Abstract
Background. The adverse effects of alcohol on the developing human represent a spectrum of structural anomalies and behavioral and neurocognitive disabilities, most accurately termed fetal alcohol spectrum disorders (FASD). The first descriptions in the modern medical literature of a distinctly recognizable pattern of malformations associated with maternal alcohol abuse were reported in 1968 and 1973. Since that time, substantial progress has been made in developing specific criteria for defining and diagnosing this condition. Two sets of diagnostic criteria are now used most widely for evaluation of children with potential diagnoses in the FASD continuum, ie, the 1996 Institute of Medicine (IOM) criteria and the Washington criteria. Although both approaches have improved the clinical delineation of FASD, both suffer from significant drawbacks in their practical application in pediatric practice.
Objective. The purpose of this report is to present specific clarifications of the 1996 IOM criteria for the diagnosis of FASD, to facilitate their practical application in clinical pediatric practice.
Methods. A large cohort of children who were prenatally exposed to alcohol were identified, through active case-ascertainment methods, in 6 Native American communities in the United States and 1 community in the Western Cape Province of South Africa. The children and their families underwent standardized multidisciplinary evaluations, including a dysmorphology examination, developmental and neuropsychologic testing, and a structured maternal interview, which gathered data about prenatal drinking practices and other demographic and family information. Data for these subjects were analyzed, and revisions and clarifications of the existing IOM FASD diagnostic categories were formulated on the basis of the results.
Results. The revised IOM method defined accurately and completely the spectrum of disabilities among the children in our study. On the basis of this experience, we propose specific diagnostic criteria for fetal alcohol syndrome and partial fetal alcohol syndrome. We also define alcohol-related birth defects and alcohol-related neurodevelopmental disorder from a practical standpoint.
Conclusions. The 1996 IOM criteria remain the most appropriate diagnostic approach for children prenatally exposed to alcohol. The proposed revisions presented here make these criteria applicable in clinical pediatric practice. Pediatrics 2005;115:39–47; fetal alcohol syndrome, fetal alcohol spectrum disorders, diagnostic criteria, mental retardation, developmental disabilities.
The adverse effects of alcohol on the developing human represent a spectrum of structural anomalies and behavioral and neurocognitive disabilities, most accurately termed fetal alcohol spectrum disorders (FASD).1 Children at the severe end of the spectrum (with the complete phenotype) have been defined as having the fetal alcohol syndrome (FAS). The societal burden of FASD is immense, in terms of suffering, lost productivity, and excess medical and educational expenses.2 It was estimated that the annual costs of FASD in the United States reached $4 billion by 1998.3 Diagnosing FASD among children and adults historically has presented physicians with a challenge. Cases of even full-blown FAS often go undetected at birth and later in life.4,5 Children with less severe phenotypes in the FASD continuum present an even greater diagnostic challenge, because often the physical signs are more subtle.6 These less severe types of FASD are much more common than FAS, however, and may affect ≥1% of all children born in the United States.7 The range of alcohol damage during fetal development, from mild to severe, is well documented in the medical literature.5,8,9
Despite ancient references to the adverse effects of alcohol on the offspring of drinking women (eg, by Aristotle10 and in the book of Judges 13:411), more recent references provide insight into the lack of recognition of the teratogenic effects of alcohol. Several physician groups in England in the 1700s described children of alcoholics as “weak, feeble, and distempered”12 and “born weak and silly … shriveled and old, as though they had numbered many years.”13 In 1899, Sullivan14 described the offspring of alcoholic women imprisoned in England. He concluded that these women produced children characterized by a pattern of birth defects of increasing severity and higher rates of miscarriage; there was a tendency for healthier infants to be born when gestation occurred in prison (thus indicating abstinence as prevention), these children were not productive members of society as they aged, and male alcoholism was not a factor in producing the abnormalities. Similar epidemiologic patterns were not documented fully until the 1980s and later.5,15-19
Clinically, the discovery of FAS is relatively recent. In 1968, Lemoine et al20 in France reintroduced the apparently ignored, unrecognized, or misunderstood concept of adverse outcomes resulting from fetal alcohol exposure when they published a report that described some of the common problems among >100 children of women who drank heavily. Although the authors documented many of the physical and behavioral patterns among those children, they drew few conclusions. That article did not present definitive diagnostic criteria, and the observations did not lead to recognition of FASD in France or elsewhere in Europe.
Jones, Smith, and colleagues21-23 were the first to describe in detail the consistent pattern of malformations among children of mothers with significant prenatal alcohol intake and to provide diagnostic criteria for the condition they termed FAS. Since the publication of the clinical delineation of FAS, several thousand articles on the effects of prenatal alcohol exposure among human subjects and for a variety of laboratory animals have been published.17
Full-blown FAS denotes a specific pattern of malformations, with a confirmed history of maternal alcohol abuse during pregnancy, prenatal onset of growth deficiency (length and/or weight) that persists postnatally, a specific pattern of minor anomalies of the face, and neurocognitive deficits (Fig 1).5 The need for a term to describe children with less severe phenotypes within the FASD continuum led to the term fetal alcohol effects (FAE). This term was not intended originally to be a diagnostic category but was a population-based term that indicated that certain congenital anomalies and developmental disabilities were observed more often among children of alcoholic women than among children in the general population. Researchers studying animal populations exposed to alcohol prenatally also used the term. Unfortunately, the term FAE was frequently applied to individual children with a variety of problems, solely on the basis of either suspected or confirmed maternal alcohol use during pregnancy. Because this term was used so frequently, some health agencies began to accept FAE as a medical diagnosis for which children could become eligible for educational and financial services.24
Fig 1.
