Abstract
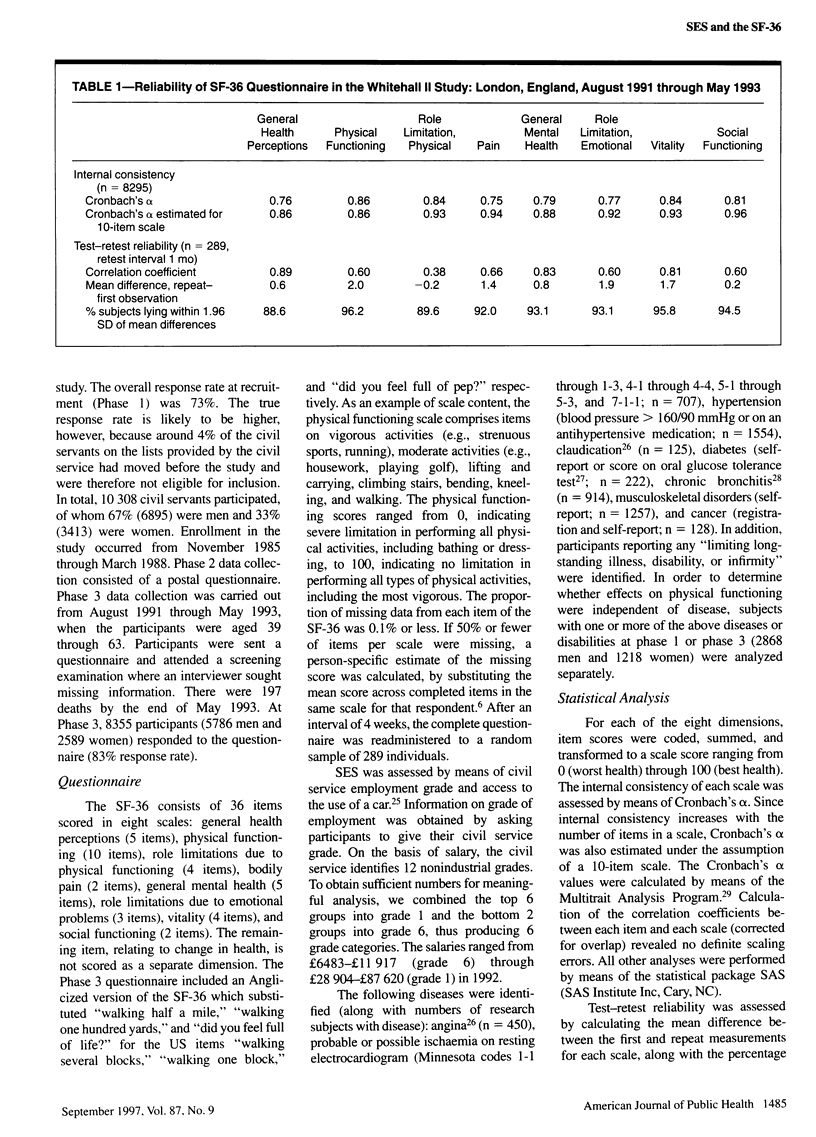
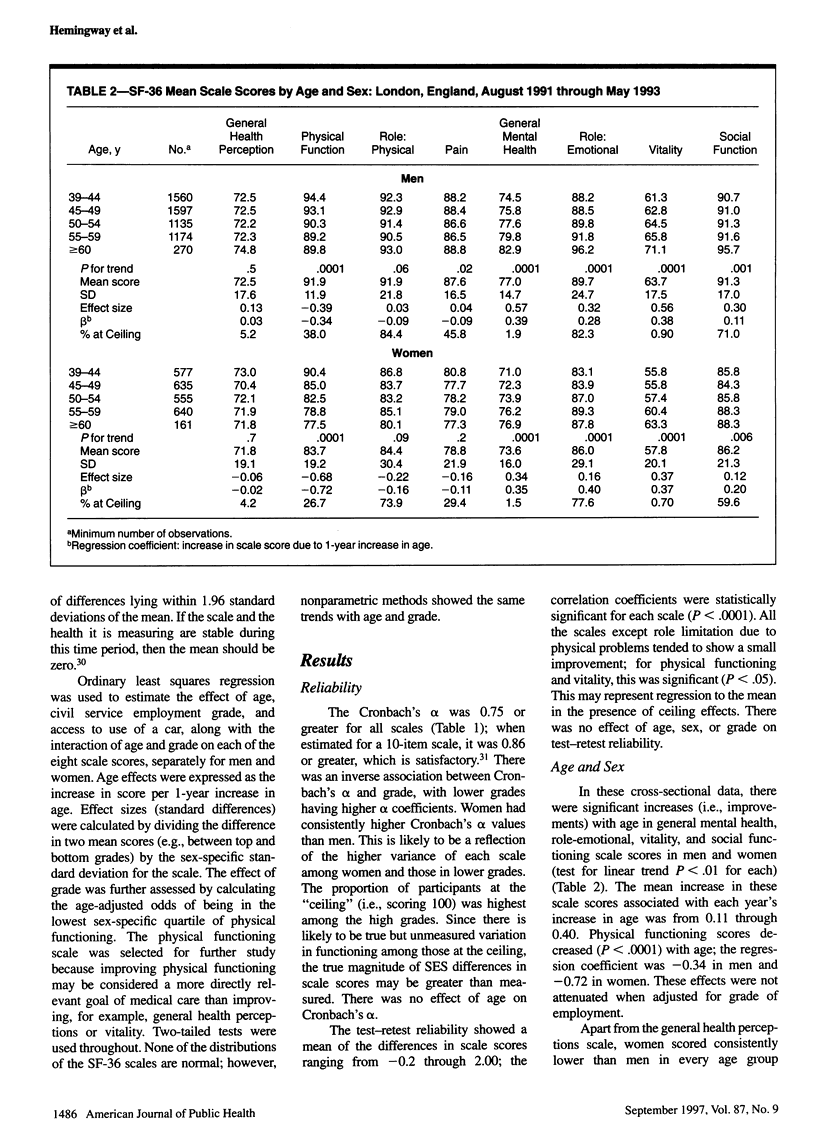
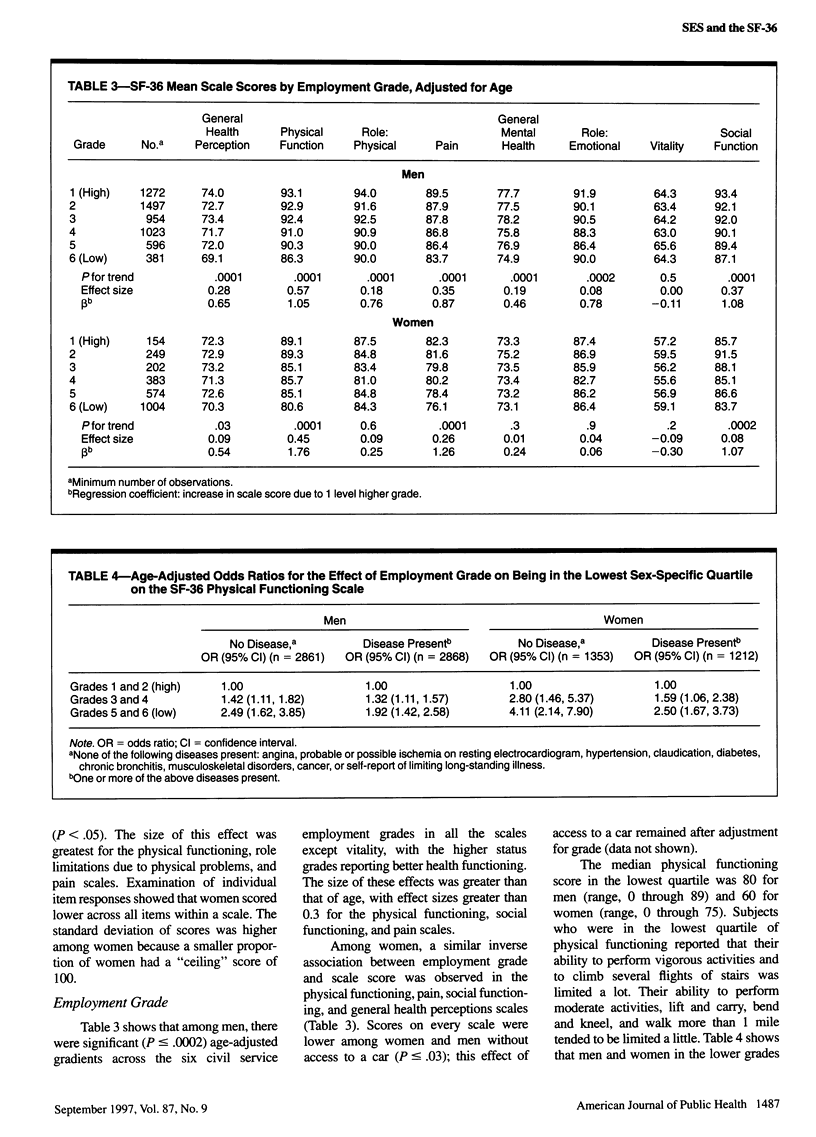
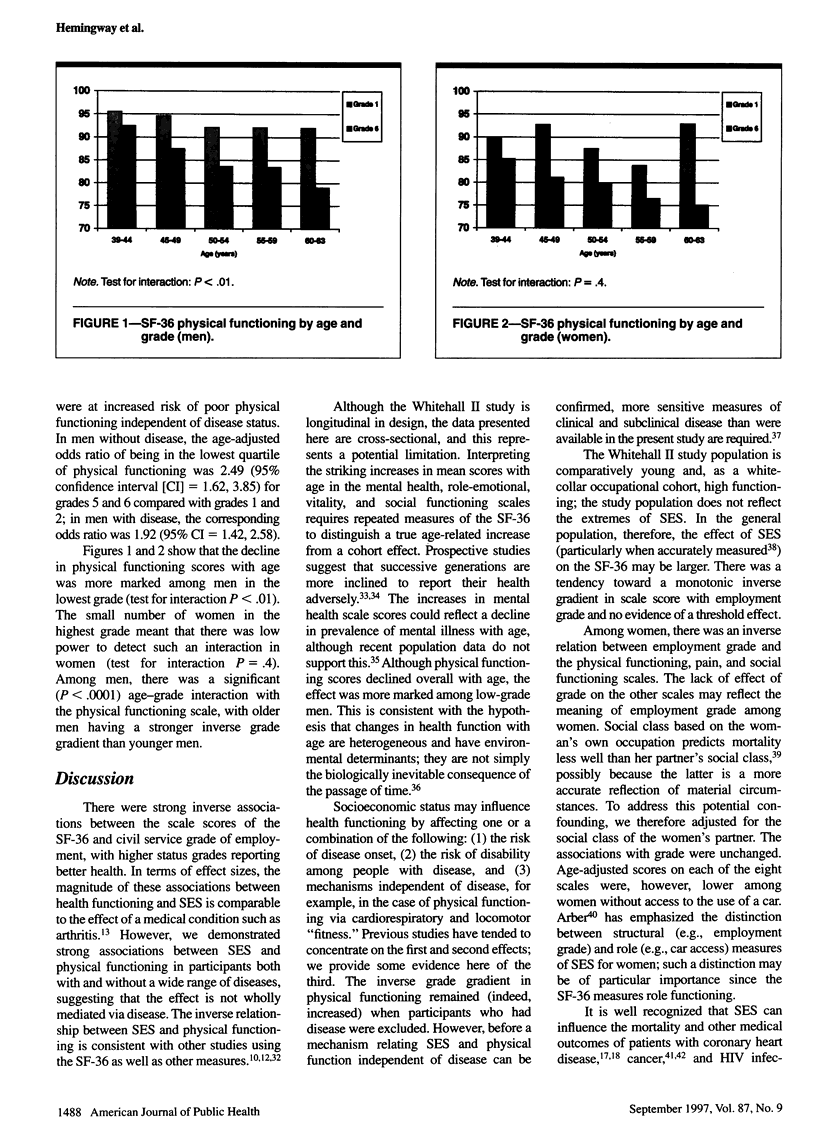
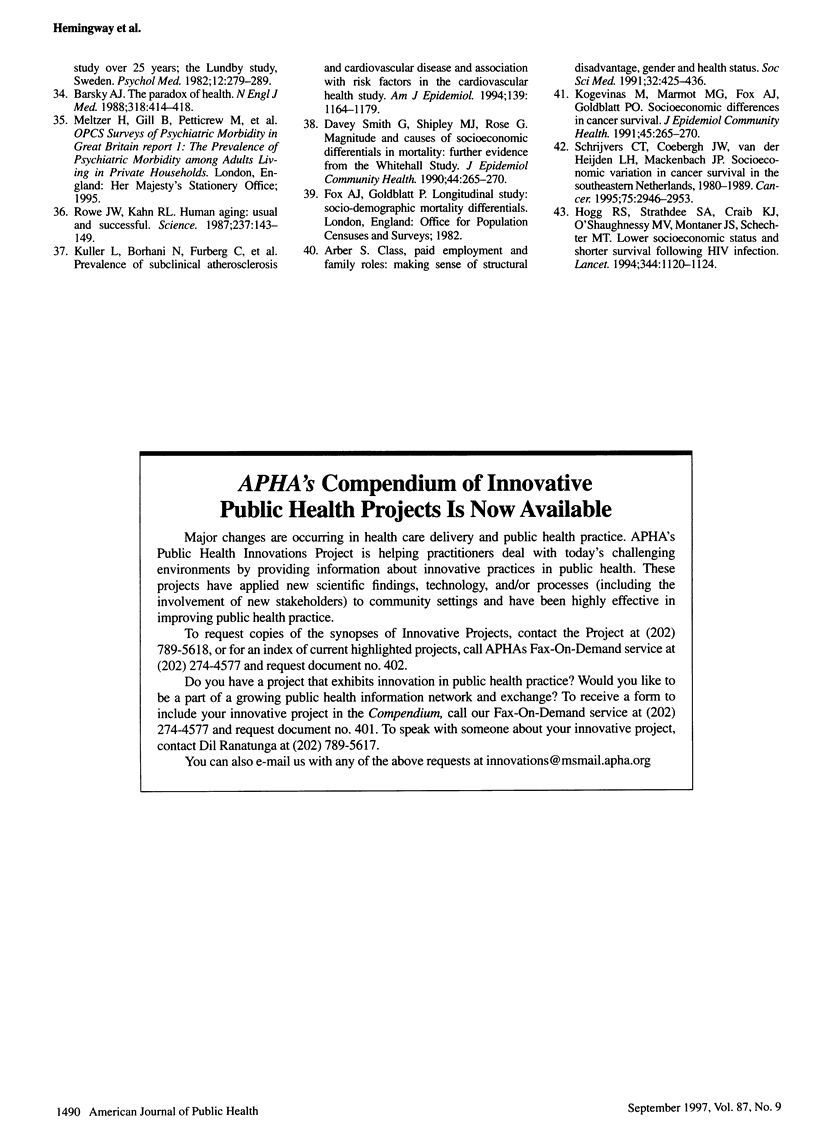
OBJECTIVES: This study measured the association between socioeconomic status and the eight scale scores of the Medical Outcomes Study short form 36 (SF-36) general health survey in the Whitehall II study of British civil servants. It also assessed, for the physical functioning scale, whether this association was independent of disease. METHODS: A questionnaire containing the SF-36 was administered at the third phase of the study to 5766 men and 2589 women aged 39 through 63 years. Socioeconomic status was measured by means of six levels of employment grades. RESULTS: There were significant improvements with age in general mental health, role-emotional, vitality, and social functioning scale scores. In men, all the scales except vitality showed significant age-adjusted gradients across the employment grades (lower grades, worse health). Among women, a similar relationship was found for the physical functioning, pain, and social functioning scales. For physical functioning, the effect of grade was found in those with and without disease. CONCLUSIONS: Low socioeconomic status was associated with poor health functioning, and the effect sizes were comparable to those for some clinical conditions. For physical functioning, this association may act both via and independently of disease.
