Abstract
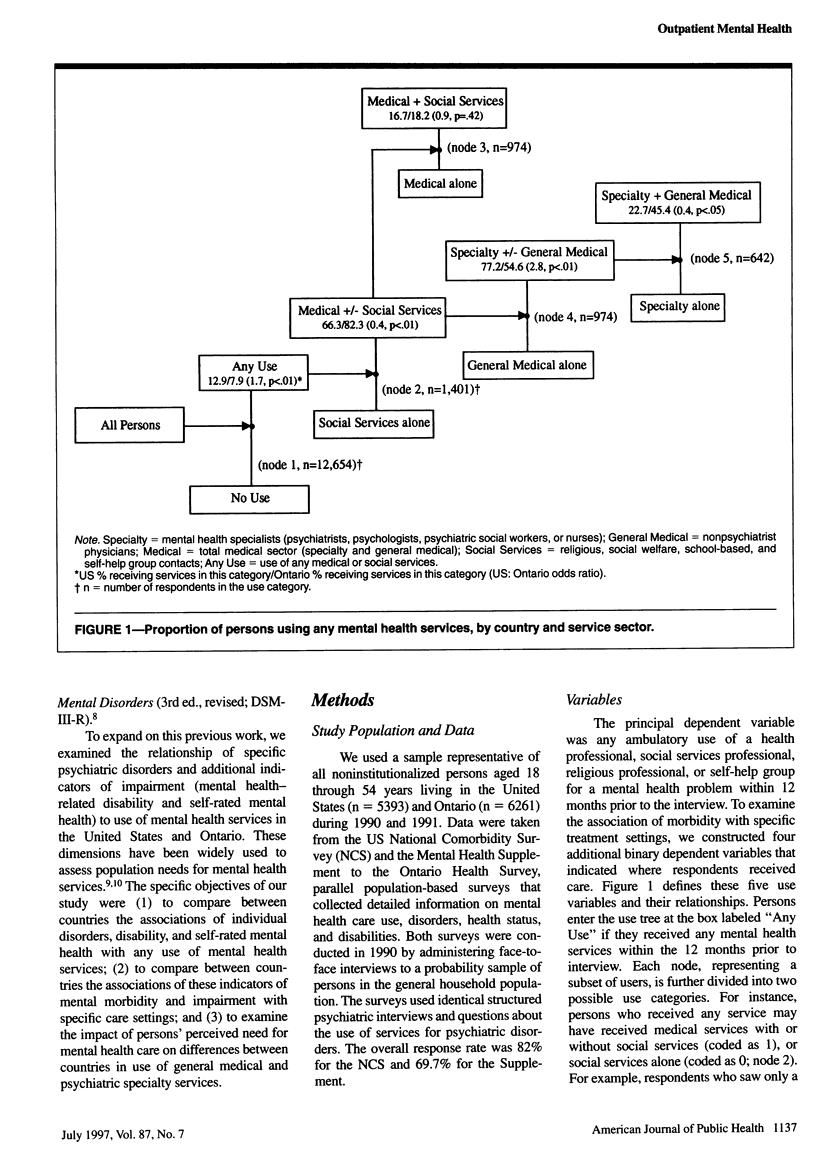
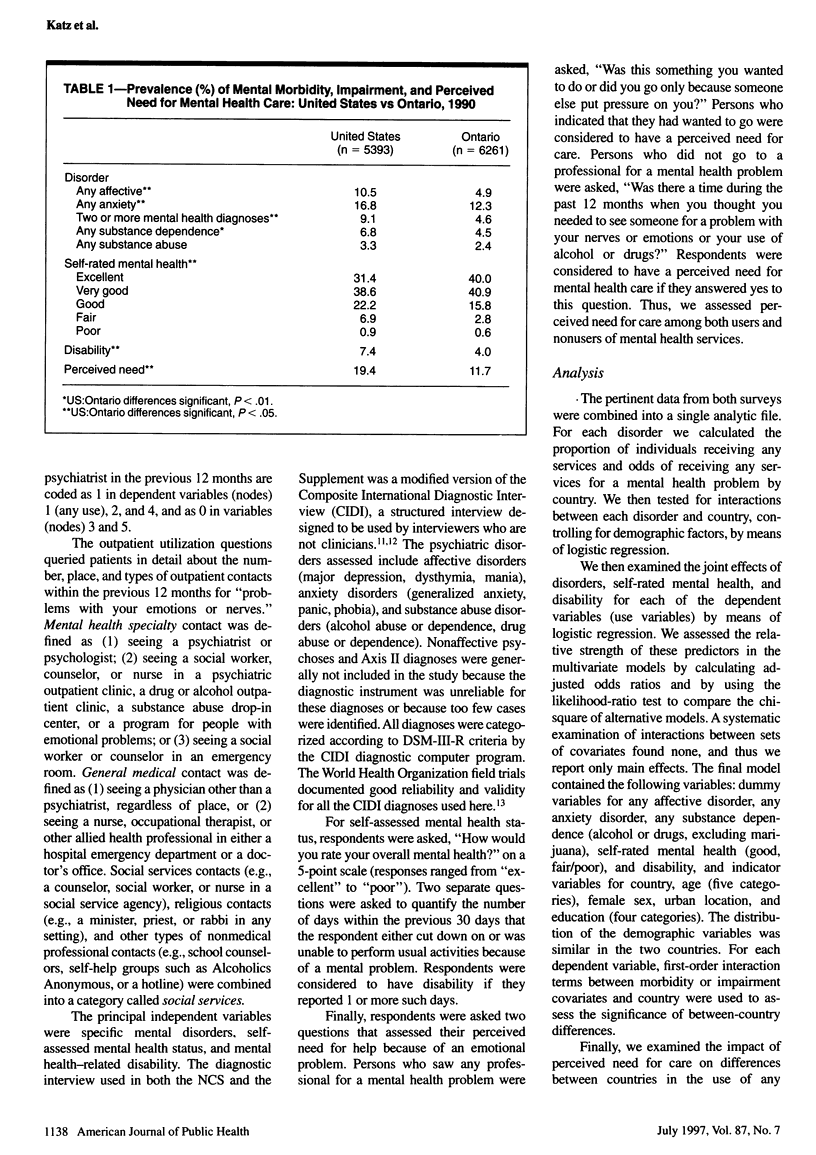
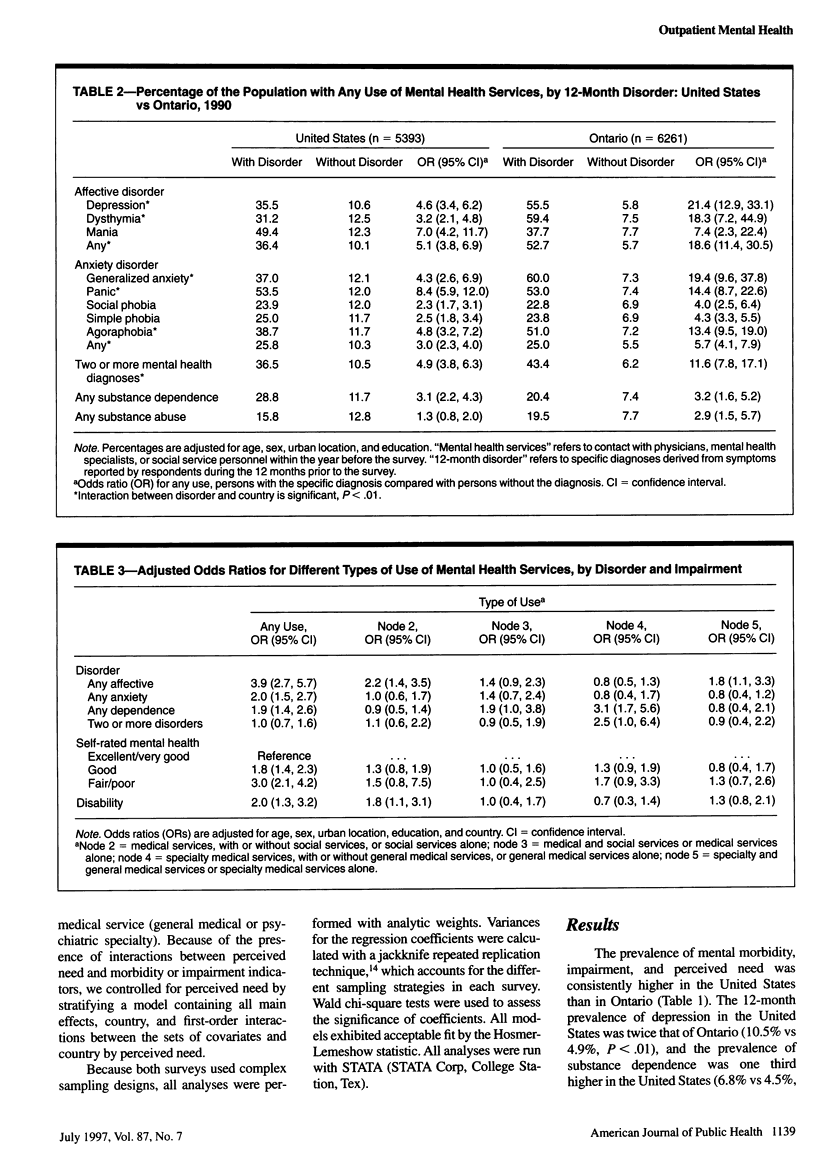
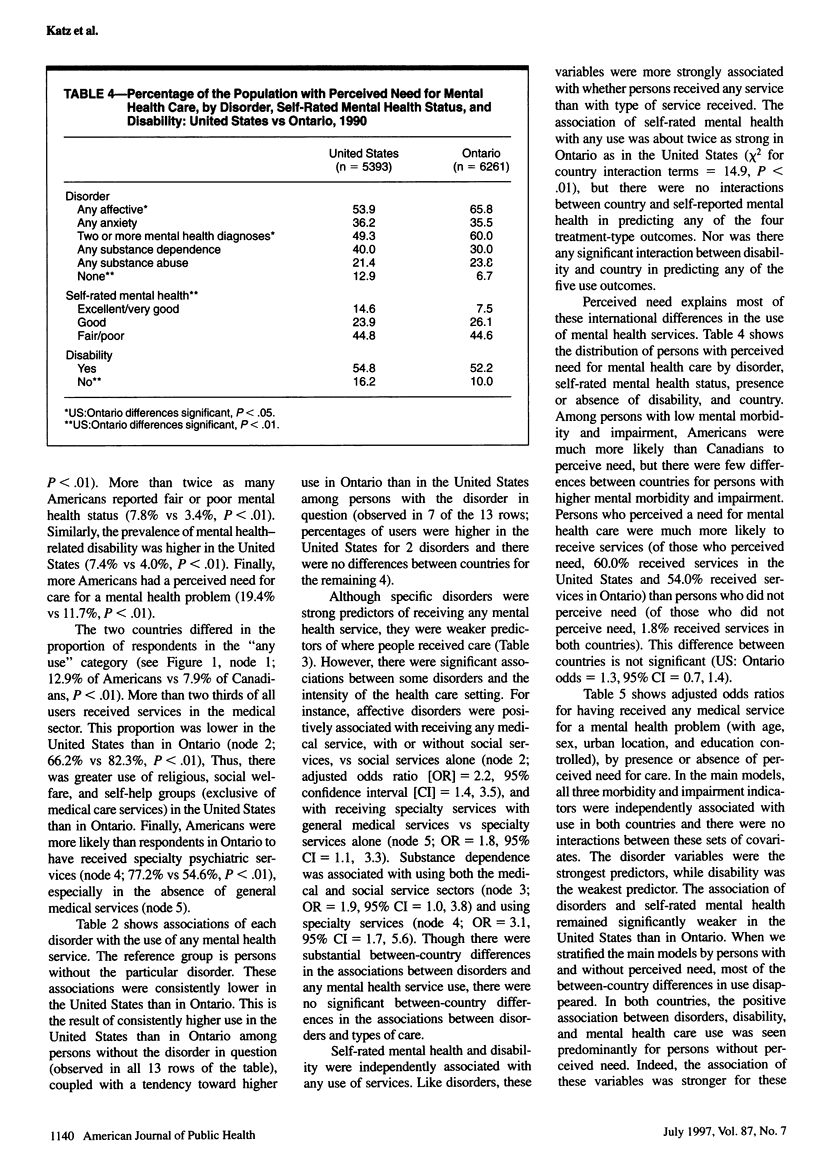
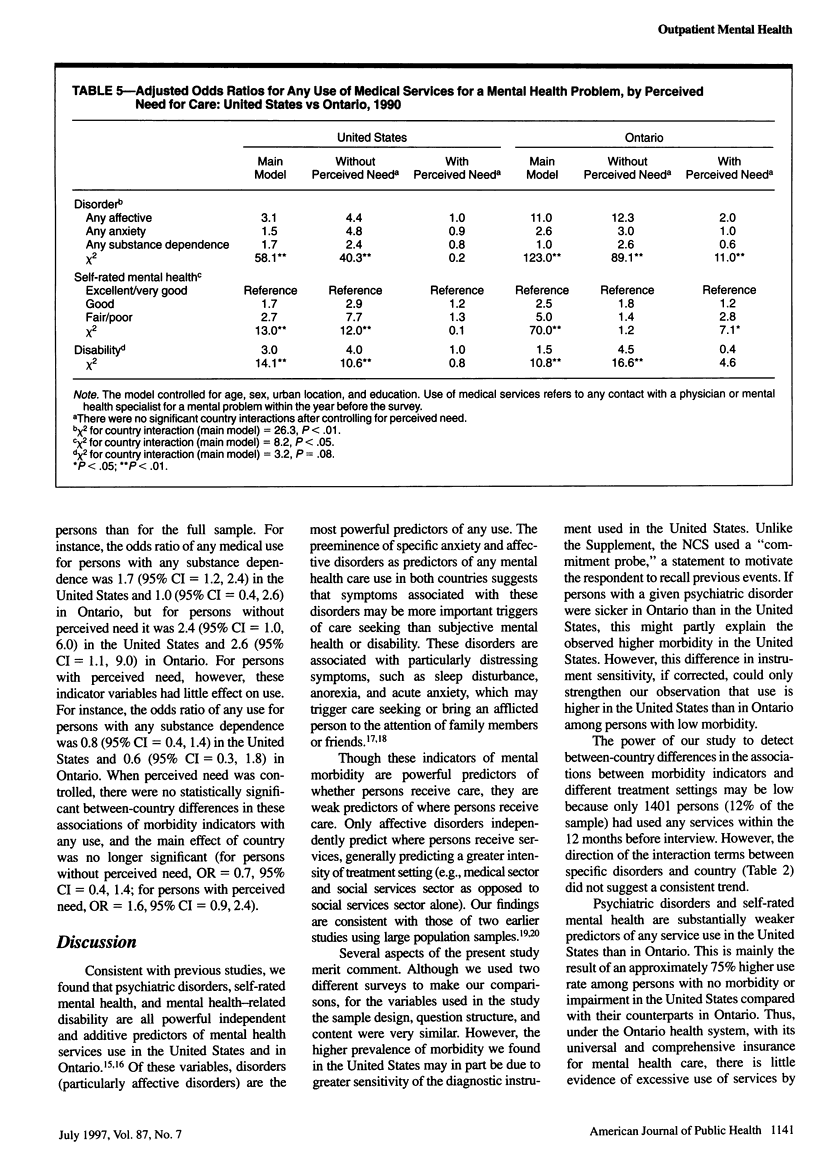
OBJECTIVES: This study compared the associations of individual mental health disorders, self-rated mental health, disability, and perceived need for care with the use of outpatient mental health services in the United States and the Canadian province of Ontario. METHODS: A cross-sectional study design was employed. Data came from the 1990 US National Comorbidity Survey and the 1990 Mental Health Supplement to the Ontario Health Survey. RESULTS: The odds of receiving any medical or psychiatric specialty services were as follows: for persons with any affective disorder, 3.1 in the United States vs 11.0 in Ontario; for persons with fair or poor self-rated mental health, 2.7 in the United States vs 5.0 in Ontario; for persons with mental health-related disability. 3.0 in the United States vs 1.5 in Ontario. When perceived need was controlled for, most of the between country differences in use disappeared. CONCLUSIONS: The higher use of mental health services in the United States than in Ontario is mostly explained by the combination of a higher prevalence of mental morbidity and a higher prevalence of perceived need for care among persons with low mental morbidity in the United States.
