Abstract
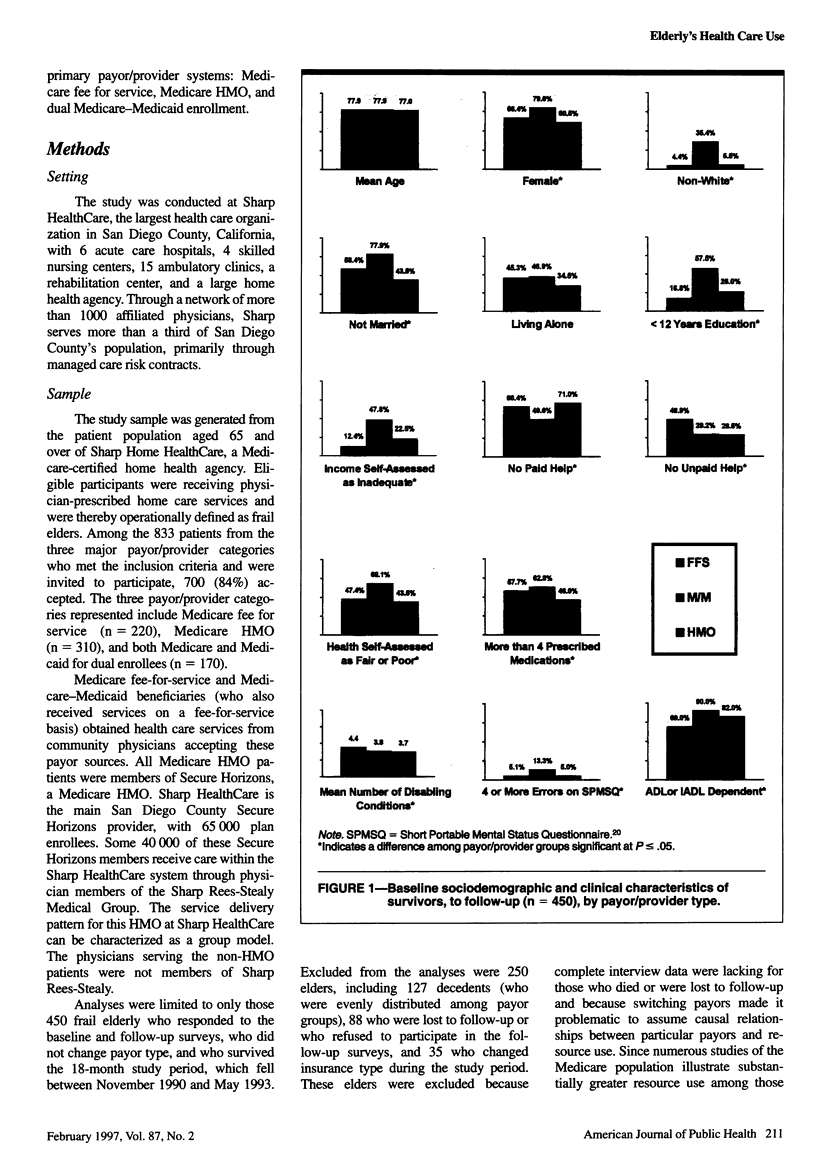
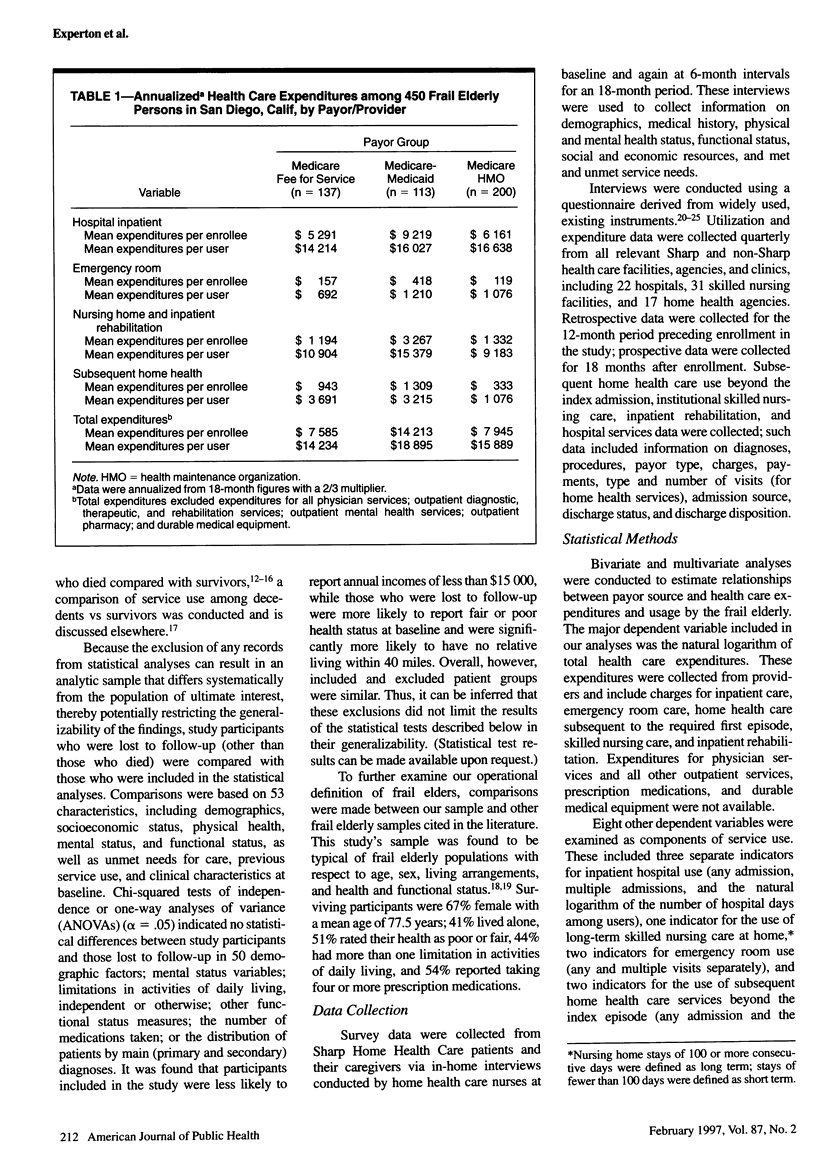
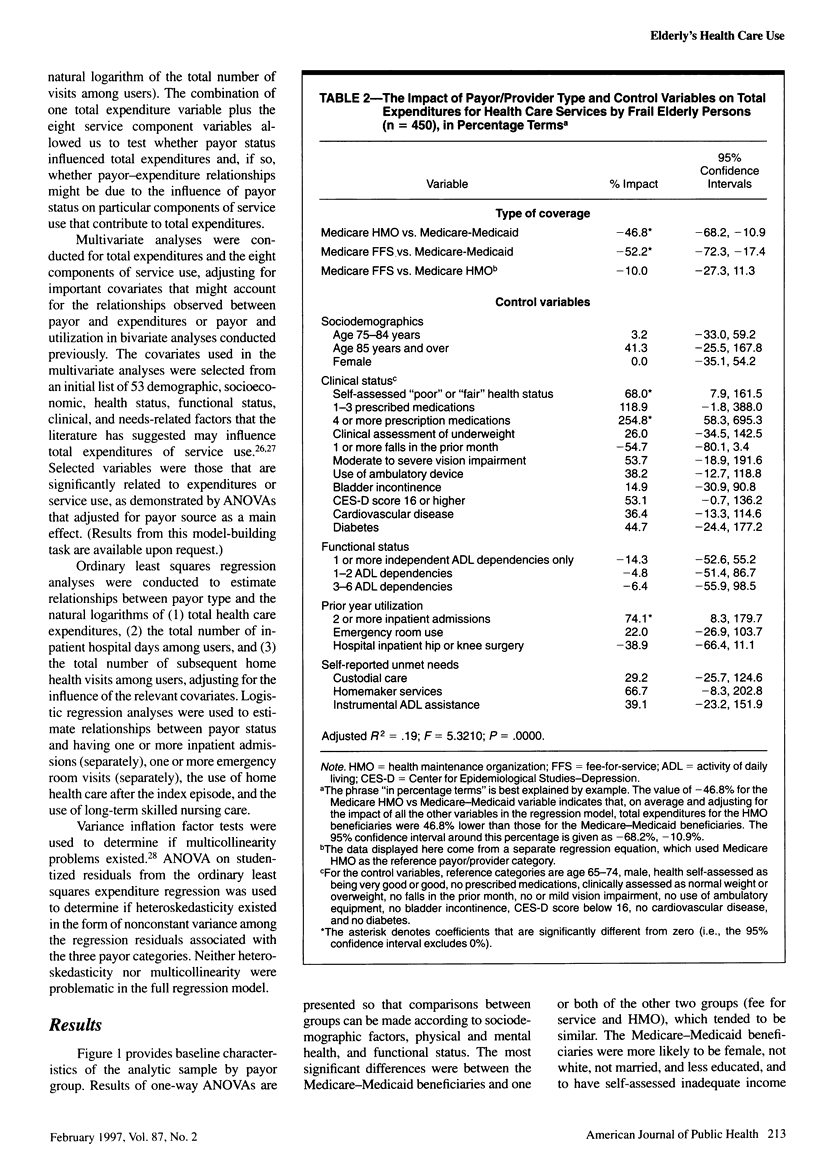
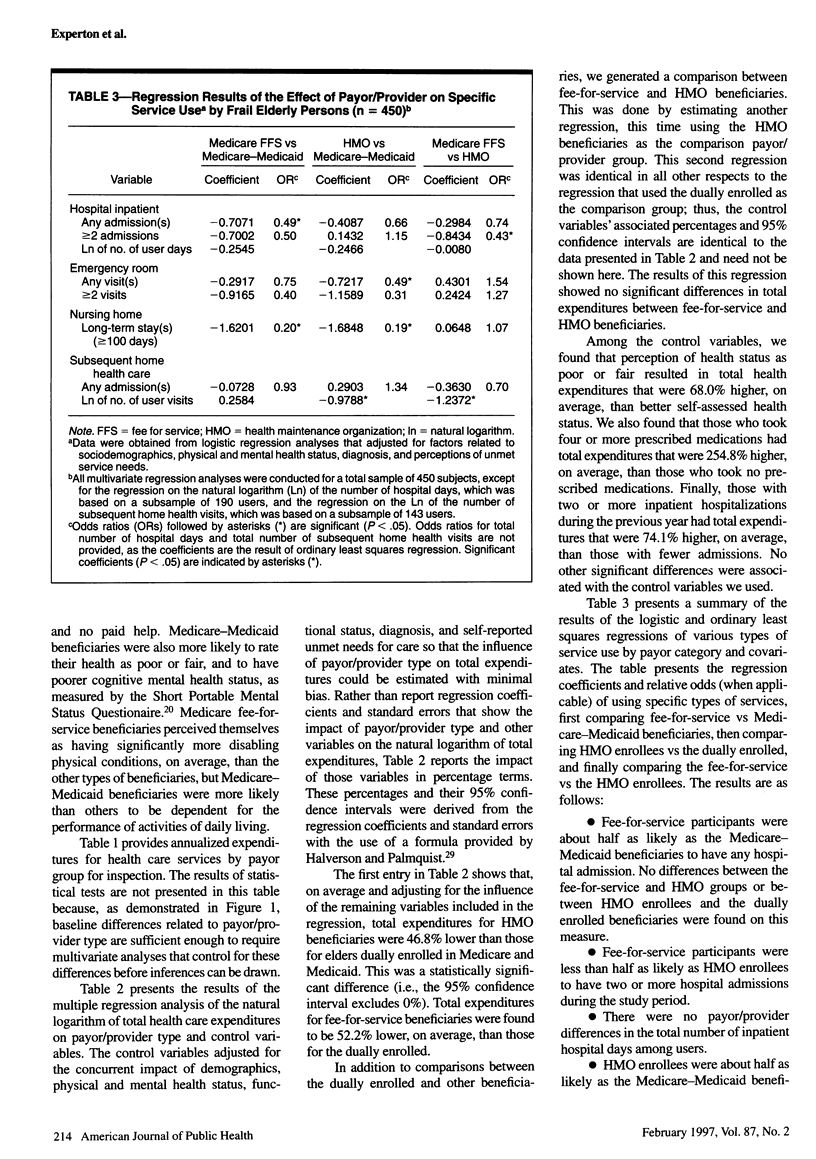
OBJECTIVES: This study examined whether health care expenditures and usage by the frail elderly differ under three payor/provider types: Medicare fee for service, Medicare health maintenance organization (HMO), and dual Medicare-Medicaid enrollment. METHODS: In-home interviews were conducted among 450 frail elderly patients of a San Diego, Calif, health care system. Cost and use data were collected from providers. RESULTS: Analyses revealed no difference in total expenditures between fee-for-service and HMO enrollees, but Medicare-Medicaid beneficiaries' expenditures were 46.8% higher than those for HMO enrollees and 52.2% higher than those for the fee-for-service group. Fee-for-service participants were less than half as likely as HMO enrollees to have two or more hospital admissions, but hospital usage rates between those two payor/provider groups did not differ. Not were there payor/provider differences in access to home health care, but HMO home health care users received significantly fewer services than the others. CONCLUSIONS: The care provided to these HMO beneficiaries resulted in a combination of restricted home health use and higher multiple hospitalizations. This raises compelling questions for future research. For the dually enrolled, stronger cost containment may be required.