Full text
PDF

Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Arber S. Class, paid employment and family roles: making sense of structural disadvantage, gender and health status. Soc Sci Med. 1991;32(4):425–436. doi: 10.1016/0277-9536(91)90344-c. [DOI] [PubMed] [Google Scholar]
- Barsky A. J. The paradox of health. N Engl J Med. 1988 Feb 18;318(7):414–418. doi: 10.1056/NEJM198802183180705. [DOI] [PubMed] [Google Scholar]
- Berkman L. F., Seeman T. E., Albert M., Blazer D., Kahn R., Mohs R., Finch C., Schneider E., Cotman C., McClearn G. High, usual and impaired functioning in community-dwelling older men and women: findings from the MacArthur Foundation Research Network on Successful Aging. J Clin Epidemiol. 1993 Oct;46(10):1129–1140. doi: 10.1016/0895-4356(93)90112-e. [DOI] [PubMed] [Google Scholar]
- Bland J. M., Altman D. G. Statistical methods for assessing agreement between two methods of clinical measurement. Lancet. 1986 Feb 8;1(8476):307–310. [PubMed] [Google Scholar]
- Brazier J. E., Harper R., Jones N. M., O'Cathain A., Thomas K. J., Usherwood T., Westlake L. Validating the SF-36 health survey questionnaire: new outcome measure for primary care. BMJ. 1992 Jul 18;305(6846):160–164. doi: 10.1136/bmj.305.6846.160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Detsky A. S. Regional variation in medical care. N Engl J Med. 1995 Aug 31;333(9):589–590. doi: 10.1056/NEJM199508313330911. [DOI] [PubMed] [Google Scholar]
- Garratt A. M., Ruta D. A., Abdalla M. I., Buckingham J. K., Russell I. T. The SF36 health survey questionnaire: an outcome measure suitable for routine use within the NHS? BMJ. 1993 May 29;306(6890):1440–1444. doi: 10.1136/bmj.306.6890.1440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hogg R. S., Strathdee S. A., Craib K. J., O'Shaughnessy M. V., Montaner J. S., Schechter M. T. Lower socioeconomic status and shorter survival following HIV infection. Lancet. 1994 Oct 22;344(8930):1120–1124. doi: 10.1016/s0140-6736(94)90631-9. [DOI] [PubMed] [Google Scholar]
- Hunt S. M., McEwen J., McKenna S. P. Social inequalities and perceived health. Eff Health Care. 1985;2(4):151–160. [PubMed] [Google Scholar]
- Jenkinson C., Coulter A., Wright L. Short form 36 (SF36) health survey questionnaire: normative data for adults of working age. BMJ. 1993 May 29;306(6890):1437–1440. doi: 10.1136/bmj.306.6890.1437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Katz J. N., Larson M. G., Phillips C. B., Fossel A. H., Liang M. H. Comparative measurement sensitivity of short and longer health status instruments. Med Care. 1992 Oct;30(10):917–925. doi: 10.1097/00005650-199210000-00004. [DOI] [PubMed] [Google Scholar]
- Kuh D. J., Wadsworth M. E., Yusuf E. J. Burden of disability in a post war birth cohort in the UK. J Epidemiol Community Health. 1994 Jun;48(3):262–269. doi: 10.1136/jech.48.3.262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kuller L., Borhani N., Furberg C., Gardin J., Manolio T., O'Leary D., Psaty B., Robbins J. Prevalence of subclinical atherosclerosis and cardiovascular disease and association with risk factors in the Cardiovascular Health Study. Am J Epidemiol. 1994 Jun 15;139(12):1164–1179. doi: 10.1093/oxfordjournals.aje.a116963. [DOI] [PubMed] [Google Scholar]
- Landefeld C. S., Palmer R. M., Kresevic D. M., Fortinsky R. H., Kowal J. A randomized trial of care in a hospital medical unit especially designed to improve the functional outcomes of acutely ill older patients. N Engl J Med. 1995 May 18;332(20):1338–1344. doi: 10.1056/NEJM199505183322006. [DOI] [PubMed] [Google Scholar]
- Liberatos P., Link B. G., Kelsey J. L. The measurement of social class in epidemiology. Epidemiol Rev. 1988;10:87–121. doi: 10.1093/oxfordjournals.epirev.a036030. [DOI] [PubMed] [Google Scholar]
- Lyons R. A., Fielder H., Littlepage B. N. Measuring health status with the SF-36: the need for regional norms. J Public Health Med. 1995 Mar;17(1):46–50. [PubMed] [Google Scholar]
