Abstract
Objectives. We evaluated the efficacy of 15 years of a public health–oriented suicidal-behavior prevention program among youths living on an American Indian reservation.
Methods. All suicides, suicide attempts, and suicidal gestures were monitored. Age-specific analyses over time were used to assess outcomes.
Results. Both descriptive and linear regression analyses indicated that a substantial drop occurred in suicidal gestures and attempts. Suicide deaths neither declined significantly nor increased, although the total number of self-destructive acts declined by 73% (P=.001).
Conclusions. Data from this community-based approach document a remarkable downward trend—measured by both magnitude and temporal trends in the specifically targeted age cohorts—in suicidal acts. The sequential decrease in age-specific rates of suicide attempts and gestures is indicative of the program’s success.
Recently, a number of scholars and officials have called for population-based public health strategies for preventing suicide in entire communities and racial/ethnic groups. Noting that approaches to suicide prevention are often narrowly based on psychiatric and individual dynamics, the surgeon general,1 the US Public Health Service,2 and the Institute of Medicine3 have voiced the need for a new, comprehensive understanding of suicidal behavior on which to base suicide prevention efforts. Three recent publications explain the rationale for a population-based approach to preventing suicidal behavior,3 calling suicide prevention a national imperative3 for public health intervention.4,5
American Indian/Alaska Native (AIAN) suicide studies and prevention programs have frequently been approached from a public health perspective,6–22 but detailed evaluation of such programs among American Indians/Alaska Natives has been quite rare in practice and in the literature.18 We describe an outcome evaluation of a suicide prevention program among the Western Athabaskan Tribal Nation (a pseudonym used to protect the identity of this tribe—one of several Athabaskan tribes in the southwestern United States—and its reservation) of New Mexico. This program is part of an ongoing effort to evaluate AIAN suicide trends, potential causes of these trends, and the efficacy of prevention programs in New Mexico19,23,24 (P. Serna, unpublished data, 1991; Western Athabaskan Tribal Nation, unpublished data, 2003).
An increase in suicidal activity among AIAN adolescents and young adults on this reservation in 1988 prompted the tribal council and community and the Indian Health Service (IHS) to work together to establish an adolescent suicide prevention program on the reservation in 1990.17 second and third leading causes of death, respectively, among American Indians/Alaska Natives aged 15–24 years, with unintentional injury and adverse effects of trauma combined being the leading cause of death.25,26 In the same time period, suicide rates among American Indians/Alaska Natives aged 15–24 years were consistently 2 times higher than those among all American 15- to 24-year-olds.3,25 However, suicide rates vary from tribe to tribe,20,21 with higher rates in Western states.25 They also vary over time in individual AIAN communities.15,22–23
In 1988, the annual rate of suicide and suicide attempts combined for the Western Athabaskan Tribal Nation was 15 times higher than the US rate and 5 times higher than rates for other New Mexico American Indians/Alaska Natives.23 From 1957 through 2000, suicide death rates on this reservation fluctuated in 6- to 8-year cycles.20–23 The Western Athabaskan Tribal Nation is rural and isolated, with 90% of the population living on the reservation, primarily in a single town. In 1990 and 2000, the total population served by the IHS on this reservation numbered 2639 and 3047, respectively. In 1990 and 2000, respectively, the population targeted by the suicidal behavior prevention program comprised 284 and 291 youths aged 10 to 14 years, 261 and 293 aged 15 to 19 years, and 224 and 245 aged 20 to 24 years23 (IHS Office of Program Planning and Evaluation, unpublished program data, July 23, 2003). Eighty percent of those aged 16 years or older were unemployed, with some seasonal employment from firefighting, hunting and fishing guiding, and agriculture (P. Serna, unpublished data, 1991).
In 1989, the IHS provided initial funding for a small model Adolescent Suicide Prevention Project. The IHS designed and implemented the project in collaboration with tribal officials in 1990 and funded it through 1994. During that time, it was the only active project in a New Mexico community specifically designed for suicide intervention and prevention (P. Serna, unpublished data, 1991; Western Athabaskan Tribal Nation, unpublished data, 2003; IHS Office of Program Planning and Evaluation, unpublished program data, July 23, 2003; K. Gaylord, MA, injury prevention manager, Office of Injury Prevention, New Mexico State Department of Health, oral communication, July 8, 2003). With grants from various sources, the project developed into a more broadly focused program; it is now the Department of Behavioral Health of the Western Athabaskan Tribal Nation, with an annual budget of more than $1 million.