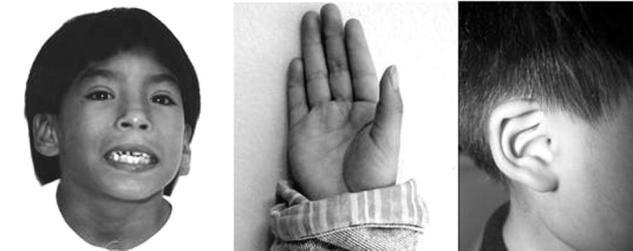
Left, Child with FAS. Short palpebral fissures, a smooth philtrum, and a thin upper lip are evident. Center, “Hockey stick” configuration of the upper palmar crease, a minor anomaly common among children with FAS. Right, “Railroad track” ear.
In 1980, the Fetal Alcohol Study Group of the Research Society on Alcoholism25 emphasized the wide range of effects of alcohol on developing fetuses, with FAS at one end of the spectrum. They proposed that the term possible FAE be used to refer to children who had disabilities that were thought to be related to prenatal alcohol exposure but did not meet the diagnostic criteria for FAS.25 This definition remained problematic, however, because it could not be proved or disproved in any given case. In addition, the vague term FAE allowed for broad interpretation by clinicians, making it clinically useless. For example, it could be applied to any structural, learning, or behavioral problem of an exposed child, regardless of the underlying diagnosis or lack thereof. Such diagnostic imprecision led to frustration among health care providers, parents, and guardians. This frustration led clinicians either to disregard alcohol as a contributing factor for any children's problems or to overdiagnose the contribution of alcohol to such problems, which hampered efforts to determine the actual magnitude of FASD.24
Because the term FAE had gained acceptance by health care agencies, tremendous pressure on clinicians to make this diagnosis often was exerted by parents, foster parents, and schools. Although the positive results of making this diagnosis are well known, the consequences of misdiagnosis frequently have been overlooked. For example, inaccurate diagnosis of an alcohol-related disability may lead to stigmatization of mothers of labeled children, although it may be unclear whether prenatal alcohol exposure led to the children's problems. Misdiagnosis also can lead to inaccurate and potentially damaging labeling and inappropriate treatment and referral by schools and social service agencies. Finally, once a diagnosis of an alcohol-related disability has been made, the search for other causes of an affected child's disabilities often is abandoned. Therefore, an inaccurate diagnosis can result in a lack or premature termination of diagnostic studies to determine the true cause and specific nature of the disabilities.24
In 1995, Aase et al24 argued that the term FAE should be eliminated because of the aforementioned ambiguities. The authors pointed out that the individual known effects of in utero exposure to alcohol together constitute FAS; each component of FAS, such as growth retardation or neurocognitive deficits, is nonspecific, and it is only the combination of all components that allows the definition of FAS. Furthermore, the authors observed that the facial features of FAS encompass a group of minor anomalies or structural variants that can be found as isolated characteristics among normal individuals and families and can be thought of as representing polygenic traits inherited in a multifactorial pattern. Therefore, the significance of these variations from normal lies only in their association with one another in a specific pattern that can be recognized as a specific syndrome. Because the term FAE does not allow for such a consistently recognized pattern, it cannot be applied to specific individuals. Aase et al24 suggested that the term FAE be used only in population or animal studies in which the independent variable is maternal alcohol use during pregnancy.
Although many investigators have attempted to define the findings necessary to make a diagnosis of FAS and the other phenotypes in the FASD continuum, there are 2 major published sets of diagnostic criteria currently used for evaluation and categorization of children prenatally exposed to alcohol. The first set of criteria was presented by the Institute of Medicine (IOM) of the National Academy of Sciences in 1996, after the US Congress mandated a study on FAS. The IOM study group developed 5 diagnostic categories for FAS and alcohol-related effects (Table 1).5
TABLE 1.
Diagnostic Categories Within FASD (1996 IOM Report)5
| FAS with confirmed maternal alcohol exposure |
| FAS without confirmed maternal alcohol exposure |
| Partial FAS with confirmed maternal alcohol exposure |
| ARBD |
| ARND |
There are several problems with the IOM criteria for the diagnosis of FAS and alcohol-related effects as they were formulated in 1996. First, they are vague, with no specific parameters being set forth for diagnosis in each category. Neither the degree of growth deficiency nor the exact facial dysmorphic features required for each category are defined. In addition, the specific behavioral/cognitive phenotype is not characterized, and no guidelines for assessment of the “complex pattern of behavioral or cognitive difficulties” are suggested. Second, assessment of the family and genetic history of each affected child is not addressed adequately. Finally, alcohol-related birth defects (ARBD) and alcohol-related neurodevelopmental disorder (ARND) are not practically defined in a clinical sense.
