Abstract
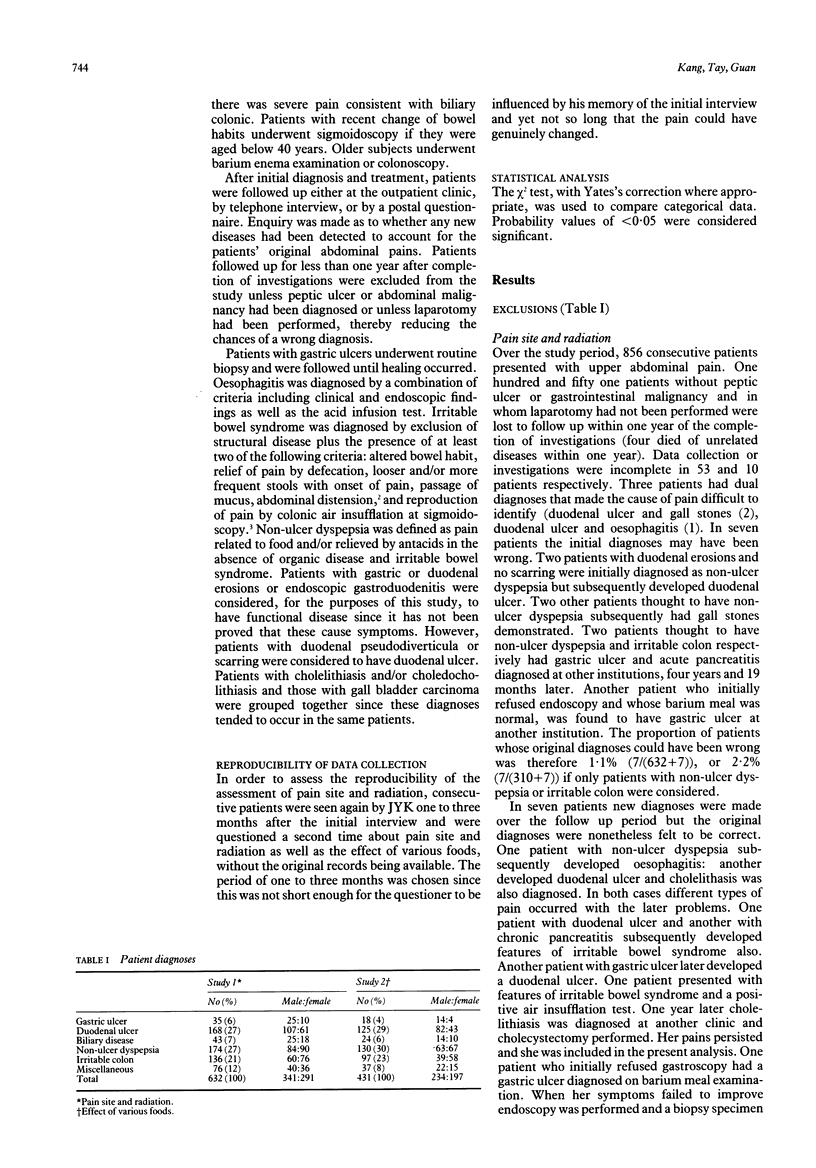
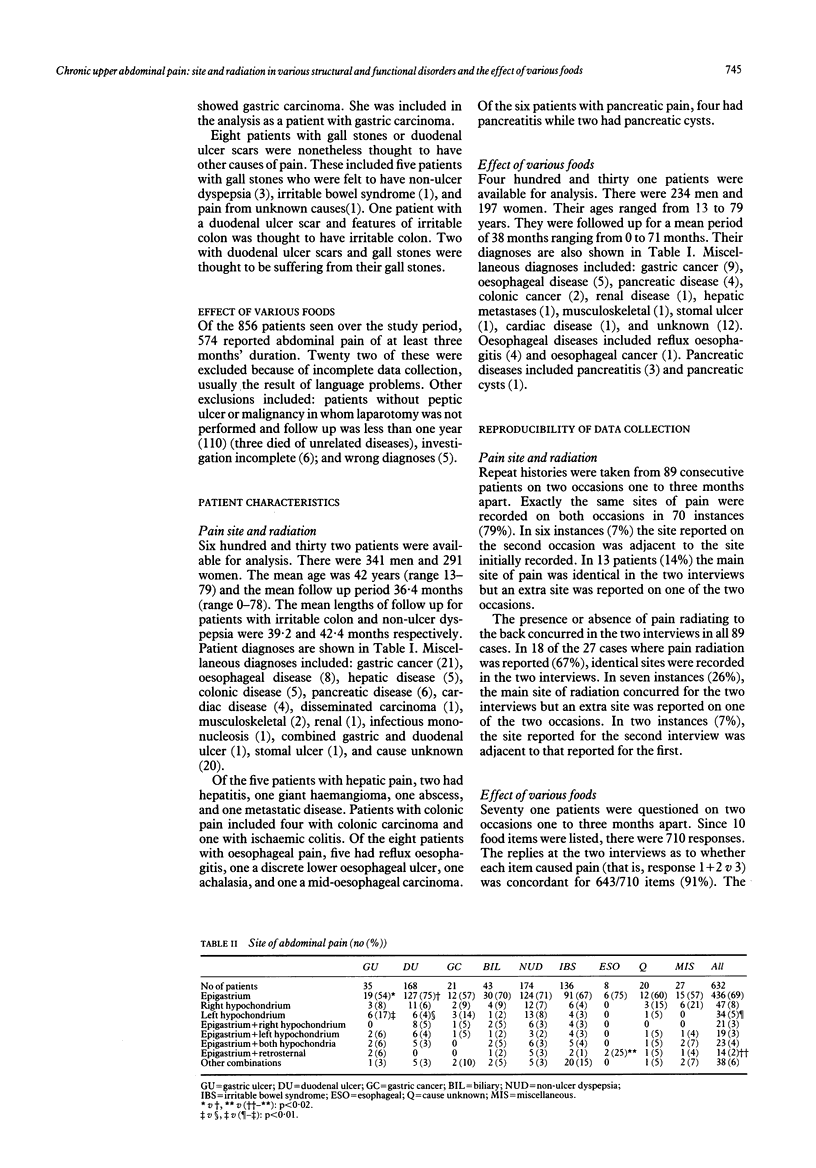
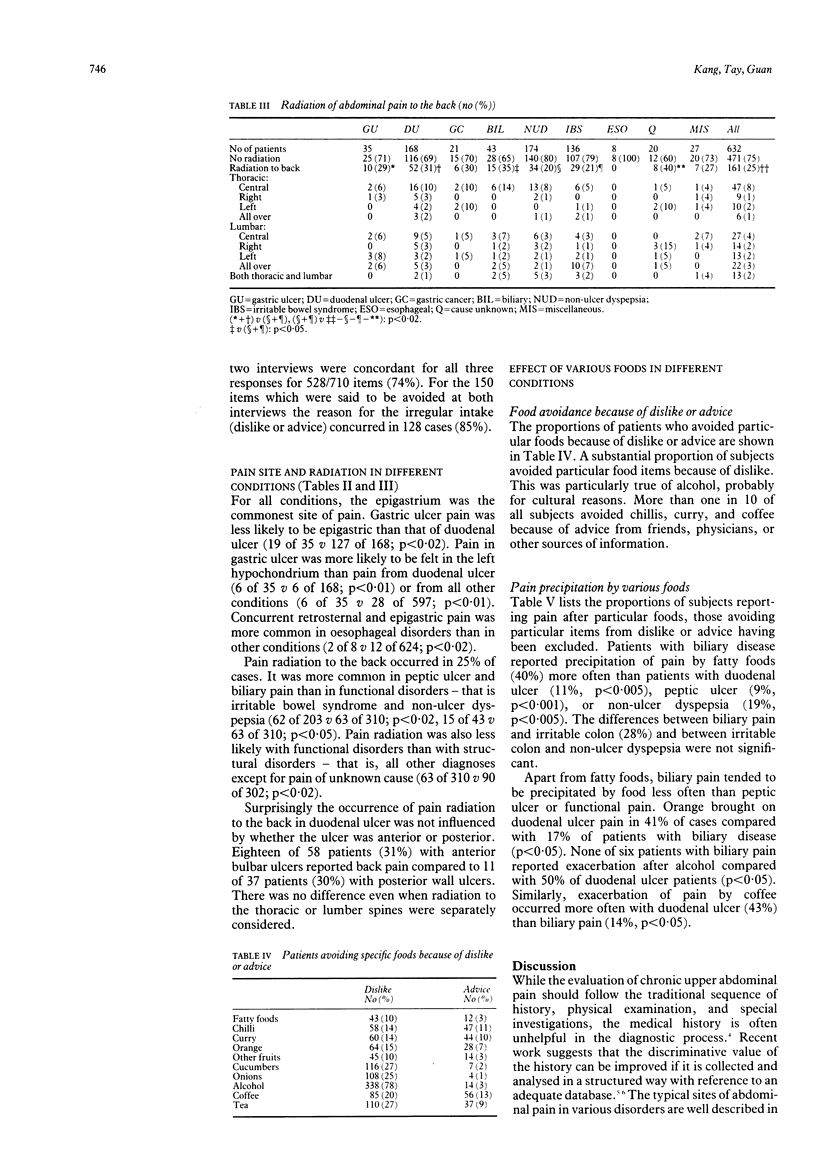
Pain site and radiation and the effect of various foods were studied prospectively in a consecutive series of patients with chronic upper abdominal pain. Patients followed for less than one year were excluded unless peptic ulcer or abdominal malignancy had been diagnosed or laparotomy had been carried out. A total of 632 patients were eligible for the first study and 431 for the second. Gastric ulcer pain was more likely to be left hypochondrial (17%) compared with pain from duodenal ulcer (4%) or from all other conditions (5%). It was less likely to be epigastric (54%) compared with duodenal ulcer pain (75%). Oesophageal pain was more likely to be both retrosternal and epigastric (25%) compared with non-oesophageal pain (2%). Radiation to the back was more common in peptic ulcer (31%) and biliary pain (35%) compared with functional pain (20%). Pain precipitation by fatty foods was commoner in biliary disease (40%) than in duodenal ulcer (11%), peptic ulcer (9%), or non-ulcer dyspepsia (19%). Orange, alcohol, and coffee precipitated pain more frequently in duodenal ulcer (41%, 50%, and 43% respectively) than in biliary disease (17%, 0%, and 14% respectively). Chilli precipitated pain in one quarter to one half of subjects regardless of diagnosis. Approximately one tenth of all subjects avoided chilli, curry, coffee, and tea because of medical or other advice.