The program focused primarily on 10- to 19-year-olds, the population in this community identified by prior research as most at risk for developing symptoms of self-destruction.16,20,21 Five years into the project, specific re-education and awareness-raising activities for the 20- to 24-year-old age group were added. The goals of the program were to reduce the incidence of adolescent suicides and suicide attempts and to increase community education and awareness about suicide and related behavioral issues, such as child abuse and neglect, family violence, trauma, and alcohol and substance abuse (P. Serna, unpublished data, 1991). All levels of prevention (universal, selective, and indicated)34 were targeted in program activities. Key components were based on the following program goals and objectives: (1) identifying suicide risk factors specific to the Western Athabaskan Tribal Nation that may be applicable to other AIAN communities; (2) identifying specific individuals and families at high risk for suicide, violence, and mental health problems; (3) identifying and implementing prevention activities to target high-risk individuals, families, and groups; (4) providing direct mental health services to high-risk individuals, families, and groups; and (5) implementing a communitywide systems approach to enhance community knowledge and awareness (P. Serna, unpublished data, 1991). A broad, community-wide systems suicide prevention model was developed4,5 that solicited active involvement from key constituencies—tribal leadership, health care providers, parents, elders, youths, and clients—in its design and implementation. The community planning process35 had a broad effect on other public institutions of the reservation, such as those involved with judicial, social service, and health program policies.
More than 50 interactive community workgroup sessions were held to examine the following questions: What are the problems and issues in the community? What are the barriers to resolving these problems? What can be done to solve problems and overcome barriers?
At each meeting, all statements and comments were recorded, and these transcribed notes were subsequently compiled into a single document and distributed throughout the community. This document formed the foundation for program components and the development and implementation of the Western Athabaskan Tribal Nation’s judicial and program policies, such as a domestic violence code and a domestic violence and child abuse prevention program. Interestingly, suicide itself was not one of the most important problems identified by the community. Instead, community members stated that, because many of the problems identified could lead to suicide, suicide could not be addressed in isolation. To prevent suicide, underlying issues of alcoholism, domestic violence, child abuse, and unemployment must also be confronted. Community meetings were held in conjunction with a community mobilization project,35 sponsored by the IHS in collaboration with Rutgers University, and continued to be held on a regular basis long after the mobilization project was completed.
The model Adolescent Suicide Prevention Project had the following integrated program components: surveillance through constant data and information gathering; screening/clinical interventions with extensive outreach in conventional institutions (health clinics, schools, and social welfare programs) and unconventional settings (outdoor venues where troubled youths and alcohol abusers frequently congregate, community functions such as traditional and modern dances); social services (child and adult welfare activities); school-based prevention programs on topics including general life skills development14; and community education for adults and youths on general topics (e.g., parenting) and specific topics (e.g., the nature of self-destructive behaviors). Neighborhood volunteers of various ages were chosen as “natural helpers” to engage in peer training, personal and program advocacy, referral of clients for professional mental health services, and provision of counseling to people who preferred to seek help and assistance from knowledgeable and trusted laypersons in less formal settings.27–29 Professional mental health staff worked as a team with the natural helpers, and these staff often provided services in unconventional settings in the community (e.g., in cars or outdoors) to avoid feelings of discomfort that might arise in visiting the mental health program offices.
Staff growth was substantial and constant throughout the evaluation period. Before 1989, the IHS employed 1 full-time mental health technician and contracted for the services of 1 master’s-level counselor and 1 doctoral-level (PhD) psychologist 1 day per week. As part of the Adolescent Suicide Prevention Project, the tribe hired 1 full-time master’s-level social worker and increased the psychologist’s time to 3 days per week in 1989. In 1992, staff increased to 5 full-time positions (82% clinical). By 1996, funding for child abuse, fetal alcohol syndrome, and domestic violence prevention activities and a contract with the IHS for mental health services increased the full-time support staff to 12. In 1997, the tribe entered into another contract with the Bureau of Indian Affairs for additional clinical social workers for child and adult welfare and financial services. In 2000, the behavioral health program had a staff of 33, including support personnel. In 2001, the tribe merged the substance abuse program with the mental health and social services functions to form the Department of Behavioral Health Department of the Western Athabaskan Tribal Nation, and project staff increased to 57 positions, including the director, the clinical director, a psychiatrist 3 days per week, and 21 clinical positions. The department encompasses 19 positions for an inpatient social detoxification program; 5 positions for maintenance/transportation services; and 9 positions for support services such as accountants, medical records personnel, receptionists, and secretaries. Most of these people also assist in public education and other prevention activities.
METHODS
Project data (i.e., clinical record reviews, lists of prevention activities, biannual reports) were maintained for recordkeeping, and systematic analyses of these data were conducted. Program evaluation has been integral in shaping public health initiatives; 3 external evaluators have produced 3 formal evaluations of the prevention program.23,24,31,32
The following definitions have been used throughout the operation of the prevention program. Suicide attempts are defined as life-threatening, self-inflicted injuries that in the absence of medical intervention would result in death. Suicide gestures are behaviors that are not in themselves physically life-threatening but that require intervention because of their self-destructive intent. Suicide completions are acts of intentional self-inflicted injury that result in death.
