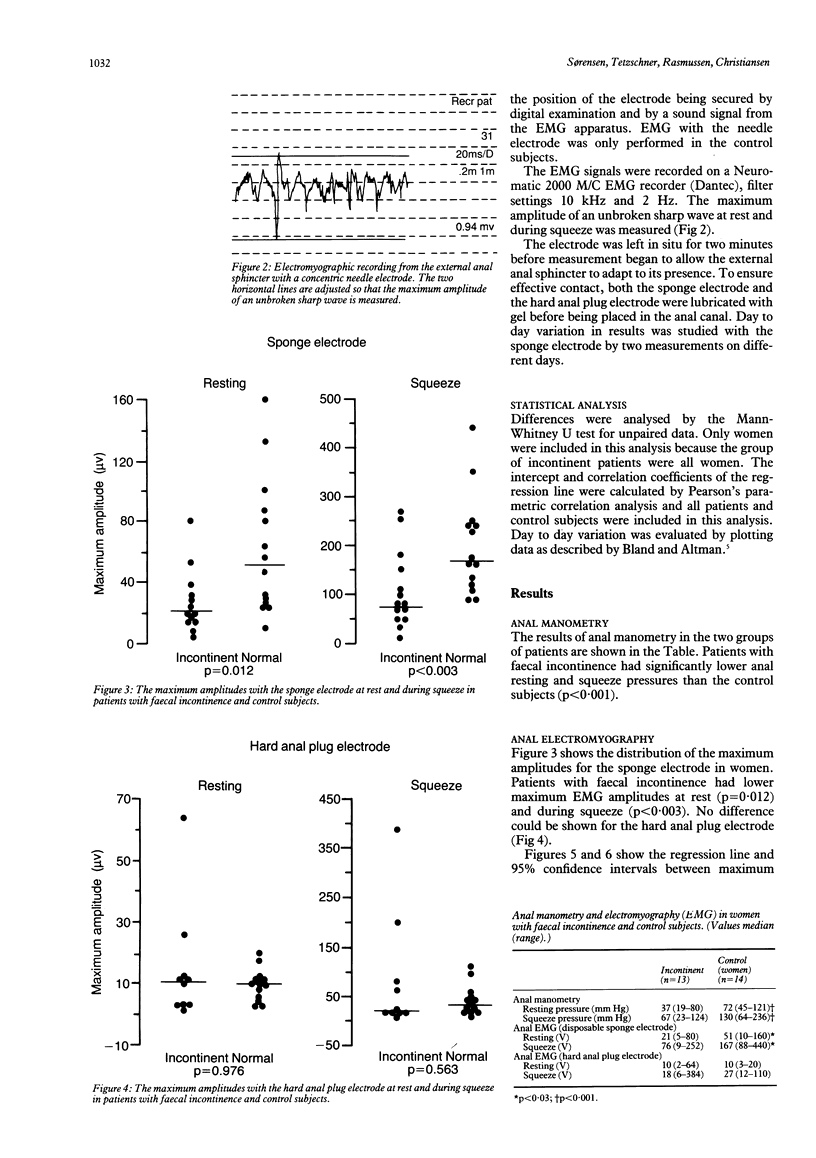
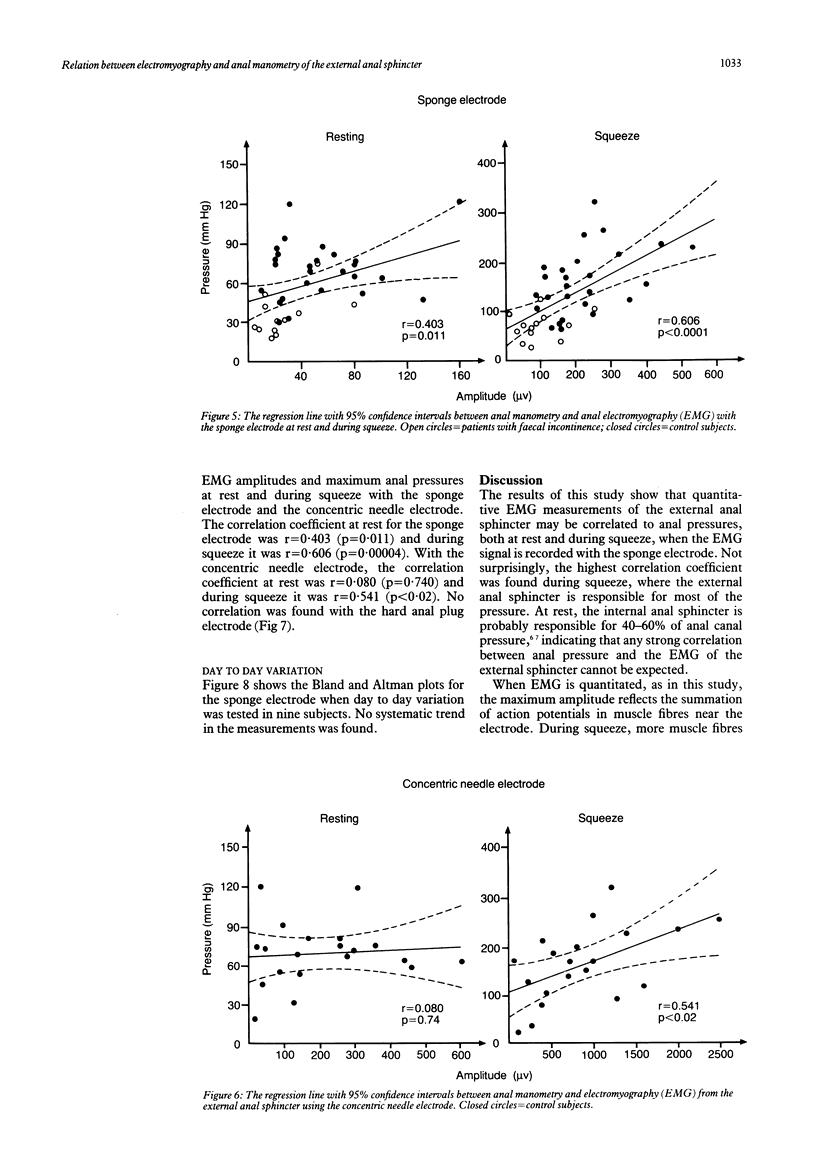
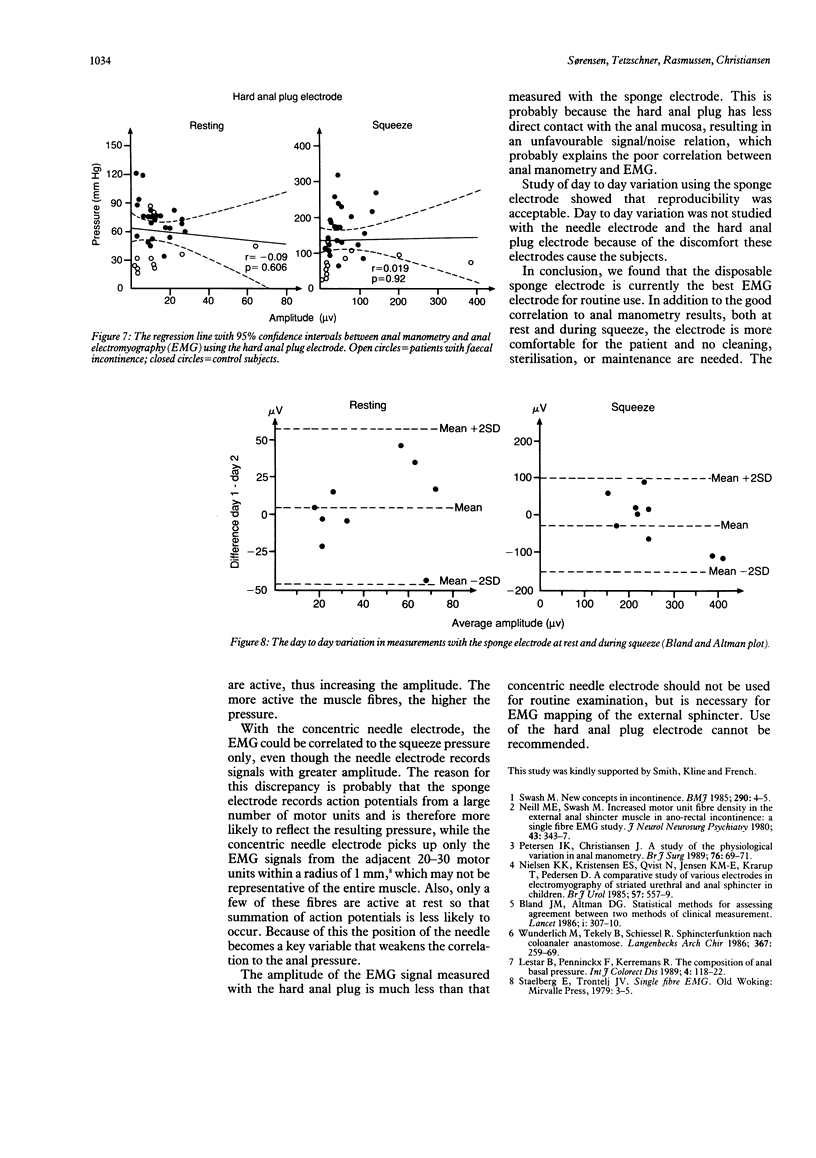
Thirteen patients with faecal incontinence and 26 control subjects were studied to investigate whether a quantitative electromyographic (EMG) signal could be correlated to anal manometry. Three different electrodes were used--a concentric needle electrode, a disposable sponge electrode, and a hard anal plug electrode. The maximum amplitude of the EMG recording was used as a quantitative parameter. Linear regression showed significant correlation between EMG and anal manometry with the sponge electrode, both at rest and during squeeze. Significant correlation was also found with the concentric needle electrode during squeeze but not at rest. No correlation was found with the hard anal plug electrode either during squeeze or at rest. Reproducibility studies using the sponge electrode showed acceptable day to day