Abstract
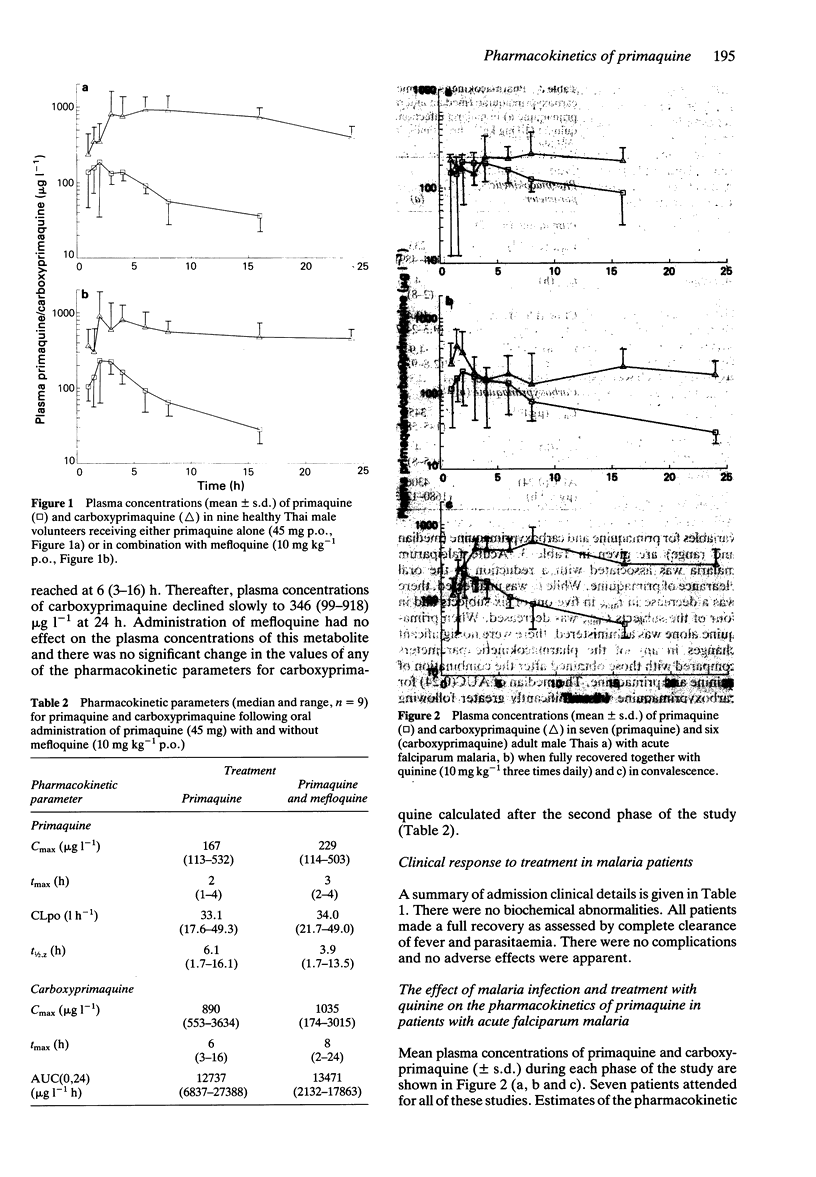
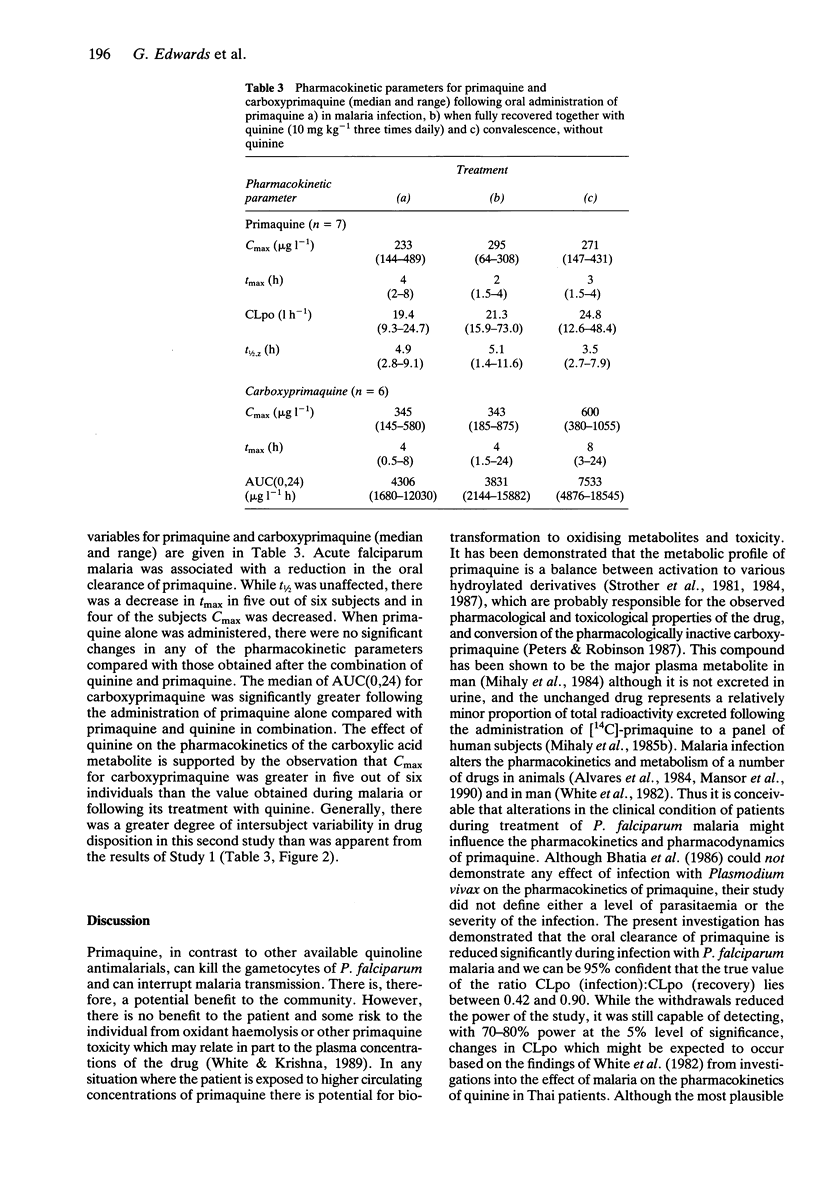
1. The pharmacokinetics of rac-primaquine (45 mg base) and its principal plasma metabolite, carboxyprimaquine have been investigated in healthy Thai adults prior to and following a single oral dose of mefloquine (10 mg kg-1). 2. Primaquine was rapidly absorbed, attaining peak plasma concentrations (median and range) of 167 (113-532) micrograms l-1 in 2 (1-4) h. Thereafter, concentrations declined rapidly with an apparent terminal half-life of 6.1 (1.7-16.1) h and an oral clearance (CLpo) of 33.1 (17.6-49.3) l h-1. Administration of mefloquine had no effect on the values of any of these parameters at the 5% level of significance [Cmax 229 (114-503) micrograms l-1; tmax 3 (2-4) h; t1/2,z 3.9 (1.7-13.5) h; CLpo 34.0 (21.7-49.0) l h-1]. 3. The carboxylic acid metabolite of primaquine achieved maximum concentrations (median and range) of 890 (553-3634) micrograms l-1 at 6 (3-16) h. Thereafter, plasma concentrations of carboxyprimaquine declined to 346 (99-918) micrograms l-1 at 24 h. AUC (0,24 h) was 12737 (6837-27388) micrograms l-1 h. Administration of mefloquine had no effect on the plasma concentrations of this metabolite [Cmax 1035 (174-3015) micrograms l-1; tmax 8 (2-24) h; AUC(0,24) 13471 (2132-17863) micrograms l-1 h]. 4. The effect of falciparum malaria and treatment with quinine (10 mg salt kg-1 p.o.) on the pharmacokinetics of primaquine (45 mg base p.o.) has been investigated in adult Thai patients during and after infection with falciparum malaria.(ABSTRACT TRUNCATED AT 250 WORDS)
