Abstract
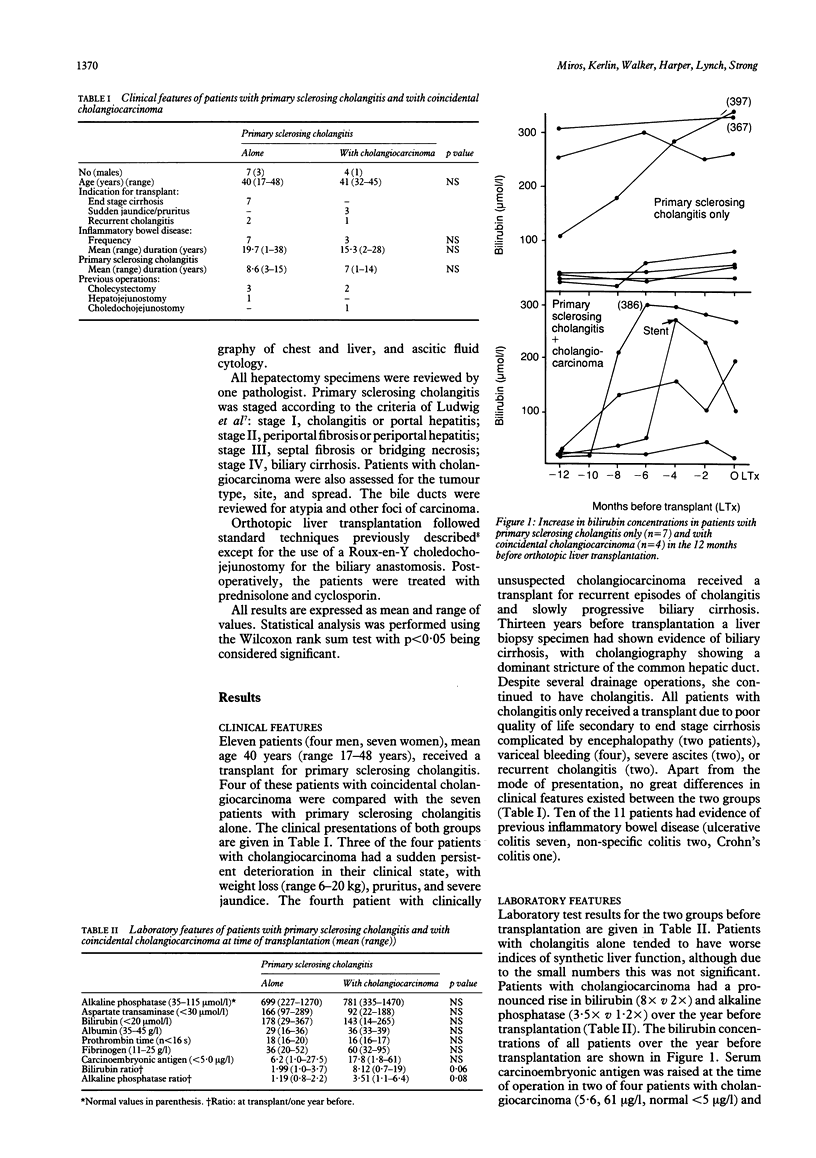
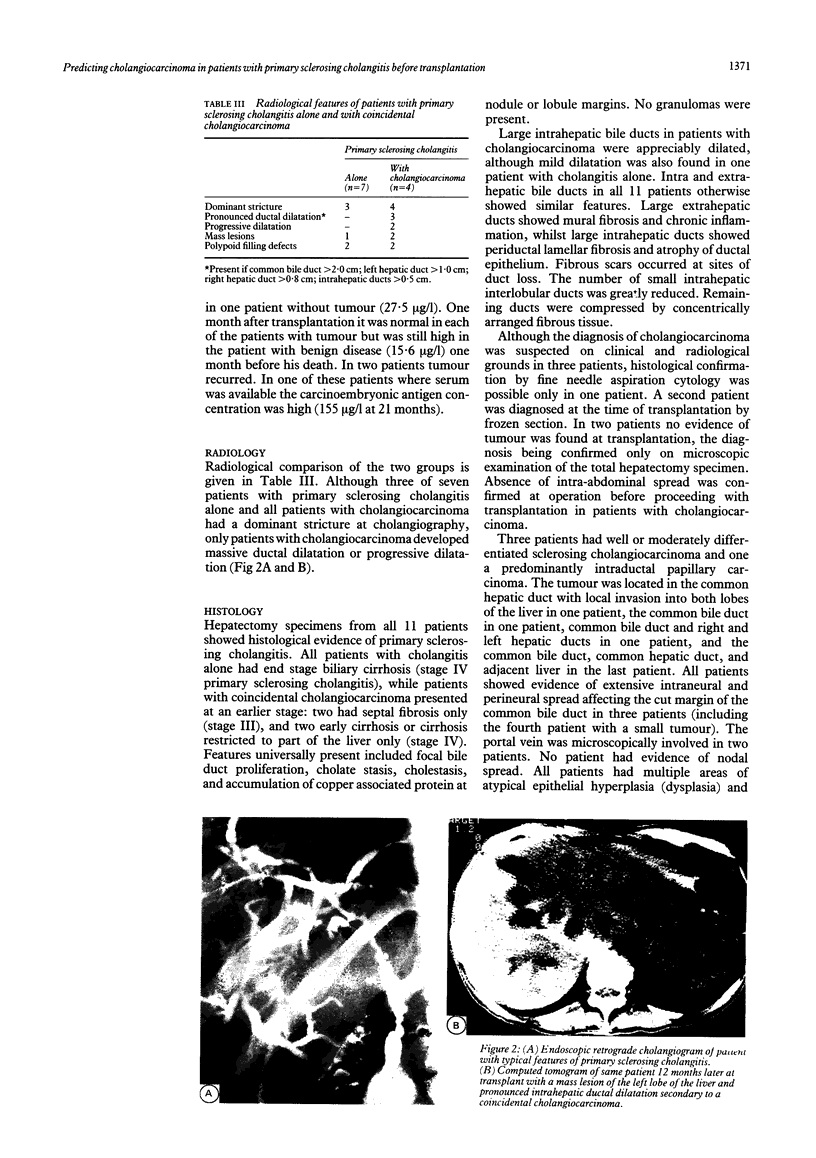
Patients with primary sclerosing cholangitis are at an increased risk of developing cholangiocarcinoma, which is difficult to diagnose because the biliary tree is already distorted. Eleven patients with primary sclerosing cholangitis who underwent orthotopic liver transplantation at this hospital were evaluated. Four patients had coincidental histologically proved cholangiocarcinoma. Patients with cholangiocarcinoma in contrast to patients without tumour presented with rapid onset of persistent jaundice, pruritus, and weight loss associated with an appreciable rise in bilirubin (8x v 2x) and alkaline phosphatase (3.5x v 1.2x) over one year. Cholangiography and computed tomography showed appreciably dilated intrahepatic bile ducts (3/4 v 0/7). The diagnosis of cholangiocarcinoma could only be established before operation in one patient by fine needle aspiration cytology. Tumour was recognised at operation in one other. Histological examination of hepatectomy specimens showed that patients with cholangiocarcinoma had less advanced histological features of primary sclerosing cholangitis. Multiple areas of carcinoembryonic antigen positive epithelial atypia and carcinoma in situ were found in all patients with cholangiocarcinoma. Cholangiocarcinoma recurred in two patients at 14 and 39 months after transplantation. Superimposed cholangiocarcinoma can be predicted in most patients with cholangitis before transplantation, although a definitive diagnosis is difficult to make. Their prognosis after successful transplantation is guarded.
