Abstract
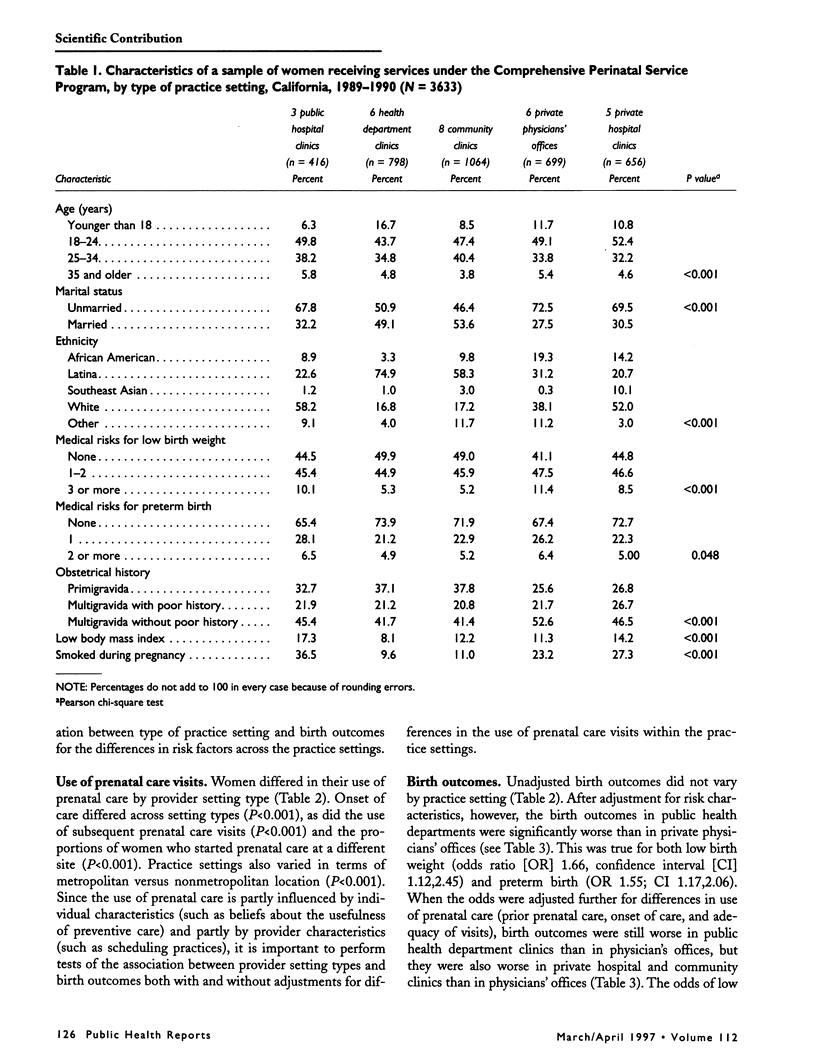
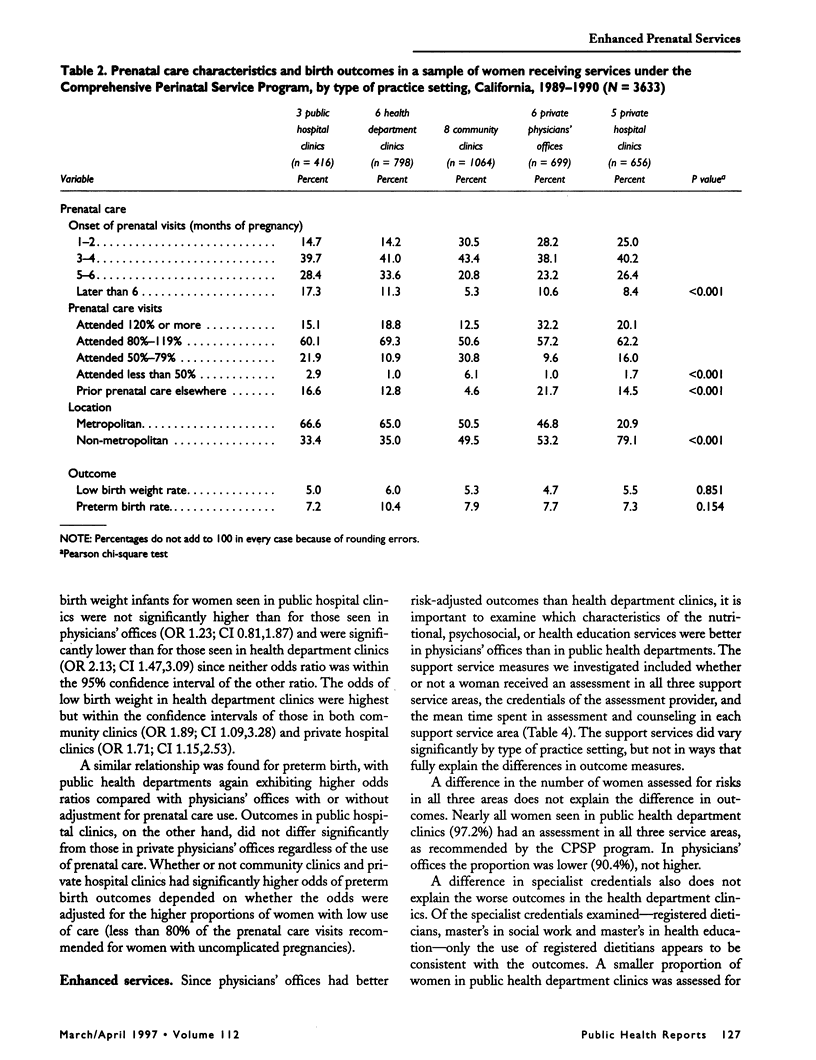
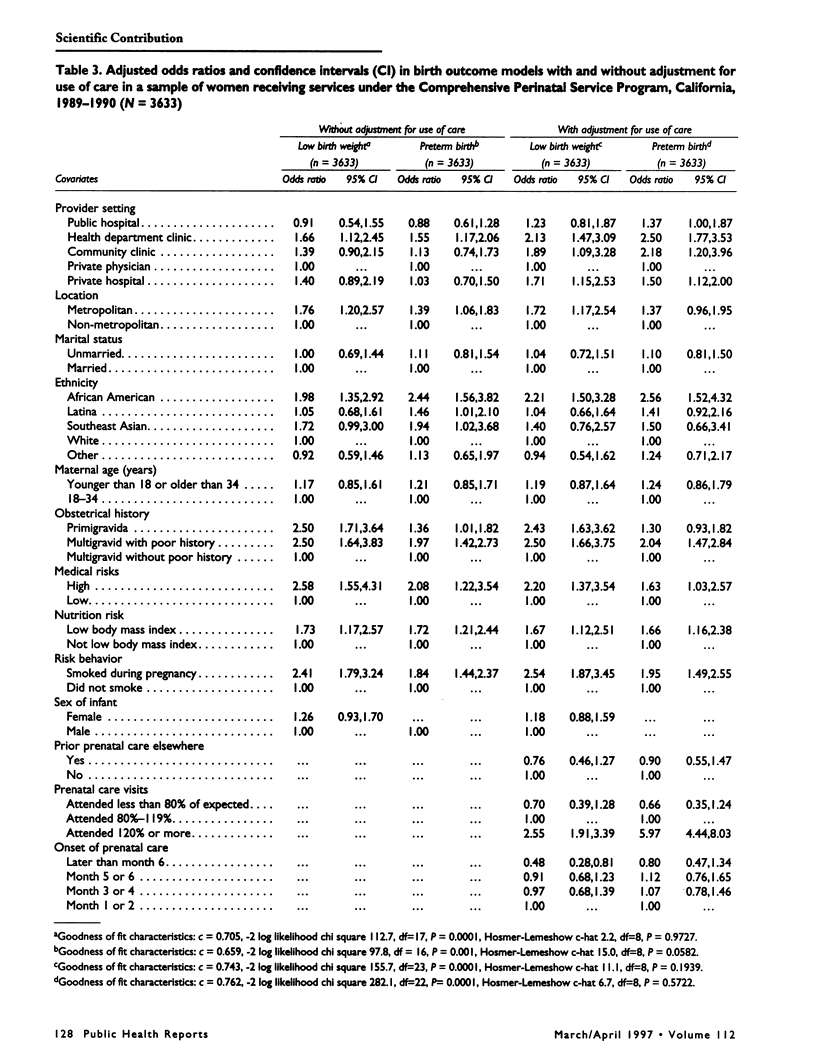
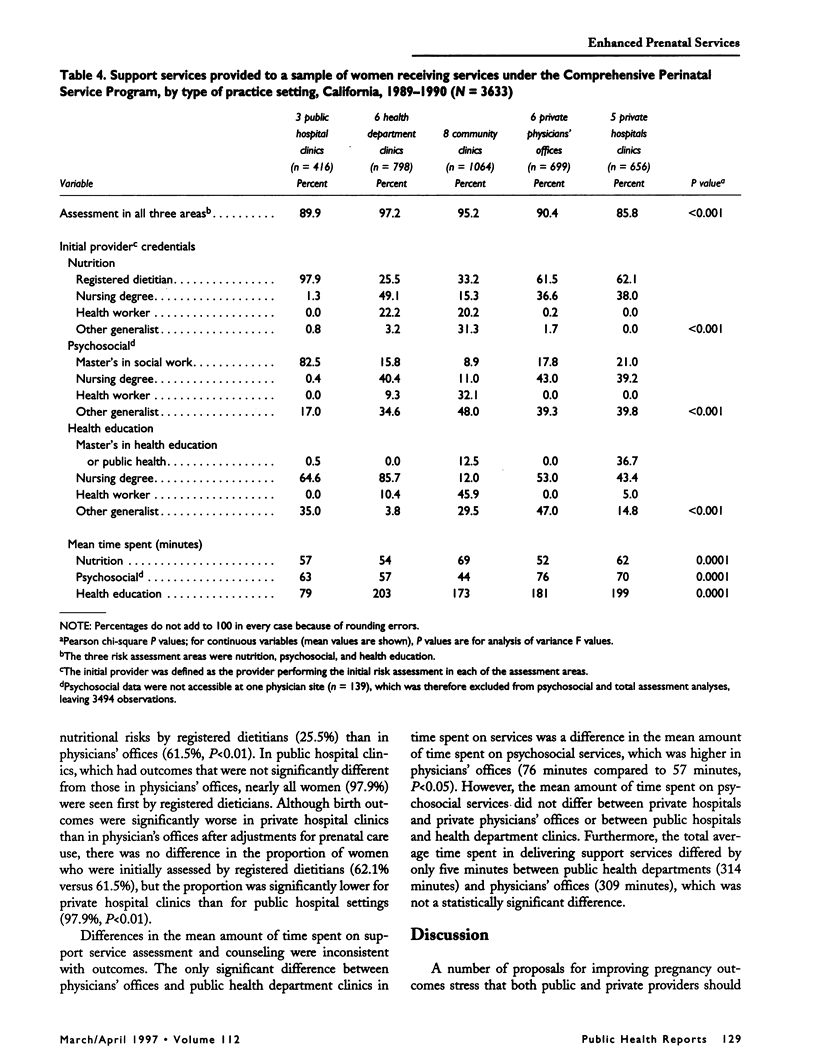
OBJECTIVE: With changes in Medicaid, more low-income women are receiving prenatal care in private practice settings. The authors sought to determine whether private settings can provide the enhanced prenatal support services for low-income women that have been offered for decades in public settings. METHODS: The authors analyzed birth outcomes of Medicaid-eligible women receiving care from public and private providers certified to deliver enhanced prenatal care services, which included assessments of nutritional, psychosocial, and health educational risks and individualized counseling along with clinical care. Birth outcomes were compared by type of provider setting using multivariate logistic regression models to adjust for differences in risks and use of care. RESULTS: Among settings certified to deliver enhanced perinatal support services, private physicians' offices had the best risk-adjusted birth outcomes and public health department clinics the worst, while public hospital clinics had outcomes no different from private physicians' offices. Adjusted for prenatal care use, outcomes were still better for women seen in private physicians' offices than for women seen in public health department clinics, community clinics, or private hospital clinics. CONCLUSIONS: The findings suggest that given a certification process, private providers can provide enhanced support services as effectively as providers in public practice settings.