Each nonfatal suicidal act is classified through staff consultation in case conferences. For example, the behavior of a client who talks about killing himself, engages in behavior leading to his arrest and detention in jail, and in his cell removes his socks and ties them around his neck—but then neither attaches the socks to a fixed object nor tightens them with any tool or implement—would be classified as a suicidal gesture. By contrast, the behavior of a client who ingests overdose quantities of 1 or more medications and then drives to an isolated spot on the reservation would be classified as a suicide attempt, even if he leaves the empty bottle where it can be noticed or found by others. More serious attempts could involve a firearm or attempted hanging, which, because the client flinched when the trigger was pulled or the neck restraint was faulty, he survived. The professional staff conducts case reviews, held as roundtable discussions on a weekly basis, with staff discussing issues of trauma or concerns about clients. These peer reviews assist in coordination of services, development of treatment plans, referral for additional services, and final diagnosis. The program’s director and psychologist have been with the program since its inception, providing continuity of definition and direction. Data on completed suicides are recorded by the local IHS clinic and verified by the State Office of Medical Investigation, which investigates all sudden and unexplained deaths.
Descriptive analyses for 2 years before program implementation and for 13 years of the program used frequencies, percentages, and rates. Graphic analyses in Figures 1 ▶ and 2 ▶ were performed with Microsoft Excel (Microsoft Corp, Redmond, Wash), and simple linear regression analyses in Table 3 ▶ were performed with SPSS Version 10 (SPSS Inc, Chicago, Ill). Where linear regression was applied to the data in Table 3 ▶, the dependent variables were annual frequencies of gestures, attempts, and completions separately and of gestures and attempts combined among selected age groups and among all age groups combined. The frequencies of the specific self-destructive behaviors are presented in Tables 1 ▶ and 2 ▶ as 2-year averages and as means per year to ease the reading and interpretation of trends. The independent variable was time in years.
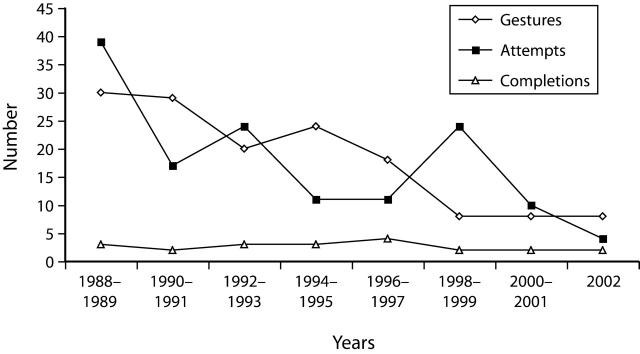
FIGURE 1—
Suicide gestures, attempts, and completions among members of the Western Athabaskan Tribal Nation.
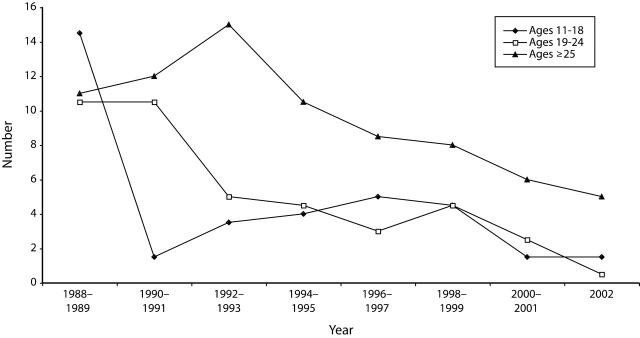
FIGURE 2—
Age-specific total suicide gestures and suicide attempts among members of the Western Athabaskan Tribal Nation.
TABLE 3—
Results of Simple Independent Linear Regression Analysis Estimating Effects Over Time of a Model Adolescent Suicide Prevention Program: Western Athabaskan Tribal Nation, 1988–2002
| Variable | Adjusted R2 | SE | Df | β | t | P |
| Individual suicidal behaviors | ||||||
| Gestures | .595 | 3.01 | 14 | −.790 | −4.65 | .000 |
| Attempts | .332 | 4.54 | 14 | −.609 | −2.77 | .016 |
| Completions | .051 | 0.84 | 14 | −.156 | −.057 | .578 (NS) |
| Suicidal gestures and attempts combined, by age group | ||||||
| 11–18 y | .211 | 4.03 | 14 | −.517 | −2.18 | .048 |
| 19–24 y | .553 | 2.50 | 14 | −.765 | −4.28 | .001 |
| ≥ 25 y | .185 | 3.48 | 14 | −.493 | −2.05 | .062 (NS) |
| All ages combined | .746 | 4.03 | 14 | −.874 | −6.48 | .000 |
| Total self-destructive acts (including suicide completions) | .729 | 4.28 | 14 | −.865 | −6.21 | .000 |
Note. NS = not significant.