Because of these concerns, Astley and Clarren6 sought to develop a more objective set of diagnostic criteria for FASD, which were published in 2000. These diagnostic criteria are commonly referred to as the Washington criteria, because they were formulated through reviews of the medical records of 1014 children diagnosed with FAS through the Washington State Fetal Alcohol Syndrome Diagnostic and Prevention Network. Their criteria retain the 4 commonly accepted, key diagnostic features of FAS, ie, growth deficiency, characteristic FAS facial phenotype, central nervous system damage/dysfunction, and alcohol exposure in utero. The degree to which each of these 4 factors is present for any given child is ranked on a 4-point Likert scale, with 1 representing the complete absence of the feature and 4 representing a classic presentation of the feature. Each child is assigned a 4-digit diagnostic code, with each digit corresponding to the degree to which 1 of the 4 main features of FAS is present. Two hundred fiftysix possible combinations (ranging from 1111 to 4444) result and are collapsed into 22 diagnostic categories (termed A through V). The authors of this system noted that, because a number of categories differ only with respect to the amount of prenatal alcohol exposure, there are only 9 unique diagnostic outcomes. These diagnostic outcomes range from no cognitive/behavioral or sentinel physical findings detected to FAS.6 Although the Washington system appears to be extremely accurate in placing each child into a specific diagnostic category within the spectrum of alcohol-associated abnormalities, the myriad of diagnostic categories is confusing and the system is impractical for routine use in clinical practice.
The Washington criteria also suffer from the same ambiguities as the IOM criteria. For example, the Washington criteria place much emphasis on the encephalopathy and neurobehavioral disorder present among affected children. These 2 findings are not specifically defined and, as general terms, they are not unique to the prenatal effects of alcohol on fetal development.26 In addition, the family and genetic background of the child is not adequately integrated into the criteria. Because this highly structured system seems all-encompassing, there is the potential for overdiagnosis of alcohol-related disabilities; any child with a disability who has been exposed to alcohol prenatally can be assigned a diagnostic classification easily, even if the cause of the disability is genetic.
One positive aspect of the Washington criteria is the attempt to define objectively the facial phenotype of FAS. The authors created a pictorial lip/philtrum guide to facilitate objective assessment of the structure of the upper lip and philtrum (Fig 2). This guide depicts 5 categories, ranging from normal findings to features observed in classic FAS. To use the guide for the diagnosis of FAS, the upper lip thinness (lip circularity) and the philtrum smoothness are assessed separately, through comparison of the child's face with the guide. A score of 1 is considered completely normal, whereas a score of 5 is most indicative of FAS.6
Fig 2.
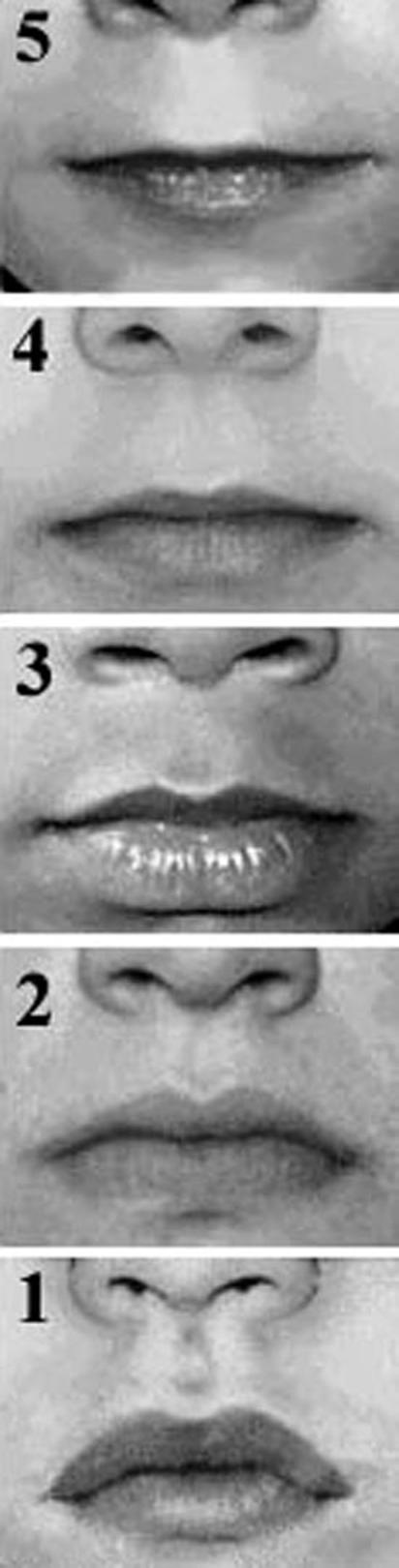
Lip-philtrum guide. The smoothness of the philtrum and the thinness of the upper lip are assessed independently. Scores of 4 or 5 are consistent with FASD. Reprinted with permission from ref 6.
An ideal classification system for FASD would allow accurate diagnoses of affected individuals by minimizing the false-positive and false-negative rates, precisely defining diagnostic categories, taking genetic and family histories into account, using a multidisciplinary approach (including careful behavioral and neuropsychologic assessments), and creating straightforward, understandable, practical terms that could be applied easily in local clinical settings. On the basis of our extensive experience with alcohol-exposed children and adults in the United States and South Africa, we propose a modification of the 1996 IOM diagnostic criteria for FASD, making them more specific and clinically applicable in general pediatric practice. Our aim is to improve both the reliability and validity of diagnoses within the FASD continuum.
METHODS
The study participants for whom data were gathered for formulation of the proposed revisions of the 1996 IOM diagnostic criteria for FASD were evaluated during a period of 5 years, among high-risk populations in the United States and South Africa. These children were identified with active case-ascertainment methods, from multiple sources. These methods were thoroughly described elsewhere.27,28 The American subjects were from 6 Native American communities and 1 urban population each in Montana, North Dakota, and South Dakota; the South African subjects were enrolled from 1 community in the wine-producing region of the Western Cape. The American children were referred to us because of developmental and/or behavioral problems and possible prenatal alcohol exposure, whereas the South African children were part of a school-based screening program involving all children in first grade in the targeted community.27 All subjects underwent comprehensive multidisciplinary evaluations in 3 areas, ie, (1) growth and structural development (assessed independently by a minimum of 2 dysmorphologists, with a standardized format), (2) neuropsychologic, intellectual, and social development, and (3) maternal risk factors (assessed with a comprehensive maternal interview). Matched control children were examined in a blinded manner. After the data were gathered for all 3 domains, each child was assigned to a FASD diagnostic category or another diagnosis, in a case conference.