variation. In conclusion, quantitative EMG recordings from a disposable sponge electrode placed in the anal canal correlate well to anal manometry and may be used for assessment of sphincter function, but the hard anal plug electrode cannot be recommended.
Full text
PDF
Images in this article
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Bland J. M., Altman D. G. Statistical methods for assessing agreement between two methods of clinical measurement. Lancet. 1986 Feb 8;1(8476):307–310. [PubMed] [Google Scholar]
- Lestar B., Penninckx F., Kerremans R. The composition of anal basal pressure. An in vivo and in vitro study in man. Int J Colorectal Dis. 1989;4(2):118–122. doi: 10.1007/BF01646870. [DOI] [PubMed] [Google Scholar]
- Neill M. E., Swash M. Increased motor unit fibre density in the external anal sphincter muscle in ano-rectal incontinence: a single fibre EMG study. J Neurol Neurosurg Psychiatry. 1980 Apr;43(4):343–347. doi: 10.1136/jnnp.43.4.343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nielsen K. K., Kristensen E. S., Qvist N., Jensen K. M., Dalsgård J., Krarup T., Pedersen D. A comparative study of various electrodes in electromyography of the striated urethral and anal sphincter in children. Br J Urol. 1985 Oct;57(5):557–559. doi: 10.1111/j.1464-410x.1985.tb05866.x. [DOI] [PubMed] [Google Scholar]
- Pedersen I. K., Christiansen J. A study of the physiological variation in anal manometry. Br J Surg. 1989 Jan;76(1):69–70. doi: 10.1002/bjs.1800760121. [DOI] [PubMed] [Google Scholar]
- Swash M. New concepts in incontinence. Br Med J (Clin Res Ed) 1985 Jan 5;290(6461):4–5. doi: 10.1136/bmj.290.6461.4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wunderlich M., Teleky B., Schiessel R. Sphincterfunktion nach coloanaler Anastomose. Langenbecks Arch Chir. 1986;367(4):259–269. doi: 10.1007/BF01263406. [DOI] [PubMed] [Google Scholar]