Full text
PDF



Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Alexander G. R., Korenbrot C. C. The role of prenatal care in preventing low birth weight. Future Child. 1995 Spring;5(1):103–120. [PubMed] [Google Scholar]
- Alexander G. R., Tompkins M. E., Cornely D. A. Gestational age reporting and preterm delivery. Public Health Rep. 1990 May-Jun;105(3):267–275. [PMC free article] [PubMed] [Google Scholar]
- Braveman P., Bennett T., Lewis C., Egerter S., Showstack J. Access to prenatal care following major Medicaid eligibility expansions. JAMA. 1993 Mar 10;269(10):1285–1289. [PubMed] [Google Scholar]
- Buescher P. A., Smith C., Holliday J. L., Levine R. H. Source of prenatal care and infant birth weight: the case of a North Carolina county. Am J Obstet Gynecol. 1987 Jan;156(1):204–210. doi: 10.1016/0002-9378(87)90239-0. [DOI] [PubMed] [Google Scholar]
- Buescher P. A., Ward N. I. A comparison of low birth weight among Medicaid patients of public health departments and other providers of prenatal care in North Carolina and Kentucky. Public Health Rep. 1992 Jan-Feb;107(1):54–59. [PMC free article] [PubMed] [Google Scholar]
- Freda M. C., Andersen H. F., Damus K., Merkatz I. R. Are there differences in information given to private and public prenatal patients? Am J Obstet Gynecol. 1993 Jul;169(1):155–160. doi: 10.1016/0002-9378(93)90153-a. [DOI] [PubMed] [Google Scholar]
- Handler A., Rosenberg D. Improving pregnancy outcomes: public versus private care for urban, low-income women. Birth. 1992 Sep;19(3):123–130. doi: 10.1111/j.1523-536x.1992.tb00669.x. [DOI] [PubMed] [Google Scholar]
- Kogan M. D., Alexander G. R., Kotelchuck M., Nagey D. A. Relation of the content of prenatal care to the risk of low birth weight. Maternal reports of health behavior advice and initial prenatal care procedures. JAMA. 1994 May 4;271(17):1340–1345. [PubMed] [Google Scholar]
- Korenbrot C. C., Gill A., Clayson Z., Patterson E. Evaluation of California's statewide implementation of enhanced perinatal services as Medicaid benefits. Public Health Rep. 1995 Mar-Apr;110(2):125–133. [PMC free article] [PubMed] [Google Scholar]
- Kotelchuck M. An evaluation of the Kessner Adequacy of Prenatal Care Index and a proposed Adequacy of Prenatal Care Utilization Index. Am J Public Health. 1994 Sep;84(9):1414–1420. doi: 10.2105/ajph.84.9.1414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kramer M. S. Birthweight and infant mortality: perceptions and pitfalls. Paediatr Perinat Epidemiol. 1990 Oct;4(4):381–390. doi: 10.1111/j.1365-3016.1990.tb00661.x. [DOI] [PubMed] [Google Scholar]
- Kramer M. S., McLean F. H., Boyd M. E., Usher R. H. The validity of gestational age estimation by menstrual dating in term, preterm, and postterm gestations. JAMA. 1988 Dec 9;260(22):3306–3308. [PubMed] [Google Scholar]
- Liang K. Y., Zeger S. L. Regression analysis for correlated data. Annu Rev Public Health. 1993;14:43–68. doi: 10.1146/annurev.pu.14.050193.000355. [DOI] [PubMed] [Google Scholar]
- Piper J. M., Mitchel E. F., Jr, Ray W. A. Expanded Medicaid coverage for pregnant women to 100 percent of the federal poverty level. Am J Prev Med. 1994 Mar-Apr;10(2):97–102. [PubMed] [Google Scholar]
- Piper J. M., Ray W. A., Griffin M. R. Effects of Medicaid eligibility expansion on prenatal care and pregnancy outcome in Tennessee. JAMA. 1990 Nov 7;264(17):2219–2223. [PubMed] [Google Scholar]
- Starfield B., Powe N. R., Weiner J. R., Stuart M., Steinwachs D., Scholle S. H., Gerstenberger A. Costs vs quality in different types of primary care settings. JAMA. 1994 Dec 28;272(24):1903–1908. [PubMed] [Google Scholar]
- Stuart M. E., Steinwachs D. M. Patient-mix differences among ambulatory providers and their effects on utilization and payments for Maryland Medicaid users. Med Care. 1993 Dec;31(12):1119–1137. doi: 10.1097/00005650-199312000-00005. [DOI] [PubMed] [Google Scholar]