Full text
PDF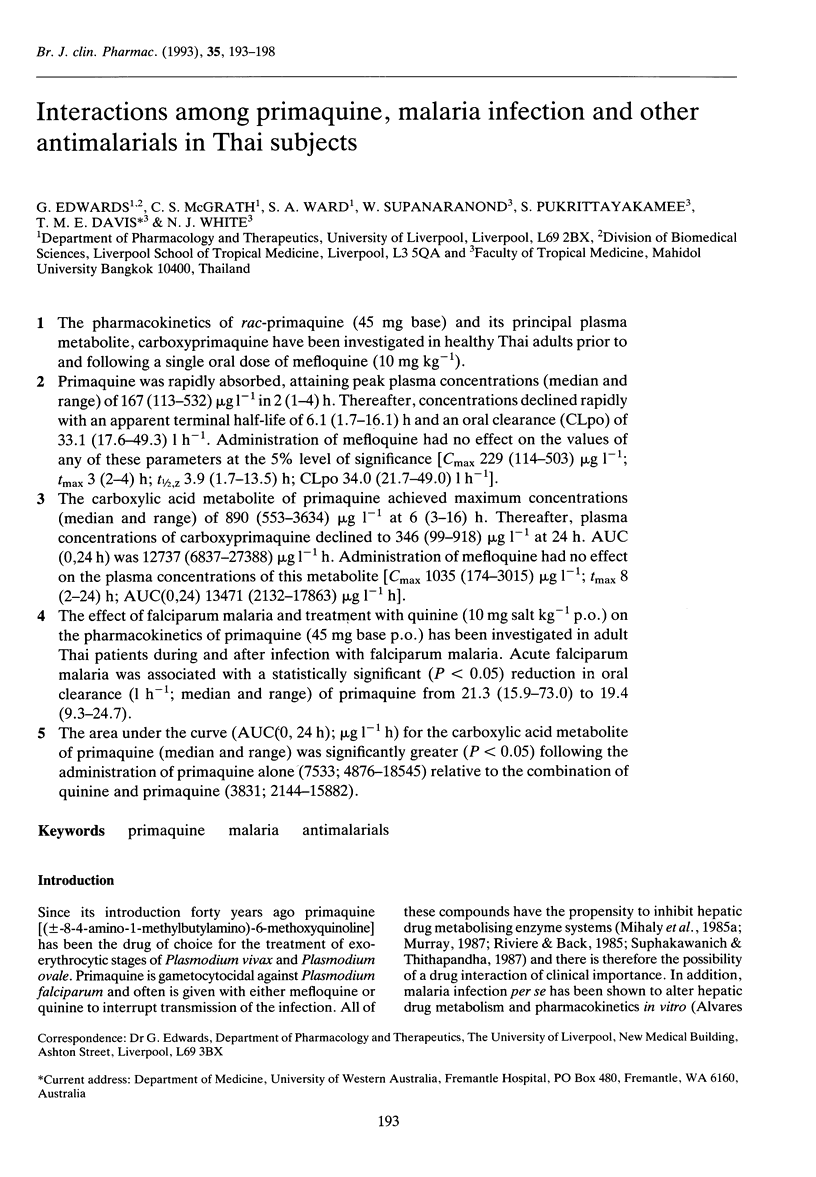
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Alvares A. P., Ueng T. H., Scheibel L. W., Hollingdale M. R. Impairment of hepatic cytochrome P-450-dependent monooxygenases by the malaria parasite Plasmodium berghei. Mol Biochem Parasitol. 1984 Nov;13(3):277–282. doi: 10.1016/0166-6851(84)90119-1. [DOI] [PubMed] [Google Scholar]
- Bangchang K. N., Karbwang J., Back D. J. Primaquine metabolism by human liver microsomes: effect of other antimalarial drugs. Biochem Pharmacol. 1992 Aug 4;44(3):587–590. doi: 10.1016/0006-2952(92)90453-p. [DOI] [PubMed] [Google Scholar]
- Bhatia S. C., Saraph Y. S., Revankar S. N., Doshi K. J., Bharucha E. D., Desai N. D., Vaidya A. B., Subrahmanyam D., Gupta K. C., Satoskar R. S. Pharmacokinetics of primaquine in patients with P. vivax malaria. Eur J Clin Pharmacol. 1986;31(2):205–210. doi: 10.1007/BF00606660. [DOI] [PubMed] [Google Scholar]
- Mansor S. M., Molyneux M. E., Taylor T. E., Ward S. A., Wirima J. J., Edwards G. Effect of Plasmodium falciparum malaria infection on the plasma concentration of alpha 1-acid glycoprotein and the binding of quinine in Malawian children. Br J Clin Pharmacol. 1991 Sep;32(3):317–321. doi: 10.1111/j.1365-2125.1991.tb03905.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mansor S. M., Ward S. A., Edwards G., Hoaksey P. E., Breckenridge A. M. The effect of malaria infection on the disposition of quinine and quinidine in the rat isolated perfused liver preparation. J Pharm Pharmacol. 1990 Jun;42(6):428–432. doi: 10.1111/j.2042-7158.1990.tb06584.x. [DOI] [PubMed] [Google Scholar]