TABLE 1—
Number (and Proportion Female) of Suicidal Gestures, Attempts, and Completions Among All Ages Combined, by 2-Year Period: Western Athabaskan Tribal Nation, 1988–2002
| Individual Suicidal Behaviors | ||||||||
| Gestures | Attempts | Completions | Total Self-Destructive Acts (Including Suicide Completions) | |||||
| Years | No. (% Female) | Mean No. per Year | No. (% Female) | Mean No. per Year | No. (% Female) | Mean No. per Year | No. | Mean No. per Year |
| 1988–1989 | 30 (66.7) | 15.0 | 39 (51.3) | 19.5 | 3 (0.0) | 1.5 | 72 | 36 |
| 1990–1991 | 29 (55.2) | 14.5 | 17 (29.4) | 8.5 | 2 (0.0) | 1.0 | 48 | 24 |
| 1992–1993 | 20 (55.0) | 10.0 | 24 (41.7) | 12.0 | 3 (0.0) | 1.5 | 47 | 23.5 |
| 1994–1995 | 24 (41.7) | 12.0 | 11 (45.5) | 5.5 | 3 (0.0) | 1.5 | 38 | 19 |
| 1996–1997 | 18 (44.4) | 9.0 | 11 (36.4) | 5.5 | 4 (0.0) | 2.0 | 33 | 16.5 |
| 1998–1999 | 8 (62.5) | 4.0 | 24 (58.3) | 12.0 | 2 (0.0) | 1.0 | 34 | 17 |
| 2000–2001 | 8 (37.5) | 4.0 | 10 (50.0) | 5.0 | 2 (0.0) | 1.0 | 20 | 10 |
| 2002 | 8 (75.0) | 8.0 | 4 (100.0) | 4.0 | 2 (50.0) | 2.0 | 14 | 14 |
| Total | 145 (54.5) | 9.7 | 140 (47.9) | 9.3 | 21 (4.8) | 1.4 | 306 | 20.4 |
TABLE 2—
Annual Number of Suicidal Gestures and Attempts (Combined), by Year and Age Group: Western Athabaskan Tribal Nation, 1988–2002
| Annual Suicidal Gestures and Attempts Combineda | ||||
| Age Group | ||||
| Years | 11–18 y | 19–24 y | ≥25 y | All Ages Combined |
| 1988–1989 | 29 (14.5) | 21 (10.5) | 22 (11) | 72 (36) |
| 1990–1991 | 3 (1.5) | 21 (10.5) | 24 (12) | 48 (24) |
| 1992–1993 | 7 (3.5) | 10 (5.0) | 30 (15) | 47 (23.5) |
| 1994–1995 | 8 (4.0) | 9 (4.5) | 21 (10.5) | 38 (19) |
| 1996–1997 | 10 (5.0) | 6 (3.0) | 17 (8.5) | 33 (17.5) |
| 1998–1999 | 9 (4.5) | 9 (4.5) | 16 (8.0) | 34 (17) |
| 2000–2001 | 3 (1.5) | 5 (2.5) | 12 (6.0) | 20 (10) |
| 2002 | 3 (1.5) | 1 (0.5) | 10 (5.0) | 14 (14) |
| Total (1988–2002) | 72 (4.8) | 82 (5.5) | 152 (10.1) | 306 (20.4) |
aNumbers are for indicated 2-year period and yearly average (in parentheses).
RESULTS
A steady reduction in suicidal gestures and attempts was recorded throughout the course of the program (Tables 1 ▶ and 2 ▶). Annual averages dropped from 15 gestures and 19.5 attempts before the program began (1988–1989) to 14.5 gestures and 8.5 attempts during the first 2 years of the program (1990–1991); annual averages dropped further to lows of 4.0 gestures (during 1998–2001) and 4.0 attempts (during 2002). No decrease or increase occurred in suicide completions, which remained at 1 to 2 per year throughout the period 1988 to 2002. Overall, the annual mean number of total self-destructive acts dropped from 36 to 14 between 1988 and 2002, an absolute drop of 61.1%. Figure 1 ▶ shows the trajectory of decline in gestures and attempts.
Fifty-five percent of gestures, 48% of attempts, and 5% of completions occurred among women. Suicidal gestures and attempts were common among both sexes, but suicide deaths occurred almost exclusively among men (95%).