For the dysmorphology examinations, each subject underwent independent evaluations by 2 dysmorphologists. A preliminary diagnostic category was assigned on the basis of the data gathered. If there was disagreement between the examiners, then consensus was reached in a case conference. Anthropometric measurements were recorded, including height, weight, head circumference, and palpebral fissure measurements. Three primary facial features were assessed, to allow a decision regarding the facial morphologic features of the subject, ie, palpebral fissure length and the morphologic features of the philtral ridges and upper lip. Palpebral fissure measurements were obtained with a rigid ruler, marked in millimeters, with the examiner seated directly in front of the subject and recording the distance from the medial canthus to the lateral canthus (Fig 3). The morphologic characteristics of each subject's upper lip and philtrum were assessed and scored with the lip/philtrum guide described by Astley and Clarren6 (Fig 2). Independent scores were assigned for the thinness of the upper lip and the prominence or flatness of the philtral ridges. Scores of 4 or 5 were considered to be consistent with FASD. Each anthropometric measurement was plotted against published normative values, to determine its age-specific percentile. For the purposes of this study, a measurement was considered abnormal if it was ≤10th percentile for age. A child was considered growth deficient if either the height or weight was determined to be ≤10th percentile. Similarly, a head circumference was considered deficient if the measurement was ≤10th percentile. Finally, a physical examination was performed, with assessment of both major and minor anomalies.
Fig 3.

Measurement of palpebral fissures. Palpebral fissures are measured in millimeters, with a rigid ruler, with the examiner seated directly in front of the subject. The ruler is canted slightly, to follow the curve of the face. The measurement is taken from the inner canthus to the outer canthus, and results are compared with published normative values.
The subjects underwent a battery of developmental and neuropsychologic tests (see Discussion), including broad measures of IQ and behavioral and social development and narrow-band tests of performance on complex tasks (typified by assessment of higher executive control functioning). Examiners included psychologists, a neuropsychologist, a developmental pediatrician, and an educational diagnostician. Although the specific personnel performing the testing varied among the sites, all examiners were skilled in testing children in the FASD spectrum. On the basis of the data gathered, each subject's neurobehavioral profile was determined to be either consistent or inconsistent with the adverse effects of prenatal alcohol exposure.
Structured interviews of the biological mothers of the subjects were conducted to determine the amount and frequency of alcohol intake during pregnancy. The mothers of the control children were interviewed as maternal control subjects. The interviews contained >300 items that explored childbearing patterns, drinking patterns before, during, and after the index pregnancy, marital and cohabitation patterns, socioeconomic status, demographic factors, social environment, and maternal nutrition (in the South African study). If mothers were deceased or unavailable, then collateral sources and available maternal health sources were sought to substantiate or to contradict a potential history of alcohol abuse during pregnancy. Sealed adoption records are common in the United States, which made data regarding prenatal maternal alcohol use difficult to obtain for many of the American subjects. In South Africa, however, the investigators had access to >80% of birth mothers, making the assessment of prenatal maternal alcohol use easier for that population.29
RESULTS
Of the 1500 children evaluated, 164 children with a potential FASD diagnosis were identified, ie, 72 Native American children and 92 South African children. At the onset of the study, subjects were assigned a diagnosis of FAS, not FAS, or diagnosis deferred. From our experience with these 164 children, we formulated more-precise clarifications of the 1996 IOM diagnostic guidelines (Table 2). Then the original diagnoses were revisited and modified, if necessary, with the revised IOM criteria.
TABLE 2.
Proposed Clarification of the 1996 IOM Criteria for Diagnosis of FASD
|
In the proposed diagnostic criteria, the following considerations apply. Each of the categories assumes that genetic and medical assessment has ruled out a phenocopy, including other genetic and malformation syndromes. Confirmed maternal alcohol exposure is defined as a pattern of excessive intake characterized by substantial regular intake or heavy episodic drinking. Evidence of this pattern may include frequent episodes of intoxication, development of tolerance or withdrawal, social problems related to drinking, legal problems related to drinking, engaging in physically hazardous behavior while drinking, or alcohol-related medical problems such as hepatic disease. Confirmation may be from maternal interview or reliable collateral sources.
ARBD and ARND refer to clinical conditions in which there must be a history of maternal alcohol exposure, and in which clinical and/or animal research must link maternal alcohol ingestion to the observed outcome. ARBD encompasses children with major and/or minor structural anomalies who display normal growth and intellectual development. ARND comprises a specific pattern of disordered behavior and development among children with normal growth and structural development.
The proposed revised IOM diagnostic categorizations of the subjects are presented in Table 3, and the clinical findings for each diagnostic category are presented in Table 4. Data in Table 3 were based on the 164 extensively reviewed cases (1998-2003) from the larger pool of 1500 subjects. Data in Table 4 were obtained from a representative group of the 164 extensively reviewed cases. Table 5 presents the research scoring system with which the dysmorphic features observed for each subject were quantified.
TABLE 3.