- Mihaly G. W., Ward S. A., Edwards G., Nicholl D. D., Orme M. L., Breckenridge A. M. Pharmacokinetics of primaquine in man. I. Studies of the absolute bioavailability and effects of dose size. Br J Clin Pharmacol. 1985 Jun;19(6):745–750. doi: 10.1111/j.1365-2125.1985.tb02709.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mihaly G. W., Ward S. A., Edwards G., Orme M. L., Breckenridge A. M. Pharmacokinetics of primaquine in man: identification of the carboxylic acid derivative as a major plasma metabolite. Br J Clin Pharmacol. 1984 Apr;17(4):441–446. doi: 10.1111/j.1365-2125.1984.tb02369.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mihaly G. W., Ward S. A., Nicholl D. D., Edwards G., Breckenridge A. M. The effects of primaquine stereoisomers and metabolites on drug metabolism in the isolated perfused rat liver and in vitro rat liver microsomes. Biochem Pharmacol. 1985 Feb 1;34(3):331–336. doi: 10.1016/0006-2952(85)90040-1. [DOI] [PubMed] [Google Scholar]
- Murray M. In vitro effects of quinoline derivatives on cytochrome P-450 and aminopyrine N-demethylase activity in rat hepatic microsomes. Biochem Pharmacol. 1984 Oct 15;33(20):3277–3281. doi: 10.1016/0006-2952(84)90090-x. [DOI] [PubMed] [Google Scholar]
- Nicholl D. D., Edwards G., Ward S. A., Orme M. L., Breckenridge A. M. The disposition of primaquine in the isolated perfused rat liver. Stereoselective formation of the carboxylic acid metabolite. Biochem Pharmacol. 1987 Oct 15;36(20):3365–3369. doi: 10.1016/0006-2952(87)90312-1. [DOI] [PubMed] [Google Scholar]