Full text
PDF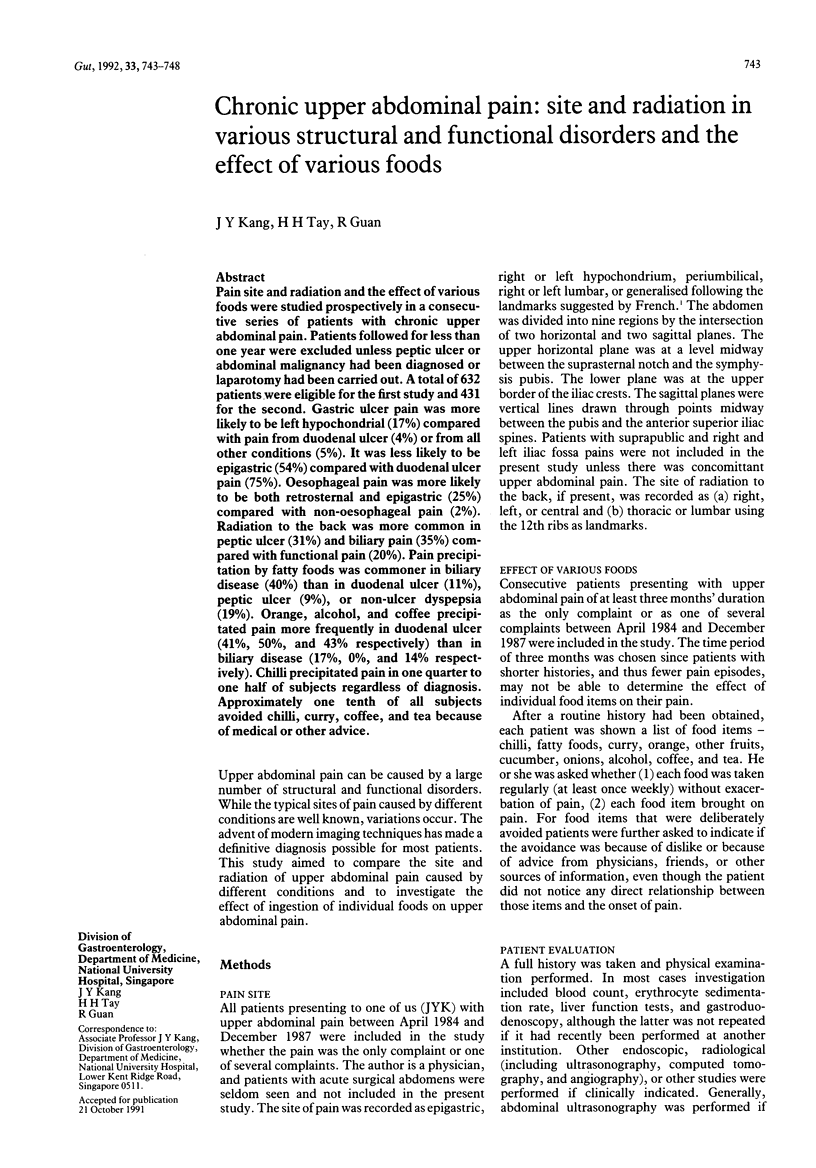


Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Earlam R. A computerized questionnaire analysis of duodenal ulcer symptoms. Gastroenterology. 1976 Aug;71(2):314–317. [PubMed] [Google Scholar]
- Eisig J. N., Zaterka S., Massuda H. K., Bettarello A. Coffee drinking in patients with duodenal ulcer and a control population. Scand J Gastroenterol. 1989 Sep;24(7):796–798. doi: 10.3109/00365528909089216. [DOI] [PubMed] [Google Scholar]
- Gunn A., Keddie N. Some clinical observations on patients with gallstones. Lancet. 1972 Aug 5;2(7771):239–241. doi: 10.1016/s0140-6736(72)91683-2. [DOI] [PubMed] [Google Scholar]
- Kingham J. G., Dawson A. M. Origin of chronic right upper quadrant pain. Gut. 1985 Aug;26(8):783–788. doi: 10.1136/gut.26.8.783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Manning A. P., Thompson W. G., Heaton K. W., Morris A. F. Towards positive diagnosis of the irritable bowel. Br Med J. 1978 Sep 2;2(6138):653–654. doi: 10.1136/bmj.2.6138.653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Swarbrick E. T., Hegarty J. E., Bat L., Williams C. B., Dawson A. M. Site of pain from the irritable bowel. Lancet. 1980 Aug 30;2(8192):443–446. doi: 10.1016/s0140-6736(80)91885-1. [DOI] [PubMed] [Google Scholar]
- Talley N. J., Phillips S. F. Non-ulcer dyspepsia: potential causes and pathophysiology. Ann Intern Med. 1988 Jun;108(6):865–879. doi: 10.7326/0003-4819-108-6-865. [DOI] [PubMed] [Google Scholar]