Diagnostic Reclassification of 164 Native American or South African Children (With a Preliminary Diagnosis of FAS or Not FAS) With the Revised IOM Diagnostic Classification System
| Original Diagnosis |
Revised IOM Diagnosis |
||||
|---|---|---|---|---|---|
| Total No. (%) | No. With Documented Prenatal Alcohol Exposure | No. Without Documented Prenatal Alcohol Exposure | Total No. (%) | ||
| FAS | 97 (59) | FAS | 49 | 10 | 59 (36) |
| Partial FAS | 42 | 10 | 52 (32) | ||
| ARBD | 5 | 5(3) | |||
| ARND | 16 | 16 (10) | |||
| Not FAS | 43 (26) | Not FAS | 17 | 17 (10) | |
| Deferred* | 24 (15) | Deferred* | 15 (9) | ||
| Total | 164 | Total | 164 | ||
A definitive diagnosis has not been assigned and alcohol exposure has not been determined for patients in the deferred category.
TABLE 4.
Summary of Clinical Findings for Each Diagnostic Category (N = 57)
| Mean Dysmorphology Score* | Height Percentile | Weight Percentile | OFC Percentile | Development Score (N = 51) | No. Neuropsychologically Impaired† (N = 32) | No. With Maternal Alcohol Use | |
|---|---|---|---|---|---|---|---|
| FAS | 16.2 | 9.9 | 13.6 | 8.1 | 74.29 | 17 | 20 |
| Partial FAS | 10.32 | 42.6 | 43.7 | 29.3 | 79.2 | 6 | 24 |
| ARBD | 7 | 46.7 | 34.3 | 38.2 | 91 | 0 | 3 |
| ARND | 4.3 | 63.3 | 69.2 | 36.7 | 82.7 | 3 | 3 |
OFC indicates occipitofrontal circumference
See Table 5.
Impairment in executive functioning, with or without cognitive impairment.
TABLE 5.
Dysmorphology Scoring System
| Feature | Points |
|---|---|
| Height <10% | 1 |
| Weight <10% | 2 |
| Occipitofrontal circumference <10% | 3 |
| Inner canthal distance <10% | 0 |
| Palpebral fissure length <10% | 3 |
| Attention-deficit/hyperactivity disorder | 1 |
| Fine motor dysfunction | 1 |
| Midfacial hypoplasia | 2 |
| “Railroad track” ears | 1 |
| Strabismus | 0 |
| Ptosis | 2 |
| Epicanthal folds (nonracial) | 1 |
| Flat nasal bridge | 1 |
| Anteverted nares | 2 |
| Long philtrum | 2 |
| Smooth philtrum | 3 |
| Thin vermilion border of upper lip | 3 |
| Prognathism cardiac murmur | 0 |
| Cardiac malformation (confirmed) | 1 |
| Hypoplastic nails | 0 |
| Decreased pronation/supination of elbow | 2 |
| Clinodactyly of fifth fingers | 1 |
| Camptodactyly | 1 |
| “Hockey stick” palmar creases | 1 |
| Hirsutism | 1 |
| Total possible dysmorphology score | 36 |
The dysmorphology score is a weighted calculation based on assigning points to clinical findings characteristic of FASD (the highest point values are assigned to the cardinal findings of FAS, ie., growth deficiency, microcephaly, short palpebral fissures, smooth philtrum, and thin upper lip). The score provides an objective method of quantifying dysmorphologic features but is not used in assigning clinical diagnoses in the FASD continuum.
DISCUSSION
Our proposed revisions to the IOM diagnostic criteria for FASD represent an attempt to clarify and to operationalize the original IOM diagnostic categories, to allow their practical application in clinical medicine and in population-based FASD research. In addition, it is expected that these diagnostic categories will provide meaningful service to affected children, by specifying each child's strengths and weaknesses as a guide to appropriate treatment planning and intervention recommendations for parents, teachers, and health care providers.
In the proposed clarifications of the IOM criteria, children with FAS (with or without confirmed maternal alcohol exposure) must have abnormalities in all domains, ie, facial dysmorphic features, growth, and brain growth or structure. In the partial FAS category (with or without confirmed maternal alcohol exposure), children must display typical facial dysmorphic features and abnormalities in 1 of the other domains (growth or central nervous system structure or function).
For the proposed clarifications of the 2 diagnoses characterized as alcohol-related effects, maternal alcohol exposure must be documented. The term ARBD is meant to apply to affected children in the FASD continuum who have typical facies, normal growth and development, and specific structural anomalies (either major malformations or a pattern of minor malformations). ARND is meant to apply to children with normal growth and structural development who display a characteristic pattern of behavioral or cognitive abnormalities typical of prenatal alcohol exposure. In this latter category, it is imperative that the neurobehavioral abnormalities not be typical of other individuals in the family who were not exposed prenatally to alcohol. In addition, the abnormalities should not be explained by post-natal environmental influences alone.