Alcohol involvement and family issues linked to all 3 types of self-destructive behavior are not presented in the tables. Two thirds (66.7%) of all self-destructive acts on the Western Athabaskan Tribal Nation reservation were alcohol-related, similar to the proportion for suicide completions among all New Mexico American Indians (69%) but lower than the proportion for suicide completions among all Western Athabaskans in New Mexico (83%).19 Most suicidal behavior (95.4%) occurred among people who had a significant family history of trauma (e.g., family disruption, violent death of relatives, abuse or neglect); 86.3% of self-destructive individuals experienced significant individual trauma. Most suicidal acts (68%) occurred among unemployed persons (aged 16 years and older).
Because the targeted age group was youths aged 11 to 18 years, the most immediate effect was expected in this group, and with a lasting effect on individuals and families, one would expect a gradual change in suicidal behavior among older age groups as these youths age. In 1988 to 1989, before the program began, the annual frequency of gestures and attempts for 11- to 18-year-olds was 14.5; this number decreased to 1.5 during the first 2 years of the program (1990–1991), rose briefly to 5.0 in 1996 to 1997, but returned to 1.5 during the period 2000 to 2002, an absolute reduction of 89.7% (Tables 1 ▶ and 2 ▶). The decrease in annual frequency of gestures and attempts occurred later among 19- to 24-year-olds, who were not intensively targeted, but as targeted youths aged, a positive program effect was observed. The annual frequency of gestures and attempts of 10.5 remained unchanged during the first 2 years of the program but subsequently declined to 2.5 (in 2000–2001) and to 0.5 (in 2002); these declines represent absolute reductions of 76.2% and 90.2%, respectively.
As expected, because young adults aged 25 years and older were not specifically targeted by the prevention program, the slowest and smallest declines in total self-destructive acts was in this age group. Any program effect could only have come later, as targeted youths aged into this group or were influenced by universal prevention (e.g., education, community awareness, social change). Frequencies of combined gestures and attempts in this group were highest in 1992 and 1993 (the third and fourth years of the program), at 15 per year, dropping to 5.0 by 2002, as illustrated in Figure 2 ▶. Thus, suicidal behavior rates remained highest in the nontargeted age group of 25 years and older.
Regression analyses showed that the clearest drop in frequency of occurrence was for suicidal gestures (R2 = .595) (Table 3 ▶). A steep, significant downward slope (β = −.790, P = .000) in suicidal gestures was seen over time, with 59.5% of the variance explained by the existence of the program. Suicide attempts were also significantly lowered (R2 = .322, β = −.609, P = .016). Suicide completions were unaffected. Young adults aged 19 to 24 years had the greatest drop in combined gestures and attempts (R2 = .533, β = −.765, P = .001). The frequency of gestures and attempts also declined significantly among youths aged 11 to 18 (R2 = .211, β = −.517, P = .048), but not among adults aged 25 years and older. For all age groups combined, rates of self-destructive behavior showed significant effects from the program regardless of whether suicide completions were included in the analysis (P = .000). The regression analysis indicates that the frequency of total self-destructive acts declined by 73% (R2 = .729; β = −.865) over the entire span of the program.
DISCUSSION
The consistency and timing of reduction in suicidal behavior correlated with the development and delivery of prevention program interventions in this small AIAN community, indicating that prevention efforts were likely successful in reducing suicidal behavior. We believe that this success is owed to the program’s public health approach, which included mental health services integrated into a comprehensive continuum of services that target other behavioral health topics at all levels of prevention.34 Lessons learned from this program are as follows. First, a suicide prevention program should not focus on a limited range of self-destructive behaviors; rather, it must include an emphasis on root conditions and an array of social, psychological, and developmental issues.1–5 Second, community involvement from the beginning is critical in developing strategies with which to address issues identified in a culturally, environmentally, and clinically appropriate manner. Third, flexibility in program development and implementation is essential, and program development should be based on continuous evaluation and feedback from community and program staff. Therefore, objectives and activities may shift while goals remain the same. Constant vigilance is necessary for maintaining a public health–focused suicide prevention program, as well as program and staff development, community relations, resource development, and administration.
We believe that the temporal association between program delivery and reduction in suicidal behavior is suggestive of a causal association. However, one can hypothesize alternative explanations for this trend. One explanation is that suicidal youths might have left the reservation, thus reducing the number of those who were high risk and independently lowering the frequency of self-destructive behaviors during the study period. Although this explanation may account for trends among other rural populations, such a trend did not occur in the Western Athabaskan Tribal Nation. At any given time, 90% of the enrolled population of the tribe is on the reservation. Approximately 54% of the population was younger than 21 years. This isolated tribal nation is neither geographically nor socially mobile. A second possible explanation is that rapid improvement in social and economic conditions might have affected the population,36 reducing suicidal behavior. However, the tribe’s hotel and casino, developed in the early 1990s, are small and have been among the least successful in the Southwest, primarily because of the isolation of the community from any substantial population center. No substantial growth has occurred in the economic sector. Therefore, the most likely explanation for the observed reduction in suicidal behavior is the presence and expansion of the behavioral health program and the comprehensive mental health, suicide prevention, and clinical services it provides.