Full text
PDF

Images in this article
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Aadland E., Schrumpf E., Fausa O., Elgjo K., Heilo A., Aakhus T., Gjone E. Primary sclerosing cholangitis: a long-term follow-up study. Scand J Gastroenterol. 1987 Aug;22(6):655–664. doi: 10.3109/00365528709011139. [DOI] [PubMed] [Google Scholar]
- Akwari O. E., Van Heerden J. A., Foulk W. T., Baggenstoss A. H. Cancer of the bile ducts associated with ulcerative colitis. Ann Surg. 1975 Mar;181(3):303–309. doi: 10.1097/00000658-197503000-00010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chapman R. W., Arborgh B. A., Rhodes J. M., Summerfield J. A., Dick R., Scheuer P. J., Sherlock S. Primary sclerosing cholangitis: a review of its clinical features, cholangiography, and hepatic histology. Gut. 1980 Oct;21(10):870–877. doi: 10.1136/gut.21.10.870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohan R. H., Illescas F. F., Newman G. E., Braun S. D., Dunnick N. R. Biliary cytodiagnosis. Bile sampling for cytology. Invest Radiol. 1985 Mar-Apr;20(2):177–179. doi: 10.1097/00004424-198503000-00015. [DOI] [PubMed] [Google Scholar]
- Converse C. F., Reagan J. W., DeCosse J. J. Ulcerative colitis and carcinoma of the bile ducts. Am J Surg. 1971 Jan;121(1):39–45. doi: 10.1016/0002-9610(71)90075-4. [DOI] [PubMed] [Google Scholar]
- Davis R. I., Sloan J. M., Hood J. M., Maxwell P. Carcinoma of the extrahepatic biliary tract: a clinicopathological and immunohistochemical study. Histopathology. 1988 Jun;12(6):623–631. doi: 10.1111/j.1365-2559.1988.tb01986.x. [DOI] [PubMed] [Google Scholar]
- Haworth A. C., Manley P. N., Groll A., Pace R. Bile duct carcinoma and biliary tract dysplasia in chronic ulcerative colitis. Arch Pathol Lab Med. 1989 Apr;113(4):434–436. [PubMed] [Google Scholar]
- Koneru B., Cassavilla A., Bowman J., Iwatsuki S., Starzl T. E. Liver transplantation for malignant tumors. Gastroenterol Clin North Am. 1988 Mar;17(1):177–193. [PMC free article] [PubMed] [Google Scholar]
- Lynch S., Kerlin P., Ong T. H., Pillay S. P., Wall D., Balderson G., Burrow B., Board J., Cleghorn G., Shepherd R. Liver transplantation in Australia: the Queensland experience. Transplant Proc. 1989 Feb;21(1 Pt 2):2399–2401. [PubMed] [Google Scholar]
- Lynch S., Kerlin P., Wall D., Ong T. H., Shepherd R. W., Cleghorn G. J., Pillay S. P., Powell L., Balderson G., O'Connor J. The Queensland Liver Transplant Programme: the first two years. Med J Aust. 1987 Oct 19;147(8):380–385. [PubMed] [Google Scholar]
- Marsh J. W., Jr, Iwatsuki S., Makowka L., Esquivel C. O., Gordon R. D., Todo S., Tzakis A., Miller C., Van Thiel D., Starzl T. E. Orthotopic liver transplantation for primary sclerosing cholangitis. Ann Surg. 1988 Jan;207(1):21–25. doi: 10.1097/00000658-198801000-00005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mir-Madjlessi S. H., Farmer R. G., Sivak M. V., Jr Bile duct carcinoma in patients with ulcerative colitis. Relationship to sclerosing cholangitis: report of six cases and review of the literature. Dig Dis Sci. 1987 Feb;32(2):145–154. doi: 10.1007/BF01297102. [DOI] [PubMed] [Google Scholar]
- Roberts-Thomson I. C., Strickland R. G., Mackay I. R. Bile duct carcinoma in chronic ulcerative colitis. Aust N Z J Med. 1973 Jun;3(3):264–267. doi: 10.1111/j.1445-5994.1973.tb03093.x. [DOI] [PubMed] [Google Scholar]
- Wee A., Ludwig J., Coffey R. J., Jr, LaRusso N. F., Wiesner R. H. Hepatobiliary carcinoma associated with primary sclerosing cholangitis and chronic ulcerative colitis. Hum Pathol. 1985 Jul;16(7):719–726. doi: 10.1016/s0046-8177(85)80158-1. [DOI] [PubMed] [Google Scholar]
- Wiesner R. H., Grambsch P. M., Dickson E. R., Ludwig J., MacCarty R. L., Hunter E. B., Fleming T. R., Fisher L. D., Beaver S. J., LaRusso N. F. Primary sclerosing cholangitis: natural history, prognostic factors and survival analysis. Hepatology. 1989 Oct;10(4):430–436. doi: 10.1002/hep.1840100406. [DOI] [PubMed] [Google Scholar]
- Yamaguchi K., Enjoji M., Nakayama F. Cancer of the extrahepatic bile duct: a clinicopathologic study of immunohistochemistry for CEA, CA19-9, and p21. World J Surg. 1988 Feb;12(1):11–17. doi: 10.1007/BF01658480. [DOI] [PubMed] [Google Scholar]