Full text
PDF

Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Berkman L. F., Berkman C. S., Kasl S., Freeman D. H., Jr, Leo L., Ostfeld A. M., Cornoni-Huntley J., Brody J. A. Depressive symptoms in relation to physical health and functioning in the elderly. Am J Epidemiol. 1986 Sep;124(3):372–388. doi: 10.1093/oxfordjournals.aje.a114408. [DOI] [PubMed] [Google Scholar]
- Brown R. S., Clement D. G., Hill J. W., Retchin S. M., Bergeron J. W. Do health maintenance organizations work for Medicare? Health Care Financ Rev. 1993 Fall;15(1):7–23. [PMC free article] [PubMed] [Google Scholar]
- Clement D. G., Retchin S. M., Brown R. S., Stegall M. H. Access and outcomes of elderly patients enrolled in managed care. JAMA. 1994 May 18;271(19):1487–1492. [PubMed] [Google Scholar]
- Dowd B., Christianson J., Feldman R., Wisner C., Klein J. Issues regarding health plan payments under Medicare and recommendations for reform. Milbank Q. 1992;70(3):423–453. [PubMed] [Google Scholar]
- Experton B., Ozminkowski R. J., Branch L. G., Li Z. A comparison by payor/provider type of the cost of dying among frail older adults. J Am Geriatr Soc. 1996 Sep;44(9):1098–1107. doi: 10.1111/j.1532-5415.1996.tb02947.x. [DOI] [PubMed] [Google Scholar]
- Gaumer G. L., Stavins J. Medicare use in the last ninety days of life. Health Serv Res. 1992 Feb;26(6):725–742. [PMC free article] [PubMed] [Google Scholar]
- Holloway J. J., Thomas J. W., Shapiro L. Clinical and sociodemographic risk factors for readmission of Medicare beneficiaries. Health Care Financ Rev. 1988 Fall;10(1):27–36. [PMC free article] [PubMed] [Google Scholar]
- Jette A. M., Branch L. G., Sleeper L. A., Feldman H., Sullivan L. M. High-risk profiles for nursing home admission. Gerontologist. 1992 Oct;32(5):634–640. doi: 10.1093/geront/32.5.634. [DOI] [PubMed] [Google Scholar]
- Langwell K. M., Hadley J. P. Evaluation of the Medicare competition demonstrations. Health Care Financ Rev. 1989 Winter;11(2):65–80. [PMC free article] [PubMed] [Google Scholar]
- Liu K., Coughlin T., McBride T. Predicting nursing-home admission and length of stay. A duration analysis. Med Care. 1991 Feb;29(2):125–141. doi: 10.1097/00005650-199102000-00005. [DOI] [PubMed] [Google Scholar]
- Lubitz J. D., Riley G. F. Trends in Medicare payments in the last year of life. N Engl J Med. 1993 Apr 15;328(15):1092–1096. doi: 10.1056/NEJM199304153281506. [DOI] [PubMed] [Google Scholar]
- McCall N. Utilization and costs of Medicare services by beneficiaries in their last year of life. Med Care. 1984 Apr;22(4):329–342. doi: 10.1097/00005650-198404000-00004. [DOI] [PubMed] [Google Scholar]
- McCoy J. L., Iams H. M., Packard M. D., Shapiro J. Health of retired workers: survival status and Medicare service use. Health Care Financ Rev. 1992 Spring;13(3):65–76. [PMC free article] [PubMed] [Google Scholar]
- Pfeiffer E. A short portable mental status questionnaire for the assessment of organic brain deficit in elderly patients. J Am Geriatr Soc. 1975 Oct;23(10):433–441. doi: 10.1111/j.1532-5415.1975.tb00927.x. [DOI] [PubMed] [Google Scholar]
- Retchin S. M., Clement D. G., Rossiter L. F., Brown B., Brown R., Nelson L. How the elderly fare in HMOs: outcomes from the Medicare competition demonstrations. Health Serv Res. 1992 Dec;27(5):651–669. [PMC free article] [PubMed] [Google Scholar]
- Scitovsky A. A. "The high cost of dying": what do the data show? Milbank Mem Fund Q Health Soc. 1984 Fall;62(4):591–608. [PubMed] [Google Scholar]
- Stern R. S., Juhn P. I., Gertler P. J., Epstein A. M. A comparison of length of stay and costs for health maintenance organization and fee-for-service patients. Arch Intern Med. 1989 May;149(5):1185–1188. [PubMed] [Google Scholar]
- Stoller E. P., Cutler S. J. Predictors of use of paid help among older people living in the community. Gerontologist. 1993 Feb;33(1):31–40. doi: 10.1093/geront/33.1.31. [DOI] [PubMed] [Google Scholar]
- Vladeck B. C., Miller N. A., Clauser S. B. The changing face of long-term care. Health Care Financ Rev. 1993 Summer;14(4):5–23. [PMC free article] [PubMed] [Google Scholar]