- Marmot M. G., Rose G., Shipley M., Hamilton P. J. Employment grade and coronary heart disease in British civil servants. J Epidemiol Community Health. 1978 Dec;32(4):244–249. doi: 10.1136/jech.32.4.244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marmot M. G., Smith G. D., Stansfeld S., Patel C., North F., Head J., White I., Brunner E., Feeney A. Health inequalities among British civil servants: the Whitehall II study. Lancet. 1991 Jun 8;337(8754):1387–1393. doi: 10.1016/0140-6736(91)93068-k. [DOI] [PubMed] [Google Scholar]
- McHorney C. A., Ware J. E., Jr, Raczek A. E. The MOS 36-Item Short-Form Health Survey (SF-36): II. Psychometric and clinical tests of validity in measuring physical and mental health constructs. Med Care. 1993 Mar;31(3):247–263. doi: 10.1097/00005650-199303000-00006. [DOI] [PubMed] [Google Scholar]
- Mor V., Murphy J., Masterson-Allen S., Willey C., Razmpour A., Jackson M. E., Greer D., Katz S. Risk of functional decline among well elders. J Clin Epidemiol. 1989;42(9):895–904. doi: 10.1016/0895-4356(89)90103-0. [DOI] [PubMed] [Google Scholar]
- Pinsky J. L., Branch L. G., Jette A. M., Haynes S. G., Feinleib M., Cornoni-Huntley J. C., Bailey K. R. Framingham Disability Study: relationship of disability to cardiovascular risk factors among persons free of diagnosed cardiovascular disease. Am J Epidemiol. 1985 Oct;122(4):644–656. doi: 10.1093/oxfordjournals.aje.a114144. [DOI] [PubMed] [Google Scholar]
- Pinsky J. L., Leaverton P. E., Stokes J., 3rd Predictors of good function: the Framingham Study. J Chronic Dis. 1987;40 (Suppl 1):159S-167S, 181S-2. doi: 10.1016/s0021-9681(87)80045-0. [DOI] [PubMed] [Google Scholar]
- Rowe J. W., Kahn R. L. Human aging: usual and successful. Science. 1987 Jul 10;237(4811):143–149. doi: 10.1126/science.3299702. [DOI] [PubMed] [Google Scholar]
- Ruberman W., Weinblatt E., Goldberg J. D., Chaudhary B. S. Psychosocial influences on mortality after myocardial infarction. N Engl J Med. 1984 Aug 30;311(9):552–559. doi: 10.1056/NEJM198408303110902. [DOI] [PubMed] [Google Scholar]
- Schrijvers C. T., Coebergh J. W., van der Heijden L. H., Mackenbach J. P. Socioeconomic variation in cancer survival in the southeastern Netherlands, 1980-1989. Cancer. 1995 Jun 15;75(12):2946–2953. doi: 10.1002/1097-0142(19950615)75:12<2946::aid-cncr2820751223>3.0.co;2-6. [DOI] [PubMed] [Google Scholar]
- Seeman T. E., Charpentier P. A., Berkman L. F., Tinetti M. E., Guralnik J. M., Albert M., Blazer D., Rowe J. W. Predicting changes in physical performance in a high-functioning elderly cohort: MacArthur studies of successful aging. J Gerontol. 1994 May;49(3):M97–108. doi: 10.1093/geronj/49.3.m97. [DOI] [PubMed] [Google Scholar]
- Smith G. D., Shipley M. J., Rose G. Magnitude and causes of socioeconomic differentials in mortality: further evidence from the Whitehall Study. J Epidemiol Community Health. 1990 Dec;44(4):265–270. doi: 10.1136/jech.44.4.265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spitzer R. L., Kroenke K., Linzer M., Hahn S. R., Williams J. B., deGruy F. V., 3rd, Brody D., Davies M. Health-related quality of life in primary care patients with mental disorders. Results from the PRIME-MD 1000 Study. JAMA. 1995 Nov 15;274(19):1511–1517. [PubMed] [Google Scholar]
- Stewart A. L., Greenfield S., Hays R. D., Wells K., Rogers W. H., Berry S. D., McGlynn E. A., Ware J. E., Jr Functional status and well-being of patients with chronic conditions. Results from the Medical Outcomes Study. JAMA. 1989 Aug 18;262(7):907–913. [PubMed] [Google Scholar]
- Tarlov A. R., Ware J. E., Jr, Greenfield S., Nelson E. C., Perrin E., Zubkoff M. The Medical Outcomes Study. An application of methods for monitoring the results of medical care. JAMA. 1989 Aug 18;262(7):925–930. doi: 10.1001/jama.262.7.925. [DOI] [PubMed] [Google Scholar]
- Williams R. B., Barefoot J. C., Califf R. M., Haney T. L., Saunders W. B., Pryor D. B., Hlatky M. A., Siegler I. C., Mark D. B. Prognostic importance of social and economic resources among medically treated patients with angiographically documented coronary artery disease. JAMA. 1992 Jan 22;267(4):520–524. [PubMed] [Google Scholar]