Although we observed a reduction in suicide gestures and attempts, suicide deaths remained the same for all ages combined. However, most suicides in the community occur among people in their late 20s and in their 30s. Furthermore, there is some evidence that suicide completions may have decreased for the target population,23 although the numbers are too small for statistical inference.
Because most suicide completions among New Mexico American Indians have historically occurred among tribal members younger than 35 years,8,22,23 have frequently involved alcohol,19 have been by firearms or hanging,22,23 and have been characterized as impulsive,37 one would expect suicide completions to be more resistant to programmatic intervention and prevention than gestures and attempts. A potentially useful conceptualization in this regard, appearing in both the general and the AIAN-specific literature,37–39 is the classification of suicidal behavior as either chronic or acute. Chronic suicidal behavior, in which the individual progresses steadily through a pattern of self-destructive thoughts and acts of increasing severity from gestures to attempts to eventual suicide, is more common in the general population (particularly among older people) than is acute ideation and suicidal behavior, in which no obvious progression precedes the impulsive act. It appears from our evaluation of the suicide prevention program in the Western Athabaskan Tribal Nation that this program may be most successful in changing the path of chronic suicidal behavior but may have minimal or no effect on acute suicidal behavior. However, no increase in suicide completions occurred on the reservation during the period of the program. In the past, the tribe in our study registered significant increases in the rate of suicide in 6- to 8-year cycles.20,21,23 Whether the program prevented such a cyclical upswing in suicide completion requires further analysis with larger numbers. Ethnographic analysis is also needed to describe program functioning and how suicide was viewed in the community before, during, and after the program. For example, using ethnographic studies elsewhere in the Southwest, Levy and Kunitz analyzed the ethnic meanings of suicidal behavior among the Hopi and uncovered an association between completed suicide and other self-destructive behavior and marriages unapproved by traditional values and cultural leaders.33 Uncovering similar cultural and social factors among the Western Athabaskan people studied here may explain the exact underlying themes or mechanisms that allowed the program to work effectively.
This AIAN community is a small and isolated one, which allows researchers relatively easy access to all community members. The longevity and growth of the evaluated program is uncommon in the American Indian context. Typically, suicide prevention initiatives are not sustained because of limited financial resources, demands on public health staff time and energy, changes in personnel, and the waning of interest once a suicidal cluster subsides. Recently, the US Commission on Civil Rights reported that federal resources directed to AIAN communities have not been sufficient to address these communities’ basic and very urgent needs.40 The commission cited health care needs, as well as the need to develop the tribal funding and infrastructure without which public health services cannot be delivered. The suicide prevention program described here is unique in that its development and funding have been increased and maintained over an extended period of time. Importantly, there was continuity of focus and emphasis on suicide prevention by key staff members who remained with the program throughout the period evaluated. The components of this effort can be adapted to larger tribal groups, because they include sound public health theory and practice, cultural relevance, and integration into the tribal infrastructure. Specifically, these components include local surveillance and outreach, careful record keeping and ongoing evaluation, a strong behavioral health base, school and community-based education, integration of violence and substance abuse prevention services, a team approach, and constant vigilance.
On the basis of the positive results reported here, we believe that other AIAN communities can develop similar programs and be equally successful in adopting a public health approach to suicide prevention. If federal and other funds become available to other tribes, the applicability of this model intervention can be tested among larger tribal communities. The program may also serve as a model for non-AIAN communities seeking to adopt a public health approach to preventing self-destructive behaviors.
Acknowledgments
This program evaluation research was supported in part by the US Indian Health Service (grant 242-95-0022) and the Centers for Disease Control and Prevention, as well as by allocations from the Western Athabaskan Tribal Nation.
We are grateful to the Western Athabaskan Tribal Council for their support of this program. We also thank all who have contributed to this project and the research and who have created a successful program, including Debra Hurt, Ricardo Gonzales, PhD, Michael Biernoff, MD, Nancy Van Winkle, PhD, Everett Vigil, Denton Garcia, and all the staff of Western Athabaskan Behavioral Health Program.
JoAnn Pappalardo of the Indian Health Service provided population data for the article. David Buckley assisted in the preparation of the graphics and data analysis and in the corrections for various drafts of the article. Phyllis Trujillo coordinated the schedules and communicated between the various authors for the entire length of this prevention project and typed parts of the article and the tables for the article.