- Riviere J. H., Back D. J. Effect of mefloquine on hepatic drug metabolism in the rat: comparative study with primaquine. Biochem Pharmacol. 1985 Feb 15;34(4):567–571. doi: 10.1016/0006-2952(85)90191-1. [DOI] [PubMed] [Google Scholar]
- Strother A., Allahyari R., Buchholz J., Fraser I. M., Tilton B. E. In vitro metabolism of the antimalarial agent primaquine by mouse liver enzymes and identification of a methemoglobin-forming metabolite. Drug Metab Dispos. 1984 Jan-Feb;12(1):35–44. [PubMed] [Google Scholar]
- Strother A., Fraser I. M., Allahyari R., Tilton B. E. Metabolism of 8-aminoquinoline antimalarial agents. Bull World Health Organ. 1981;59(3):413–425. [PMC free article] [PubMed] [Google Scholar]
- Ward S. A., Mihaly G. W., Edwards G., Looareesuwan S., Phillips R. E., Chanthavanich P., Warrell D. A., Orme M. L., Breckenridge A. M. Pharmacokinetics of primaquine in man. II. Comparison of acute vs chronic dosage in Thai subjects. Br J Clin Pharmacol. 1985 Jun;19(6):751–755. doi: 10.1111/j.1365-2125.1985.tb02710.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- White N. J., Krishna S. Treatment of malaria: some considerations and limitations of the current methods of assessment. Trans R Soc Trop Med Hyg. 1989 Nov-Dec;83(6):767–777. doi: 10.1016/0035-9203(89)90322-2. [DOI] [PubMed] [Google Scholar]
- White N. J., Looareesuwan S., Warrell D. A., Warrell M. J., Bunnag D., Harinasuta T. Quinine pharmacokinetics and toxicity in cerebral and uncomplicated Falciparum malaria. Am J Med. 1982 Oct;73(4):564–572. doi: 10.1016/0002-9343(82)90337-0. [DOI] [PubMed] [Google Scholar]