Simple IQ tests are inadequate to differentiate children with ARND from those with developmental disabilities resulting from other causes. Despite inconsistencies in reported research on FASD, there is an emerging consensus that children with ARND are markedly impaired in executive functioning, as in the performance of relatively complex tasks, irrespective of the domain of functioning; however, these children perform in the normal range with relatively simple tests. Tests of executive functioning assess the ability of subjects to perform complex tasks that require considerable cognitive efforts (eg, complex problem-solving, planning, judgment, and arithmetic tasks). Examples of tests of executive function that may serve to differentiate children with ARND from normal children and children with other developmental disabilities include Wechsler Intelligence Scale for Children-III mazes (for assessment of planning), the trail-making test (for measurement of shifting of the perceptual set), consonant trigrams (for evaluation of working memory), and the Wisconsin card-sorting test and category test (for assessment of reactive flexibility).30,31
The behavioral profile of children with FASD includes problems with communication and speech (eg, speaking too much and/or too fast and interrupting others), difficulties in personal manner (eg, clumsiness, disorganization, and losing or misplacing things), emotional lability (eg, rapid mood swings and overreacting), motor dysfunction (eg, difficulty playing sports), poor academic performance (eg, poor attention span and difficulty completing tasks), deficient social interactions (eg, lack of awareness of consequences of behavior and poor judgment), and unusual physiologic responses (eg, hyeracusis, hyperactivity, and sleep disturbances).32 Such behavior can be assessed with a number of tools, including the Personal Behaviors Checklist, among others.33
Our clinical experience has demonstrated that FASD must always be a diagnosis of exclusion. Many genetic and malformation syndromes have some of the clinical characteristics of FAS (Fig 4),32 and children with other genetic and dysmorphic syndromes are born as frequently to women who abuse alcohol as they are to other women in the general population. Therefore, a diagnosis in the FASD continuum should not automatically be assigned to a child with disabilities, merely because his or her mother drank alcohol during the pregnancy.
Fig 4.

Patients with genetic disorders who display some of the craniofacial features of FAS. Left, Williams syndrome. Center, De Lange syndrome. Right, VCFS.
For example, FAS shares many common features with velocardiofacial syndrome (VCFS) (associated with a microdeletion of chromosome 22q11). Children with VCFS demonstrate short palpebral fissures, malar hypoplasia, microcephaly, and learning disabilities. However, children with VCFS also can have a broad nasal root with bulbous nasal tip, deficiency of the alae nasi, hypocalcemia, and long slender fingers. Although children with FAS often have congenital heart defects, children with VCFS have a higher prevalence of congenital heart defects, most commonly of the conotruncal type.34 FAS also shares many features with Williams syndrome (caused by a microdeletion of chromosome 7q11). Patients with Williams syndrome may exhibit mild prenatal growth deficiency, microcephaly, short palpebral fissures, a long smooth philtrum, and learning and behavioral problems. In contrast to children with FAS, however, patients with Williams syndrome also usually display periorbital fullness, stellate irises, hallux valgus, hypercalcemia, a distinctive “cocktail party” personality, and congenital heart defects, most commonly supravalvar aortic stenosis or peripheral pulmonic stenosis.34 Blepharophimosis syndrome, an autosomal dominant disorder typified by short palpebral fissures with lateral displacement of the inner canthi, can also be mistaken for FAS. Mental retardation and cardiac defects are variable features of that disorder.34 Dubowitz syndrome is also characterized by prenatal growth deficiency, mental retardation, microcephaly, short palpebral fissures, and ptosis (all of which can be indicative of FAS). However, children with that autosomal recessive condition can also manifest an eczema-like skin eruption, limb anomalies, cryptorchidism, and ocular abnormalities.34 Finally, Cornelia de Lange syndrome, another autosomal dominant genetic condition, shares some features with FAS. Children with de Lange syndrome exhibit prenatal-onset growth deficiency, mental retardation, a long philtrum, and a thin upper lip. However, they also display synophrys, downturned angles of the mouth, and various limb defects, most commonly micromelia.34 These examples are not exhaustive, but they do point out the need to consider other genetic and nongenetic diagnoses for children with disabilities who have had prenatal alcohol exposure.
For the clinical application of these guidelines, if the general pediatrician does not have access to a multidisciplinary FASD diagnostic team, then he or she should first gather historical information about prenatal alcohol exposure for the child in question, either through direct interview of the biological mother or from reliable collateral sources. A family history of similarly affected individuals, learning disabilities, mental retardation, psychiatric disorders, and birth defects should be sought. A careful physical examination should be performed (as outlined previously), ascertaining growth, specific anthropo-metric parameters, and major or minor anomalies. The child should then be referred for psychologic testing, specifically assessment of the learning and behavioral characteristics typical of children in the FASD continuum. After all of the data have been obtained, if there are any characteristics inconsistent with a FASD diagnosis, then referral to a dysmorphologist/clinical geneticist may be indicated. If there is no indication of another genetic or malformation syndrome, then the revised IOM criteria can be applied to categorize a diagnosis within the FASD continuum.
The proposed diagnostic method for FASD has many strengths. (1) These revisions correct the vagueness of the original IOM criteria by defining the degree of growth deficiency and specifying the minor physical anomalies required to make diagnoses in the FASD continuum. (2) ARBD and ARND are specifically defined. (3) The diagnostic approach is multidisciplinary and uses the input of physicians, psychologists, educational diagnosticians, and skilled maternal interviewers in categorizing the disabilities. (4) The approach is evidence based and uses data from previous animal and human studies. (5) Application to our extensive database of children prenatally exposed to alcohol demonstrates that the method is rigorous and accurate. (6) The suggested method is not based only on prenatal alcohol exposure but stresses diagnosis based on elimination of known genetic and malformation syndromes and inclusion based on the pattern of deficits observed among children prenatally exposed to alcohol.
A weakness of the proposed diagnostic approach is that the normative values currently used for growth and facial morphologic features are based largely on white populations. Therefore, the judgment of a skilled physician with experience in examining children from a variety of racial backgrounds is required for application of the criteria across races. There is a need for development of normal height and weight curves and anthropometric data for palpebral fissure lengths for other races. However, in the absence of such specific racial/ethnic group-based data, normal control findings or general clinical experience with the same population must be used. Formulation of lip/philtrum guides for various racial/ethnic groups should lead to improved accuracy in the application of the revised diagnostic criteria.