Human Participant Protection Institutional review of all research protocols was carried out and approved by the Indian Health Service Albuquerque Area and National Boards. In addition, the Western Athabaskan Tribal Council and Tribal Health Board approved the original version of this article.
Peer Reviewed
Contributors P.A. May was the principal investigator and codesigner of the prevention program evaluation. P. Serna directed the prevention program, instituted the program components and the evaluation plan, and oversaw the routine collection of all data during the project period described in this report. P. Serna, L. Hurt, and L. DeBruyn cowrote the program description portion. L. Hurt was the clinical director of the prevention program, and L. DeBruyn was with the Indian Health Service and subsequently the Centers for Disease Control and Prevention and provided direct consultation to the program.
Note. The opinions expressed by the authors are theirs and do not necessarily represent those of the Indian Health Service, the Western Athabaskan Tribal Nation, or the Centers for Disease Control and Prevention.
References
- 1.The Surgeon General’s Call to Action to Prevent Suicide. Washington, DC: US Public Health Service; 1999.
- 2.National Strategy for Suicide Prevention: Goals and Objective for Action. Washington, DC: US Public Health Service; 2002. [PubMed]
- 3.Goldsmith SK, Pellmar TC, Kleinman AM, Bunney WE, eds. Reducing Suicide: A National Imperative. Washington, DC: National Academy Press; 2002. [PubMed]
- 4.Knox KL, Conwell Y, Caine ED. If suicide is a public health problem, what are we doing to prevent it? Am J Public Health.2004;94:37–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sanddal ND, Sanddal TL, Berman AL, Silverman MM. A general systems approach to suicide prevention: lessons learned from cardiac prevention and control. Suicide Life Threat Behav.2003;33:341–352. [DOI] [PubMed] [Google Scholar]
- 6.Dizmang LH, Watson J, May PA, Bopp J. Adolescent suicide at an Indian reservation. Am J Orthopsychiatry.1974;44:43–49. [DOI] [PubMed] [Google Scholar]
- 7.Shore JH, Bopp JE, Waller TR, Dawes JW. A suicide prevention center on an Indian reservation. Am J Psychiatry.2001;128:91–96. [DOI] [PubMed] [Google Scholar]
- 8.May PA. Suicide and self-destruction among American Indian youths. Am Indian Alsk Native Ment Health Res.1987;1:52–69. [PubMed] [Google Scholar]
- 9.Tower M. A suicide epidemic in an American Indian community. Am Indian Alsk Native Ment Health Res.1989;3:34–44. [DOI] [PubMed] [Google Scholar]
- 10.Bechtold DW. Indian adolescent suicide: clinical and developmental considerations. Am Indian Alsk Native Ment Health Res Monogr Ser.1994;4:71–80. [DOI] [PubMed] [Google Scholar]
- 11.Bee-Gates D, Howard-Pitney B, LaFramboise TD, Rowe W. Help-seeking behavior among Native American Indian high school students. Prof Psychol Res Pr.1996;27:495–499. [Google Scholar]
- 12.Claymore BJ. A public health approach to suicide attempts on a Sioux reservation. Am Indian Alsk Native Ment Health Res.1988;1:19–24. [DOI] [PubMed] [Google Scholar]
- 13.LaFromboise TD. American Indian Life Skills Development Curriculum. Madison, Wis: University of Wisconsin Press; 1996.
- 14.LaFromboise TD, Howard-Pitney B. The Zuni life skills development curriculum: description and evaluation of a suicide prevention program. J Couns Psychol.1995;42:479–486. [Google Scholar]
- 15.Thompson JW, Walker RD. Adolescent suicide among American Indians and Alaska Natives. Psychiatr Ann.1990;20:128–133. [Google Scholar]
- 16.May PA. Suicide and suicide attempts among American Indians and Alaska Natives: a bibliography. Omega.1990;21:199–214. [Google Scholar]
- 17.DeBruyn LM, Hymbaugh K, Simpson D, Wilkins B, Nelson S. When communities are in crisis: planning for response to suicides and suicide attempts among American Indian tribes. Am Indian Alsk Native Ment Health Res Monogr Ser.1994;4:223–234. [DOI] [PubMed] [Google Scholar]
- 18.Middlebrook DL, LeMaster PL, Beals J, Novins DK, Manson SM. Suicide prevention in American Indian and Alaska Native communities: a critical review of programs. Suicide Life Threat Behav.2001;31(suppl): 132–139. [DOI] [PubMed] [Google Scholar]
- 19.May PA, Van Winkle NW, Williams M, McFeeley PJ, DeBruyn LM, Serna P. Alcohol and suicide death among American Indians of New Mexico: 1980–1998. Suicide Life Threat Behav.2002;32:240–255. [DOI] [PubMed] [Google Scholar]
- 20.Van Winkle NW, May PA. Native American suicide in New Mexico, 1957–1979: a comparative study. Hum Organ.1986;45:296–309. [DOI] [PubMed] [Google Scholar]
- 21.Van Winkle NW, May PA. An update on Native American suicide in New Mexico, 1980–1987. Hum Organ.1993;52:304–315. [DOI] [PubMed] [Google Scholar]
- 22.May PA, Van Winkle NW. Durkheim’s suicide theory and its applicability to contemporary American Indians and Alaska Natives. In: Lester D, ed. Emile Durkheim: Le Suicide 100 Years Later. Philadelphia, Pa: Charles Press; 1994:296–318.