Full text
PDF

Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Bigelow D. A., McFarland B. H. Comparative costs and impacts of Canadian and American payment systems for mental health services. Hosp Community Psychiatry. 1989 Aug;40(8):805–808. doi: 10.1176/ps.40.8.805. [DOI] [PubMed] [Google Scholar]
- Bland R. C., Newman S. C., Orn H. Health care utilization for emotional problems: results from a community survey. Can J Psychiatry. 1990 Jun;35(5):397–400. doi: 10.1177/070674379003500506. [DOI] [PubMed] [Google Scholar]
- Frank R. G., Kamlet M. S. Determining provider choice for the treatment of mental disorder: the role of health and mental health status. Health Serv Res. 1989 Apr;24(1):83–103. [PMC free article] [PubMed] [Google Scholar]
- Frank R. G., McGuire T. G. A review of studies of the impact of insurance on the demand and utilization of specialty mental health services. Health Serv Res. 1986 Jun;21(2 Pt 2):241–265. [PMC free article] [PubMed] [Google Scholar]
- Greenley J. R., Mechanic D., Cleary P. D. Seeking help for psychologic problems. A replication and extension. Med Care. 1987 Dec;25(12):1113–1128. doi: 10.1097/00005650-198712000-00001. [DOI] [PubMed] [Google Scholar]
- Kessler R. C., Frank R. G., Edlund M., Katz S. J., Lin E., Leaf P. Differences in the use of psychiatric outpatient services between the United States and Ontario. N Engl J Med. 1997 Feb 20;336(8):551–557. doi: 10.1056/NEJM199702203360806. [DOI] [PubMed] [Google Scholar]
- Kessler R. C., McGonagle K. A., Zhao S., Nelson C. B., Hughes M., Eshleman S., Wittchen H. U., Kendler K. S. Lifetime and 12-month prevalence of DSM-III-R psychiatric disorders in the United States. Results from the National Comorbidity Survey. Arch Gen Psychiatry. 1994 Jan;51(1):8–19. doi: 10.1001/archpsyc.1994.03950010008002. [DOI] [PubMed] [Google Scholar]
- Leaf P. J., Bruce M. L., Tischler G. L., Freeman D. H., Jr, Weissman M. M., Myers J. K. Factors affecting the utilization of specialty and general medical mental health services. Med Care. 1988 Jan;26(1):9–26. doi: 10.1097/00005650-198801000-00002. [DOI] [PubMed] [Google Scholar]
- Leaf P. J., Livingston M. M., Tischler G. L., Weissman M. M., Holzer C. E., 3rd, Myers J. K. Contact with health professionals for the treatment of psychiatric and emotional problems. Med Care. 1985 Dec;23(12):1322–1337. doi: 10.1097/00005650-198512000-00002. [DOI] [PubMed] [Google Scholar]
- Mechanic D., Cleary P. D., Greenley J. R. Distress syndromes, illness behavior, access to care and medical utilization in a defined population. Med Care. 1982 Apr;20(4):361–372. doi: 10.1097/00005650-198204000-00002. [DOI] [PubMed] [Google Scholar]
- Ormel J., VonKorff M., Ustun T. B., Pini S., Korten A., Oldehinkel T. Common mental disorders and disability across cultures. Results from the WHO Collaborative Study on Psychological Problems in General Health Care. JAMA. 1994 Dec 14;272(22):1741–1748. doi: 10.1001/jama.272.22.1741. [DOI] [PubMed] [Google Scholar]
- Regier D. A., Narrow W. E., Rae D. S., Manderscheid R. W., Locke B. Z., Goodwin F. K. The de facto US mental and addictive disorders service system. Epidemiologic catchment area prospective 1-year prevalence rates of disorders and services. Arch Gen Psychiatry. 1993 Feb;50(2):85–94. doi: 10.1001/archpsyc.1993.01820140007001. [DOI] [PubMed] [Google Scholar]
- Susser M. Disease, illness, sickness; impairment, disability and handicap. Psychol Med. 1990 Aug;20(3):471–473. doi: 10.1017/s0033291700016974. [DOI] [PubMed] [Google Scholar]
- Wittchen H. U. Reliability and validity studies of the WHO--Composite International Diagnostic Interview (CIDI): a critical review. J Psychiatr Res. 1994 Jan-Feb;28(1):57–84. doi: 10.1016/0022-3956(94)90036-1. [DOI] [PubMed] [Google Scholar]