In addition, our experience indicates that accurate assignment of a diagnosis in the FASD continuum remains problematic for infants and very young children. Although some progress has been made in objective assessment of the effects of prenatal alcohol exposure on growth and morphologic features among newborns, much work remains to be performed.35
Finally, although we have characterized the developmental and neurobehavioral phenotype of children with ARND, children in this category of the FASD continuum currently are the subject of intense study. It is anticipated that this diagnostic classification may be refined as additional research delineates more completely the unique behavioral and developmental phenotype of ARND.
CONCLUSIONS
We have proposed revision and clarification of the 1996 IOM criteria for diagnosis of FASD. Data from our large multiracial cohort of children prenatally exposed to alcohol indicate that this method can be applied easily in clinical practice, thus improving care for affected children and leading to improved precision of clinical and population-based research in FASD.
ACKNOWLEDGMENTS
This research was funded in part by National Institute on Alcohol Abuse and Alcoholism grants R01AA09440 and R01AA11685, the National Institutes of Health Office of Minority Health and Health Disparities, and the Mosbacher Family Distinguished Packard Fellowship.
Special thanks go to our colleagues Irene Lake, Rose Maestas, Paul Dauphinais, Betty R. Poitra, Joan Trottier Alvord, Lorinda Beck, Mary White Country, Karen Goodhart, Renee Fasthorse, Mabel Granados, Jill Plumage, Deborah Henderson, Marjean Magraw, Mary Beth Palmerton, Carol Keaster, Anna-Susan Marais, Lesley Brooke, Julie Croxford, Loretta Hendrichs, and Cudore Snell, all of whom helped set up and maintain the vital referral network that yielded the cases examined in 3 states in the northern United States and in South Africa. We also gratefully acknowledge the assistance of Dr Jon Aase of the University of New Mexico and Dr Karen Hymbaugh of the Centers for Disease Control and Prevention in the development of the dysmorphology scoring system used in this project.
ABBREVIATIONS
- FASD
fetal alcohol spectrum disorders
- FAS
fetal alcohol syndrome
- FAE
fetal alcohol effects
- ARND
alcohol-related neurodevelopmental disorder
- IOM
Institute of Medicine
- VCFS
velocardiofacial syndrome
- ARBD
alcohol-related birth defects
Footnotes
No conflict of interest declared.
REFERENCES
- 1.Barr HM, Streissguth AP. Identifying maternal self-reported alcohol use associated with fetal alcohol spectrum disorders. Alcohol Clin Exp Res. 2001;25:283–287. [PubMed] [Google Scholar]
- 2.Lupton C, Burd L, Harwood R. Cost of fetal alcohol spectrum disorders. Am J Med Genet. 2004;127C:42–50. doi: 10.1002/ajmg.c.30015. [DOI] [PubMed] [Google Scholar]
- 3.Harwood H. Updating Estimates of the Economic Costs of Alcohol Abuse in the United States: Estimates, Updated Methods, and Data: Report Prepared by the Lewin Group. National Institute on Alcohol Abuse and Alcoholism; Bethesda, MD: 2000. [Google Scholar]
- 4.Little BB, Snell LM, Rosenfeld CR, Gilstrap LC, III, Gant NF. Failure to recognize fetal alcohol syndrome in newborn infants. Am J Dis Child. 1990;144:1142–1146. doi: 10.1001/archpedi.1990.02150340088030. [DOI] [PubMed] [Google Scholar]
- 5.Stratton KR, Howe CJ, Battaglia FC, editors. Fetal Alcohol Syndrome: Diagnosis, Epidemiology, Prevention, and Treatment. National Academy Press; Washington, DC: 1996. [Google Scholar]
- 6.Astley SJ, Clarren SK. Diagnosing the full spectrum of fetal alcohol-exposed individuals: introducing the 4-digit diagnostic code. Alcohol Alcohol. 2000;35:400–410. doi: 10.1093/alcalc/35.4.400. [DOI] [PubMed] [Google Scholar]
- 7.Sampson PD, Streissguth AP, Bookstein FL, et al. Incidence of fetal alcohol syndrome and prevalence of alcohol-related neurodevelopmental disorder. Teratology. 1997;56:317–326. doi: 10.1002/(SICI)1096-9926(199711)56:5<317::AID-TERA5>3.0.CO;2-U. [DOI] [PubMed] [Google Scholar]
- 8.Sokol RJ, Clarren SK. Guidelines for use of terminology describing the impact of prenatal alcohol on the offspring. Alcohol Clin Exp Res. 1989;13:597–598. doi: 10.1111/j.1530-0277.1989.tb00384.x. [DOI] [PubMed] [Google Scholar]
- 9.Aase JM. Clinical recognition of FAS: difficulties of detection and diagnosis. Alcohol Health Res World. 1994;18:5–9. [PMC free article] [PubMed] [Google Scholar]
- 10.Abel EL. Was the fetal alcohol syndrome recognized by the Greeks and Romans? Alcohol Alcohol. 1999;34:868–872. doi: 10.1093/alcalc/34.6.868. [DOI] [PubMed] [Google Scholar]
- 11.Holy Bible: New International Version. Zondervan; Grand Rapids, MI: 1978. [Google Scholar]