- 23.Van Winkle NW, Williams M. Evaluation of the National Model Adolescent Suicide Prevention Project: A Comparison of Suicide Rates Among New Mexico American Indian Tribes, 1980–1998. Tulsa, Okla: Oklahoma State University School of Osteopathic Medicine; 2001.
- 24.DeBruyn LM, May PA, O’Brien M. Suicide Intervention and Prevention: Evaluation of Community-Based Programs in Three American Indian Communities. Atlanta, Ga: Division of Injury Control, US Centers for Disease Control and Prevention; 1997.
- 25.Web-based Injury Statistics Query and Reporting System (WISQARS) Web site. Atlanta, Ga: National Center for Injury Prevention and Control, Centers for Disease Control and Prevention. Available at: http://www.cdc.gov/ncipc/wisqars. Accessed October 24, 2002.
- 26.Indian Health Service. Trends in Indian Health, 1998–1999. Washington, DC: US Dept of Health and Human Services; 2001.
- 27.Forbes NE. The state’s role in suicide prevention programs for Alaska Native youth. Am Indian Alsk Native Ment Health Res Monogr Ser.1994;4:235–249. [DOI] [PubMed] [Google Scholar]
- 28.Fox J, Manitonabi D, Ward JA. An Indian community with a high suicide rate: five years after. Can J Psychiatry.1984;29:425–427. [DOI] [PubMed] [Google Scholar]
- 29.Rogers DD. Community crisis intervention in suicide epidemics. Arctic Med Res.1991;50(suppl): 276–280. [PubMed] [Google Scholar]
- 30.Ward JA. Preventive implications of a Native mental health program: focus on suicide and violent death. J Prev Psychiatry.1984;2:371–385. [Google Scholar]
- 31.Centers for Disease Control and Prevention. Suicide prevention evaluation in a Western Athabaskan American Indian tribe: New Mexico, 1988–1997. MMWR Morbid Mortal Wkly Rep.1998;47:257–261. [PubMed] [Google Scholar]
- 32.May PA, Del Vecchio A. National Model Adolescent Suicide Prevention Project: Evaluation Report to the Western Athabaskan Tribe. Albuquerque, NM: Center on Alcoholism, Substance Abuse and Addictions, University of New Mexico; 1994.
- 33.Levy JE, Kunitz SJ. A suicide prevention program for Hopi youth. Soc Sci Med.1987;25:931–940. [DOI] [PubMed] [Google Scholar]
- 34.Institute of Medicine. Reducing Risks for Mental Disorders: Frontiers for Preventive Intervention Research. Washington, DC: National Academy Press; 1994. [PubMed]
- 35.Chavis DM, Speer P, Reznick I, Zippay A. Building community capacity to address alcohol and drug abuse. In: Davis RC, Lurgio AJ, Rosenbaum DP, eds. Drugs and the Community. Springfield, Ill: Charles C Thomas; 1993:251–284.
- 36.Costello EJ, Compton S, Keeler G, Angold A. Relationships between poverty and psychopathology: a natural experiment. JAMA.2003;290:2023–2029. [DOI] [PubMed] [Google Scholar]
- 37.Berlin IN. Prevention of adolescent suicide among some Native American tribes. In: Feinstein SC, ed. Adolescent Psychiatry: Developmental and Clinical Studies. Chicago, Ill: University of Chicago Press; 1985:77–93. [PubMed]
- 38.Kehoe JP, Abott AP. Suicide and attempted suicide in the Yukon territories. Can Psychiatr Assoc J.1975;20:15–23. [DOI] [PubMed] [Google Scholar]
- 39.Berlin IN. Suicide among American Indian adolescents: an overview. Suicide Life Threat Behav.1987;17: 218–232. [DOI] [PubMed] [Google Scholar]
- 40.US Commission on Civil Rights. A quiet crisis: federal funding and unmet needs in Indian country. July 2003. Available at: http://www.usccr.gov. Accessed July 17, 2003.