- 12.Royal College of Physicians of London . Annals. Royal College of Physicians; London, England: 1726. p. 253. [Google Scholar]
- 13.Goodacre K. Guide to the Middlesex Sessions Records 1549 –1889: Prepared for the Standin. Greater London Records Office; London, United Kingdom: 1965. p. 785. [Google Scholar]
- 14.Sullivan WC. A note on the influence of maternal inebriety on the offspring. J Ment Sci. 1899;45:489–503. doi: 10.1093/ije/dyr006. [DOI] [PubMed] [Google Scholar]
- 15.May PA, Hymbaugh KJ, Aase JM, Samet JM. Epidemiology of fetal alcohol syndrome among American Indians of the Southwest. Soc Biol. 1983;30:374–387. doi: 10.1080/19485565.1983.9988551. [DOI] [PubMed] [Google Scholar]
- 16.Abel EL. An update on incidence of FAS: FAS is not an equal opportunity birth defect. Neurotoxicol Teratol. 1995;17:437–443. doi: 10.1016/0892-0362(95)00005-c. [DOI] [PubMed] [Google Scholar]
- 17.Abel EL. Fetal Alcohol Abuse Syndrome. Plenum Press; New York, NY: 1998. [Google Scholar]
- 18.Abel EL, Hannigan JH. Maternal risk factors in fetal alcohol syndrome: provocative and permissive influences. Neurotoxicol Teratol. 1995;17:445–462. doi: 10.1016/0892-0362(95)98055-6. [DOI] [PubMed] [Google Scholar]
- 19.May PA. A multiple-level, comprehensive approach to the prevention of fetal alcohol syndrome (FAS) and other alcohol-related birth defects (ARBD) Int J Addict. 1995;30:1549–1602. doi: 10.3109/10826089509104417. [DOI] [PubMed] [Google Scholar]
- 20.Lemoine P, Harousseau H, Borteyru JP, Menuet JC. Les enfants des parents alcoholiques: anomolies observees a propos de 127 cas [The children of alcoholic parents: anomalies observed in 127 cases] Ouest Med. 1968;8:476–482. [Google Scholar]
- 21.Jones KL, Smith DW, Ulleland CN, Streissguth AP. Pattern of malformation in offspring of chronic alcoholic mothers. Lancet. 1973;1:1267–1271. doi: 10.1016/s0140-6736(73)91291-9. [DOI] [PubMed] [Google Scholar]
- 22.Jones KL, Smith DW. Recognition of the fetal alcohol syndrome in early infancy. Lancet. 1973;2:999–1001. doi: 10.1016/s0140-6736(73)91092-1. [DOI] [PubMed] [Google Scholar]
- 23.Ulleland CN. The offspring of alcoholic mothers. Ann NY Acad Sci. 1972;197:167–169. doi: 10.1111/j.1749-6632.1972.tb28142.x. [DOI] [PubMed] [Google Scholar]
- 24.Aase JM, Jones KL, Clarren SK. Do we need the term “FAE”? Pediatrics. 1995;95:428–430. [PubMed] [Google Scholar]
- 25.Rosett HL. A clinical perspective of the fetal alcohol syndrome. Alcohol Clin Exp Res. 1980;4:119–122. doi: 10.1111/j.1530-0277.1980.tb05626.x. [DOI] [PubMed] [Google Scholar]
- 26.Kodituwakku P. Piyadasa Kodituwakku Comments on Sandra and Joseph Jacobson and Susan Astley on FAS/FAE. In: Tremblay RE, Barr RG, Peters RDeV, editors. Encyclopedia on Early Childhood Development. Centre of Excellence for Early Childhood Development; Montreal, Canada: 2003. pp. 1–6. Available at. Accessed February 17, 2003. [Google Scholar]
- 27.May PA, Brooke L, Gossage JP, et al. Epidemiology of fetal alcohol syndrome in a South African community in the Western Cape Province. Am J Public Health. 2000;90:1905–1912. doi: 10.2105/ajph.90.12.1905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.May PA, Gossage JP. Estimating the prevalence of fetal alcohol syndrome: a summary. Alcohol Res Health. 2001;25:159–167. [PMC free article] [PubMed] [Google Scholar]
- 29.Viljoen D, Croxford J, Gossage JP, Kodituwakku P, May PA. Characteristics of mothers of children with FAS in the Western Cape Province of South Africa: a case control study. J Stud Alcohol. 2002;63:6–17. [PubMed] [Google Scholar]
- 30.Connor PD, Sampson PD, Bookstein FL, Barr HM. Direct and indirect effects of prenatal alcohol damage on executive function. Dev Neuropsychol. 2000;18:331–354. doi: 10.1207/S1532694204Connor. [DOI] [PubMed] [Google Scholar]
- 31.Spreen O, Strauss E. A Compendium of Neuropsychological Tests: Administration, Norms, and Commentary. Oxford University Press; New York, NY: 1998. [Google Scholar]
- 32.Streissguth AP, Bookstein FL, Barr HM, Press S, Sampson PD. A fetal alcohol behavior scale. Alcohol Clin Exp Res. 1998;22:325–333. doi: 10.1111/j.1530-0277.1998.tb03656.x. [DOI] [PubMed] [Google Scholar]
- 33.Streissguth AP, Barr H. Personal Behaviors Checklist. University of Washington School of Medicine; Seattle, WA: 1998. [Google Scholar]
- 34.Jones KL. Smith's Recognizable Patterns of Human Malformation. 5th WB Saunders; Philadelphia, PA: 1997. [Google Scholar]
- 35.Stoler JM, Holmes LB. Recognition of facial features of fetal alcohol syndrome in the newborn. Am J Med Genet. 2004;127C:21–27. doi: 10.1002/ajmg.c.30012. [DOI] [PubMed] [Google Scholar]


